Abstract
Background: Little is known about factors that affect a family's ability to engage in pediatric weight management clinics (PWMCs). We aimed at comparing child and family characteristics of patients referred to a PWMC by participants' attendance at orientation, attendance at intake, or completing the program.
Methods: We performed a retrospective study of patients ages 2–18 years referred to a PWMC between 2014 and 2017. We extracted data from electronic medical records and clinic databases, including age, sex, race/ethnicity, language, referral year, address, and insurance. We performed t-tests and chi-square tests to examine the association of engagement outcomes with covariates. We used separate multivariate logistic regression models to assess the predictors of engagement outcomes, including significant covariates from bivariate analyses.
Results: Participants (N = 2020 referred) had a mean age of 11.5 ± 3.5 years; 72% had Medicaid, and 34% lived in city limits. Participants were 39% white, 30% black, and 27% Hispanic. Of those referred, 41% attended orientation, 14% attended intake, and 9% completed. Significant predictors of attending orientation were age [odds ratio (OR): 0.93, 95% confidence interval (CI): 0.91–0.96], male sex (OR: 0.74, 95% CI: 0.60–0.91), Hispanic ethnicity (OR: 1.69, 95% CI: 1.26–2.26), living in city limits (OR: 1.39, 95% CI: 1.11–1.75), and Medicaid (OR: 0.77, 95% CI: 0.60–0.98). Significant predictors of attending intake were age (OR: 0.93, 95% CI: 0.90–0.96), Medicaid (OR: 0.61, 95% CI: 0.46–0.81), and 2017 referral year (OR: 0.21, 95% CI: 0.12–0.35). Hispanic ethnicity was associated with twice the odds of completion (OR: 2.07, 95% CI: 1.10–3.91).
Conclusions: Child and family characteristics more strongly predicted initial engagement with a PWMC than completion. Future research should examine how targeting these predictors (e.g., referring at younger age) can improve PWMC engagement.
Keywords: attrition, children, engagement, obesity, referral
Introduction
Rates of obesity among children and adolescents remain high in the United States, and the prevalence of severe obesity continues to increase.1 For children with obesity, the American Academy of Pediatrics recommends that the first stage of treatment, Prevention Plus, focuses on healthy lifestyle activities and is typically delivered by the child's primary care provider (PCP).2 The second stage, structured weight management, often involves additional support for counseling and goal-setting beyond the PCP, and the third stage, comprehensive multidisciplinary intervention, recommends referral by the PCP to a pediatric weight management clinic (PWMC). PWMCs use a multidisciplinary team, individualized goal setting, and a medium- to high-intensity structured program involving both the child and their family.
Nobles et al. have proposed an “engagement pathway” in which the time after referral to a PWMC is followed by an enrollment stage, in which families either initiate participation in the program or do not.3 Families who are “intenders” want to initiate treatment, and some may not actually enroll due to external factors such as cost, transportation, or health problems. Families are “initiators” if they successfully act on their intention to begin treatment. The enrollment stage is followed by the intervention and maintenance stages, in which families can either attend and adhere, or drop out. It is considered attrition if participants drop out and remain disengaged from the program, or participants can re-engage with the program during this stage. Much research has been done examining predictors of attrition in families enrolled in a PWMC. Demographics associated with increased attrition from PWMC include male sex, African American race, Medicaid insurance, and increased age.4–7 However, little is known about the predictors of treatment initiation in a PWMC. Therefore, we aimed at describing child and family characteristics of the patients referred to our institution's PWMC based on whether participants attended a program orientation, attended an intake visit, and completed the program.
Methods
Study Overview
We performed a retrospective chart review of 2020 patients ages 2–18 years old referred to our institution's PWMC, Brenner FIT®, between January 1, 2014 and July 31, 2017. This time frame was chosen, as these were the dates in which our program utilized a paper referral form that was sent from the referring providers to Brenner FIT. Data extraction was performed in November 2018. Patients are referred to Brenner FIT most often from their PCPs, but may be referred by any community provider. Referrals may be faxed or sent through our electronic medical record (EMR). Once patients are referred, their information is collected in a clinical database. Two attempts are made by Brenner FIT in the family's preferred language to contact the family by phone to schedule an orientation; a voicemail is left if they do not answer. If unable to reach the family after two attempts, a letter is mailed asking them to call and schedule the orientation. This study was approved by the Institutional Review Board at Wake Forest School of Medicine. Informed consent and assent were waived, as this was a retrospective study.
