Highlights
-
•
Rectal GIST is a rare disease, and have often grown by the time of discovery due to lack of initially subjective symptoms.
-
•
A large rectal GIST often require extensive surgery which may lead to postoperative bowel dysfunction.
-
•
Preoperative chemotherapy with imatinib mesylate is effective for reducing the rectal GIST.
-
•
Laparoscopic intersphincteric resection may be a useful technique for giant rectal GIST, which enables anal preservation.
Abbreviations: GIST, gastrointestinal stromal tumor; IM, imatinib mesylate; ISR, intersphincteric resection
Keywords: Rectal gastrointestinal stromal tumor, Imatinib, Laparoscopic intersphincteric resection
Abstract
Introduction
Anus-preserving surgery for a large rectal gastrointestinal stromal tumor (GIST) may be difficult because of the location of the tumor in the pelvis. Therefore, rectal GIST might require extensive surgery, such as abdominoperineal resection. In recent years, preoperative imatinib therapy has been used to reduce tumor size and preserve the anus in some cases. However, there have been few reports of laparoscopic anal-preserving surgery for giant rectal GIST.
Presentation of a case
We present the case of a 55-year-old man who was referred to our hospital for examination of a 10-cm pelvic mass in the lower rectum. Endoscopic ultrasound with fine needle aspiration was performed, and the pathological findings resulted in a diagnosis of GIST. The mass had spread to the prostate and left levator ani muscles, and as a result, surgery was deemed difficult to perform without damaging the pseudo-capsule. Therefore, preoperative chemotherapy with imatinib mesylate (IM) was performed for 8 months. The mass was reduced to 7.8 cm, and laparoscopic intersphincteric resection (ISR) was performed.
Discussion
We also review prior cases of rectal GIST where patients had undergone anal-preserving surgery following preoperative chemotherapy with IM. Our case represented the largest tumor size in a review of cases of patients who had successful anal-preserving laparoscopic surgery following preoperative chemotherapy with IM.
Conclusion
Preoperative chemotherapy with imatinib mesylate was effective for reducing the rectal GIST, and laparoscopic ISR was useful for anal preservation, even when a tumor is large.
1. Introduction
Surgical resection is the preferred treatment for gastrointestinal stromal tumors (GISTs). Due to lack of initially subjective symptoms, rectal GISTs have often grown by the time of discovery, and therefore, anus preservation during surgery is often difficult [1]. Recently, the effectiveness of preoperative chemotherapy with imatinib mesylate (IM) has been shown, resulting in some cases where anal-preserving surgery was possible after tumor reduction. However, there have been few reports of laparoscopic anal-preserving surgery for giant rectal GIST. We present the case of a patient with a 10 cm rectal GIST who was successfully treated with IM and laparoscopic intersphincteric resection (ISR) to preserve the anus. We also review prior cases of rectal GIST where patients had undergone anal-preserving surgery following preoperative chemotherapy with IM. Our case represented the largest tumor size in that review witch was operated laparoscopically.
The work has been reported in line with the SCARE criteria [2].
