Abstract
Background: Associations between household chaos and childhood overweight have been identified, but the mechanisms of association are not clearly established in young children, with some studies linking higher chaos to increased obesity risk, whereas other studies link higher chaos to lower obesity risk. Given the lack of consistent findings and early sex differences in vulnerability to chaos, we examined child sex as a moderator of the chaos-child overweight association. We also tested these associations with self-regulation, as self-regulation has been implicated in understanding the chaos-obesity risk association in low-income toddlers.
Methods: Parent-reported household chaos and observed child self-regulation were collected at baseline [n = 132; M age 23.0 months (standard deviation 2.8)]. Children's body mass index z-score (BMIz) was measured at 33 months. Multivariate linear regression models were used to assess whether child sex moderated the chaos-BMIz association. A three-way interaction between chaos, child sex, and self-regulation was also tested.
Results: Child sex moderated the chaos-BMIz association (b = −0.11, p = 0.04) such that chaos was positively associated with BMIz among boys (b = 0.12, p = 0.003), but unrelated in girls (b = 0.01, p = 0.78). A three-way interaction with self-regulation indicated that a positive chaos-BMIz association existed only for boys with average (b = 0.12, p = 0.004) and low (b = 0.22, p < 0.001) self-regulation.
Conclusions: Boys with poor self-regulation may be particularly vulnerable to obesogenic effects of chaotic households.
Keywords: early childhood, household chaos, self-regulation, sex, weight
Introduction
Household chaos, defined by unpredictability, lack of structure, crowding, and disorganization,1 is known to interfere with child health and development. Studies with infants and toddlers have found positive associations between household chaos and adverse child outcomes, including delayed language,2 problematic behavior,3 and poorer general health.4 Beyond these developmental outcomes, household chaos may have implications for early childhood obesity. A recent review found that the degree of organization in the home environment was significantly associated with child overweight in 27 of 32 studies, with 10 of 14 studies finding significant associations during early childhood.5 Although many studies in this review reported significant associations, the results were inconsistent, with some studies linking higher chaos to increased obesity risk,6–8 whereas other studies reported higher chaos is associated with lower obesity risk.9–11 The mechanisms of association are also unclear; however, there is evidence that household chaos may interfere with self-regulation,12–16 a protective factor against obesity.17–20 We posit that moderating variables, such as child sex, may be important to consider, given early sex differences in self-regulation21 and vulnerability to chaos22,23 that may shape these associations.
Child sex differences in household chaos-overweight associations may be one reason for inconsistent results, as environmental stress may affect boys and girls differently.24–26 For example, prior work has found boys are more sensitive to external stressors such as environmental chaos23,24 and crowding.27,28 Among older children, sex moderated the impact of family routines on obesity risk, such that routine family meals were associated with lower obesity risk in boys, but not in girls, suggesting boys may particularly benefit from such routines.9 Yet, sex differences have not been considered in prior work with toddlers.
Self-regulation, which develops rapidly across toddlerhood, refers to the ability to manage attention, emotions, and behaviors to accomplish goal-directed actions.29 Better self-regulation skills have been identified as a protective factor against obesity.17–20 Self-regulation can be compromised among children living in chaotic households,12–16 as the psychosocial stress of a chaotic environment can impair development of such skills.30 Thus, self-regulation may be a mechanism by which household chaos influences obesity risk differently between sexes. Indeed, a longitudinal study with low-income preschoolers found family routines at 24 months of age had stronger positive associations with self-regulation among boys (vs. girls) at 36 months.22 Furthermore, associations between self-regulation and obesity risk can vary by sex. In a nationally representative sample, obesity prevalence was lowest among boys with self-regulation scores in the highest quartile at 2 years of age, whereas for girls, obesity prevalence was lowest among those with self-regulation scores in the middle quartiles.21
Despite these sex differences, only one study has investigated the role of child sex in the association between chaos and obesity risk.9 In order for interventions to better identify and target children most at risk for obesity, it is critical to understand what factors impact chaos-overweight associations during early childhood. Thus, this study aims to investigate child sex as a moderator of the association between household chaos and child body mass index z-score (BMIz). To our knowledge, just two studies have examined mechanisms by which organization of the home environment is associated with obesity risk in toddlerhood16,31; therefore, we also examine the extent to which the interaction between child sex and chaos varies across different levels of self-regulation. Importantly, we investigate these patterns longitudinally in a sample of low-income toddlers, who are at high risk for living in chaotic households32 and maintaining excessive weight into later life.33 Due to evidence that boys are more sensitive to environmental chaos,23,24 we hypothesize sex will moderate the chaos-BMIz association such that higher household chaos will associate with increased BMIz only among boys. However, given that self-regulation may help protect against obesity in boys,21 we hypothesize that higher household chaos will not be associated with BMIz among boys with high self-regulation.
