Abstract
The global outbreak of the 2019 novel coronavirus disease has had a tremendous psychological impact on individuals around the world. Individuals with obesity are susceptible to distress and psychological sequalae secondary to this pandemic, which can have detrimental effects on obesity management. In particular, individuals undergoing bariatric surgery could experience increased emotional distress, resulting in increased eating psychopathology, mental health exacerbation, and difficulties with self‐management. Addressing these challenges requires novel approaches to redefining psychosocial care before and after bariatric surgery. Emerging evidence suggests that the remote delivery of care using virtual care models, including mobile and online modalities, could extend the reach of psychosocial services to individuals after bariatric surgery and mitigate weight regain or impairment in quality of life. Because of this pandemic, the rapid integration of virtual psychosocial care in bariatric surgery programs to address patients’ needs will create new opportunities for clinical and implementational scientific research.
The outbreak of coronavirus disease 2019 (COVID‐19) has undoubtedly caused much distress among patients with obesity. The emergence of COVID‐19, the largest outbreak of atypical pneumonia since the 2013 outbreak of severe acute respiratory syndrome (SARS), has radically changed our way of life and has caused significant mortality and massive stress on our health care system. COVID‐19 may have detrimental effects on individuals with obesity, including increased risks of severe complications due to increased medical comorbidities in this population. Given that obesity alone is a major cause of physical and mental health impairment, the additive effect of COVID‐19 can also impact patients’ ability to sustain healthy lifestyle changes and routinely engage with their health care teams.
The current pandemic is also associated with additional psychological distress in the general population. Lessons learned from SARS suggest that approximately 35% of individuals at 1 month after pandemic infection experience moderate to severe depression or anxiety symptoms (1), and up to 64% of patients can have high levels of distress suggestive of psychiatric morbidity at 1 year after the pandemic (2). Cross‐sectional survey data of the general public in mainland China during the COVID‐19 outbreak showed that 54% of respondents self‐reported moderate to severe levels of psychological distress (3). Self‐isolation and quarantine have been common recommendations globally during the COVID‐19 pandemic; however, these recommendations may precipitate additional distress, such as posttraumatic stress disorder and depression, especially when implemented for prolonged periods of time (4). Patients may experience additional challenges related to quarantine, including financial difficulties resulting from loss of employment, limited access to food and other household items, and a sense of isolation (5). Self‐distancing measures and travel restrictions to reduce virus spread add additional barriers to traveling long distances to see health care teams in bariatric centers or to accessing in‐person supports.
Moreover, approximately 70% of bariatric surgery candidates have a lifetime history of psychiatric illness, which could be exacerbated by COVID‐19 pandemic–related stress (6). Data from SARS suggest that past psychiatric illness is a risk factor for developing active psychiatric illness after the pandemic (7). Extrapolating from these findings, bariatric patients may be at risk for mental health decompensation, which could impact obesity treatment adherence and long‐term patient outcomes.
Elevated levels of distress secondary to COVID‐19 may lead to emotional dysregulation, which can increase emotional eating and binge‐eating symptoms before and after bariatric surgery (8, 9). Postoperative eating psychopathology has been linked to poorer long‐term outcomes, including diminished weight loss and weight regain (10). As the pandemic continues to rapidly evolve, a positive feedback loop between COVID‐19–related distress, maladaptive eating behaviors, and psychosocial distress may develop. It is therefore imperative that patients be monitored closely for emotional dysregulation secondary to the COVID‐19 pandemic in order to mitigate problematic eating behavior and support sustained improvement in weight and quality of life.
Despite the potential challenges for patients with obesity, health care teams can use several interventions to prevent COVID‐19 sequalae using a multimodal approach starting from education and information sharing related to COVID‐19 and moving to direct psychosocial services based on patient need (Figure 1). Evidence‐based psychological interventions are needed for more severe distress in patients with obesity during COVID‐19. Cognitive behavioral therapy (CBT) and dialectical behavioral therapy offer a number of strategies that may help people cope while self‐isolating at home for an indeterminant amount of time. For example, dialectical behavioral therapy–related distress tolerance skills (e.g., distraction, self‐soothing) may be helpful in tolerating COVID‐19 events and emotions that cannot be changed immediately. CBT skills, such as cognitive restructuring, may be helpful for identifying and challenging thoughts such as “Everybody is going to die” or “This is never going to end” that may increase vulnerability to intense negative emotions and maladaptive behaviors (e.g., continuous monitoring of new COVID‐19 deaths), which can negatively affect weight management and mental health.
Figure 1.
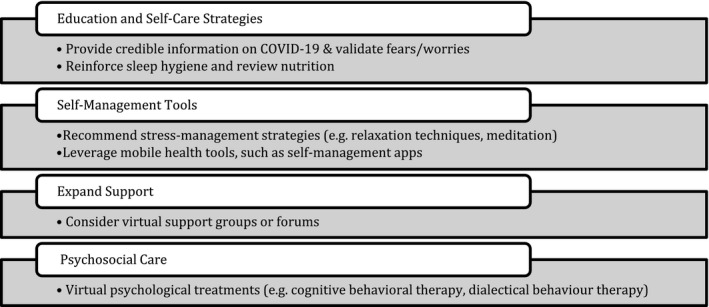
Psychosocial interventions to support mental health and bariatric care during coronavirus disease 2019 (COVID‐19).