2. Presentation of case
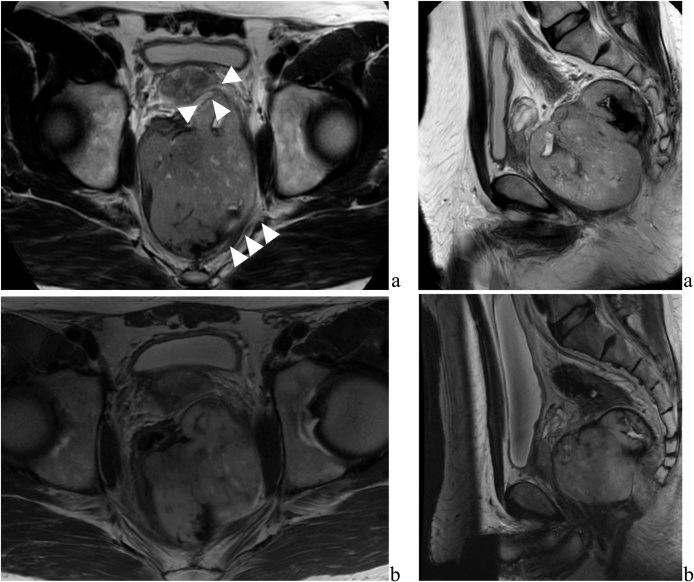
A 55-year-old man, with a history of abnormal bowel movements, visited local clinics over a 5-month period. Lower gastrointestinal endoscopy showed no abnormality in the rectal mucosa. An abdominal computed tomography (CT) found a huge mass in the Ra (rectum/above the peritoneal reflection) -Rb (rectum/below the peritoneal reflection) section of the rectum, and the patient was referred to the hospital for thorough examination. Pelvic magnetic resonance imaging (MRI) showed a mass measuring 10 cm on the left side of the lower rectum (Fig. 1). The tumor extended to the left side of the prostate and the left levator ani muscle. Endoscopic ultrasound-fine needle aspiration revealed bundles of spindle cells with positive immunohistochemical staining for c-Kit and DOG-1 but negative for S-100 protein, leading to a diagnosis of rectal GIST. Since it would be difficult to excise the tumor without pseudo-capsule damage, neoadjuvant imatinib (400 mg/day) was initiated. In a CT scan 2 months later, the tumor diameter had shrunk to 9.5 cm and the contrast effects inside the tumor had disappeared (Fig. 1). Eight months after chemotherapy was initiated, the tumor showed marked shrinkage to 7.8 cm, an almost maximum tumor response. It was decided that surgical treatment was possible at this point.
Fig. 1.
a: Magnetic resonance imaging showed a mass measuring 10 cm in maximum on the left side of the lower rectum. The tumor extended to the left side of the prostate and part of the left levator ani muscle. b: After 8 months preoperative chemotherapy with imatinib mesylate, it showed that marked shrinkage of tumor to 7.8 cm.
The patient indicated a strong desire to preserve the anus, and therefore, we chose laparoscopic ISR and temporary transverse colostomy (Fig. 2). Surgery was started from mobilizing the descending colon and sigmoid colon. The origin of the inferior mesenteric artery was exposed and dissected. Next, mesorectal excision was performed as much as possible. Around the left side of the rectum, we dissected the tumor without damaging the pseudo-capsule (Fig. 2a). When the tumor location was confirmed by intraoperative rectal examination, we judged that it was difficult to dissect the rectum from the intraperitoneal with a enough anal margin (Fig. 2b), so got started anal-side approach under the microscope. A transanal access platform (GelPOINT Path; Applied Medical) and AirSeal (CONMED) platform was introduced. Mucosal dissection was performed at the height of dentate line. The tumor was extended to the left levator ani muscle, so the mass was dissected with some muscles attached to it. The abdominal cavity and anal side was opened all around (Fig. 2c). The anal side of rectum and oral side of colon was resected, and we removed the specimen. The rectosigmoid colon and anal canal was anastomosed by handsewn suture and a temporary transverse colostomy was performed. The operation time was 608 min, and the blood loss was 130 ml.
Fig. 2.
Intraoperative laparoscopic view.
a: Large tumor where is left side of the rectum from the view of Intraperitoneal (white line). Without damaging the pseudo-capsule, we dissected the tumor. b: Tumor extending to the left levator ani muscle from the view of Intraperitoneal (yellow line). A part of tumor was attached to it (blue arrow). c: The abdominal cavity and anal side was opened all around by anal-side approach. The white line points to the tumor.
The patient recovered with no postoperative complications and left the hospital on postoperative day 10. In histopathological tissue, most of the tumor disappeared by vitrification and fibrosis (Fig. 3). One year after postoperative chemotherapy with IM, the patient exhibits no evidence of recurrence.