Brenner FIT (Families in Training)
Brenner FIT is an interdisciplinary, family-centered, pediatric weight management program in Northwest North Carolina, and it is a part of Brenner Children's Hospital and Wake Forest Baptist Medical Center. Throughout the program, families meet regularly with a pediatrician, family counselor, dietitian, physical therapist, and exercise specialist. The treatment team uses motivational interviewing to assist families in identifying unhealthy habits and setting realistic goals for changing behaviors. Participants who live farther away can chose to complete visits in person with the team at our clinic in Winston-Salem, NC or to participate in the telemedicine program, in which most visits are performed at one of the 10 telemedicine sites throughout Western NC. In addition, families who speak Spanish are placed on a treatment team with primarily Spanish-speaking providers. Further details of the Brenner FIT program have been previously described.8,9
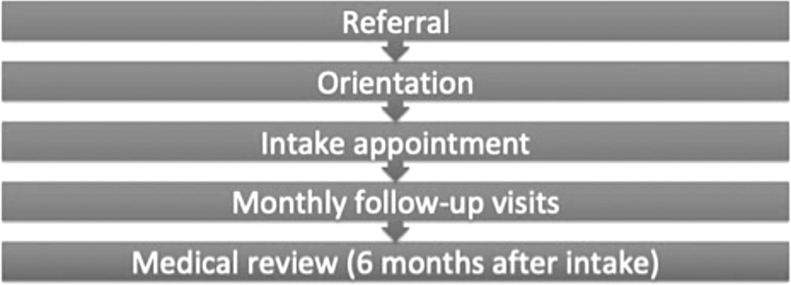
Children ages 2–18 years are referred and seen if they have obesity (have a BMI ≥95th percentile for age and sex) and have one or more obesity-related medical comorbidities or have a BMI ≥99th percentile. After attending a group orientation, patients are scheduled for an individual intake appointment with the team. Families participate in visits with their treatment team every 3–4 weeks over the next 6 months (six treatment visits), and they then attend a medical review visit with the physician to assess treatment progress. Patients who attend the 6-month review visit are considered to have completed the program, although some families elect to continue team visits for another 6 months or longer (Fig. 1).
Figure 1.
Brenner FIT engagement pathway.
Data Extraction
Data were extracted from both the program database and the EMR. Data extracted from the program database included child's age, sex, race, ethnicity, primary language, insurance status, date of referral, date of orientation attendance, date of intake visit, and date of 6-month medical review visit (as applicable). Data extracted from the EMR included child's visit dates, height, and weight. Of note, EMR data were not available on all participants referred to the program and were only used in this analysis for participants who completed an intake visit. Anthropometrics (extracted from the EMR) and participation in the telemedicine program (extracted from the program database) were only available for participants who attended intake.
Statistical Analysis
Intake height and weight were used to calculate BMI, and then BMI percentiles and percent of the 95th percentile were calculated by using the CDC SAS program to generate sex- and age-specific percentiles. We used t-tests and chi-square tests to examine the association of engagement outcomes (attending orientation, intake, and 6-month medical review visits) with covariates. We used separate multivariate logistic regression models to assess the predictors of whether referred patients attended an orientation, intake, or 6-month review visits, adjusting for significant covariates from bivariate analyses. Of note, the covariates of participation the telemedicine program and percent of the 95th BMI percentile were only included in the models for 6-month review visits, as this information was only available for those who completed an intake visit. We also used separate multivariate logistic regression models to assess whether the time to orientation and intake were associated with the odds of attending subsequent visits, adjusting for the same covariates as described earlier. Analyses were performed by using Stata v14.
Results
Of the 2020 patients referred to Brenner FIT between January 1, 2014 and July 31, 2017, 821 patients attended an orientation visit, 286 attended an intake visit, and 172 completed a 6-month medical review visit. The number of referrals increased with each subsequent year. Referred children were a mean of 11.5 years old (standard deviation 3.5) and were 39% non-Hispanic white, 30% non-Hispanic black, and 27% Hispanic. Most were Medicaid insured (72%), had a parent who spoke English as their primary language (75%), and lived outside of the Winston–Salem city limits (66%). Of those who attended intake, a minority of families (19%) participated in the telemedicine program (Table 1).
Table 1.