Methods
Participants
Participants were originally recruited for a longitudinal study about child stress and eating behaviors34 through flyers posted in Early Head Start; Women, Infant, and Children (WIC) offices; and pediatric clinics in urban, suburban, and rural areas. Inclusion criteria were as follows: biological mother was child's legal guardian, ≥18 years old, with education <4-year college degree; child was 21–27 months of age, born at ≥36 weeks gestation without significant perinatal/neonatal complications, no food allergies, and no significant health problems or developmental delays; and the family met eligibility requirements for Head Start, WIC, or Medicaid and was English-speaking. The study was approved by the University of Michigan Institutional Review Board. Mothers provided written informed consent.
Of the 244 children, 112 children were excluded from analyses due to missing data at baseline and/or follow-up. The analytic sample included 132 children (47% female; 52% non-Hispanic white), whose mothers reported all variables of interest. Mean child age at baseline was 23.0 months [standard deviation (SD) = 2.8]. Children included in the analyses were more likely to be non-Hispanic white (64% of excluded children Hispanic or not white; p = 0.01). Sex was unlikely to vary between included and excluded participants (p = 0.54).
Measures
Household chaos
The level of confusion and disorganization in the child's household was assessed at baseline using the Confusion, Hubbub, and Order Scale (CHAOS),35 which consists of 15 statements such as “first thing in the day, we have a regular routine at home.” Participants answered each statement as true (1) or false (0). Total score was calculated by summing responses (higher score indicated higher chaos; α = 0.81).
Self-regulation
Research assistants were trained to implement the snack delay task by the study PI. The task, which assessed self-regulation at baseline, took place in participants' homes during daytime hours and was videotaped for later coding.20,36 Parents were instructed to complete questionnaires during the task. The child was seated at a child-sized table and directed to place both hands on the table, where an examiner placed a red Froot Loop under a transparent cup and said, “It's a game where you wait for me to ring this triangle before you eat a snack.” The examiner demonstrated ringing the triangle and eating the snack to avoid food neophobia. Before each trial, the examiner reminded the child “After I ring, you can eat.” Halfway through each trial, the examiner lifted the triangle wand, but did not ring the triangle. Four trials were conducted using standard delay times of 5, 10, 15, and 20s. Independent coders were trained to reliability (Cohen's κ > 0.7) to score each trial as 0 (eats snack before wand lifted); 1 (eats snack after wand lifted, but not rung); 2 (touches wand, triangle, or cup before wand lifted); 3 (touches wand, triangle, or cup after wand lifted); and 4 (waits for ring before touching anything). Scores were averaged across all trials per standard scoring instructions, with higher scores indicating better self-regulation.37
Body mass index
During the follow-up visit (33 months of age), child and mother weight and height were measured by examiners certified in standardized measurement technique (measurements collected twice and averaged; if the two measurements differed by ≥0.1 kg for weight or ≥0.5 cm for height, two additional measurements were taken and a new average calculated). Child BMIz was calculated based on the US Centers for Disease Control Growth Charts.38 Mother's BMI was also calculated.
Covariates
Mothers reported presence of the child's biological father in the household, child race/ethnicity, and maternal education level (categorized as more than a high school diploma/General Educational Development [GED] vs. not) for use as covariates in the analyses since these variables are associated with key study variables in prior literature.39–43 Maternal BMI and self-reported maternal depression symptoms using the Center for Epidemiologic Studies Depression Scale (CES-D),44 a 20-item scale with responses ranging from 1 (rarely; <1 day per week) to 4 (most of the time; ≥5 days per week), were also used as covariates. Total depression score was calculated by summing responses (higher scores indicated more depression symptoms; α = 0.89).
Statistical Analyses
Data were analyzed using SPSS (Version 24.0) and PROCESS macro (Version 3.3),45 a widely used path analysis modeling tool for estimating interactions in moderation models and testing simple slopes to further understand interactions. Descriptive statistics were conducted to characterize the sample (Table 1). Independent t-tests assessed whether key study variables varied by presence of biological father, child race/ethnicity, or mother's education level. Bivariate correlations were conducted to examine associations between key study variables and continuous covariates.
Table 1.
Demographic and Descriptive Characteristics (n = 132)
| Demographics and descriptive variables | |
|---|---|
| Age, months, mean (SD) | 23.0 (2.8) |
| Female, raw count, n (%) | 62 (47.0) |
| Child race/ethnicity, raw count, n (%) | |
| Hispanic/Latino and/or not white | 64 (48.5) |
| Non-Hispanic white | 68 (51.5) |
| Biological father present in home, n (%) | 84 (63.6) |
| Maternal education, n (%) | |
| More than high school | 81 (61.4) |
| High school or less | 51 (38.6) |
| CES-D total score, mean (SD) | 13.22 (10.41) |
| Maternal BMI, mean (SD) | 32.90 (9.93) |
| Child BMIz, mean (SD) | 0.33 (1.01) |
| Home chaos, mean (SD) | 4.21 (3.23) |
| Snack delay, mean (SD) | 1.99 (1.22) |
BMIz, body mass index z-score; CES-D, Center for Epidemiologic Studies Depression Scale; SD, standard deviation.
