Abstract
Background
Transcatheter mitral valve repair and replacement (TMVR) is a minimally invasive alternative to conventional open-heart mitral valve replacement (OMVR). The present study aims to compare the burden, demographics, cost, and complications of TMVR and OMVR.
Methods
The United States National Inpatient Sample (US-NIS) for the year 2017 was queried to identify all cases of TMVR and OMVR. Categorical and continuous data were analyzed using Pearson chi-square and independent t-test analysis, respectively. An adjusted odds ratio (aOR) based on the ordinal logistic regression (OLR) model was calculated to determine the association between outcome variables.
Results
Of 19,580 patients, 18,460 (94%) underwent OMVR and 1120 (6%) TMVR. Mean ages of patients were 63 ± 14 years (OMVR) and 67 ± 13 years (TMVR). Both cohorts were predominantly Caucasian (73% OMVR vs. 74.0% TMVR). The patients who underwent TMVR were more likely to belong to a household with an income in the highest quartile (26.1% vs. 22.0% for OMVR) versus the lowest quartile (22.1% vs. 27.8%). The average number of days from admission to TMVR was less compared to OMVR (2.63 days vs. 3.02 days, p = 0.015). In-hospital length of stay (LOS) was significantly lower for TMVR compared to OMVR (11.56 vs. 14.01 days, p=<0.0001). Adjusted in-hospital mortality taking into account comorbidities showed no significant difference between the two groups (OR 1.2, 0.93–1.68, p = 0.15).
Conclusion
Patients undergoing TMVR were older and more financially affluent. TMVR was more costly but was associated with a shorter hospital stay and similar mortality to OMVR.
Keywords: Mitral valve regurgitation, Valve surgery, TMVR
1. Introduction
Transcutaneous mitral valve repair (TMVR) has recently emerged as an alternative to open mitral valve repair (OMVR). [1] An edge-to-edge mitral leaflet repair device (the MitraClip) is currently the only US Food and Drug Administration (FDA) approved non-surgical device for mitral regurgitation. This transcatheter technology involves clipping together the middle segments of the anterior and posterior mitral valve leaflets, thereby reducing the regurgitant area by creating a “double orifice” mitral valve [1]. The anterior and posterior mitral valve leaflets are grasped together with a cobalt-chromium clip covered with polypropylene fabric, thereby reducing mitral regurgitant backflow [2].
Individuals with multiple co-morbidities and at high surgical risks, who are not suitable candidates for OMVR, may benefit from TMVR. TMVR is associated with lower procedural and postoperative complications [1]. TMVR resulted in better preservation of ventricular function and decreased the need for anticoagulant use [2]. In some cases, this procedure needs to be repeated if the regurgitant flow remains high [3]. In-hospital complications occur in up to 13% of patients; mostly major bleeding in 7.4% patients, and stroke and myocardial infarction in < 1% cases [3]. Earlier studies have linked TMVR with a higher mortality rate. This can be attributed to the complex anatomy of the mitral valve; and the fact that mitral valve replacement or repair affects cardiac function and physiology, regardless of the method used to fix the mitral valve [4]. Complications mainly occurred in older patients who were critically ill prior to intervention [3].
Despite an increase in patients undergoing TMVR as alternative management to OMVR, there is limited literature on this topic [5]. The present study aims to compare the burden, demographics, cost, and complications of TMVR and OMVR.
2. Methods
2.1. Source of data
The National Inpatient Sample (NIS) database for the year 2017 was systematically searched using international classification of diseases, 10th revision (ICD-10) coding. The NIS is the largest accessible dataset, which contains a 20% sample of all discharges from>4000 United States (US) hospitals [6]. The total unweighted sample comprises 7 million nationwide discharges. Due to the anonymous nature of data, NIS does not require approval from the institutional review board (IRB). The Healthcare Cost and Utilization Project (HCUP) provides detailed information about the NIS database.
2.2. Study population
The included study population had to meet all of the following inclusion criteria: 1) Age > 18 years, male or female; 2) patients who underwent OMVR or TMVR for any indication of valvular pathology; 3) sufficient clinical and demographic data available for comparison. All patients age less that under 18 years of age, or who underwent procedure than OMVR or TMVR were excluded.
