Abstract
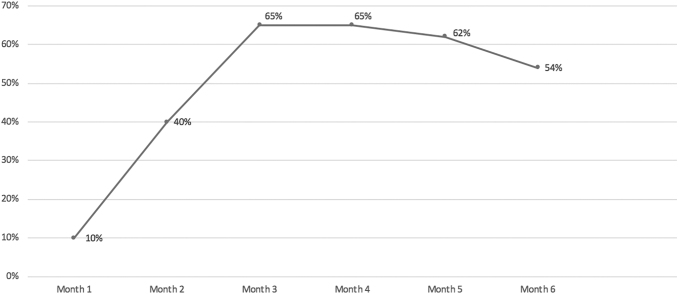
We aimed to systematically evaluate the feasibility of integrating HIV prevention services, including pre-exposure prophylaxis (PrEP), into a family planning setting in a high-prevalence community. We used the RE-AIM Framework (Reach, Efficacy, Adoption, Implementation, Maintenance) to evaluate the integration of HIV prevention services into a family planning clinic over 6 months. Before the integration, PrEP was not offered. We implemented a staff training program on HIV PrEP. We determined the proportion of women presenting to the clinic who were screened, eligible for, and initiated PrEP through chart review. We assessed staff comfort with PrEP pre- and post-integration. We compared planned and actual implementation, interviewed staff to determine barriers and facilitators, and tracked systems adaptations. We assessed maintenance of PrEP after the study concluded. There were 640 clinical encounters for 515 patients; the rate of HIV counseling and PrEP screening was 50%. The rate was 10% in month 1 and peaked to 65% in month 3. Nearly all screened patients were eligible for PrEP (98.4%) and 15 patients (6%) initiated PrEP. Staff knowledge and comfort discussing PrEP improved after education. Facilitators included partnering with local experts, continuing education, clinical tools for providers, and patient education materials. Barriers included competing priorities during clinical encounters, limited woman-centered patient education materials, and insurance-related barriers. Embedding HIV prevention services in the family planning setting was feasible in this pilot. The proportion of women screened for PrEP rapidly increased. In this high HIV prevalence community, nearly all screened women were eligible and 6% initiated PrEP.
Keywords: HIV prevention, PrEP, women, family planning, implementation
Introduction
Despite representing 20% of new HIV cases in the United States, women represent less than 5% of HIV pre-exposure prophylaxis (PrEP) users.1–3 High-risk sexual activities that increase risk for HIV also increase risk for unintended pregnancy, leading women to seek care in family planning clinics. Women's health and HIV prevention experts have called for increasing access to HIV prevention and PrEP in settings that provide family planning services to women.4–6
PrEP with daily tenofovir/emtricitabine (Truvada®) reduces transmission of HIV by up to 92%.7–9 CDC and American College of Obstetricians and Gynecologists (ACOG) recommend HIV PrEP for women who “engage in sexual activity in a high prevalence area” and inconsistently use condoms.10,11 Yet, local and state efforts to curb the HIV epidemic in the United States have not consistently translated into offering PrEP more widely to high-risk cisgender women.
Despite the synergies in offering PrEP alongside contraception, pregnancy termination, and sexually transmitted infection (STI) services, most family planning clinics do not offer PrEP. In 2016, Seidman et al. demonstrated low levels of PrEP knowledge and comfort prescribing PrEP among family planning providers. Most providers reported interest in learning about PrEP and the majority of family planning patients reported they would consider using PrEP, but providers reported multiple barriers to PrEP provision, including insufficient provider education, patient costs, and time constraints.12 While suggestions have been made regarding implementation of PrEP for women,6 the feasibility, facilitators, and barriers to the integration of HIV PrEP services in family planning settings have not been systematically investigated.
We aimed to evaluate the feasibility and impact of integrating HIV PrEP services with family planning services using the RE-AIM Framework. RE-AIM is a widely accepted framework used to assess the feasibility, quality, and public health impact of a health intervention.13 The framework includes five dimensions: Reach intended population, Efficacy or effectiveness, Adoption by target staff, settings, or institutions, Implementation consistency and adaptations, and Maintenance of the intervention over time.13,14 We hypothesized that most family planning patients in a high-prevalence community would be eligible for PrEP and that some patients would be interested in initiating PrEP. We hypothesized that the integration would be feasible and that RE-AIM analysis would identify barriers and facilitators to PrEP integration.
