Abstract
We reviewed the literature concerning the innate response from nasal and oral epithelial cells and their reaction to hydrogen peroxide (H2O2). Hydrogen peroxide is produced physiologically by oral bacteria and plays a significant role in the balance of oral microecology since it is an important antimicrobial agent. In the epithelial cells, the enzyme superoxide dismutase catalyzes a reaction leading from hydrogen peroxide to the ion superoxide. The induced oxidative stress stimulates a local innate response via activation of the toll-like receptors and the NF-κB. Those kinds of reactions are also activated by viral infections. Virus-induced oxidative stress plays an important role in the regulation of the host immune system and the specific oxidant-sensitive pathway is one of the effective strategies against viral infections. Therefore, nose/mouth/throat washing with hydrogen peroxide may enhance those local innate responses to viral infections and help protect against the current coronavirus pandemic. We strongly encourage the rapid development of randomized controlled trials in both SARS-CoV-2 positive and negative subjects to test the preliminary findings from the in-vitro and in-vivo observational studies that we identified.
Keywords: Hydrogen peroxide, Innate immunity, Viruses, Coronavirus, COVID-19, SARS-CoV-2
Introduction
The current coronavirus outbreak appears to be characterized by respiratory transmission and respiratory infection, although the routes of transmission and the pathophysiology of the disease have not been fully clarified yet. However, it is proven that the virus resides in the nasal and oral mucosa [1].
While impeding person-to-person transmission is key to limiting the outbreak, so far little importance has been given to the events taking place after a transmission has happened, when innate immunity plays a crucial role. The main purpose of the innate immune response is to immediately prevent the spread and movement of foreign pathogens throughout the body. There is a close interplay between innate immunity and oxidative stress, and the molecule hydrogen peroxide may play a central role [2].
We reviewed the literature concerning the innate response from nasal and oral epithelial cells to evaluate the role of hydrogen peroxide (H2O2).
Methods
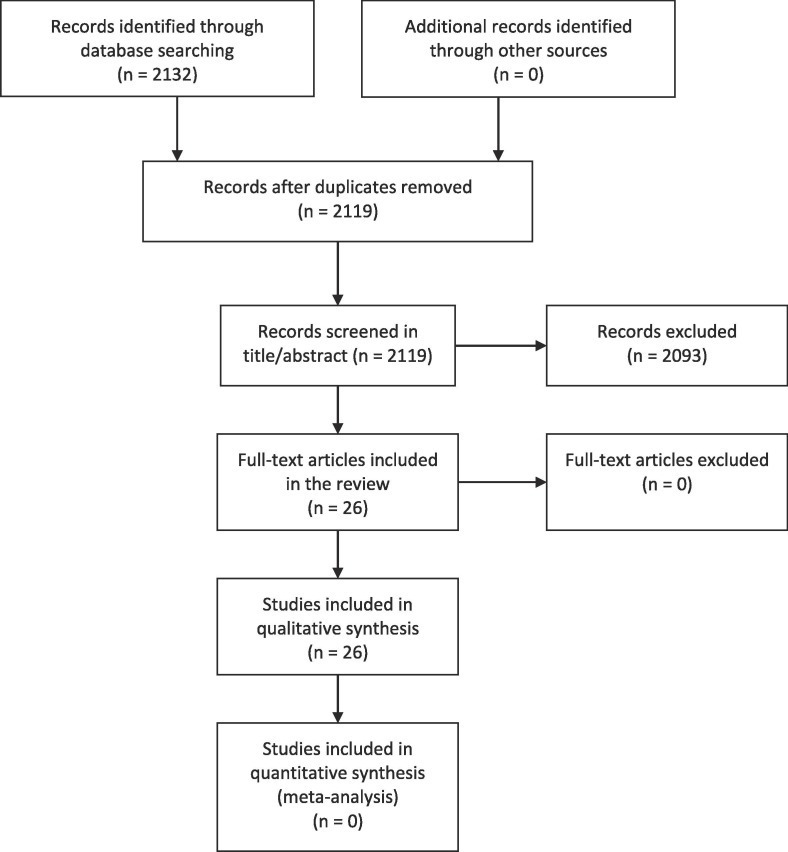
We searched the databases EMBASE and PubMed for relevant papers using the following entry terms: (“hydrogen peroxide” OR H2O2) AND (virus OR viral infection OR innate response). We have not used any other constrains. After duplicates were removed, we identified 2119 papers. Two independent observers scrutinized those articles in their titles and abstracts to apply eligibility criteria and filter the relevant ones. Disagreements were resolved by discussion. We defined the eligibility criteria using a PICO model as follows. Population: no specific reference population. Intervention: administration of hydrogen peroxide within clinical studies or animal studies or in-vitro studies. Comparison: placebo controlled or intra-individual pre-post comparison. Outcome: duration of current viral infection or protection against viral infections or enhancement of innate immunity reactions. All references from all eligible articles were assessed for eligibility, with no success. Finally, the papers were read, criticized, and narratively summarized. Fig. 1 shows a flow chart of the literature screening method used.