The NIS database between duration October 2016 to September 2017 meeting procedure coding system (PCS) codes 02QG0Z and 02QG3Z for OMVR and TMVR, respectively were selected. The PCS is a US cataloging system for procedural codes that track various open and transcutaneous interventions. The associated co-morbidities and procedures were identified using the standardized ICD-10 clinical modification (ICD-10-CM) and ICD-10-PCS.
2.3. Study outcomes
Baseline demographics, age, admitting diagnosis, hospital-level characteristics, co-morbidities and concomitant procedures between OMVR and TMVR were compared. Primary endpoints were in-hospital mortality, and procedure and hospital cost in US dollars ($). Secondary outcomes included mean length of hospital stay and trends of procedure preference in terms of patient demographics and socioeconomic status.
2.4. Statistical analyses
The set discharge weight (DISCWT) provided by the NIS database was applied to all variables to generate national estimates. Categorical variables were assessed using the Pearson Chi-square test and independent student’s t-tests were used for comparing continuous variables between OMVR and TMVR groups. A multivariate analysis based on the ordinal logistic regression model (OLR) was used to calculate odds ratios (aOR) adjusted for possible covariates including age, race, sex, elective-non-elective, median household income, admission type, length of stay, hospital bed size, location/teaching status of the hospital and all baseline co-morbidities. An alpha criterion of<0.05 was used as a cutoff for statistical significance. The analysis was performed using IBM SPSS Statistics 22.0 (IBM Corp, Armonk, New York).
3. Results:
3.1. Baseline characteristics of the study population
A total of 19,580 patients who underwent MVR were identified. Of these, 18,460 (94%) underwent OMVR and 1120 (6%) had TMVR. The mean age of patients who underwent OMVR was 62.7 ± 15.3 years, significantly younger by 7.91 years ± 0.53 (p=<0.0001) compared to TMVR (70.65 ± 13.17 years). Both cohorts consisted predominantly of Caucasian patients (73% OMVR versus 74.0% TMVR), followed by African American (12% versus 11%), Hispanic (7% versus 6%), and Asian (2% versus 2%). Baseline study demographics are shown in Table 1.
Table 1.
Showing baseline demographics, co-morbidities, procedural complications.
| Analyte | TMVR | OMVR |
|---|---|---|
| Demographics | ||
| Sample n (%) | 1120 (6%) | 18,460 (94%) |
| Age with range (years) | 62.7 ± 15.3 | 70.65 ± 13.17 years |
| Males n (%) | 330 (29.4%) | 6920 (37.4%) |
| Females n (%) | 520 (46.4%) | 8375 (45.3%) |
| Caucasians | 74% | 73.00% |
| African Americans | 11% | 12% |
| Others race | 8% | 9% |
| Median household Income 1st Quartile: 1–43,999$ n (%) | 245 (22.1%) | 5020 (27.8%) |
| MHI 2nd Quartile: 44,000–55,999$ (n%) | 315 (28.4%) | 4735 (26.2%) |
| MHI 3rd Quartile: 56,000–73,999$ n (%) | 260 (23.4%) | 4320 (23.9%) |
| MHI 4th Quartile: >74,000$ n (%) | 290 (26.1%) | 3965 (22.0%) |
| New admission for sole purpose of procedure n (%) | 880 (78.6%) | 15,700 (85.3%) |
| Transfer in from acute facility n (%) | 210 (18.8%) | 2345 (12.7%) |
| Transfer in from non-acute facility n (%) | 30 (2.7%) | 370 (2.0%) |
| No transfer out to other facility n (%) | 825(73.7%) | 12705(68.8%) |
| Transfer to acute care facility n (%) | 5 (0.4%) | 260 (1.4%) |
