Abstract
Coronavirus-caused pneumonia (COVID-19) broke out in December 2019. The virus soon proved to be extremely contagious and caused an international pandemic. Clinicians treating COVID-19 patients face considerable danger of occupational exposure because of the highly infectious nature of the virus, and precautions must be taken to prevent medical staff infections. This article lists important measures that may save the lives of patients and medical staff during the COVID-19 pandemic and help stop the transmission of COVID-19 on hospital grounds. The suggestions include establishing detailed infection control and prevention protocols in the operating room; expediting testing procedures and patient screening for COVID-19; using case-specific treatment planning for vascular patients with COVID-19, favoring minimally invasive methods; and establishing and reinforcing protective awareness of medical personnel.
Keywords: COVID-19, Emergency vascular case, Medical staff, Prevention and control strategy
Coronavirus-caused pneumonia (COVID-19) broke out in December 2019. Because of the strong contagious characteristics of this disease, frontline medical staff is at high risk for occupational exposure and infection.1 , 2 Therefore, preventing nosocomial infections is a particularly important and challenging task during this pandemic.
The special conditions warranted by the COVID-19 pandemic may have certain negative impacts on the diagnosis, treatment, and relocation of patients with emergency vascular cases, such as acute aortic dissection, ruptured thoracoabdominal aortic aneurysms, acute arterial embolism, deep venous thrombosis of the lower extremities, or other high-mortality vascular diseases that have a short rescue window. Nosocomial infections are most likely to occur from contact during patient transport and management.
To prevent frontline medical staff members from being infected, The First Affiliated Hospital, Sun Yat-sen University vascular center has used the diagnosis and treatment plan of COVID-19 pneumonia (trial version 7)3 and the infection prevention and control protocols (IPCPs) of The First Affiliated Hospital, Sun Yat-sen University operating center to devise various protection and control strategies regarding the management of vascular emergencies during the pandemic.
Given that the pandemic has spread worldwide and many international colleagues deal now with similar highly challenging and dangerous scenarios, we are pleased to share these guidelines and strategies for everyone's benefit.
General principles
Under the provision and regulation of a medical task force, the IPCPs are formulated and carried out by the operating center. The IPCPs reinforce and ensure the protection of medical personnel, the implementation of preoperative evaluations and preventive measures, the use of protective strategies for patients preoperatively and postoperatively, the use of isolated operating rooms, and the rehearsal of these procedures.
Blood availability for transfusions is often a challenge during epidemics; hospitals need to communicate closely with their local blood banks and keep track of blood available for planning operations. Hospitals should initiate as many blood donations as possible.
To avoid cross-contamination and to prevent further spread of the infection, elective and nonurgent vascular operations should be delayed on the basis of the current and predicted numbers of COVID-19 patients. Elective operations should be performed only when the number of COVID-19 patients is low.
COVID-19 screening and triage coupled with vascular imaging studies should be performed expeditiously. Screening for COVID-19 includes a history and physical examination with temperature check, chest computed tomography scanning, pharyngeal swab samples for nucleic acid tests, and point-of-care antibody tests; imaging relevant to the patient's vascular emergency should be completed. Nucleic acid tests require an extended time (4-6 hours) and may produce incorrect or unreadable results from improperly retrieved samples. Point-of-care antibody tests for COVID-19 may be quick but limited in locations. Performing plain chest computed tomography reveals characteristic lung inflammation caused by COVID-19 infections. These screening results can immediately differentiate COVID-19 patients from those with other conditions and expedite treatment planning.
If surgical intervention is required, minimally invasive endovascular interventions are preferred because of less blood loss, reduced likelihood of blood infection, and decreased postoperative recovery time. If open surgery is necessary, staged procedures and alternative methods can be used to avoid major surgical operations that involve major blood loss. Life-threatening conditions should be addressed first, with secondary operations performed only after limits on personal protective equipment (PPE) and blood bank volume have been lifted.
Training medical personnel for COVID-19-related procedures and rules is critical as most physicians have limited knowledge and experience in the prevention and control of infectious diseases. Details such as wearing proper personal protection, enforcing disinfection measures, and engaging in proper training are vital to avoid nosocomial transmissions.