Participant Characteristics at Time of Referral by Primary Care Provider and at Brenner FIT Intake Visit
| Variable | n (%) |
|---|---|
| Characteristics at referral | |
| Age (years), mean (SD) | 11.5 (3.5) |
| Male sex | 781 (45.9) |
| Race/ethnicity | |
| White | 657 (39.1) |
| Black | 496 (29.5) |
| Hispanic | 452 (26.9) |
| Other | 75 (4.5) |
| Primary language | |
| English | 1276 (75.0) |
| Spanish | 412 (24.2) |
| Referral year | |
| 2014 | 534 (26.4) |
| 2015 | 555 (27.5) |
| 2016 | 647 (32.0) |
| 2017 | 284 (14.1) |
| Lives in city limits | 746 (34.1) |
| Medicaid insurance | 1106 (72.4) |
| Characteristics at intake | |
| Telemedicine participation | 74 (18.8) |
| BMI: % of 95th percentile, mean (SD) | 143.6 (86.5) |
SD, standard deviation.
Families were less likely to attend an orientation if the child was older [odds ratio (OR): 0.93, 95% confidence interval (CI): 0.91–0.96), male (OR: 0.74, 95% CI: 0.60–0.91), and Medicaid insured (OR: 0.77, 95% CI: 0.60–0.98). Families were more likely to attend orientation if the child was Hispanic (OR: 1.69, 95% CI: 1.26–2.26) and if the family lived within city limits (OR: 1.39, 95% CI: 1.11–1.75). Similar results were seen for correlates of attending intake visits (Table 2), except that referral year of 2017 was also significantly associated (OR: 0.21, 95% CI: 0.12–0.35) and male sex, Hispanic ethnicity, and living in the city limits were not significantly associated. Hispanic ethnicity was associated with twice the odds of completing the 6-month medical review visit (Table 2).
Table 2.
Logistic Regression Results Reporting Predictors of Attendance at Orientation, Attendance at Intake Visit, and Completion of the Program, Including Child and Family Characteristics
| Variable | Model 1: Attending orientation, OR (95% CI) | Model 2: Attending intake, OR (95% CI) | Model 3: Completing program, OR (95% CI) |
|---|---|---|---|
| Age (years) | 0.93 (0.91–0.96)*** | 0.93 (0.90–0.96)* | 0.97 (0.90–1.04) |
| Male sex | 0.74 (0.60–0.91)** | 0.79 (0.62–1.00) | 0.82 (0.52–1.29) |
| Race/ethnicity | |||
| White | Ref. | Ref. | Ref. |
| Black | 0.87 (0.66–1.15) | 1.12 (0.82–1.53) | 1.01 (0.56–1.80) |
| Hispanic | 1.69 (1.26–2.26)*** | 1.05 (0.75–1.48) | 2.07 (1.10–3.91)* |
| Other | 1.19 (0.68–2.07) | 1.20 (0.63–2.27) | 1.66 (0.54–3.91) |
| Referral year | |||
| 2014 | Ref | Ref | Ref |
| 2015 | 0.97 (0.74–1.28) | 0.92 (0.68–1.24) | 0.88 (0.52–1.51) |
| 2016 | 1.14 (0.86–1.50) | 0.87 (0.64 – 1.18) | 0.80 (0.46–1.39) |
| 2017 | 0.75 (0.53–1.05) | 0.21 (0.12–0.35)*** | 0.34 (0.09–0.1.28) |
| Lives in city limits | 1.39 (1.11–1.75)** | 1.05 (0.80–1.36) | 1.11 (0.67–1.87) |
| Medicaid | 0.77 (0.60–0.98)* | 0.61 (0.46–0.81)** | 0.81 (0.49–1.35) |
| Telemedicine | — | — | 0.80 (0.42–1.54) |
| BMI: % of the 95th percentile | — | — | 0.99 (0.98–1.01) |
Denotes p < 0.05, **p < 0.01, ***p < 0.001. Bold indicates statistically significant results.
CI, confidence interval; OR, odds ratio.
Increased time (each additional month) between referral and the family attending orientation was associated with decreased odds of attending an intake visit (OR: 0.90, 95% CI: 0.89–0.92). Increased time between referral and the family attending intake predicted decreased odds of attending a 6-month medical review visit (OR: 0.93, 95% CI: 0.88–0.98), but the time between referral and orientation was no longer a significant predictor (Table 3).
Table 3.
