Sir
The COVID‐19 pandemic is causing untold disruption across the globe, and all countries irrespective of the strength and resilience of their health systems are feeling the burden. Intensive care units are facing a surge of patients requiring invasive ventilation.
It is likely that requests for a tracheostomy in COVID‐19 ventilated patients will soon come our way. It is difficult to predict the burden, but it would be remiss not to be prepared. Tracheostomy is almost certainly an aerosol generating procedure and represents a risk to surgeons and others in the operating room. In the SARS epidemic, a survey suggested that healthcare workers who performed tracheostomy had a fourfold increased risk of developing disease. 1 Full personal protective equipment must be used, as failure to comply is a risk factor for infection in healthcare workers. 2 , 3
We have developed guidance and cognitive aids to help departments prepare for tracheostomies in COVID‐19 patients (Figure 1A‐D), based upon processes that we believe minimise risk of aerosol generation. This builds on earlier opinion 4 and incorporates our experience from simulation with a multidisciplinary team. We also consulted with a number of stakeholders, the Head & Neck Society of ENT UK, British Head & Neck Oncologists (BAHNO), British Laryngological Association, National Tracheostomy Safety Project, Difficult Airway Society (DAS) and the executive of ENT UK, who endorse the guidance.
Figure 1.
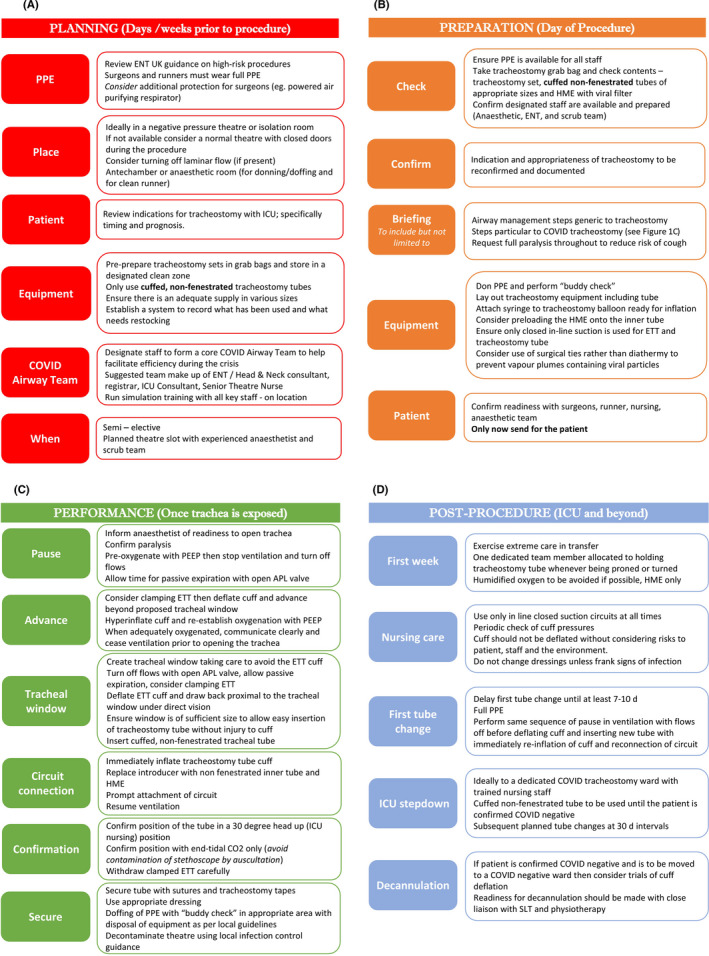
A, Planning steps recommended in the days and weeks prior to predicted tracheostomy. PPE = Personal Protective Equipment, COVID = novel Coronavirus‐19 (nCov19), ICU: Intensive Care Unit, B, Proposed checklist for the day of tracheostomy. HME = Heat and Moisture Exchanger, ETT: Endotracheal tube. C, Performance of critical steps in open tracheostomy once the trachea is exposed. PEEP = Positive End‐Expiratory Pressure, APL valve = Adjustable Pressure Limiting valve, CO2 = carbon dioxide, D, Care for the tracheostomy patient after procedure in critical care and beyond. SLT = Speech and Language Therapist
Although general complications rates using a percutaneous technique are largely similar to open tracheostomies, 5 the unanswered question here is which generates less aerosol exposure to the healthcare workers involved. Our own work with simulation would suggest that a controlled open technique as described here is potentially safer, but this is not yet validated in practice. This and other questions about when and where to perform these interventions will be influenced by local factors, competencies and experience.
Therefore, without being prescriptive, this guide is aimed at outlining the steps that can be taken by surgeons to best protect themselves and minimise aerosol generation when called on to perform open surgical tracheostomies on COVID‐19 patients.
We suggest that departments identify a core “COVID‐19 Airway team” who can rapidly adapt these guidelines to local factors and take a lead in training their colleagues. It is necessary and advisable to share the burden of these high risk and stressful events amongst all colleagues.
The key message is to prepare and stay safe.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1. Wei‐Qing Chen W, Ling W, Lu C, et al. Which preventive measures might protect health care workers from SARS? BMC Public Health. 2009;9:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tang J, Chan R. Severe acute respiratory syndrome (SARS) in intensive care units (ICUs): limiting the risk to healthcare workers. Curr Anaesth Crit Care. 2004;15(3):143‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chee VWT, Khoo M‐C, Lee SF, Lai YC, Chin NM. Infection control measures for operative procedures in severe acute respiratory syndrome–related patients. Anesthesiology. 2004;100(6):1394‐1398. [DOI] [PubMed] [Google Scholar]
- 4. Harrison L, Ramsden J. Tracheostomy guidance during the COVID‐19‐Pandemic. 2020: https://www.entuk.org/tracheostomy‐guidance‐during‐covid‐19‐pandemic
- 5. Brass P, Hellmich M, Ladra A, Ladra J, Wrzosek A. Percutaneous techniques versus surgical techniques for tracheostomy. Cochrane Database Syst Rev. 2016;7:CD008045. [DOI] [PMC free article] [PubMed] [Google Scholar]