Overall assessment and treatment principles
Treatment of confirmed/suspected COVID-19 patients with acute vascular surgical diseases
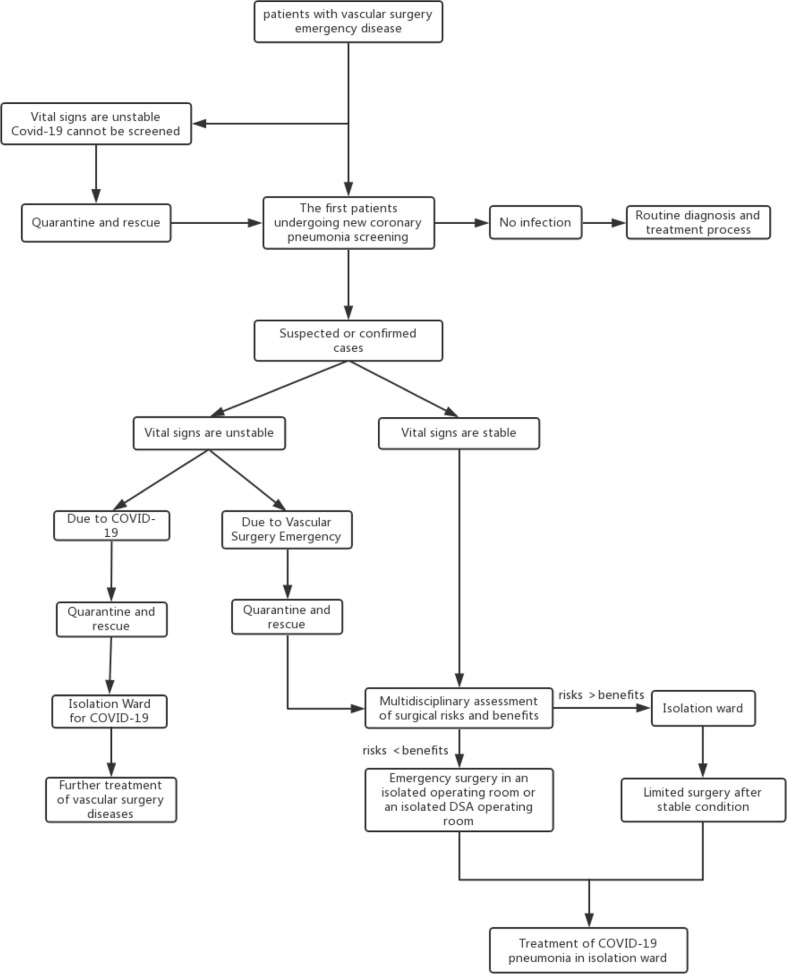
Patients with vascular emergencies with unstable vital signs caused by COVID-19 should be immediately separated and isolated (Fig 1 ). A multidisciplinary team should quickly assess these patients. Under the level three protective standard, tracheal intubation is performed, combined with other required resuscitation treatments. If possible, vascular treatment is performed after the patient is in stable condition.
Fig 1.
Flow chart with recommendations for the diagnosis and treatment of vascular surgery-related emergencies during the COVID-19 pandemic. DSA, Digital subtraction angiography.
Suspected or confirmed COVID-19 patients with unstable vital signs caused by vascular emergencies should be resuscitated in an isolated area. A multidisciplinary team performs a rapid assessment of the risk-benefit ratio. If the benefit is greater than the risk, a surgical treatment plan is quickly formulated. The operation is performed in an isolated digital subtraction angiography or hybrid operating room. After surgery, patients are transported to an isolation ward that actively treats COVID-19. If the risk is greater than the benefit, the patient should be isolated for conservative treatment following the same isolation procedures until his or her condition is stable enough for surgery.
Patients who have unstable vital signs and cannot be screened should be treated as if they were confirmed COVID-19 patients. Testing can be conducted later if the patient stabilizes.
Treatment of non-COVID-19 patients with acute vascular surgical disease
Patients who screen negative for COVID-19 should be treated as usual following the process for diagnosis and treatment of vascular emergencies.