| Transfer out to non-acute care facility n (%) | 290 (25.9%) | 5490 (29.7%) |
| Baseline Comorbidities n (%) | ||
| Hypertensive heart disease with heart failure I110 | 25 (2.2%) | 200 (1.1%) |
| Hypertension and chronic kidney disease I-V | 25 (2.2%) | 290 (2.3%) |
| Rheumatic valvular disease | 170 (14%) | 6175 (33.4%) |
| Nonrheumatic valvular disease | 275 (24.5%) | 5980 (32.5%) |
| Procedural Characteristics | ||
| Number of Days from admission to procedure | 2.6 ± 4.5 | 3 ± 5 |
| Length of hospital stay (days) | 11.5 ± 10 | 14 ± 12.7 |
| Total Cost ($) | 318,882 | 38,341 |
| Procedural Complications n (%) | ||
| Sepsis due to MSSA | 10 (0.9%) | 140 (0.8%) |
| Sepsis secondary to other strep and staph | – | 240 (1.3%) |
| Sepsis secondary to gram negative infection and candida | – | 200 (1.08%) |
| Acute and subacute infective endocarditis | 45 (4%) | 900 (4.9%) |
| Atrial fibrillation | 10 (0.8%) | 85 (0.5%) |
| STEMI | 20 (1.7%) | 120(0.7%) |
| NSTEMI | 50 (4.5%) | 455 (2.5%) |
| Heart Failure | 125 (1.1%) | |
| Leakage/mechanical complication of prosthesis | 100 (8.9%) | 315 |
| Infection/thrombosis of prosthesis/other complications | 260 (23.2%) | 1215 |
3.2. Baseline comorbidities of the study population
The most common indications for valve replacement in the OMVR and TMVR groups were nonrheumatic mitral valve insufficiency (29.2% vs. 20.5%) followed by rheumatic mitral stenosis (5.1% vs. 5.4%). In addition to mitral valve involvement, OMVR patients had associated additional valvular lesions, including rheumatic disorder of tricuspid valves (9.0%), rheumatic stenosis of aortic valves (8.4%), and combined rheumatic disorders of aortic and tricuspid valves (5.1%). Multiple valvular lesions justified the need for open-heart surgery to have concomitant valvular replacements. The baseline comorbidities, and indications are shown in table 1 and table 2 respectively.
Table 2.
Showing indications of OMVR and TMVR with sample frequency and percentages.
| ICD-10 CODE and indication for the procedure | OMVR | % | TMVR | % |
|---|---|---|---|---|
| Nonrheumatic mitral (valve) insufficiency (I340) | 5385 | 29.20% | 230 | 20.50% |
| Rheumatic disorders of both mitral and tricuspid valves (I081) | 1660 | 9.00% | 25 | 2.20% |
| Rheumatic disorders of both mitral and aortic valves (I080) | 1545 | 8.40% | 25 | 2.20% |
| Rheumatic mitral stenosis with insufficiency (I052) | 950 | 5.10% | 60 | 5.40% |
| Rheumatic mitral stenosis (I050) | 675 | 3.70% | 25 | 2.20% |
| Nonrheumatic mitral (valve) insufficiency (I340) | 5385 | 29.20% | 230 | 20.50% |
| Stenosis of other cardiac prosthetic devices, implants and grafts, initial encounter (T82857A) | 570 | 3.10% | 195 | 17.40% |
| Rheumatic mitral stenosis with insufficiency (I052) | 950 | 5.10% | 60 | 5.40% |
| Non-ST elevation myocardial infarction (NSTEMI) (I214) | 455 | 2.50% | 50 | 4.50% |
| Acute and subacute infective endocarditis (I330) | 900 | 4.90% | 45 | 4% |
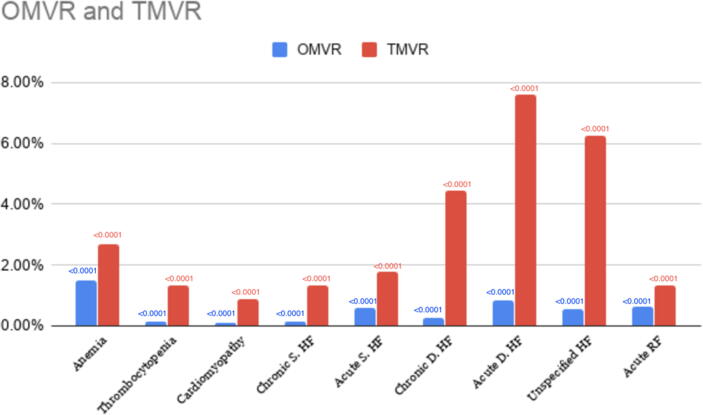
In the TMVR cohort, 4.5% of patients had non-ST segment elevation myocardial infarction (NSTEMI), and 4.0% of patients had acute or subacute infective endocarditis on presentation. Patients in the TMVR group had significantly higher percentages of respiratory failure, heart failure, anemia, thrombocytopenia and cardiomyopathy (p=<0.0001). (Fig. 1)
Fig. 1.