Fig. 3.
Pathological examinations.
a: The resected tumor was 70 × 50 mm in size with necrotic change. b: Histological examination (hematoxylin and eosin staining). Most of the tumor was disappeared by vitrification and fibrosis.
3. Discussion
Primary rectal GIST is a relatively rare disease, accounting for approximately 5% of all GIST [3]. The current report presents the case of a patient who had a large rectal GIST that had progressed to other organs and was successfully treated with preoperative IM and anus-preserving anus ISR [1]. The primary treatment for a rectal GIST is complete surgical resection with negative microscopic margins, but this procedure is challenging for surgeons because of the confined pelvic space and the nature of the GIST to densely adhere to the pelvic floor [4]. Therefore, rectal GIST might require extensive surgery, such as abdominoperineal resection or pelvic exenteration, which may lead to postoperative bowel dysfunction [3]. Recently, there have been some reported cases where anal preservation surgery was possible for large tumors following preoperative chemotherapy with IM [1,[5], [6], [7], [8], [9]].
Preoperative chemotherapy with IM is useful for the treatment of rectal GIST. Cvanar et al. studied 83 patients with rectal GIST who underwent preoperative chemotherapy and found a high tumor shrinkage rate. Sixty patients (72.3%) had a partial response (PR), 18 (21.7%) had stable disease (SD), 3 (4.8%) had a complete response (CR), and 1 (1.2%) had progressive disease (PD) according to RECIST guidelines [5]. In addition, in their retrospective series examining surgical margins, 46 of 51 patients (90%) who underwent neoadjuvant Imatinib and surgery had negative margins compared to 33 of 63 (52%) patients who did not [5]. Jakob et al. reviewed 39 patients and reported that preoperative chemotherapy led to improved surgical margins and increased local disease-free and overall survivals [6]. Wilkinson et al. examined 19 patients who underwent extended surgery for rectal GIST and reported that reducing the tumor size with preoperative chemotherapy resulted in an increased likelihood of sphincter-sparing surgery [7]. Thus, preoperative chemotherapy with IM for rectal GIST can be expected to have a tumor shrinking effect, ensure surgical margins that avoid false capsule damage, and improve postoperative oncological outcomes and anal function.
A goal of surgery for GIST is to ensure a surgically safe margin without pseudo-capsule damage [8]. For small tumors, local excision, such as transanal, transsacral, and transperineal approaches, may be selected since they are minimally invasive and preserve defecation function. On the other hand, local excision may experience a poor surgical field of view, and therefore, it may be difficult to ensure the surgical margin. Jakob et al. examined 36 patients who underwent surgical treatment for rectal GIST and reported that all cases with local recurrence had undergone local excision with positive margins and with no preoperative Imatinib [6]. They concluded that local resection should only be performed when microscopically clear margins can be safely achieved [6].
Laparoscopic ISR may, therefore, be a useful technique for giant rectal GIST. The advantages of this procedure are: 1. it may preserve anal function for tumors located in a lower position of the rectum and 2. it may ensure a safe surgical margin by extending to the intersphincteric plane through the abdomen and in resection of distal margins under a direct view through the anus [9]. However, few reports have studied the benefits of laparoscopic ISR for rectal GIST. Fuimoto et al. performed laparoscopic ISR for 5 patients with a rectal GIST after preoperative chemotherapy. All cases achieved curative resection and recurrence did not occur for any patient during the 1- to 4-year postoperative period [10].
A review of cases of patients in Japan who had successful anal-preserving surgery following preoperative chemotherapy with IM is provided (Table 1). The median tumor size was 57.5 mm, and the median tumor response rate was 33.5%, with 21 patients exhibiting a PR (75%) and seven exhibiting SD (25%). The median period for chemotherapy with IM was 4 months, and laparoscopic ISR was performed in 10 of the cases (35.7%). The current case represented the largest tumor where treatment preserved the anus using laparoscopic surgery.