PROCESS macro for SPSS45 was used to test sex as a moderator of the association between household chaos and child BMIz. Covariates included presence of biological father, child race/ethnicity, maternal education, maternal BMI, and maternal depression symptoms. Self-regulation was tested as a moderator in this model to investigate whether it further explicated the association between household chaos and child BMIz.
Results
Descriptive and Bivariate Analyses
Independent t-tests suggested key study variables (household chaos, child BMIz, and Snack Delay score) were unlikely to differ by presence of a biological father, child race/ethnicity, child sex, or maternal education level (0.10 < ps < 0.90). Children obtained an average score of 1.99 (SD = 1.22) out of a possible 4 on the snack delay task in which higher scores reflected better self-regulation. Scores on this task were lower than studies using the same task with somewhat older children,36 as may be expected, and were evenly distributed, with 18.2% of children scoring the maximum amount, indicating they waited the required amount of time on all four trials. Results from bivariate analyses (Table 2) indicated a positive association between maternal BMI and child BMIz (r = 0.18) and negative association with Snack Delay score, such that higher maternal BMI was related to poorer child self-regulation (r = −0.19). Household chaos was positively associated with maternal depression symptoms (r = 0.40).
Table 2.
Bivariate Correlations between Covariates, Predictor, and Outcome
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Household Chaos | — | |||
| 2. Child BMIz | 0.13 | — | ||
| 3. Snack Delay | 0.06 | −0.16† | — | |
| 4. Maternal BMI | 0.02 | 0.18* | −0.19* | — |
| 5. CES-D | 0.40** | −0.11 | −0.01 | 0.06 |
p ≤ 0.10. *p ≤ 0.05. **p ≤ 0.01.
Moderation Analysis
Results from the overall model that included child sex as a moderator of the chaos-BMIz association suggested a nonzero moderator effect by child sex; as shown in Table 3, the interaction of household chaos and child sex was significant [F(1, 123) = 4.46, R2 = 0.03, p = 0.04].
Table 3.
Results of Regression Analyses Predicting Child Body Mass Index z-Score and Testing Sex as a Moderator
| Variable | Model 1 |
Model 2 |
||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | p | △R2 | b | SE | p | △R2 | |
| Covariate | ||||||||
| Biological father in home | −0.04 | 0.18 | 0.85 | −0.08 | 0.18 | 0.68 | ||
| Child race/Ethnicity | 0.13 | 0.18 | 0.46 | 0.07 | 0.18 | 0.69 | ||
| Maternal education | 0.03 | 0.18 | 0.89 | −0.01 | 0.17 | 0.94 | ||
| Maternal BMI | 0.02 | 0.01 | 0.02 | 0.02 | 0.01 | 0.02 | ||
| Maternal CES-D | −0.02 | 0.01 | 0.01 | −0.03 | 0.01 | 0.00 | ||
| Predictors | ||||||||
| Household chaos | 0.07 | 0.03 | 0.02 | 0.07 | 0.03 | 0.02 | ||
| Sex | 0.22 | 0.17 | 0.20 | 0.24 | 0.17 | 0.16 | ||
| Household chaos × Sex | −0.11 | 0.05 | 0.04 | 0.03 | −0.10 | 0.05 | 0.07 | |
| Snack delay | −0.11 | 0.07 | 0.12 | |||||
| Household chaos × Snack delay | −0.04 | 0.02 | 0.09 | |||||
| Sex × Snack delay | −0.16 | 0.14 | 0.25 | |||||
| Household chaos × Sex × Snack delay | 0.10 | 0.05 | 0.04 | 0.03 | ||||
Thus, slopes for the association between household chaos and child BMIz were tested stratified by sex and indicated that household chaos was positively associated with BMIz among boys (b = 0.12, SEb = 0.04, p = 0.003, 95% CI = [0.04–0.20]), but unlikely to be associated with BMIz among girls (b = 0.01, SEb = 0.04, p = 0.78, 95% CI = [−0.06 to 0.09]). All regression coefficients are reported as unstandardized.