Baseline comorbidities of patients across TMVR and OMVR. p-values shown on top of each bar chart represent statistically significant distribution among both groups for all comorbidities.
3.3. Hospital-based characteristics and Outcomes:
Average number of days from admission to the TMVR procedure was 2.63 days, significantly lower compared to the OMVR group (3.02 days, p = 0.015). The average in-hospital LOS was also markedly lower by 0.388 days for the TMVR group compared to the OMVR group (11.56 vs. 14.01 days, p=<0.0001). (Table 1; Table 3) The mean cost for TMVR was $383,401, which was significantly higher compared to OMVR ($318,882; p < 0.0001) (Table 3). The patients who underwent TMVR were more likely to belong to a household with an income in the highest 4th quartile (26.1% vs. 22.0%) and less likely to be in the lowest 1st quartile (22.1% vs. 27.8%).
Table 3.
Clinical outcomes of continuous variables between patients undergoing OMVR vs. TMVR.
| Characteristic | OMVR | TMVR | Mean difference | SE | T-test | p-value |
|---|---|---|---|---|---|---|
| Total charges (US$) | 318,882 | 383,401 | −64518 | 8254 | −7.8 | <0.0001 |
| Admission to procedure (days) | 3.02 | 2.63 | 0.397 | 0.163 | 2.4 | 0.015 |
| Length of stay (days) | 14.01 | 11.56 | 2.448 | 0.388 | 6.3 | <0.0001 |
Abbreviations: OMVR: Open mitral valve replacement; TMVR: Transcatheter mitral valve replacement.
Approximately 7% of TMVR patients, and 9% of OMVR patients were admitted on the weekend. Sixty three percent of TMVR patients and 64% of OMVR patients underwent an elective procedure. The adjusted odds for weekend admissions (OR 0.814, 95% CI 0.622–1.065, p = 0.15) and elective procedure (OR 1.005, 95% CI 0.870–1.161, p = 0.973) were not significantly different between groups. (Table 4)
Table 4.
Clinical outcomes of categorical variables between patients undergoing OMVR vs. TMVR.
| Characteristics | OMVR | TMVR | Chi-Square | P-value |
|---|---|---|---|---|
| Mortality Rate % (deaths/total procedure) | 5.3% (985/18455) | 13.4% 150/112 | 125.44 | 0.00 |
| Elective Vs non-elective procedure | 11485/18370. 62.50% | 575/1120 51.30% | 55.947 | 0.00 |
Abbreviations: OMVR: Open mitral valve replacement; TMVR: Transcatheter mitral valve replacement.
