There are about to be very large numbers of sick and dying older people in this country. Reports from other countries indicate that COVID‐19 has a low overall mortality, on par with the seasonal flu. However, in adults older than age 80, the numbers are staggeringly higher, more like 15%. The numbers of critically ill are too great to even ponder. Primary care doctors and emergency department doctors are going to be overwhelmed, but lots of others can help.
We need all of the doctors of the United States—every single one of you—to help take care of this nation's sick and dying elders. Many of you have had elective procedures and follow‐up appointments canceled. Most of you are wondering what to do, probably thinking about how to sign up to help in the emergency department or intensive care unit. As a geriatrician who does house calls for a living, I’m happy to lend my advice on how you, yes you, the orthopedists and gastroenterologists and dermatologists and psychiatrists of the United States, can help stem the tide of new infections and manage the pandemic we are facing, by helping keep your patients at home. Even the pediatricians can help check on their patients’ parents and grandparents.
Your task, should you choose to accept it: Review your list of patients older than age 60. Table 1 will walk you through the next steps.
Table 1.
Questions to Ask Yourself as You Care for Your Older Patients
| Question | Context | Steps you can take |
|---|---|---|
| How do I triage my patients aged ≥60? | Most current clinical algorithms do not differentiate between a 65‐year‐old and a 95‐year old. Even among older adults of the same age, there are large variations in level of vulnerability and physiologic reserve. | Use validated rapid risk‐stratification tools like the FRAIL screen (Figure 1), the Clinical Frailty Scale,1 or http://eprognosis.org to group older adults into categories of robust, vulnerable, and frail. Allot more time and resources for frail patients. |
| How has age contributed to my patients’ physiology? | Many practicing clinicians trained at a time when the physiologic changes of aging were not well understood. Although the science has advanced, the dissemination of knowledge still lags. Without those fundamentals, clinicians will miss subtle or variable signs of disease in their older patients, increasing the risk that their patients’ disease will progress. | Familiarize yourself with the physiologic changes of aging, especially the respiratory system.2, 3 Know, at minimum, that chief complaints and presentations are a lot less specific with age. An 85‐year‐old with an acute respiratory illness might present first, before the onset of fever, shortness of breath, and hypoxia, with delirium, fatigue, (pre)syncope, or a “mechanical” fall. Orthostatics are the most valuable vital sign change. |
| How can I take care of patients without them coming into clinic or the hospital? | To prevent the spread of infection, many health systems have limited outpatient visits. This could lead to older adults going without necessary care and thus decompensating from other illnesses. | Be proactive and reach out to your previously‐identified frail patients. Call them or do a video visit. Family members can often help navigate telehealth. If you need physical exam data, utilize home health agencies; visiting nurses can extend the reach of care. CMS has recently loosened the requirements for ordering home health services, equipment, and oxygen.4 If that is not sufficient, perform a house call. |
| How do I perform a house call? | Emergency departments and urgent care centers will be very full as COVID‐19 spreads, and there will be less availability for patients with other needs. Clinicians must adapt to help their older patients maintain their health in alternative settings. Sometimes, a hands‐on physical exam will be necessary. |
Work with your practice partners to create a geographically efficient strategy. Have administrative staff call and screen for unanticipated obstacles, such as a broken doorbell or an overly friendly dog. Wear scrubs and, if you can, change in between visits. Bring a minimum of supplies with you: PPE, a thermometer, blood pressure cuff, pulse oximeter, zip‐lock bags, and bleach wipes. Create a “clean” and a “dirty” area in your car to make decontamination easier. For more tips, ask colleagues who make house calls, or use resources from the American Academy of Home Care Medicine or the American Geriatrics Society. |
| What if older patients need to be hospitalized? | The hazards of hospitalization in older adults have been well documented for decades.5 Without careful attention to minimizing harms, there will be a second epidemic of post‐hospital disability and post‐delirium cognitive impairment. The ICU is a particularly high‐risk environment for vulnerable older adults. |
If you able to, deploy the hospital at home.6 If not, familiarize yourself with the techniques proven to reduce harm.7, 8 At the minimum, know these facts: ‐ Delirium confers a two‐fold increased risk of death and long‐term cognitive impairment.9 It is a symptom of one or more underlying problems that need to be solved10 and not with antipsychotics.11 ‐ Bedrest is toxic.12 Get rid of restraints themselves or their analogs: telemetry, continuous pulse oximeter, the Foley, the SCDs that do not do anything,13 etc. At the very least, get patients in a chair three times a day for meals. ‐ People need sensory stimulation. Do not let the hospital lose their glasses, hearing aids, or dentures. ‐ Sleep is medicine. Most people should not be woken to be monitored. ‐ Avoid hazardous medications. Benzodiazepines and antihistamines are the worst. There are other bad ones. Try not to give them, especially if nonpharmacologic techniques might help.14 |
| How do I keep my patients safe at home? | Shelter‐in‐place orders have disrupted many usual sources of community support for homebound older adults. Additionally, the rise in number of admissions is already leading to a lack of available post‐acute resources. Case managers and social workers will be overwhelmed by the demands of planning for both outpatient and post‐acute needs. |