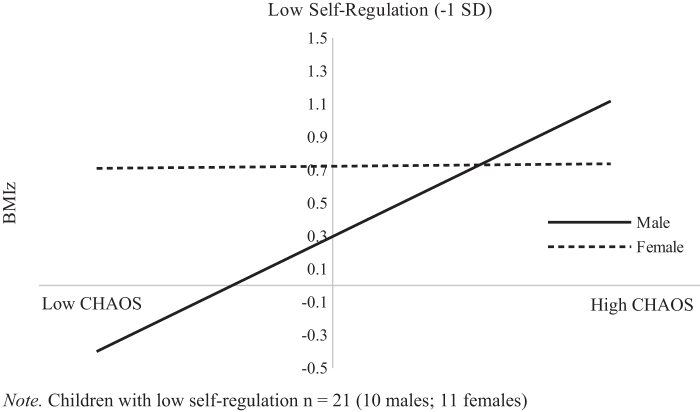
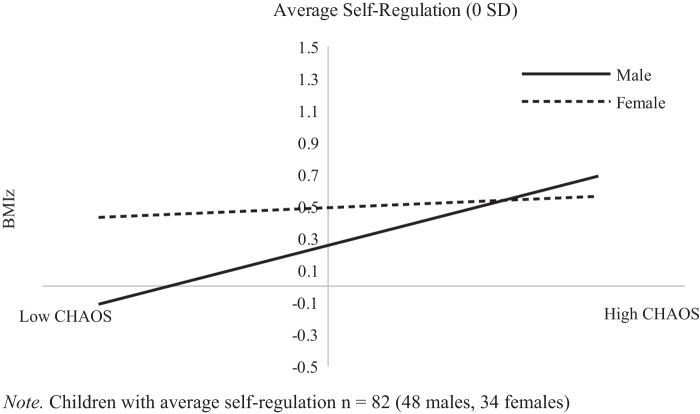
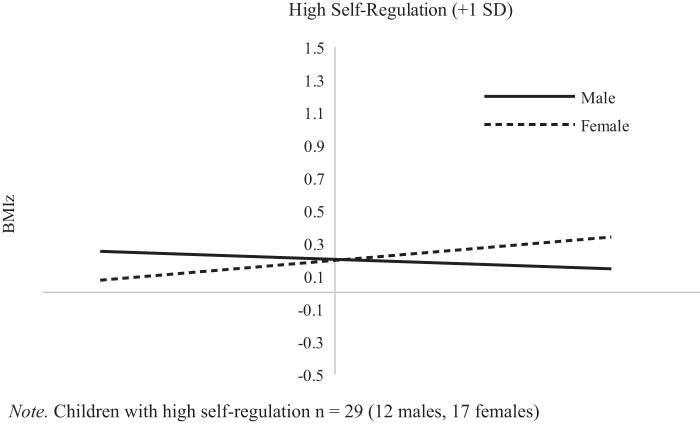
To investigate whether child self-regulation further explained the interaction between household chaos and sex to predict child BMIz, self-regulation was tested as an additional moderator. Results indicated a significant three-way interaction between household chaos, child sex, and self-regulation [F(1, 119) = 4.30, ΔR2 = 0.03, p = 0.04]. Simple slopes for the association between household chaos and child BMIz were estimated by child sex and for low (−1 SD below the mean), average, and high (+1 SD above the mean) levels of self-regulation. For boys, an association between higher household chaos and higher BMIz is significant among boys with low levels of self-regulation and decreases as level of self-regulation increases, with no significant effect among boys who express a high level of self-regulation. Specifically, at low levels of self-regulation (Fig. 1), the chaos-BMIz association was nonzero and strongest (b = 0.22, SEb = 0.06, p < 0.001, 95% CI = [0.11–0.33]), and at average self-regulation (Fig. 2), the association was lower, but still nonzero (b = 0.12, SEb = 0.04, p = 0.004, 95% CI = [0.04–0.19]). In contrast, as shown in Figure 3, the association between household chaos and BMIz was indistinguishable from zero among boys with high levels of self-regulation (b = 0.01, SEb = 0.62, p = 0.88, 95% CI = [−0.11 to 0.13]). For girls, the association between household chaos and BMIz was indistinguishable from zero and this association was unlikely to vary by self-regulation level (0.55 < ps < 0.94).
Figure 1.
The association between BMIz and household chaos in children with low self-regulation. BMIz, body mass index z-score.
Figure 2.
The association between BMIz and household chaos in children with average self-regulation.
Figure 3.
The association between BMIz and household chaos in children with high self-regulation.
Discussion
This study investigated whether child sex moderated the association between household chaos and child BMIz in a sample of low-income toddlers. Findings indicated the household chaos-child BMIz association varies by child sex, such that higher household chaos is associated with higher BMIz among boys, but not associated with BMIz among girls. Given that self-regulation may help protect against obesity in boys,21 it is possible that this finding is modified by the role of child self-regulation, which was explored by testing a three-way interaction between household chaos, sex, and self-regulation. Results suggested household chaos and child BMIz were positively associated only among boys with low or average self-regulation. For children with high self-regulation, sex differences were unlikely, with the association between chaos and BMIz indistinguishable from zero for both sexes.