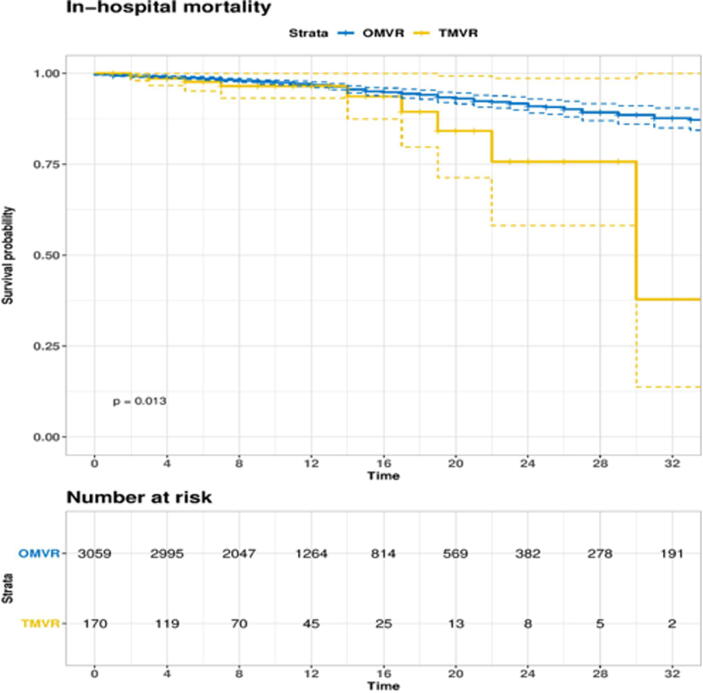
In-hospital mortality was significantly higher for the TMVR group at 13.4%, as compared to the OMVR group at 5.3% (p = 0.013). However, the adjusted odds of in-hospital mortality taking into co-morbidities showed no significant difference between the two groups (OR 1.2, 0.93–1.68, p = 0.15). (Table 4) The survival analysis of TMVR and OMVR is shown in Kaplan-Meier curve in Fig. 2. The subgroup analysis showed similar mortality across both genders in OMVR. The mortality review among subgroups were more prevalent in OMVR with organ failure, and the most common complication were respiratory failure, hepatic failure, acute kidney injury and heart failure. Further subgroup difference of mortality in terms of race, gender, and complications are shown in table 5.
Fig. 2.
Kaplan Meir Curve showing in-hospital mortality of OMVR and TMVR.
Table 5.
Showing Mortality differences across subgroups of Race, Gender, and Complications.
| Variable | OMVR | TMVR |
|---|---|---|
| Race n (%) | ||
| White | 585 (94.4%) | 35 (5.60%) |
| Black | 65(86.70%) | 10(13.30%) |
| Hispanics | 20(100.00%) | <1% |
| Asian | 30 (100.0%) | <1% |
| Others | 5(50.00%) | 5(50.00%) |
| Gender Differences n (%) | ||
| Male | 345(93.2%) | 25 (6.8%) |
| Female | 380(93.8%) | 25(6.2%) |
| Complications n (%) | ||
| Respiratory failure with hypoxia | 125(17.24%) | <1% |
| Hepatic Failure | 70(9.66%) | <1% |
| AKI | 65(8.97%) | <1% |
| Heart Failure | 60(8.27%) | <1% |
| Cardiogenic Shock | 45(6.20%) | <1% |
| Sepsis | 30 (4%) | <1% |
| Acute post hemorrhagic anemia and DIC | 30(4%) | <1% |
| STEMI | 25(3.4%) | <1% |
| Acute and subacute endocarditis | 20(2.75%) | 20(40%) |
| ESRD | 20(2.75%) | <1% |
| Papillary Muscle rupture | 15(2.06%) | <1% |
| NSTEMI | 10(1.3%) | <1% |
4. Discussion:
The main findings of this study are: (1) Patients with TMVR had a higher socioeconomic status and were older compared to OMVR. (2) TMVR patients had a lower in-hospital stay and had a shorter admission to procedure time. (3) The unadjusted in-hospital mortality odds were higher for TMVR patients. However, there was no significant difference between the two groups when the odds of mortality were adjusted based on co-morbidities. (4) Patients undergoing TMVR did not differ significantly from OMVR in terms of admission day (weekday vs. weekend) and procedure type (emergent vs. elective).