Methods
Study design and setting
We conducted a 6-month prospective cohort study, including clinic staff and female patients at MedStar Washington Hospital Center's Family Planning and Preventative Care clinic (FPPC), from September 2017 to March 2018. FPPC is an outpatient family planning clinic within an urban tertiary care hospital in Washington, DC. FPPC is a training site for fellows, medical students, and residents in family planning, obstetrics/gynecology, family medicine, and pediatrics offering comprehensive reproductive health care for women, including contraception, abortion, STI testing and treatment, and gynecology. The majority of FPPC patients are younger than 30 years, African American, and publicly insured. Most self-refer for abortion and contraceptive services. Clinical services are not offered to male partners because the clinic is staffed by gynecologists. Before the study, PrEP was not offered to FPPC patients. IRB approval was obtained from MedStar Health Research Institute.
We developed a staff and provider training program before the integration of PrEP services. Providers (physicians) and staff (nurses, medical assistants, and receptionists) were independently trained by a local HIV PrEP expert, who was additionally available for questions and phone consultations. Providers were trained to counsel, prescribe, and follow-up patients who initiated PrEP. Family planning patients were to be verbally screened for PrEP during the history-taking portion of the encounter and offered initiation if eligible based on CDC recommendations (Table 1). Patients interested in PrEP but unable to initiate through our clinic due to insurance barriers or patient preference were linked to local PrEP clinics and were included in the study as participants who did not initiate PrEP.
Table 1.
| Substantial HIV risk | Sexual partner with HIV |
| Recent bacterial STD | |
| High number of sex partners | |
| History of inconsistent or no condom use | |
| Commercial sex work | |
| Lives in high-prevalence area or network | |
| Clinical eligibility | Documented negative HIV test before prescribing PrEP |
| No signs/symptoms of acute HIV infection | |
| Normal renal function, no contraindicated medications | |
| Documented hepatitis B virus infection and vaccination status |
PrEP, pre-exposure prophylaxis.
One week after training was completed, universal HIV prevention and PrEP integration were implemented. All patients were exposed to a 5-min video on PrEP (www.whatisprep.org)15 in the waiting room, following which providers assessed risk factors for HIV and discussed HIV prevention. Patients choosing to initiate PrEP completed same-day laboratories, were provided a 30-day prescription, and scheduled for a follow-up appointment in 4 weeks, at which time their HIV test was repeated and a 3-month supply of PrEP was prescribed. Quarterly follow-ups were subsequently scheduled. Women interested but not ready to initiate PrEP were offered another appointment to discuss HIV prevention.
We administered quantitative surveys and qualitative interviews to staff and providers before training (N = 8), immediately post-training (N = 8), and 1 (N = 7), 3 (N = 6), and 6 months (N = 6) post-training. The written anonymous multi-choice survey was administered by a research coordinator and assessed staff and provider self-rated knowledge, attitudes, efficacy, and experience with PrEP. All quantitative survey items used 5-point Likert scales. Semistructured interviews were administered individually by the research coordinator and assessed satisfaction with implementation, perceived barriers and facilitators to PrEP implementation, and suggestions for improvement.
Outcomes
Constructs, outcomes, measures, and data sources are summarized in Table 2.
Table 2.
RE-AIM Constructs and Analysis Plan
| Construct | Definition | Outcomes | Measures | Data source |
|---|---|---|---|---|
| Reach | Individual-level measure of participation | Proportion and characteristics of women counseled on HIV prevention and screened for PrEP eligibility | Number of encounters | EMR |
| Number of patients served | EMR | |||
| Patient characteristics | EMR | |||
| Proportion of patients counseled | EMR | |||
| Proportion of counseled patients eligible for PrEP | EMR | |||
| Effectiveness | Achievement of program goals and objectives | Patient uptake of PrEP | Proportion of patients who initiated PREP | EMR |
| PrEP continuation rate | One-month PrEP follow-up rate | EMR | ||
| Staff and provider perception | Staff and provider knowledge of PrEP | Quantitative survey | ||
| Provider experience prescribing PrEP | Quantitative survey | |||
| Provider comfort prescribing PrEP | Quantitative survey | |||
| Adoption | Assessment of the delivery setting | Description of the setting | Proportion of staff and providers who participated in the intervention | Training log and quantitative survey |
| Description of actual vs. planned implementation | Training and implementation logs | |||
| Barriers and facilitators to adoption | Qualitative interviews | |||
| Implementation | Extent to which the intervention is delivered | Adherence to the planned intervention | Trends in patient counseling and screening | EMR |
| Description of adaptations | Implementation log and qualitative interviews | |||
| Maintenance | Institutionalization of the program | Adherence to the planned integration beyond the study time period | Current provider assessment of program integration | Qualitative provider comments |
| Staff and provider satisfaction with the integration | Qualitative interviews |
EMR, electronic medical record; PrEP, pre-exposure prophylaxis.
