To the Editor,
Coronavirus disease 2019 (COVID‐19), caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), is now overwhelming spreading in the world. As of 11 April 2020, a total of 1.61 million COVID‐19 patients were confirmed in more than 200 countries and regions with 99 690 deaths. 1 While each country has taken all measures to control the spreading, wearing mask in general population is still controversial and different countries have different recommendations on mask use in community settings. 2 Some scholars strongly suggest wearing masks in general population, 3 however, WHO does not recommend wear masks in general population because of lack of evidence. 4 However, the absence of evidence of effectiveness just means no relevant investigation, but is not equal to evidence of ineffectiveness. 3 So far, accumulating evidence has indicated that wearing mask in general population is useful to prevent SARS‐CoV‐2 transmission.
It is infeasible to conduct well designed prospective studies to obtain evidence to evaluate the efficacy of wearing mask in general population in preventing SARS‐CoV‐2 transmission. However, it is well known that wearing mask can prevent other airborne infectious diseases, such as pulmonary tuberculosis and influenza. As a general rule, an infection can occur only after exposure to sufficient amount of an infectious pathogen. Masks cannot completely prevent the pathogen exposure, but can reduce the amount of exposed pathogen to below the infectious dose, a certain amount that can cause an infection. Even if failed in preventing an infection, wearing mask can still reduce the amount of exposed pathogen, which will cause a relatively mild disease. Thus, wearing masks in general population can prevent at least a considerable proportion of COVID‐19. More recently, Ma et al 5 showed that N95 mask, medical mask, and homemade mask with 4‐layer kitchen paper and 1‐layer cloth blocked 99.98%, 97.14%, and 95.15% of avian influenza virus in aerosols respectively, which provide evidence that masks can block the transmission of viruses in publics.
Currently, SARS‐CoV‐2 was mainly transmitted in communities and most patients had no history of contacting COVID‐19 patients. It has been demonstrated that COVID‐19 patients can spread SARS‐CoV‐2 when they are at asymptomatic incubation period, and some SARS‐CoV‐2 infected individuals do not have symptoms at all. 6 , 7 These individuals are belonging to healthy general population before they are identified. Without use of masks, they will directly release the viruses, leading to the silent spreading in community settings.
The facts that COVID‐19 transmission occurred in hundreds of persons after religion convenes in South Korea showed us lessons for the super spreading of COVID‐19 without wearing masks 8 ; none of those participants wore mask in the convenes. After this event, almost all persons in South Korea wore masks when they were outdoors or had public activities, as recommended by the South Korea Government. The daily confirmed cases were significantly reduced after 3 weeks, with daily around 100 or fewer new cases (Figure 1A). By contrast, after the surge of COVID‐19 in Italy at the beginning of March, 2020 and having taken strict measures such as “home stay” and “social distance” since then and “city quarantine in whole country” since 10 March 2020, the number of daily new cases had not significantly reduced, with daily about 4000 new cases (Figure 1B). Although the prevention strategies in South Korea and Italy may be somewhat varied, an obvious difference between South Korea and Italy appeared to the use of masks in general population, since wearing mask is not recommended in general population in Italy. The situations in other European countries, such as France and Germany, were similar to that in Italy (Figure 1B), even after having taken comprehensive control measures for several weeks.
Figure 1.
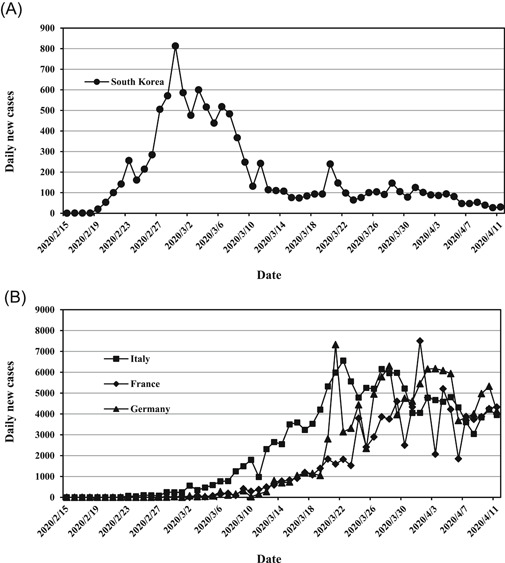
Evolution of daily confirmed new COVID‐19 patients in South Korea, Italy, France, and Germany. The data were derived from the situation reports of coronavirus disease (COVID‐19) outbreak of the World Health Organization (https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports/)
As SARS‐CoV‐2 appeared to be more rapidly spreading in Europe and USA than in Asia, some scholars in Europe argued that it is time to apply the precautionary principle and to advise wearing masks in public. 9 Actually, ordinary masks used in publics can be reused after a couple of hours in sunshine and several masks may be used in turn, 10 which has minimal influence on the mask use of healthcare providers. In conclusion, we consider that wearing mask in general population is an effective way to control COVID‐19, and should be recommended.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
REFERENCES
- 1. The World Health Organization . Coronavirus disease 2019 (COVID‐19) situation report–82. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200411‐sitrep‐82‐covid‐19.pdf?sfvrsn=74a5d15_2. Accessed April 12, 2020.
- 2. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID‐19 pandemic. Lancet Respir Med. 2020;8(5):434–436. 10.1016/S2213-2600(20)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leung CC, Lam TH, Cheng KK. Mass masking in the COVID‐19 epidemic: people need guidance. Lancet. 2020;395(10228):945. 10.1016/S0140-6736(20)30520-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO . Coronavirus disease (COVID‐19) advice for the public: when and how to use masks. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/advice‐for‐public/when‐and‐how‐to‐use‐masks. Accessed April 12, 2020.
- 5. Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask‐wearing and instant hand hygiene for fighting SARS‐CoV‐2. J Med Virol. 2020. 10.1002/jmv.25805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. He G, Sun W, Fang P, et al. The clinical feature of silent infections of novel coronavirus infection (COVID‐19) in Wenzhou. J Med Virol. 2020. 10.1002/jmv.25861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lu S, Lin J, Zhang Z, et al. Alert for non‐respiratory symptoms of coronavirus disease 2019 (COVID‐19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID‐19 patients. J Med Virol. 2020. 10.1002/jmv.25776 [DOI] [PubMed] [Google Scholar]
- 8. Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare‐associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention . Report on the epidemiological features of coronavirus disease 2019 (COVID‐19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35(10):e112. 10.3346/jkms.2020.35.e112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the COVID‐19 crisis. BMJ. 2020;369:m1435. 10.1136/bmj.m1435 [DOI] [PubMed] [Google Scholar]
- 10. Zhou ZG, Yue DS, Mu CL, Zhang L. Mask is the possible key for self‐isolation in COVID‐19 pandemic. J Med Virol. 2020. 10.1002/jmv.25846 [DOI] [PMC free article] [PubMed] [Google Scholar]