TMVR offers a less invasive approach and quicker recovery compared to OMVR for eligible patients with mitral regurgitation [3]. A team of specialists is involved in determining the eligibility for TMVR and requires an elaborate screening protocol [4]. Patients with isolated mitral valve disease would benefit the most from TMVR, while OMVR is preferred in patients with multiple valvular lesions or having a concomitant coronary artery disease [3]. Additionally, the complexity of mitral anatomy, device-related factors, physician’s discretion and expertise also plays a role in decision making. Being a relatively novel approach with limited evidence, reported experience on TMVR outcome is limited; consequently, even skilled physicians may opt to perform OMVR on patients with complex mitral lesions [3], [4]. The commercially available device design (MitraClip) may limit application in the comorbid, dynamic environment of the mitral annulus. To size and position these devices on asymmetrical and saddle-shaped mitral annulus could be challenging [7]. Similarly, calcified and rheumatic mitral disease repaired by TMVR may produce suboptimal results as they may pose an increased risk of left ventricular outflow tract obstruction, late device detachment, and paravalvular leakage [8]. These potential complications are weighed against the surgical risk of OMVR to decide about the appropriate intervention.
This study showed that patients undergoing TMVR were relatively older by a mean age of about eight years compared to patients undergoing OMVR. These findings were consistent with the results of previous studies (Vassileva et al., and Del Val et al.), where the mean age of patients undergoing TMVR was approximately 75 years compared to 50 years for patients undergoing OMVR [9], [10]. TMVR, thus, presents itself as a safer alternative in patients with advanced age where frailty, multiple co-morbidities and stress intolerance renders them at high risk for open surgery [11].
This study also found that TMVR was more frequently performed in patients with higher socioeconomic status compared to patients undergoing OMVR. There was no statistically significant difference demonstrated between patients admitted on weekdays vs. weekends or patients undergoing emergent vs. elective procedure. TMVR patients had a shorter overall in-hospital length of stay, yet the mean cost for overall TMVR related hospitalization was significantly higher compared to OMVR. Continued advancement in procedural technique and increasing availability of the TMVR devices will reduce its cost in the future. A patient-level economic analysis in the context of its long-term benefits is required to determine its financial implications.
The adjusted mortality odds in patients undergoing TMVR was not significantly different from patients undergoing OMVR. On the contrary, in a multicenter, retrospective study by Guerrero et al., the 30-day and 1-year all-cause mortality associated with TMVR was 25% and 53.7%, respectively [12]. Elbadawi et al. also reported about 2% overall in-hospital mortality in patients with TMVR compared to 6% for patients undergoing OMVR [6]. This mortality rate was found to be directly correlated with the degree of mitral regurgitation and left ventricular dysfunction [13], [14]. Our unadjusted analysis showed a significantly higher in-hospital mortality for patients undergoing TMVR compared to the OMVR (13.4% vs. 5.3%, respectively). When adjusted for the relatively sicker populations in the TMVR group, there was no significant difference in the mortality odds of the two groups. This indicates that TMVR has potentially equal efficacy as OMVR and could be a viable option for patients with multiple comorbidities.
5. Limitations:
Due to the retrospective cross-sectional and nonrandomized nature of the data, this study is subject to the selection bias, confounding bias, and also failure to associate definitive causation. Furthermore, due to cross sectional nature of the study, the time wise long-term graphical presentation of Kaplan Meier curve was not possible. The reported findings merely represent an association between different variables and inferences drawn about the incidence of the outcomes could be misleading.
6. Conclusion:
TMVR appears to be an attractive alternative to OMVR due to a significantly lower hospital stay, admission to procedure time and an identical risk of mortality. The associated cost with TMVR was high and more studies are needed to determine the cost-benefit analysis.