Reach
We determined the number of clinical encounters and individuals seen for family planning visits during the study by reviewing the schedule in the electronic medical record (EMR). We reviewed the EMR for family planning patient encounters during the study period to extract data on age, race, ethnicity, and visit type (pregnancy termination, contraception, or other). We assessed the proportion of patients screened for PrEP by reviewing the clinical documentation.
Effectiveness
We evaluated the proportion of patients who initiated and continued PrEP by reviewing electronic prescriptions for PrEP and follow-up appointments for PrEP, respectively.
Adoption
We documented adherence to the planned training schedule. We determined the proportion of staff and providers who attended planned training through attendance logs. We assessed facilitators and barriers to the adoption of HIV prevention integration through surveys and interviews of staff and providers.
Implementation
The program goal was to offer universal HIV prevention counseling and PrEP eligibility screening. We logged adaptations and improvements made to the planned integration.
Maintenance
We surveyed and interviewed staff and providers to identify barriers to long-term integration of the program and to assess provider satisfaction. We describe ongoing adaptations made to the program.
Analysis
We performed descriptive analysis of the RE-AIM outcomes described above. We assessed the association between patient characteristics, screening rates, and eligibility for PrEP using chi-square and Fisher's exact tests. Statistical analysis was performed using Stata 14.2 (StataCorp LLC, College Park, TX, 2015). Qualitative data were recorded, transcribed, and deidentified. Qualitative data were examined for common themes, but thematic saturation was not expected due to the small sample size.
Results
Reach
There were 640 clinical encounters for 515 patients. Patients were predominately African American and >75% presented for abortion services (Table 3). Half (n = 252) were counseled on HIV prevention and screened for PrEP eligibility. Women who are African American race and those seeking abortion services were more likely to be screened for PrEP eligibility compared with all patients (58.1% and 51.3%, p < 0.005).
Table 3.
Demographics, Reason for Care, and Pre-Exposure Prophylaxis Screening Among Women Presenting for Care at a Family Planning Clinic in Washington, DC
| Overall (N = 515) | Screened (n = 252) | Not screened (n = 263) | p | |
|---|---|---|---|---|
| Age in years | 28.9 ± 7.5 | 27.6 ± 6.5 | 30.3 ± 8.1 | <0.005 |
| Race | <0.005 | |||
| African American | 344 (66.8) | 200 (58.1) | 144 (41.9) | |
| White | 62 (12) | 11 (17.7) | 51 (82.3) | |
| Other/multiracial | 90 (17.5) | 32 (35.6) | 58 (64.4) | |
| Unknown | 19 (3.7) | 9 (47.4) | 10 (52.6) | |
| Ethnicity Hispanic/Latina | 40 (7.7) | 36 (32.5) | 27 (67.5) | 0.09 |
| Reason for visit | N = 640 | n = 271 | n = 369 | <0.005 |
| Abortion | 486 (75.9) | 249 (51.3) | 236 (48.7) | |
| Miscarriage | 33 (5.2) | 13 (39.4) | 20 (60.6) | |
| Contraception | 82 (12.8) | 8 (9.8) | 74 (90.2) | |
| Other gynecologic care | 40 (6.3) | 1 (2.5) | 39 (97.5) |
N = 515 patients except where specified. Age presented as mean ± SD. All other data presented as n (%).
Effectiveness
Four physicians, two medical assistants, and two nurses completed the baseline survey (N = 8). Seven of eight were very comfortable discussing sexual health and risk reduction with female patients. Seven of eight had heard of PrEP. None was previously trained on PrEP, prescribed PrEP, or referred a patient for PrEP. Self-reported knowledge of PrEP was poor or fair for all participants. Mean comfort screening for PrEP eligibility was 3.25 on a 5-point Likert scale (1 = very uncomfortable, 5 = very comfortable). The most common perceived barriers to offering PrEP were staffing and time constraints, lack of training, lack of institution clinical guidelines, and insurance coverage.