Strategies for the prevention and control of COVID-19 during emergency vascular surgery
Preparation of isolation room
Requirements for isolation of the operating room
An isolated operating room should be under negative pressure. An operating room with separate air conditioning can serve as an alternative if a negative pressure operating room is unavailable. It usually takes at least 15 minutes to depressurize the room. Outside the operating room, a clean room and buffer zone are established before an operation. Isolation signs marking the presence of possibly harmful aerosols, droplets, and contact should be displayed outside the operating room door. The PPE involved in the operation should be streamlined. The number of staff in the room is limited as much as possible, and unnecessary personnel and visitors are not allowed.
Surgical supply preparation
All supplies are fully prepared before the patient enters the room. All medical personnel should be equipped with PPE according to the level three protection standard. For reusable equipment, protective covers should be used as much as possible. The minimum surgical supplies should be in the room.
Patient transport
When transported in the hospital, patients with suspected or confirmed cases of COVID-19 should be moved along the special routes designated by the hospital task force. Routes should be cleared and have minimal human traffic before transportation to limit contact. While transporting these patients, medical personnel should wear level three PPE, including N95 masks, goggles, gowns, double gloves, and shoe covers. The patient must wear a mask and is transported in a negative pressure isolation chamber if it is available. Equipment must be disinfected after each use with a disinfectant containing 2000 mg/L chlorine or 75% ethanol,4 and the elevator must be immediately closed and disinfected with ultraviolet light for 1 hour.
Surgical protective wear and intraoperative precautions
All operative personnel must enter the potential buffer room from the clean room. Surgical personnel in buffer rooms need to disinfect their hands5 and put on protective clothing, protective masks, trouser covers, shoe covers, two layers of sterile gloves, and sterile disposable surgical clothing before entering. The surgeon may use positive pressure headgear if it is available.
The type of anesthesia is basically determined by the type of emergency vascular case. Aortic surgery should be performed under intubation, and lower limb surgery can be performed under local nerve block or intubation if necessary. A surgical assistant will usually care for the patient alongside an anesthesiologist, anesthesiology assistant, and circulating nurse during anesthesia in the isolated operating room. During intubation, the anesthesiologists are equipped with level three PPE including gowns, goggles, and N95 mask and positive-pressure headgear if it is available (Fig 2 ).
Fig 2.
Level three personal protective equipment (PPE) including gown, goggles, N95 mask, and positive-pressure headgear.
Intraoperatively, contamination of the environment should be minimized. Once contaminated, surfaces should be disinfected immediately. Small amounts of contaminants are carefully removed using disposable absorbent materials (eg, gauze, rags) with 5000 to 10,000 mg/L chlorine-containing disinfectant solution (or disinfectant wipes/dry towels that can achieve high levels of disinfection). Large quantities of contaminants should be covered entirely with disinfectant or bleach-containing absorbent ingredients or with a sufficient amount of 5000 to 10,000 mg/L chlorine-containing disinfectant after being completely covered with disposable absorbent materials. The area is treated with absorbent materials for >30 minutes (or disinfectant wipes/dry towels that can achieve a high level of disinfection) and carefully cleaned. Contact with contaminants is avoided during removal, and contaminants are disposed of in a centralized medical waste disposal area. After visible contaminants are removed from the floor and walls, the surfaces are wiped or sprayed with chlorine-containing disinfectant solution (2000 mg/L). The solution should be left in place for at least 30 minutes.6
Postoperative management
Patients
Any blood or secretions should be wiped off the patient's body. Surgical wounds must be adequately covered. The patient is extubated in the isolated intensive care unit. A disposable sheet is used to cover the patient during transfer. The surgeon and anesthesiologist, while adhering to level three protective measures, transport the patient to the isolation intensive care unit.
Surgical personnel
IPCPs are strictly enforced in contaminated areas and buffer zones. PPE worn in the isolated area is removed before entering a locker room/stall, and personnel should shower and change their clothes before leaving. Medical personnel and staff who participated in the operation should undergo further medical observation and quarantine if necessary for 14 days.
Reusable surgical instruments
The following sequence should be performed to sanitize reusable surgical instruments: disinfection, cleaning, and sterilization. Subjected items should be soaked in chlorine disinfectant (5000-10,000 mg/L) for ≥60 minutes in the operating room.