Logistic Regression Results Reporting Predictors of Attendance at Intake Visit and Completion of the Program, Including Child and Family Characteristics and Time after Referral
| Variable | Model 1: Intake, OR (95% CI) | Model 2: Complete, OR (95% CI) |
|---|---|---|
| Referral to orientation time (months) | 0.90 (0.89–0.92)*** | 1.01 (0.98–1.03) |
| Referral to intake time (months) | — | 0.93 (0.88–0.98)** |
| Age (years) | 0.96 (0.91–0.99)* | 0.95 (0.89–1.03) |
| Male sex | 0.96 (0.72–1.29) | 0.80 (0.50–1.26) |
| Race/ethnicity | ||
| White | Ref | Ref |
| Black | 1.46 (0.98–2.15) | 1.08 (0.59–1.96) |
| Hispanic | 0.79 (0.52–1.18) | 2.74 (1.40–5.38)** |
| Other | 1.27 (0.57–2.85) | 1.64 (0.53–5.09) |
| Referral year | ||
| 2014 | Ref | Ref |
| 2015 | 0.85 (0.58–1.22) | 0.83 (0.48–1.44) |
| 2016 | 0.64 (0.44–0.94)* | 0.70 (0.40–1.25) |
| 2017 | 0.15 (0.08–0.26)*** | 0.28 (0.07–2.05) |
| Lives in city limits | 0.80 (0.58–1.09) | 1.12 (0.66–1.89) |
| Medicaid | 0.61 (0.43–0.86)** | 0.83 (0.50–1.39) |
| Telemedicine | — | 0.81 (0.42–1.58) |
| BMI: % of the 95th percentile | — | 0.99 (0.98–1.01) |
Denotes p < 0.05, **p < 0.01, ***p < 0.001. Bold indicates statistically significant results.
Discussion
Child and family characteristics more strongly predicted the family's initiation of engagement with the PWMC than completion of the program. Families were less likely to attend orientation and intake if the child was older, male, and Medicaid insured. Hispanic families were more likely to attend orientation and to complete the program. In our program, native-Spanish speaking team members work with those families, not relying on interpreters, which we believe improves retention. Almost all Hispanic families (∼92%) chose to participate in the program in-person (compared with 80% of non-Hispanic white families and 76% of non-Hispanic black families).
Three studies have examined predictors of initial attendance in obesity treatment,10 two of these examining community-based obesity treatment programs11,12 and one a pilot study of a randomized controlled trial.13 These studies all found that boys were less likely to enroll than girls. In our program, male children were also less likely to attend orientation and intake; however, the attrition literature is less clear on this factor.14 Our finding that older children and children who received Medicaid insurance were less likely to engage in care at PWMC is consistent with most literature in attrition from PWMC.14 It is possible that older children have other commitments (sports, school activities, jobs, etc.) that make engagement difficult, or may hold perceptions of stigma about PWMC that make participation unappealing to the child. Adolescent autonomy likely contributes to this lack of engagement, as their participation in treatment is of greater importance compared with younger children. Families with children on Medicaid insurance may have difficulties getting to appointments due to working hours, inability to take time off, or transportation difficulties that make engagement challenging. Our finding that Hispanic families were more likely to engage with and complete participation in the PWMC is also consistent with attrition literature demonstrating that Hispanic parents and parents who spoke Spanish were more likely to complete recommended treatment.15 Similarly, the use of telemedicine programs has been associated with decreased attrition from PWMC as well.8,16
Although strengthened by our large sample size, diverse patient population, and inclusion of patients who were referred but never seen by a PWMC, our study does have limitations. All data are from referrals to a single tertiary care pediatric weight management program and may not be applicable to all programs. Though more than a year elapsed between when the last referrals were placed for our inclusion criteria and the time of data extraction, yet patients referred in 2017 had less time to engage with the weight management program compared with previous years, which may explain why these patients were less likely to attend orientation or intake. In addition, because we relied on information from the EMR and referral form, other important contributors to engagement and attrition were not examined, such as scheduling,17 transportation barriers,17 parent mental health,18 family conflict,19 and family feeding practices.19 Future qualitative work should focus on evaluating barriers and facilitators to engagement among patients referred to PWMC. Finally, we defined engagement in the program by attendance at a visit, but true engagement in a program is more complex and future work should examine the degree of involvement in the program after attendance.3