Numerous studies have found household chaos to be associated with childhood overweight.5 This study is the first to examine child sex as a moderator of the household chaos and childhood overweight association in this age range. One prior study investigated moderators of the association between childhood overweight and family mealtime routines, a component of household chaos, among older children (6–11 years) and found regular family meals was negatively associated with risk of overweight/obesity in non-Hispanic black boys, whereas no association was found in non-Hispanic black girls.9 Rollins et al.9 also found ethnicity to be a moderator and proposed their results may be due to differences in mealtime practices between sexes and ethnicities, such as non-Hispanic white parents placing more foods within reach for boys than girls during family meals.46 Further investigation into potential pathways through which household chaos may influence overweight differently between sexes, for example, through different parenting47 or child feeding practices,48 may be useful for understanding sex differences in the household chaos-BMIz association.
In addition to organized home environments exposing children to health behaviors that help protect against obesity such as nighttime sleep routines and limited screen time,5,6,16 less chaotic households may be beneficial for child self-regulation, which can protect against the effects of a stressful environment.49–51 Previous studies, however, have focused on whether self-regulation buffers the association between stressful environments and behavioral outcomes, rather than weight. For instance, in a longitudinal study among low-income toddlers, household chaos was positively associated with child internalizing and externalizing problems, but not among toddlers with high self-regulation.50 This is consistent with the present finding that boys with high self-regulation did not exhibit a chaos-BMIz association, suggesting better self-regulation skills may be protective for these individuals. Self-regulation is also a predictor of general resilience among children living in poverty,52 and benefits of self-regulation may extend well beyond protecting against obesity in a chaotic household.50,52
There are known sex differences in self-regulation in early childhood, and evidence that contextual factors like household chaos may associate with boys' and girls' self-regulation differently. For example, among 3-year olds, less household chaos, as measured by family routines at 14 months, was associated with higher self-regulation among girls, but not associated with self-regulation among boys.22 Furthermore, the association between self-regulation and overweight is not consistent between sexes. In a nationally representative sample, 2-year-old boys in the highest quartile for self-regulation had the lowest obesity prevalence at age 5, whereas 2-year-old girls in the middle quartiles for self-regulation displayed the lowest obesity prevalence at age 5.21 Our results are consistent with this finding, suggesting self-regulation may be protective for boys in high-chaos households.
Other explanations for reported sex differences include higher maturity levels53 and resilience to environmental stress early in life among girls.24,27,28,54 From birth, boys have less mature stress-response systems53; thus, boys may experience more difficulty reducing arousal in response to chaos. Prolonged secretion of stress hormones brought forth from chaotic household environments may lead to biological changes, including increased visceral fat55,56 and increased desire to consume palatable foods.57–59 Furthermore, researchers have found household chaos is associated with more emotional negativity among infant boys, but not among infant girls.23 It is plausible that boys may engage in suboptimal emotion regulation strategies, such as emotional eating in response to stress. Hence, the less developed male stress-response system may result in boys being more vulnerable to the obesogenic effects of household chaos.
Other indirect mechanisms by which boys are more vulnerable to household chaos may also help account for sex differences. For example, household chaos may interfere with sleep,60–64 which is important for self-regulation.65,66 The association of sleep duration and risk of overweight/obesity may be stronger in boys,67 with some studies finding an association between sleep duration and weight status among boys, but not girls.60,61,68 Due to stronger associations between sleep and overweight in boys, household chaos may have stronger associations with boys' BMIz through sleep. Similarly, household chaos is positively associated with screen time,69 and it has been posited that boys are more influenced by food-related advertising.70,71 Boys' greater susceptibility to food advertisements could encourage boys to consume more obesogenic foods in chaotic households. Studies should further investigate mediating pathways of household chaos and child overweight during early childhood to extend our understanding of reported sex differences.
Our results are relevant for obesity interventions. A randomized trial with preschool-aged children found that participating in a home-based intervention that promotes household routines (i.e., promoting family meals, adequate sleep, limiting screen time, and removing the television from child's bedroom) resulted in a decreased BMI.72 Our results suggest that weight management programs seeking to reduce household chaos may be most effective for male toddlers. Our findings also suggest boys' self-regulation skills may be an important intervention target to help protect against obesogenic effects of household chaos. Since boys have poorer self-regulation than girls during toddlerhood73 and preschool-age,74 self-regulation interventions may be especially needed for young boys, and recent work shows promise for such interventions.75 Future research could identify whether self-regulation interventions are more useful for reducing obesity risk in boys (vs. girls) living in a chaotic household.
This study investigated longitudinal associations between chaos and BMIz during toddlerhood, which is important for understanding how early-life factors emerge and inform how we may prevent obesity. Additional strengths include the sample of low-income families, who are more likely to live in chaotic households.32 We used objective measures of BMIz and self-regulation,37 and our CHAOS measure demonstrates strong correlations with directly observed measures of household chaos.35
Limitations include challenges to external validity. Since participants were limited to low-income families living in the Midwest United States, these findings may not apply to other samples (e.g., socioeconomically diverse samples or children from other cultures). Future work with other samples may seek to replicate these findings, especially considering that self-regulation may vary between samples. Our analyses did not account for changes in household chaos between baseline and follow-up, although the intensity of chaos experienced by families may change across time. These associations may not be causal, as other variables associated with household chaos that were not assessed (e.g., family functioning) may have influenced child BMIz.