At month 3, knowledge of PrEP was rated as good or very good for all respondents (N = 6). Mean comfort screening for PrEP eligibility was 4.3 on a 5-point scale. Mean physician comfort prescribing PrEP increased from 1.5 at baseline to 3 on a 5-point Likert scale (n = 3). All surveyed physicians had discussed PrEP with patients and two of three had prescribed PrEP. The majority of respondents agreed that all providers should be trained to counsel and prescribe PrEP. By 6 months, five of six respondents reported good or very good knowledge of PrEP, mean comfort screening for PrEP eligibility decreased to 3.2, and mean physician (n = 3) comfort prescribing PrEP decreased to 2.7.
Nearly all screened patients were eligible for PrEP (98.4%), all due to no or inconsistent condom use in a high-prevalence area. Fifteen patients (6%) initiated PrEP and three (1%) continued its use beyond 1 month.
Adoption
All staff and providers participated in the initial planned training, although not all completed research surveys. A theme that emerged during interviews was the request for additional training, especially during 3- and 6-month interviews. Planned pharmacy and billing training was not completed. Instead, providers were trained on billing- and pharmacy-related barriers to PrEP initiation and compliance.
Facilitators to adopting the integration of PrEP services included the development of tools that served as reference guides for providers (“job aids”). Staff mentioned the benefit of having patients watch the PrEP video in the waiting room, stating it oriented patients to PrEP and facilitated efficient discussions with providers.
Two systems barriers were identified by staff: insurance coverage and the need for ongoing training. Many patients seeking abortion services paid out-of-pocket and our clinic was not within their insurance network. Thus, the baseline laboratories required for PrEP initiation would not be covered by insurance if completed in our clinic. Patients with DC Medicaid were required to obtain their PrEP at specific pharmacies, so a list of participating pharmacies was provided to these patients. The difficulty of providing consistent training to rotating residents and medical students, as well as newly hired staff, was also a barrier. A suggestion was that a single provider should be designated as a “PrEP expert” or “champion” who would address complicated questions about PrEP and provide PrEP follow-up.
Other barriers included time constraints, lack of on-site psychosocial support for risk reduction and adherence counseling, sensitivity to the emotional needs of patients seeking abortion, and the importance of addressing the patient's primary reason for the visit rather than HIV prevention. We could find no high-quality printed PrEP education materials for cisgender women at the initiation of the study. By the 6-month time point, ACOG had developed patient education materials on PrEP, which we utilized.
Implementation
Before implementation, women seeking care at FPPC were not routinely counseled on HIV prevention and none was offered PrEP. During the 6-month pilot, 50% of patients were screened for PrEP eligibility, rapidly increasing from 10% in the first month and peaking at 65% in the third and fourth months. Screening then decreased slightly (Fig. 1).
FIG. 1.
Trends in counseling on HIV prevention and PrEP eligibility at a family planning clinic in Washington, DC during the 6-month PrEP Integration Program. PrEP, pre-exposure prophylaxis.
The program underwent several adaptations. Follow-up training was developed and offered through teleconference with all providers and staff participating. Training was developed for newly hired staff. Formal training was offered to medical students and residents, but they could seldom attend due to schedule conflicts. One physician in the clinic provided brief PrEP training to rotating medical students and residents, but this was implemented inconsistently. Job aids outlined PrEP initiation procedures (e.g., laboratory orders, prescription details, and contraindications) and billing codes while “quick-texts” standardized documentation. Similar tools were developed for PrEP follow-up appointments. The patient intake form was revised to include an item assessing the patient's interest in discussing HIV prevention. Contraceptive option videos were looped with the PrEP video because some patients complained that the video repeated too frequently.
Maintenance
We continue to discuss HIV prevention with a majority of patients presenting for family planning services, facilitated by the updated intake form. New residents, students, and office staff are educated on the office protocols and reminded to counsel patients. Insurance coverage remains a barrier and we give women without in-network insurance coverage the ACOG brochure on PrEP and written referral information.
