Short abstract
To minimize disruptions to the practice of academic pathology, one can leverage modern information and communication technologies to create virtual connections. The overall sentiment after switching to a predominantly remote environment has been overwhelmingly positive, and this presents a novel opportunity to explore additional digital workflows.
Keywords: COVID‐19, remote, remote learning, SARS‐CoV‐2, social distancing, video conference, virtual, virtual conference, virtual tumor board
Less than 2 months after the first case of coronavirus disease (COVID‐19) was reported in the United States, its incidence has started to grow exponentially. Without an available vaccine to slow the spread of the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), many pathology departments are following the guidance of public health professionals, who recommend the practice of social distancing by avoiding common spaces and generally limiting human interactions. Nationally, at many academic medical centers, this has led to the deferrals of elective procedures and the consolidation of clinical services, thereby considerably reducing the number of attendings, fellows, and residents physically present on campus. To minimize disruptions to the practice of academic pathology, one can leverage modern information and communication technologies to create virtual connections.
Daily consensus conferences in our pathology laboratories, including cytology, are valuable, educational, and necessary, but sitting around a multihead microscope with several colleagues neutralizes the goal of social distancing. Using web‐based video conferencing tools with an end‐to‐end encrypted connection allows pathologists to share diagnostically challenging cases remotely. Once the online conference is initiated, invited participants can join the session. One or more participants can share their computer screen, enabling them to broadcast the feed of a microscope‐mounted camera as they drive a slide in real time (Fig. 1). Other windows, such as the electronic health record or laboratory information system, can be shared. Participants communicate via chat or voice (computer microphone or telephone call). A collaboration interface component facilitates on‐screen annotations, which are ideal for highlighting diagnostic findings. Similarly, other clinical activities such as multidisciplinary tumor boards can benefit from the same setup, in which clinicians, diagnosticians, and surgeons can broadcast patients' charts and diagnostic imaging while openly discussing management plans.
Figure 1.
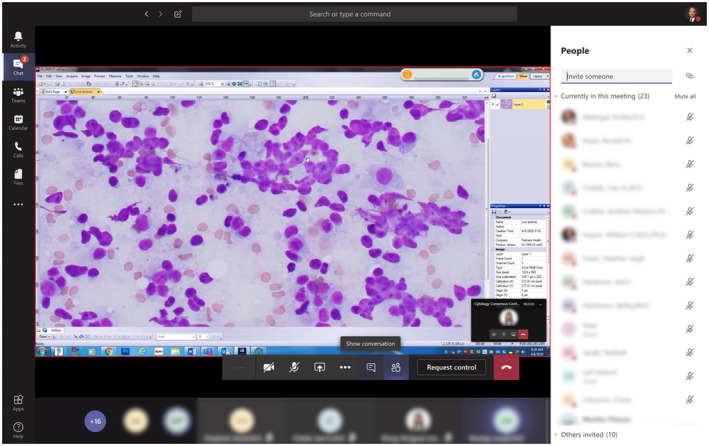
Remote cytology consensus conference. Screen capture showing 23 participants assessing a fine needle aspiration biopsy positive for lymphoma. The meeting host was broadcasting a real‐time feed of their microscope‐mounted camera.
One of the pillars of academic pathology is the education of residents and fellows. In emergencies wherein workforce preservation is of the utmost importance, residents and fellows may be asked to stay home unless covering a critical service. To mitigate the loss of teaching “scope” sessions, pathologists continue to review cases with residents and fellows following an approach similar to that of consensus conferences. Another essential educational effort is a daily “unknown” session. These sessions present a unique challenge when most residents are remote, considering they need to review the glass slides before the meeting. Using whole‐slide imaging scanners capable of producing multilayer captures, which are particularly important for cytology specimens, enables us to distribute digitized slides for remote viewing through our web‐based educational platform.
At the Massachusetts General Hospital, the resiliency of our anatomic, clinical, and cytology laboratories has been challenged, but working together to devise solutions under unprecedented circumstances has been a fruitful experience. Through ingenuity and adaptability, patient care continues to benefit from professional discussions, and educational sessions have remained intact. The overall sentiment after switching to a predominantly remote environment has been overwhelmingly positive, and this presents a novel opportunity to explore additional digital workflows.
Funding Support
No specific funding was disclosed.
Conflict of Interest Disclosures
The author made no disclosures.
Please see related articles on pages https://doi.org/10.1002/cncy.22275, https://doi.org/10.1002/cncy.22280, and https://doi.org/10.1002/cncy.22281, this issue.