Conclusion
In low-income toddlers, household chaos is positively associated with child BMIz among boys with average or low self-regulation, whereas no association is found in girls. Obesity prevention in the home environment is the preferred method of delivery for obesity prevention programs for many families.76 Findings suggest that obesity prevention strategies, which seek to establish routines and organize the household, may be important for young boys. Future research should consider testing these associations in other age groups and investigate other mechanisms by which these associations occur.
What Is New
Child sex moderated the household chaos-BMIz association such that higher household chaos was associated with greater BMIz only among boys. Further analyses revealed that household chaos was positively associated with BMIz only for boys with low and average self-regulation, suggesting that self-regulation may help protect against the obesogenic effects of a chaotic household among boys.
Funding Information
This work was supported by the National Institutes of Health, award number 1R01HD069179 to Alison Miller and Julie Lumeng.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Evans GW, Gonnella C, Marcynyszyn LA, et al. The role of chaos in poverty and children's socioemotional adjustment. Psychol Sci 2005;16:560–565 [DOI] [PubMed] [Google Scholar]
- 2. Vernon-Feagans L, Garrett-Peters P, Willoughby M, Mills-Koonce R. Chaos, poverty, and parenting: Predictors of early language development. Early Child Res Q 2012;27:339–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coldwell J, Pike A, Dunn J. Household chaos—Links with parenting and child behaviour. J Child Psychol Psychiatry 2006;47:1116–1122 [DOI] [PubMed] [Google Scholar]
- 4. Coley RL, Lynch AD, Kull M. Early exposure to environmental chaos and children's physical and mental health. Early Child Res Q 2015;32:94–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bates CR, Buscemi J, Nicholson LM, et al. Links between the organization of the family home environment and child obesity: A systematic review. Obes Rev 2018;19:716–727 [DOI] [PubMed] [Google Scholar]
- 6. Anderson SE, Whitaker RC. Household Routines and Obesity in US Preschool-Aged Children. Pediatrics 2010;125:420–428 [DOI] [PubMed] [Google Scholar]
- 7. Jones B, Fiese B. Parent routines, child routines, and family demographics associated with obesity in parents and preschool-aged children. Front Psychol 2014;5:374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Horning ML, Schow R, Friend SE, et al. Family dinner frequency interacts with dinnertime context in associations with child and parent BMI outcomes. J Fam Psychol 2017;31:945–951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rollins BY, Belue RZ, Francis LA. The beneficial effect of family meals on obesity differs by race, sex, and household education: The National Survey of Children's Health, 2003–2004. J Am Diet Assoc 2010;110:1335–1339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Starling WP, Reifsnider E, Bishop SL, et al. Changes in family variables among normal and overweight preschoolers. Issues Compr Pediatr Nurs 2010;33:20–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schuch I, Castro TGd, de Vasconcelos FdA, et al. Excess weight in preschoolers: Prevalence and associated factors. J Pediatr 2013;89:179–188 [DOI] [PubMed] [Google Scholar]
- 12. Hails KA, Zhou Y, Shaw DS. The mediating effect of self-regulation in the association between poverty and child weight: A systematic review. Clin Child Fam Psychol Rev 2019;22:290–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barton AW, Brody GH, Yu T, et al. The profundity of the everyday: Family routines in adolescence predict development in young adulthood. J Adolesc Health 2019;64:340–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miller AL, Song J-H, Sturza J, et al. Child cortisol moderates the association between family routines and emotion regulation in low-income children. Dev Psychobiol 2017;59:99–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bridgett DJ, Burt NM, Laake LM, Oddi KB. Maternal self-regulation, relationship adjustment, and home chaos: Contributions to infant negative emotionality. Infant Behav Dev 2013;36:534–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anderson SE, Sacker A, Whitaker RC, Kelly Y. Self-regulation and household routines at age three and obesity at age eleven: Longitudinal analysis of the UK Millennium Cohort Study. Int J Obes 2017;41:1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. Int J Obes 2010;34:633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med 2009;163:297–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Seeyave DM, Coleman S, Appugliese D, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med 2009;163:303–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miller AL, Rosenblum KL, Retzloff LB, Lumeng JC. Observed self-regulation is associated with weight in low-income toddlers. Appetite 2016;105:705–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Anderson SE, Whitaker RC. Association of self-regulation with obesity in boys vs girls in a US National sample. JAMA Pediatr 2018;172:842–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ferretti LK, Bub KL. The influence of family routines on the resilience of low-income preschoolers. J Appl Dev Psychol 2014;35:168–180 [Google Scholar]