Fig. 1.
Systematic review flow diagram.
Results
26 Papers resulted eligible for review (Figure 1), none of which was a randomized controlled trial or a clinical observational study with a control group.
Hydrogen peroxide is produced physiologically by oral bacteria and plays a significant role in the balance of oral microecology since it is an important antimicrobial agent [3]. In the epithelial cells, the enzyme superoxide dismutase catalyzes a reaction leading from hydrogen peroxide to the ion superoxide. The induced oxidative stress stimulates a local innate response via activation of the toll-like receptors and the NF-κB [4]. Those kinds of reactions are also activated by viral infections [5]. Virus-induced oxidative stress plays an important role in the regulation of the host immune system and the specific oxidant-sensitive pathway is one of the effective strategies against viral infections [6], [7], [8].
Many viruses have been found to be sensitive to hydrogen peroxide, including swine flu, rubella, rabies, and others [7], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21].
We therefore hypothesize that nose and mouth washing with hydrogen peroxide may enhance those local innate responses to viral infections and help protect against viral infections, including the current coronavirus pandemic.
Moreover, a hydrogen peroxide solution of a concentration as little as 0.5% efficiently inactivates coronaviruses (e.g. SARS, MERS) on inanimate surfaces within 1 min [22]. This may justify the use of hydrogen peroxide washes in infected people too: the solution may decrease the viral load of their respiratory droplets, hence help tackle the spread in the community.
In the British Nationally Formulary, H2O2 is indicated for oral hygiene at the concentration of 6%. Hydrogen peroxide is safe to use for gargling or as a nasal spray: its 3% solution is commonly used off-label in otolaryngology to treat many viral conditions [23], [24], [25], [26], and moderate concentrations are present in drinks including tea and instant coffee [27].
Conclusions
There are no randomized controlled trials or clinical observational studies concerning the curative or preventive effect of hydrogen peroxide against viral infections. However, the literature from in-vitro immunological studies clearly points out that the application of hydrogen peroxide on the epithelial cells of nose, throat and mouth may well be extremely effective against viruses, including coronaviruses. We strongly encourage the rapid development of randomized controlled trials in both SARS-CoV-2 positive and negative subjects to study the effects that we have hypothesized. Those trials would be inexpensive to implement and compatible with other ongoing trials. Positive results would lead to remarkable global health gain with extremely limited costs. As a starting dose to test, we propose two puffs (about 0.28 ml) of 1.5% H2O2 nasal spray into each nostril two times daily combined with a mouth wash and gargling for 1 min with a 3% H2O2 solution two times daily.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors received no funding from any source. All authors contributed to the conception of the study. AIL wrote the manuscript. All authors approved the manuscript before submission.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mehy.2020.109910.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Y., Zhou Z., Min W. Mitochondria, Oxidative Stress and Innate Immunity. Front Physiol. 2018;9:1487. doi: 10.3389/fphys.2018.01487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keke Z., Xuedong Z., Xin X. The origin of hydrogen peroxide in oral cavity and its role in oral microecology balance. Hua Xi Kou Qiang Yi Xue Za Zhi. 2017;35:215–220. doi: 10.7518/hxkq.2017.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang M., Lu M., Zhang C., Wu X., Chen J., Lv W. Oxidative stress modulates the expression of toll-like receptor 3 during respiratory syncytial virus infection in human lung epithelial A549 cells. Mol Med Rep. 2018 doi: 10.3892/mmr.2018.9089. [DOI] [PubMed] [Google Scholar]
- 5.To E.E., Broughton B.R.S., Hendricks K.S., Vlahos R., Selemidis S. Influenza A virus and TLR7 activation potentiate NOX2 oxidase-dependent ROS production in macrophages. Free Radic Res. 2014;48:940–947. doi: 10.3109/10715762.2014.927579. [DOI] [PubMed] [Google Scholar]
- 6.Liu M., Chen F., Liu T., Chen F., Liu S., Yang J. The role of oxidative stress in influenza virus infection. Microbes Infect. 2017;19:580–586. doi: 10.1016/j.micinf.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Zobel S, Lorenz M, Frascaroli G, Böhnke J, Bilz NC, Stanifer ML, et al. Rubella Virus Strain-Associated Differences in the Induction of Oxidative Stress Are Independent of Their Interferon Activation. Viruses 2018;10. https://doi.org/10.3390/v10100540. [DOI] [PMC free article] [PubMed]