Based on our findings, providers should consider referring younger children when appropriate, as these families were more likely to engage. PWMCs should also consider outreach opportunities and introduction of telemedicine options for orientation for families living outside of city limits, as these families were less likely to establish engagement with the program. PWMCs that can expedite time between referral and intake may improve likelihood of maintaining longer engagement with families, as this was associated with increasing the odds of completing the 6-month review. Child and family characteristics were more strongly predictive of initial engagement in our PWMC (orientation and intake) than completion of the program, which may be due to the personalized and family-centered nature of the program. Providers making referrals to PWMC should be aware of risk factors for families not engaging in the program and should be proactive about helping families address barriers to participation.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding Information
Data extraction for the project described was provided by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Skinner AC, Ravanbakht SN, Skelton JA, et al. . Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018;141:e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spear BA, Barlow SE, Ervin C, et al. . Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007;120(Suppl. 4):S254–S288 [DOI] [PubMed] [Google Scholar]
- 3. Nobles JD, Perez A, Skelton JA, et al. . The engagement pathway: A conceptual framework of engagement-related terms in weight management. Obes Res Clin Pract 2018;12:133–138 [DOI] [PubMed] [Google Scholar]
- 4. Skelton JA, Beech BM. Attrition in paediatric weight management: A review of the literature and new directions. Obes Rev 2011;12:e273–e281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cote MP, Byczkowski T, Kotagal U, et al. . Service quality and attrition: An examination of a pediatric obesity program. Int J Qual Health Care 2004;16:165–173 [DOI] [PubMed] [Google Scholar]
- 6. Heinberg LJ, Kutchman EM, Berger NA, et al. . Parent involvement is associated with early success in obesity treatment. Clin Pediatr (Phila) 2010;49:457–465 [DOI] [PubMed] [Google Scholar]
- 7. Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr 2006;45:355–360 [DOI] [PubMed] [Google Scholar]
- 8. Guzman A, Irby MB, Pulgar C, et al. . Adapting a tertiary-care pediatric weight management clinic to better reach Spanish-speaking families. J Immigr Minor Health 2012;14:512–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Irby MB, Boles KA, Jordan C, et al. . TeleFIT: Adapting a multidisciplinary, tertiary-care pediatric obesity clinic to rural populations. Telemed J Ehealth 2012;18:247–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kelleher E, Davoren MP, Harrington JM, et al. . Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: A systematic review. Obes Rev 2017;18:183–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fagg J, Cole TJ, Cummins S, et al. . After the RCT: Who comes to a family-based intervention for childhood overweight or obesity when it is implemented at scale in the community? J Epidemiol Community Health 2015;69:142–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Welsby D, Nguyen B, O'Hara BJ, et al. . Process evaluation of an up-scaled community based child obesity treatment program: NSW Go4Fun®. BMC Public Health 2014;14:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O'Connor T, Hilmers A, Watson K, et al. . Feasibility of an obesity intervention for paediatric primary care targeting parenting and children: Helping HAND. Child Care Health Dev 2013;39:141–149 [DOI] [PubMed] [Google Scholar]
- 14. Dhaliwal J, Nosworthy NM, Holt NL, et al. . Attrition and the management of pediatric obesity: An integrative review. Childhood Obes 2014;10:461–473 [DOI] [PubMed] [Google Scholar]
- 15. Hampl SE, Borner KB, Dean KM, et al. . Patient attendance and outcomes in a structured weight management program. J Pediatr 2016;176:30–35 [DOI] [PubMed] [Google Scholar]
- 16. Davis AM, Sampilo M, Gallagher KS, et al. . Treating rural paediatric obesity through telemedicine vs. telephone: Outcomes from a cluster randomized controlled trial. J Telemed Telecare 2016;22:86–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hampl S, Demeule M, Eneli I, et al. . Parent perspectives on attrition from tertiary care pediatric weight management programs. Clin Pediatr 2013;52:513–519 [DOI] [PubMed] [Google Scholar]
- 18. Braden AL, Madowitz J, Matheson BE, et al. . Parent binge eating and depressive symptoms as predictors of attrition in a family-based treatment for pediatric obesity. Childhood Obes 2015;11:165–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Byrd-Bredbenner C, Delaney C, Martin-Biggers J, et al. . The marketing plan and outcome indicators for recruiting and retaining parents in the HomeStyles randomized controlled trial. Trials 2017;18:540. [DOI] [PMC free article] [PubMed] [Google Scholar]