Disclosures: none
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100540.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Ramlawi B., Gammie J.S. Mitral valve surgery: current minimally invasive and transcatheter options. Methodist DeBakey cardiovascular journal. 2016 Jan;12(1):20. doi: 10.14797/mdcj-12-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vahanian A, Alfieri O, Andreotti F. Guidelines on the management of valvular heart disease (version 2012) Eur Heart J. 2012 Oct;33(19):2451–96. et al.; Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS) [DOI] [PubMed]
- 3.Eggebrecht H., Schelle S., Puls M., Plicht B., von Bardeleben R.S., Butter C., May A.E., Lubos E., Boekstegers P., Ouarrak T., Senges J. Risk and outcomes of complications during and after MitraClip implantation: experience in 828 patients from the German TRAnscatheter mitral valve interventions (TRAMI) registry. Catheterization and Cardiovascular Interventions. 2015 Oct;86(4):728–735. doi: 10.1002/ccd.25838. [DOI] [PubMed] [Google Scholar]
- 4.De Backer O., Piazza N., Banai S. Percutaneous transcatheter mitral valve replacement: an overview of devices in preclinical and early clinical evaluation. Circ Cardiovasc Interv. 2014;7:400–409. doi: 10.1161/CIRCINTERVENTIONS.114.001607. [DOI] [PubMed] [Google Scholar]
- 5.von Ballmoos M.C., Kalra A., Reardon M.J. Complexities of transcatheter mitral valve replacement (TMVR) and why it is not transcatheter aortic valve replacement (TAVR) Annals of cardiothoracic surgery. 2018 Nov;7(6):724. doi: 10.21037/acs.2018.10.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healthcare cost and utilization project (HCUP) database overview of the national (nationwide) inpatient sample. 2020. https://www.hcup-us.ahrq.gov/nisoverview.jsp
- 7.Elbadawi A., Elgendy I.Y., Mohamed A., Almahmoud M.F., Omer M.A., Abuzaid A.S., Denktas A.E., Paniagua D., Banerjee S., Jneid H. Temporal Trends and Outcomes of Transcatheter Mitral Valve Repair and Surgical Mitral Valve Interventions. Circulation. 2019;140(Suppl_1):A13941. doi: 10.1016/j.carrev.2020.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Mangieri Antonio, Laricchia Alessandra, Giannini Francesco, Gallo Francesco, Kargoli Faraj, Ladanyi Annamaria, Testa Luca, Colombo Antonio, Latib Azeem. Emerging Technologies for Percutaneous Mitral Valve Repair. Front. Cardiovasc. Med. 2019;6 doi: 10.3389/fcvm.2019.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.del Val D., Ferreira-Neto A.N., Wintzer-Wehekind J., Dagenais F., Paradis J.M., Bernier M., O'Connor K., Beaudoin J., Freitas-Ferraz A.B., Rodés-Cabau J. Early experience with transcatheter mitral valve replacement: a systematic review. Journal of the American Heart Association. 2019 Sep 3;8(17) doi: 10.1161/JAHA.119.013332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vassileva C.M., Boley T., Markwell S., Hazelrigg S. Meta-analysis of short-term and long-term survival following repair versus replacement for ischemic mitral regurgitation. European journal of cardio-thoracic surgery. 2011 Mar 1;39(3):295–303. doi: 10.1016/j.ejcts.2010.06.034. [DOI] [PubMed] [Google Scholar]
- 11.Messika-Zeitoun D., Nickenig G., Latib A., Kuck K.H., Baldus S., Schueler R. Transcatheter mitral valve repair for functional mitral regurgitation using the cardioband system: 1 year outcomes. Eur Heart J. 2019;40:466–472. doi: 10.1093/eurheartj/ehy424. [DOI] [PubMed] [Google Scholar]
- 12.Guerrero M, Rihal C. Taking transcatheter mitral valve replacement to the next level. [DOI] [PubMed]
- 13.Baron S.J., Wang K., Arnold S.V., Magnuson E.A., Whisenant B., Brieke A., Rinaldi M., Asgar A.W., Lindenfeld J., Abraham W.T., Mack M.J. Cost-effectiveness of transcatheter mitral valve repair versus medical therapy in patients with heart failure and secondary mitral regurgitation: results from the COAPT Trial. Circulation. 2019 Dec 3;140(23):1881–1891. doi: 10.1161/CIRCULATIONAHA.119.043275. [DOI] [PubMed] [Google Scholar]
- 14.Seeburger J., Raschpichler M., Garbade J., Davierwala P., Pfannmueller B., Borger M.A. Minimally invasive mitral valve surgery in octogenarians-a brief report. Ann Cardiothorac Surg. 2013;2:765–767. doi: 10.3978/j.issn.2225-319X.2013.10.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.