Discussion
This study systematically evaluated the integration of comprehensive HIV prevention services, including PrEP, in a family planning setting that primarily serves cisgender women. Staff and providers were eager to learn about PrEP and demonstrated improved knowledge and self-efficacy discussing and prescribing PrEP after training. Involvement of a local PrEP expert strengthened collaborations between sexual and reproductive health clinics, facilitated a referral process, and allowed family planning providers to develop a new skill set. PrEP counseling and screening grew rapidly in the first 3 months of implementation, with a peak screening rate of 65%.
We identified multiple facilitators to offering PrEP in our family planning clinic. Ongoing training was perceived as critical for staff and providers. This is consistent with national research demonstrating that lack of education and training is a major barrier to PrEP implementation.12 Clinical tools such as job aids, order sets, and documentation aids improved efficiency for providers. Education materials in the waiting room prepared patients for discussions about HIV prevention. Data from family planning clinics in Georgia suggest that women want waiting-room materials on PrEP, such as brochures and posters, and that 39% wanted doctors to initiate discussions on PrEP.16 Woman-centered PrEP materials continue to be developed and a list of patient and provider resources can be found at hiveonline.org. It was also suggested that one clinician be identified as the “PrEP Champion,” to take the lead in addressing systems issues.
Lack of insurance coverage due to being out of network was consistently identified as an insurmountable barrier to PrEP uptake for interested patients at our location. We referred these patients to a nearby clinic. This is likely to be an issue in similar settings where patients pay out of pocket for sexual and reproductive health services. Insurance coverage of PrEP prescription was not a barrier; however, patients with Medicaid required referral to specific pharmacies. Insurance- and pharmacy-related issues illustrate a few of the structural barriers and biases in PrEP access. We hypothesize that decreased reported PrEP knowledge and confidence among providers at 6 months were due to turnover in trainees and staff. This reflects a missed opportunity for resident training on HIV prevention and PrEP and highlights the importance of training new providers, especially in sites with high turnover. Finally, providers questioned if discussing PrEP during visits sought for contraception and abortion was patient centered.
Limitations of our study include the single site, small sample size, and the 6-month time line. It is unknown whether universally screening and offering PrEP would significantly impact the workflow in high-volume clinics. Six months is a short time frame in which to assess implementation, and thus, factors related to maintenance are not fully explored. We reviewed EMR documentation of counseling and PrEP eligibility to assess the screening rate, which would not account for counseling that occurred but was not documented. We hypothesize that the increased rate of screening among African American women and women seeking abortion was related to an increased risk perception by providers, but we did not assess reasons for nonscreening or the impact of bias among providers. Inequitable access to PrEP due to provider bias based on patient sociodemographic characteristics has been documented among both physicians and medical students.17,18 We also did not follow-up patients who were referred elsewhere for PrEP initiation.
Much remains unknown about the cascade of PrEP uptake for cisgender women. Prior research indicates that the majority of women attending family planning clinics who are at risk for HIV are interested in learning about PrEP.19–22 Our PrEP initiation rate was 6% and only three participants continued PrEP beyond 1 month, suggesting a disconnect between PrEP interest and utilization of PrEP. We hypothesize that many high-risk women are interested in PrEP but perceive that the barriers to PrEP use outweigh the benefits. Future research should investigate the cascade of events leading to PrEP initiation, continuation, and adherence among women and how family planning providers can better support PrEP uptake among interested women.
In this pilot, embedding comprehensive HIV prevention and PrEP services into family planning clinics was feasible and well received by staff and providers. Based on our experience, we developed a list of practices that support offering comprehensive HIV prevention in women's health clinics (Table 4). Family planning clinics that provide abortion and contraception in high HIV prevalence areas are an ideal setting for PrEP provision, given that they predominantly serve women who are eligible for and would benefit from PrEP.
Table 4.