Table 1.
A review of cases of patients who had successful anal-preserving surgery following preoperative chemotherapy with IM.
| Case | Author | Year | Age | Size (mm) | Response Rate (%) | NAC (a) Period (month) | Surgical Procedure |
|---|---|---|---|---|---|---|---|
| 1 | Takahashi | 2005 | 44 | 30 | 0 | 3 | Transsacral resectioln |
| 2 | Natori | 2007 | 30 | 50 | 50 | 4 | Transsacral resectioln |
| 3 | Ebihara | 2008 | 63 | 60 | 31.2 | 5 | Transanal Resection |
| 4 | Sekoguchi | 2009 | 64 | 63 | 31.2 | 4 | Transanal Resection |
| 5 | Yamakawa | 2011 | 62 | 28 | 14 | 11 | Lap-ISR (b) |
| 6 | Sakon | 2011 | 52 | 50 | 22 | 3 | Transanal Resection |
| 7 | Matsuo | 2011 | 75 | 25 | 56 | 6 | Lap-ISR |
| 8 | Kato | 2012 | 55 | 112 | 61.6 | 4 | ISR |
| 9 | Nakajima | 2012 | 58 | 66 | 68 | 6 | Lap-ISR |
| 10 | Nakajima | 2012 | 66 | 62 | 53 | 3 | Lap-ISR |
| 11 | Nakamura | 2012 | 56 | 80 | 37.5 | 3 | Lap-ISR |
| 12 | Hirata | 2013 | 94 | 80 | 38 | 4 | Transsacral resectioln |
| 13 | Ide | 2013 | 30s | 55 | 32.7 | 11 | Lap-ISR |
| 14 | Babaya | 2014 | 60 | 24 | 0 | 1 | Transperineal resection |
| 15 | Ishii | 2014 | 43 | 90 | 50 | 6 | Partial ISR |
| 16 | Yaguda | 2014 | 77 | 42 | 45.2 | 5 | Transperineal Resection |
| 17 | Shimomura | 2015 | 63 | 60 | 33 | 6 | Lap-ISR |
| 18 | Torashima | 2015 | 59 | 79 | 41.7 | 7 | ISR |
| 19 | Arimoto | 2016 | 60 | 30 | 30 | 2 | Lap-ISR |
| 20 | Takeda | 2016 | 76 | 80 | 30 | 4 | Lap-sLAR (c) |
| 21 | Tate | 2016 | 43 | 45 | 15.5 | 1.5 | Lap-sLAR |
| 22 | Kosuge | 2016 | 65 | 30 | 50 | 3 | Transsacral resectioln |
| 23 | Tazawa | 2017 | 75 | 53 | 34 | 4 | ISR |
| 24 | Yoshioka | 2017 | 67 | 50 | 24 | 1 | Transanal Resection |
| 25 | Fukuda | 2017 | 76 | 28 | 61 | 6 | Lap-ISR |
| 26 | Kenno | 2017 | 40s | 90 | 53 | 6.5 | Transperitoneal Resection |
| 27 | Mizutani | 2019 | 56 | 60 | 11 | 6 | Transperineal resection |
| 28 | Our case | 2019 | 55 | 100 | 30 | 9 | Lap-ISR |
The median tumor size was 57.5 mm, and the median tumor response rate was 33.5%, with 21 patients exhibiting a PR (75%) and seven exhibiting SD (25%). The median period for chemotherapy with IM was 4 months, and laparoscopic ISR was performed in 10 of the cases (35.7%).
NAC: Neoadjuvant chemotherapy.
Lap-ISR: Laparoscopic intersphincteric resection.
sLAR: Super lower anterior resection.
4. Conclusion
Preoperative chemotherapy with IM for giant rectal GIST is effective because it can be expected to reduce tumor size, allowing laparoscopic ISR to be a safe surgical technique for the preservation of the anus when treating a large rectal GIST.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This case report was exempted from ethical approval from the institution.