- 23. Matheny AP, Phillips K.. Temperament and context: Correlates of home environment with temperament continuity and change, newborn to 30 months. In: McCrae RR, Wachs TD, Kohnstemm GA (eds.). Temperament Context Psychology Press: New York, 2001, pp. 81–101 [Google Scholar]
- 24. Ponitz Claire C, Rimm-Kaufman Sara E, Brock Laura L, Nathanson L. Early adjustment, gender differences, and classroom organizational climate in first grade. Elem Sch J 2009;110:142–162 [Google Scholar]
- 25. Hay DF, Asten P, Mills A, et al. Intellectual problems shown by 11-year-old children whose mothers had postnatal depression. J Child Psychol Psychiatry 2001;42:871–889 [DOI] [PubMed] [Google Scholar]
- 26. Edwards RC, Hans SL. Prenatal depressive symptoms and toddler behavior problems: The role of maternal sensitivity and child sex. Child Psychiatry Hum Dev 2016;47:696–707 [DOI] [PubMed] [Google Scholar]
- 27. Aiello JR, Nicosia G, Thompson DE. Physiological, social, and behavioral consequences of crowding on children and adolescents. Child Dev 1979;50:195–202 [PubMed] [Google Scholar]
- 28. Evans GW, Lepore SJ, Shejwal BR, Palsane MN. Chronic residential crowding and children's well-being: An ecological perspective. Child Dev 1998;69:1514–1523 [PubMed] [Google Scholar]
- 29. Blair C, Raver CC. Child development in the context of adversity: Experiential canalization of brain and behavior. Am Psychol 2012;67:309–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vernon-Feagans L, Willoughby M, Garrett-Peters P. Predictors of behavioral regulation in kindergarten: Household chaos, parenting, and early executive functions. Dev Psychol 2016;52:430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lumeng JC, Miller A, Peterson KE, et al. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite 2014;73:65–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Evans GW. The environment of childhood poverty. Am Psychol 2004;59:77–92 [DOI] [PubMed] [Google Scholar]
- 33. Nader PR, O'Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics 2006;118:e594–e601 [DOI] [PubMed] [Google Scholar]
- 34. Miller AL, Kaciroti N, Sturza J, et al. Associations between stress biology indicators and overweight across toddlerhood. Psychoneuroendocrinology 2017;79:98–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Matheny AP, Wachs TD, Ludwig JL, Phillips K. Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. J Appl Dev Psychol 1995;16:429–444 [Google Scholar]
- 36. Kochanska G, Murray K, Jacques TY, et al. Inhibitory control in young children and its role in emerging internalization. Child Dev 1996;67:490–507 [PubMed] [Google Scholar]
- 37. Kochanska G, Murray KT, Harlan ET. Effortful control in early childhood: Continuity and change, antecedents, and implications for social development. Dev Psychol 2000;36:220–232 [PubMed] [Google Scholar]
- 38. Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: Methods and Development. National Center for Health Statistics, 2002 [PubMed] [Google Scholar]
- 39. Schmeer KK. Family structure and obesity in early childhood. Soc Sci Res 2012;41:820–832 [DOI] [PubMed] [Google Scholar]
- 40. Augustine JM, Kimbro RT. Family structure and obesity among US children. J Appl Res Child Inform Policy Child Risk 2013;4:1–24 [Google Scholar]
- 41. Taveras EM, Gillman MW, Kleinman K, et al. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics 2010;125:686–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Isong IA, Rao SR, Bind M-A, et al. Racial and ethnic disparities in early childhood obesity. Pediatrics 2018;141:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Johnson AD, Martin A, Brooks-Gunn J, Petrill SA. Order in the house! Associations among household Chaos, the home literacy environment, maternal Reading ability, and Children's early Reading. Merrill Palmer Q 2008;54:445–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measur 1977;1:385–401 [Google Scholar]
- 45. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Publications, 2017 [Google Scholar]
- 46. Klesges RC, Coates TJ, Brown G, et al. Parental influences on children's eating behavior and relative weight. J Appl Behav Anal 1983;16:371–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cabrera NJ, Tamis-LeMonda CS, Bradley RH, et al. Parenting during early childhood in low-income families: Variation by child gender. Fam Sci 2012;3:201–214 [Google Scholar]
- 48. Orrell-Valente JK, Hill LG, Brechwald WA, et al. “Just three more bites”: An observational analysis of parents' socialization of children's eating at mealtime. Appetite 2007;48:37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Flouri E, Midouhas E, Joshi H. Family poverty and trajectories of children's emotional and behavioural problems: The moderating roles of self-regulation and verbal cognitive ability. J Abnorm Child Psychol 2014;42:1043–1056 [DOI] [PubMed] [Google Scholar]