Practices That Support Integrating Comprehensive HIV Prevention Services into Family Planning Clinics
| Cultivation of relationships with local PrEP experts and organizations providing HIV prevention services |
| Development of a referral process for patients who need to initiate PrEP elsewhere due to insurance barriers |
| Development of a PrEP training program for staff and providers, implemented at regular intervals Incorporation of PrEP training into on-boarding for staff, providers, and trainees |
| Assessment of insurance coverage and insurance networks of the patient population to anticipate insurance-related barriers |
| Utilization of woman-centered PrEP patient education materials |
| Designation of a “PrEP Champion” to lead systems initiatives and manage more complicated PrEP clinical scenarios |
PrEP, pre-exposure prophylaxis.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Research reported in this publication was supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001409. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1. Wu H, Mendoza MCB, Huang YA, Hayes T, Smith DK, Hoover KW. Uptake of HIV preexposure prophylaxis among commercially insured persons—United States, 2010–2014. Clin Infect Dis 2017;64:144–149 [DOI] [PubMed] [Google Scholar]
- 2. Marcus JL, Hurley LB, Hare MCB, Silverberg MJ, Volk JE. Disparities in uptake of HIV preexposure prophylaxis in a large integrated health care system. Am J Public Health 2016;106:e2–e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol 2018;28:841–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bradley ELP, Hoover KW. Improving HIV preexposure prophylaxis implementation for women: Summary of key findings from a discussion series with women's HIV prevention experts. Womens Health Issues 2019;29:3–7 [DOI] [PubMed] [Google Scholar]
- 5. Aaron E, Blum C, Seidman D, et al. Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care STDS 2018;32:16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Seidman D, Weber S, Carlson K, Witt J. Family planning providers' role in offering PrEP to women. Contraception 2018;97:467–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Murnane PM, Celum C, Mugo N, et al. Efficacy of preexposure prophylaxis for HIV-1 prevention among high-risk heterosexuals: subgroup analyses from a randomized trial. AIDS 2013;27:2155–2160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med 2012;367:399–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med 2012;367:423–434 [DOI] [PubMed] [Google Scholar]
- 10. CDC. HIV in the United States: At a glance [Internet]. HIV/AIDS, Statistics Center. 2016. [cited December 28, 2016]. Available at: www.cdc.gov/hiv/statistics/overview/ataglance.html
- 11. Committee on Gynecologic Practices. ACOG Committee Opinion no 595: Preexposure prophylaxis for the prevention of human immunodeficiency virus. Obstet Gynecol 2014;123:1133–1136 [DOI] [PubMed] [Google Scholar]
- 12. Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers' knowledge of and attitudes towards pre-exposure prophylaxis for HIV prevention: A national survey. Contraception 2016;93:463–469 [DOI] [PubMed] [Google Scholar]
- 13. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the re-aim framework. Am J Public Health 1999;89:1322–1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kessler RS, Purcell EP, Glasgow RE, Kesges LM, Benkeser RM, Peek CJ. What does it mean to “employ” the RE-AIM model? Eval Health Prof 2013;36:44–66 [DOI] [PubMed] [Google Scholar]
- 15. Pre-Exposure Prophylaxis. What is PrEP. YouTube. [Published February 2014]. Available at: https://www.youtube.com/channel/UCDaazwMAbb8t7r6jYbUU2rA
- 16. Sales JM, Phillips AL, Tamler I, Munoz T, Cwiak C, Sheth AN. Patient recommendations for PrEP information dissemination at family planning clinics in Atlanta, Georgia. Contraception 2019;99:233–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Calabrese SK, Tekest M, Mayer KH, et al. Considering stigma in the provision of HIV pre-exposure prophylaxis: Reflections from current prescribers. AIDS Patient Care STDS 2019;33:79–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Calabrese SK, Earnshaw VA, Underhill K, et al. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): Assumptions about sexual risk compensation and implications for access. AIDS Behav 2014;18:226–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS 2015;29:102–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, Decker MR. Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care 2017;29:751–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Seidman D, Cipres D, Rodriguez A, Alvarez J, Stern L. Women's knowledge of, interest in, and eligibility for HIV pre-exposure prophylaxis at family planning clinics in Northern California. Oral abstract # OA16.04. Research for prevention. Chicago IL, 2016. 10.1089/aid.2016.5000.abstracts [DOI] [Google Scholar]
- 22. Scott R, Brant A, Dhillon P, Coleman M, Ye P, Lotke P, Hull S. Knowledge and acceptability of HIV preexposure prophylaxis (PrEP) among women presenting for family planning services in a high-prevalence community. Contraception 2018;98:368–369 [Google Scholar]
- 23. CDC. Pre-exposure prophylaxis (PrEP) for HIV prevention [Internet]. May 2014. [cited June 12, 2019]. Available at: www.cdc.gov/hiv/pdf/PrEP_fact_sheet_final.pdf