- 8.Aizawa H., Koarai A., Shishikura Y., Yanagisawa S., Yamaya M., Sugiura H. Oxidative stress enhances the expression of IL-33 in human airway epithelial cells. Respir Res. 2018;19:52. doi: 10.1186/s12931-018-0752-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abd-Elghaffar A.A., Ali A.E., Boseila A.A., Amin M.A. Inactivation of rabies virus by hydrogen peroxide. Vaccine. 2016;34:798–802. doi: 10.1016/j.vaccine.2015.12.041. [DOI] [PubMed] [Google Scholar]
- 10.Cusinato R., Pacenti M., Martello T., Fattori P., Morroni M., Palù G. Effectiveness of hydrogen peroxide and electron-beam irradiation treatment for removal and inactivation of viruses in equine-derived xenografts. J Virol Methods. 2016;232:39–46. doi: 10.1016/j.jviromet.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Lei R., Du Z., Qiu Y., Zhu S. The detection of hydrogen peroxide involved in plant virus infection by fluorescence spectroscopy. Luminescence. 2016;31:1158–1165. doi: 10.1002/bio.3090. [DOI] [PubMed] [Google Scholar]
- 12.Chan S.-W. Hydrogen peroxide induces La cytoplasmic shuttling and increases hepatitis C virus internal ribosome entry site-dependent translation. J Gen Virol. 2016;97:2301–2315. doi: 10.1099/jgv.0.000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zonta W., Mauroy A., Farnir F., Thiry E. Virucidal efficacy of a hydrogen peroxide nebulization against murine norovirus and feline calicivirus, two surrogates of human norovirus. Food Environ Virol. 2016;8:275–282. doi: 10.1007/s12560-016-9253-5. [DOI] [PubMed] [Google Scholar]
- 14.Hole K., Ahmadpour F., Krishnan J., Stansfield C., Copps J., Nfon C. Efficacy of accelerated hydrogen peroxide® disinfectant on foot-and-mouth disease virus, swine vesicular disease virus and Senecavirus A. J Appl Microbiol. 2017;122:634–639. doi: 10.1111/jam.13361. [DOI] [PubMed] [Google Scholar]
- 15.Holtkamp D.J., Myers J., Thomas P.R., Karriker L.A., Ramirez A., Zhang J. Efficacy of an accelerated hydrogen peroxide disinfectant to inactivate porcine epidemic diarrhea virus in swine feces on metal surfaces. Can J Vet Res. 2017;81:100–107. [PMC free article] [PubMed] [Google Scholar]
- 16.Hyodo K., Suzuki N., Mise K., Okuno T. Roles of superoxide anion and hydrogen peroxide during replication of two unrelated plant RNA viruses in Nicotiana benthamiana. Plant Signal Behav. 2017;12 doi: 10.1080/15592324.2017.1338223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker K.L., Thomas P.R., Karriker L.A., Ramirez A., Zhang J., Wang C. Evaluation of an accelerated hydrogen peroxide disinfectant to inactivate porcine epidemic diarrhea virus in swine feces on aluminum surfaces under freezing conditions. BMC Vet Res. 2017;13:372. doi: 10.1186/s12917-017-1300-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sassi H.P., Reynolds K.A., Pepper I.L., Gerba C.P. Evaluation of hospital-grade disinfectants on viral deposition on surfaces after toilet flushing. Am J Infect Control. 2018;46:507–511. doi: 10.1016/j.ajic.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Ragland N.H., Miedel E.L., Engelman R.W. PCR prevalence of murine opportunistic microbes and their mitigation by using vaporized hydrogen peroxide. J Am Assoc Lab Anim Sci. 2019;58:208–215. doi: 10.30802/AALAS-JAALAS-18-000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vannier M., Chewins J. Hydrogen peroxide vapour is an effective replacement for Formaldehyde in a BSL4 Foot and mouth disease vaccine manufacturing facility. Lett Appl Microbiol. 2019;69:237–245. doi: 10.1111/lam.13203. [DOI] [PubMed] [Google Scholar]
- 21.Kalmar I.D., Cay A.B., Tignon M. Sensitivity of African swine fever virus (ASFV) to heat, alkalinity and peroxide treatment in presence or absence of porcine plasma. Vet Microbiol. 2018;219:144–149. doi: 10.1016/j.vetmic.2018.04.025. [DOI] [PubMed] [Google Scholar]
- 22.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marshall M.V., Cancro L.P., Fischman S.L. Hydrogen peroxide: a review of its use in dentistry. J Periodontol. 1995;66:786–796. doi: 10.1902/jop.1995.66.9.786. [DOI] [PubMed] [Google Scholar]
- 24.Harkins H.P. Treatment of pharyngitis and laryngitis with an improved hydrogen peroxide. Eye Ear Nose Throat Mon. 1959;38:942–944. [PubMed] [Google Scholar]
- 25.Brown E.A. Glycerite of hydrogen peroxide; a correlative review of laboratory and clinical data. Ohio State Med J. 1946;42:600–604. [PubMed] [Google Scholar]
- 26.Aagesen W.J., Brown E.A., Weiss L.R. Glycerite of hydrogen peroxide; its use in various inflammatory aural conditions. Eye Ear Nose Throat Mon. 1947;26:27–31. [PubMed] [Google Scholar]
- 27.Halliwell B., Clement M.V., Long L.H. Hydrogen peroxide in the human body. FEBS Lett. 2000;486:10–13. doi: 10.1016/s0014-5793(00)02197-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.