- 50. Crespo LM, Trentacosta CJ, Udo-Inyang I, et al. Self-regulation mitigates the association between household chaos and children's behavior problems. J Appl Dev Psychol 2019;60:56–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lengua LJ, Bush NR, Long AC, et al. Effortful control as a moderator of the relation between contextual risk factors and growth in adjustment problems. Dev Psychopathol 2008;20:509–528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Buckner JC, Mezzacappa E, Beardslee WR. Characteristics of resilient youths living in poverty: The role of self-regulatory processes. Dev Psychopathol 2003;15:139–162 [DOI] [PubMed] [Google Scholar]
- 53. Kudielka BM, Kirschbaum C. Sex differences in HPA axis responses to stress: A review. Biol Psychol 2005;69:113–132 [DOI] [PubMed] [Google Scholar]
- 54. Carmody DP, Bennett DS, Lewis M. The effects of prenatal cocaine exposure and gender on inhibitory control and attention. Neurotoxicol Teratol 2011;33:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pervanidou P, Chrousos GP. Stress and obesity/metabolic syndrome in childhood and adolescence. Int J Pediatr Obes 2011;6(Suppl 1):21–28 [DOI] [PubMed] [Google Scholar]
- 56. Pervanidou P, Chrousos GP. Metabolic consequences of stress during childhood and adolescence. Metabolism 2012;61:611–619 [DOI] [PubMed] [Google Scholar]
- 57. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav 2007;91:449–458 [DOI] [PubMed] [Google Scholar]
- 58. Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry 2013;73:827–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sinha R. Role of addiction and stress neurobiology on food intake and obesity. Biol Psychology 2018;131:5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Spilsbury JC, Patel SR, Morris N, et al. Household chaos and sleep-disturbing behavior of family members: Results of a pilot study of African American early adolescents. Sleep Health 2017;3:84–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Appelhans BM, Fitzpatrick SL, Li H, et al. The home environment and childhood obesity in low-income households: Indirect effects via sleep duration and screen time. BMC Public Health 2014;14:1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mindell JA, Li AM, Sadeh A, et al. Bedtime routines for young children: A dose-dependent association with sleep outcomes. Sleep 2015;38:717–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Whitesell CJ, Crosby B, Anders TF, Teti DM. Household chaos and family sleep during infants' first year. J Fam Psychol 2018;32:622–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Boles RE, Halbower AC, Daniels S, et al. Family chaos and child functioning in relation to sleep problems among children at risk for obesity. Behav Sleep Med 2017;15:114–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hagger MS. Sleep, self-regulation, self-control and health. Stress Health 2010;26:181–185 [Google Scholar]
- 66. Miller AL, Seifer R, Crossin R, Lebourgeois MK. Toddler's self-regulation strategies in a challenge context are nap-dependent. J Sleep Res 2015;24:279–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity 2008;16:265–274 [DOI] [PubMed] [Google Scholar]
- 68. Tatone-Tokuda F, Dubois L, Ramsay T, et al. Sex differences in the association between sleep duration, diet and body mass index: A birth cohort study. J Sleep Res 2012;21:448–460 [DOI] [PubMed] [Google Scholar]
- 69. Emond JA, Tantum LK, Gilbert-Diamond D, et al. Household chaos and screen media use among preschool-aged children: A cross-sectional study. BMC Public Health 2018;18:1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chernin A. The effects of food marketing on children's preferences: Testing the moderating roles of age and gender. Ann Am Acad Political Soc Sci 2008;615:101–118 [Google Scholar]
- 71. Balfour Jeffrey D, McLellarn RW, Fox DT. The development of children's eating habits: The role of television commercials. Health Educ Q 1982;9:78–93 [PubMed] [Google Scholar]
- 72. Haines J, McDonald J, O'Brien A, et al. Healthy habits, happy homes: Randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr 2013;167:1072–1079 [DOI] [PubMed] [Google Scholar]
- 73. Vallotton C, Ayoub C. Use your words: The role of language in the development of toddlers' self-regulation. Early Child Res Q 2011;26:169–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lonigan CJ, Spiegel JA, Goodrich JM, et al. Does Preschool Self-Regulation Predict Later Behavior Problems in General or Specific Problem Behaviors? J Abnorm Child Psychol 2017;45:1491–1502 [DOI] [PubMed] [Google Scholar]
- 75. Pandey A, Hale D, Das S, et al. Effectiveness of universal self-regulation–based interventions in children and adolescents: A systematic review and meta-analysis effectiveness of universal self-regulation–based interventions in youth effectiveness of universal self-regulation–based interventions in youth. JAMA Pediatrics 2018;172:566–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. O'Kane CMRD, Wallace AMRD, Wilson LMRD, et al. Family-based obesity prevention: perceptions of canadian parents of preschool-age children. Can J Diet Pract Res 2018;79:13–17 [DOI] [PubMed] [Google Scholar]