Physical distancing, self‐isolation practices, and travel restrictions have necessitated a shift from in‐person to remotely delivered bariatric care. Rapid use of virtual health tools, such as telemedicine, has been instrumental to extending care to patients during the COVID‐19 pandemic. Telemedicine‐delivered care has been shown to result in weight loss and psychosocial outcomes comparable to those of in‐person bariatric care (11). Remotely delivered CBT by telephone or videoconferencing is effective in improving binge eating, emotional eating, depression, and anxiety among bariatric patients (12). Rapid implementation of telemedicine requires integration with existing electronic health records, policies to ensure use of secure modalities, consideration of privacy, patient safety protocols (e.g., remote management of suicidal ideation), cost analysis, and clinician training on both the technology and ability to deliver patient‐centered care using telemedicine.
Additional virtual care tools, such as app‐based tools, can also support patients with obesity when patients’ health care teams are unavailable because of COVID‐19 redeployment. Obesity‐specific support groups may provide further help to patients seeking social support during the pandemic. Although synchronous (e.g., “Zoom groups”) and asynchronous bariatric surgery–specific groups (e.g., Facebook) may be viable options, it is important to consider issues of privacy and the credibility of the information shared. An analysis of a bariatric surgery Facebook group showed that more than half the posts had information that was inaccurate or too ambiguous to assess (13).
Although the evidence for mobile and online technologies (e‐health) in obesity and bariatric care is still in its infancy, there is emerging evidence that these e‐health tools are acceptable to patients, have the potential for significant reach, and demonstrate efficacy for psychological symptoms and eating psychopathology (14). The rapid implementation of virtual care during COVID‐19 will offer greater research opportunities for improving our understanding of e‐health effectiveness in youth populations, long‐term outcomes (including weight loss), key implementation factors, and patient response.
As the number of COVID‐19 cases increases globally and extends this pandemic, it is paramount that we embrace alternate methods for delivering care to overcome challenges with physical distancing and self‐isolation. With the rapid expansion of virtual care across bariatric programs during this pandemic, we are forced to reassess our current psychosocial models and reimagine new models integrating virtual mental health tools and supports. Although these solutions provide unique opportunities to address COVID‐19–related distress, there is potential to increase our understanding and improve our delivery of psychosocial care beyond this pandemic.
Funding agencies
This manuscript was funded by a grant from the Canadian Institutes of Health Research Project (376045).
Disclosure
The authors declared no conflict of interest.
References
- 1. Cheng SK, Wong CW, Tsang J, Wong KC. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol Med 2004;34:1187‐1195. [DOI] [PubMed] [Google Scholar]
- 2. Lee AM, Wong JG, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry 2007;52:233‐240. [DOI] [PubMed] [Google Scholar]
- 3. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:E1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004;10:1206‐1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mitchell JE, Selzer F, Kalarchian MA, et al. Psychopathology before surgery in the Longitudinal Assessment of Bariatric Surgery‐3 (LABS‐3) psychosocial study. Surg Obes Relat Dis 2012;8:533‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lancee WJ, Maunder RG, Goldbloom DS; Coauthors for the Impact of SARS Study . Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv 2008;59:91‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Taube‐Schiff M, Van Exan J, Tanaka R, Wnuk S, Hawa R, Sockalingam S. Attachment style and emotional eating in bariatric surgery candidates: the mediating role of difficulties in emotion regulation. Eat Behav 2015;18:36‐40. [DOI] [PubMed] [Google Scholar]
- 9. Shakory S, Van Exan J, Mills JS, Sockalingam S, Keating L, Taube‐Schiff M. Binge eating in bariatric surgery candidates: the role of insecure attachment and emotion regulation. Appetite 2015;91:69‐75. [DOI] [PubMed] [Google Scholar]
- 10. Nasirzadeh Y, Kantarovich K, Wnuk S, et al. Binge eating, loss of control over eating, emotional eating, and night eating after bariatric surgery: results from the Toronto Bari‐PSYCH cohort study. Obes Surg 2018;28:2032‐2039. [DOI] [PubMed] [Google Scholar]
- 11. Wang CD, Rajaratnam T, Stall B, Hawa R, Sockalingam S. Exploring the effects of telemedicine on bariatric surgery follow‐up: a matched case control study. Obes Surg 2019;29:2704‐2706. [DOI] [PubMed] [Google Scholar]
- 12. David LA, Sijercic I, Cassin SE. Preoperative and post‐operative psychosocial interventions for bariatric surgery patients: a systematic review. Obes Rev 2020;21:e12926. doi: 10.1111/obr.12926 [DOI] [PubMed] [Google Scholar]
- 13. Koball AM, Jester DJ, Pruitt MA, Cripe RV, Henschied JJ, Domoff S. Content and accuracy of nutrition‐related posts in bariatric surgery Facebook support groups. Surg Obes Relat Dis 2018;14:1897‐1902. [DOI] [PubMed] [Google Scholar]
- 14. Messiah SE, Sacher PM, Yudkin J, et al. Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: a systematic review. Digit Health 2020;6:2055207619898987. doi: 10.1177/2055207619898987 [DOI] [PMC free article] [PubMed] [Google Scholar]