Assess your patients’ level of function and supports. Ask these questions: ‐ What (if any) things do you need help with on a day‐to‐day basis? (showering, toileting, and other activities of daily living) ‐ Right now, are you getting that help? From whom? Are they available now, or are they sick or quarantined? ‐ How are you getting your meals, medications, and other instrumental activities of daily living met? ‐ If there are not adequate resources in place, help find them. Area Agencies on Aging are a good place to start. Additionally, trainees are stepping up to organize community services on #medstudenttwitter. |
| How do I protect my patients in nursing homes and other facilities? | Infection control in congregate settings has always been a challenge, long before the COVID‐19 outbreak. The people who staff these facilities (mostly women of color) are universally poorly paid and lacking benefits, especially paid sick leave. Additionally, there is inconsistent training on infection control, PPE availability, and testing. | Advocate your elected officials for labor protections for these workers, so that they do not come into work sick and infect vulnerable older adults. Help create partnerships between your health system and these facilities to share precious resources and knowledge. Additionally, you can come see your patients in their facilities, so that institutionalized patients do not need to come to the hospital or clinic to see you, and we can again reduce spread. |
| What do my patients actually want? |
Many older adults do not want to be intubated, but few have documented advance care plans. Patients are thinking about this as they watch the news. Primary care doctors may not have the bandwidth to have all these conversations and will need help from their colleagues. Advance care planning helps: ‐ Give your dying patients a good death. Help them die where they want and how they want. ‐ Relieve families’ guilt by not asking, “What would Mom want?” in times of crisis because you’ll already know what Mom would have wanted. ‐ Prevent equipment shortages from being exacerbated by overtreatment of people who do not want it. ‐ Help build a framework based on patient preferences for care and not across‐the‐board ageist cutoffs, for how to ration what will likely become scarce resources. |
These discussions seem hard, but there are easier ways to do it. Use proven resources, such as http://prepareforyourcare.org, Vital Talk, and http://respectingchoices.org for training, videos, discussion guides, and blank documents in many different languages and specific to many states. Make sure your documents get scanned into your EMR, and document your conversation in a way that is easy for other clinicians to find, should that be necessary. |
Abbreviations: CMS, Centers for Medicare & Medicaid Services; EMR, electronic medical record; ICU, intensive care unit; PPE, personal protective equipment; SCD, sequential compression device.
Figure 1.
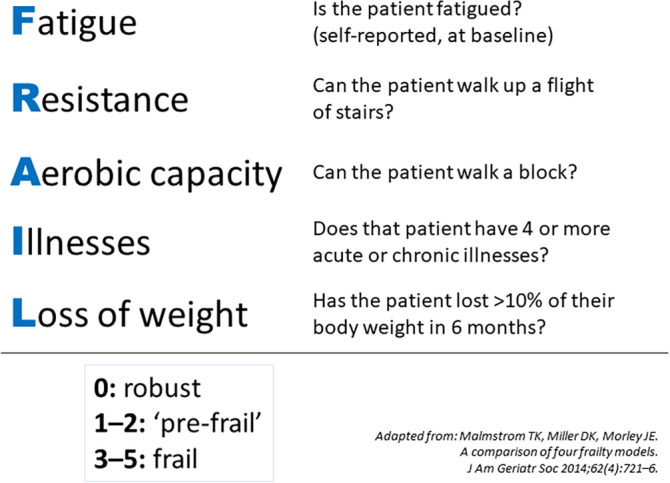
The FRAIL screen. Adapted from Malmstrom et al.16
It will require both massive efforts from individual clinicians and massive coordination from systems and institutions to give our nation’s elders the care that they want and need. If you need help, your local Big G geriatrician is probably more than willing to offer advice. But in the midst of this incoming plague, we must all become little g geriatricians now.15
ACKNOWLEDGMENTS
Financial Disclosure
None.
Conflicts of Interest
The author has declared no conflicts of interest for this article.
Author Contributions
The author is solely responsible for the content.
Sponsor’s Role
None.
This article originally appeared as a blog post on http://medium.com and is republished with permission. Minor modifications were made for journal publication.
REFERENCES
- 1. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752‐762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1(3):253‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. Physicians and other clinicians: CMS flexibilities to fight COVID‐19. https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf. Accessed April 6, 2020.
- 5. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219‐223. [DOI] [PubMed] [Google Scholar]
- 6. Hospital at Home . Hospital care in the comfort of home. http://www.hospitalathome.org/. Accessed March 19, 2020.
- 7. Inouye SK, Bogardus ST Jr, Baker DI, Leo‐Summers L, Cooney LM Jr. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. J Am Geriatr Soc. 2000;48(12):1697‐1706. [DOI] [PubMed] [Google Scholar]
- 8. Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1339. [DOI] [PubMed] [Google Scholar]
- 9. Pandharipande PP, Girard TD, Ely EW. Long‐term cognitive impairment after critical illness. N Engl J Med. 2014;370(2):185‐186. [DOI] [PubMed] [Google Scholar]
- 10. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157‐1165. [DOI] [PubMed] [Google Scholar]
- 11. Nikooie R, Neufeld KJ, Oh ES, Wilson LM, Zhang A, Robinson KA, Needham DM. Antipsychotics for treating delirium in hospitalized adults: a systematic review. Ann Intern Med. 2019; doi:10.7326/M19‐1860. [DOI] [PubMed] [Google Scholar]
- 12. Loyd C, Markland AD, Zhang Y, et al. Prevalence of hospital‐associated disability in older adults: a meta‐analysis. J Am Med Dir Assoc. 2020;21(4):455‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holleck JL, Gunderson CG. Things we do for no reason: intermittent pneumatic compression for medical ward patients? J Hosp Med. 2019;14(1):47‐50. [DOI] [PubMed] [Google Scholar]
- 14. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel . American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674‐694. [DOI] [PubMed] [Google Scholar]
- 15. Callahan KE, Tumosa N, Leipzig RM. Big ‘G’ and little ‘g’ geriatrics education for physicians. J Am Geriatr Soc. 2017;65(10):2313‐2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Malmstrom TK, Miller DK, Morley JE. A comparison of four frailty models. J Am Geriatr Soc. 2014;62(4):721‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]