Consent
Written informed consent was obtained from the patients for publication of this case report and accompanying images.
Author contribution
S.N and N.M wrote this manuscript. S.N, N.M, T.T, H.I, S.F, T.O, H.T, M.U, C.M, T.M, MM and Y.D had medical conference to decide this surgical procedure. All authors approved the manuscript to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Registration of research studies
This paper is a clinical report, so the authors declare that no registration is needed.
Guarantor
Norikatsu Miyoshi is the Guarantor for this work.
Provenance and peer review
Editorially reviewed, not externally peer-reviewed.
Acknowledgements
This report was approved by the ethical committee of our institution. Written, informed consent was obtained from the patient, and patient anonymity was preserved.
We thank Dr. Satoshi Nojima and Dr. Shinnichiro Tahara for their clinical treatments and helpful supports.
References
- 1.Yasuhiro T., Tetsuya K., Kazuhiro Y., Hideyuki K., Katsuhiko Y. Successful neoadjuvant imatinib mesylate followed by anus-preserving laparoscopic surgery for lower rectal gastrointestinal stromal tumor (GIST): a case report. J. Jpn. Soc. Coloproctol. 2016;69:221–226. [Google Scholar]
- 2.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 3.Miettinen M., Lasota J. Gastrointestinal stromal tumors (GISTs): definition, occurrence, pathology, differential diagnosis and molecular genetics. Pol. J. Pathol. 2003;54:3–24. [PubMed] [Google Scholar]
- 4.Tielen R., Verhoef C., van Coevorden F., Reyners A.K., van der Graaf W.T., Bonenkamp J.J. Surgical management of rectal gastrointestinal stromal tumors. J. Surg. Oncol. 2013;107:320–323. doi: 10.1002/jso.23223. [DOI] [PubMed] [Google Scholar]
- 5.Cavnar M.J., Wang L., Balachndran V.P., Antonescu C.R., Tap W.D., Keohan M. Rectal gastrointestinal stromal tumor (GIST) in the era of imatinib: organ preservation and improved oncologic outcome. Ann. Surg. Oncol. 2017;24:3972–3980. doi: 10.1245/s10434-017-6087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jakob J., Mussi C., Ronellenfitsch U., Wardelmann E., Negri T., Gronchi A. Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of Imatinib. Ann. Surg. Oncol. 2013;20:586–592. doi: 10.1245/s10434-012-2647-1. [DOI] [PubMed] [Google Scholar]
- 7.Wilkinson M.J., Fitzgerald J.E., Strauss D.C., Hayes A.J., Thomas J.M., Messiou C. Surgical treatment of gastrointestinal stromal tumor of the rectum in the era of imatinib. Br. J. Surg. 2015;102:965–971. doi: 10.1002/bjs.9818. [DOI] [PubMed] [Google Scholar]
- 8.ESMO/European Sarcoma Network Working Group Gastrointestinal stromal tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2014;25:321–326. doi: 10.1093/annonc/mds252. [DOI] [PubMed] [Google Scholar]
- 9.Kaneko M., Nozawa H., Emoto S., Murono K., Sasaki K., Otani K. Neoadjuvant Imatinib therapy followed by intersphincteric resection for low rectal gastrointestinal stromal tumors. Anticancer Res. 2017;37:5155–5160. doi: 10.21873/anticanres.11936. [DOI] [PubMed] [Google Scholar]
- 10.Fujimoto Y., Akiyoshi T., Konishi T., Nagayama S., Fukunaga Y., Ueno M. Laparoscopic sphincter-preserving surgery (intersphincteric resection) after neoadjuvant Imatinib treatment for gastrointestinal stromal tumor (GIST) of the rectum. Int. J. Colorectal Dis. 2014;29:111–116. doi: 10.1007/s00384-013-1769-7. [DOI] [PubMed] [Google Scholar]