Pathologic specimens
Specimens should be placed in a double layer of specimen bags, affixed with a unified label (COVID-19), and transported from the negative pressure operating room along the designated pathway to the pathology department. Pneumatic transport should not be used at any point.
Waste disposal
After the air is disinfected, the wasteful items are packaged in a double layer of yellow medical waste bags. Bags should be labeled (COVID-19), and the supply room is notified by telephone immediately before the items are transported there for treatment. Waste disposal procedures should adhere to the requirements of the infectious disease prevention and control protocols, medical waste management regulations, and management measures for medical waste and are performed in a timely manner.
Final disinfection
The final cleaning of the operating room and the negative pressure transport chamber is performed by the medical staff and the cleaning personnel. Cleaning personnel should receive relevant training and wear appropriate PPE. Surgery should be registered in the "Register of surgery under special infection conditions after completion" or other special surgical records.
When there are visible contaminants on the ground, walls, or other surfaces in the operating room, the contaminants are removed entirely from these surfaces before disinfection. When there are no visible contaminants, the surfaces are wiped or rinsed with 2000 mg/L chlorine-containing disinfectant and then wiped clean with water after 30 minutes.6
Indoor air
Negative pressure laminar flows should be closed, and peracetic acid fumigation disinfection (concentration 1 g/m3) should be performed. The operating room remains closed for 2 hours. The negative pressure laminar flow is then opened 30 minutes before the operating room is cleaned. After cleaning, the negative pressure laminar flow should remain open for 30 minutes. The air purification system is checked often and repaired as needed, and filters are replaced at least 30 minutes after the operating room has been cleaned.7 After the air is sterilized, filters need to be removed and treated according to the medical waste protocols. The operating room can be used only after two samples have tested negative for contamination.
Conclusions
With proper training, information, and study regarding the routes and mechanisms of transmission of the COVID-19 coronavirus, infection and mortality rates in medical personnel will gradually decrease. It is critical to identify ways to optimize relevant treatment strategies from vascular emergencies during the COVID-19 outbreak. In addition, we look forward to receiving the latest guidance on COVID-19 from public health experts.
The provision of PPE to patients and staff when needed is also crucial. Government/third-party assistance to enhance PPE manufacturing is vital to guarantee that a steady and reasonable amount of PPE is consistently available. As an example of how government or third-party assistance can benefit the situation, such assistance turned the city of Qingyuan, China, with only a single PPE manufacturing company, into a PPE manufacturing center with >20 factories.8
This article is based on our hospital's medical, surgical, and protective protocols along with related management processes that were developed on the basis of our hospital's experience in the treatment of vascular diseases and emergencies. There are inevitably deficiencies and omissions in these guidelines, and constructive criticism and corrections are always welcome.
Author contributions
Conception and design: JW, MK, LC, SW
Analysis and interpretation: JW, CL, LZ
Data collection: Not applicable
Writing the article: JW, CL, LZ
Critical revision of the article: JW, MK, LC, CL, LZ, SW
Final approval of the article: JW, MK, LC, CL, LZ, SW
Statistical analysis: Not applicable
Obtained funding: Not applicable
Overall responsibility: JW
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese J Epidemiol. 2020;41:145–151. [Google Scholar]
- 2.Wang D.W., Hu B., Hu C., Zhu F.F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Commission of the People's Republic of China Diagnosis and treatment plan of COVID-19 pneumonia (trial version 7) http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml Available at:
- 4.WST 367-2012 . National Health Commission of the People's Republic of China; Beijing, China: 2012. Medical institution disinfection technical specifications. [Google Scholar]
- 5.WST313-2009 . National Health Commission of the People's Republic of China; Beijing, China: 2009. Medical staff hand hygiene regulations. [Google Scholar]
- 6.WST512-2016 . National Health Commission of the People's Republic of China; Beijing, China: 2016. Code of management for cleaning and disinfection of environmental surface of medical institutions. [Google Scholar]
- 7.GB50333-2013 . National Health Commission of the People's Republic of China; Beijing, China: 2013. Technical specification for construction of clean operation department in hospital. [Google Scholar]
- 8.The Paper News More than 1.3 million masks are produced every day, and an industrial chain of masks has been established in Qingyuan. https://www.thepaper.cn/newsDetail_forward_6684978 Available at: