Abstract
Substance use problems undermine HIV treatment and secondary prevention efforts. Research is needed to better understand predictors of substance use among people living with HIV (PLWH). We examined whether internalized stigma and enacted HIV stigma are associated with three indicators of substance use among PLWH, including numbers of (1) substances used, (2) substances used at moderate to high risk, and (3) times substances were used before sex, through the mediator of depressive symptoms. Participants included 358 PLWH aged 18–35 years from Georgia, United States. At baseline, participants completed measures of internalized and enacted stigma, depressive symptoms, and substance use severity. Substance use was additionally tested with urinalysis. Following baseline, participants reported their use of substances before sex for 28 days through daily text messaging. Data were analyzed using path analysis in R. On average, participants tested positive for 1.24 (range: 0–6) substances used, reported moderate to high risk on 2.01 (range: 0–8) substances, and reported using substances 1.57 (range: 0–20) times before sex over 28 days. Internalized stigma and enacted stigma were associated with greater depressive symptoms, and depressive symptoms were associated with all three indicators of substance use. Moreover, the indirect effects between internalized and enacted stigma with indicators of substance use were significant, suggesting that depressive symptoms partially mediated associations between stigma and substance use. Interventions may be needed to address both stigma and depressive symptoms among PLWH to reduce substance use and support HIV treatment and prevention efforts.
Keywords: addiction, depression, HIV, substance use, stigma
Introduction
In the United States, people living with HIV (PLWH) are affected by substance use problems at higher rates than people not living with HIV.1 In addition to harming overall mental and physical health,2 substance use problems undermine HIV treatment and secondary prevention efforts. Cannabis, alcohol, and opioid use problems are associated with lower adherence to antiretroviral therapy,3–5 tobacco use with coinfections such as bacterial pneumonia and tuberculosis,6,7 and cocaine use with faster HIV progression.8 Alcohol and methamphetamine use is associated with behaviors that increase risk of HIV transmission such as condomless sex and sexual marathons.9,10 Research identifying risk factors for substance use among PLWH is needed to strengthen HIV treatment and prevention efforts.
HIV stigma plays a role in a wide range of negative health behaviors and outcomes among PLWH11–14 and may play a role in substance use. Internalized stigma, or endorsing negative beliefs and feelings associated with HIV and applying them to the self, is related to greater avoidant coping and feelings of helplessness, longer gaps in HIV care, and lower likelihood of antiretroviral therapy initiation.15,16 Enacted stigma, or experiencing discrimination from others due to one's HIV, is related to greater stress and more missed HIV clinic appointments.17,18 Growing literatures have established associations between sexual and gender minority19–22 and race-based23–25 stigma with substance use. In comparison, fewer studies have examined associations between HIV stigma and substance use. Quantitative studies to date show associations of internalized HIV stigma with hazardous drinking26 and enacted HIV stigma with frequency of illicit drug use.27 Yet, other work on associations between HIV stigma and substance use has been mixed.28,29 To build a more comprehensive understanding of HIV stigma and substance use, additional research is needed to explore associations between multiple stigma mechanisms and multiple indicators of substance use.
There have been increasing calls to identify modifiable psychosocial variables that mediate associations between stigma and negative health behaviors among PLWH14 because they can be intervened upon to disrupt the impact of stigma on health. Depressive symptoms may mediate associations between HIV stigma and substance use given evidence demonstrating that both internalized stigma and enacted stigma are associated with greater depressive symptoms30–32 and that depressive symptoms are associated with greater substance use.33 Evidence of this pathway additionally comes from qualitative work wherein PLWH have reported engaging in substance use to cope with the negative mental health effects of stigma.34
In the current study, we examined whether internalized and enacted HIV stigma are associated with three key indicators of substance use among PLWH, including numbers of (1) substances used, (2) substances used at moderate to high risk, and (3) times substances were used before sex over the course of a month. Additionally, we explored whether depressive symptoms mediated these associations.
Methods
Participants and procedures
The current study was conducted as part of a lead-in study for a larger behavioral intervention trial to improve access to health care. PLWH were recruited through social media advertisements, flyers at social service agencies, and participant referrals. Interested individuals contacted a study recruiter through instant message or phone. Individuals were eligible to enroll if they were 18–35 years old (inclusive), living with HIV, and have a cell phone. They provided documentation of HIV status through medical records or by providing a saliva sample for rapid antibody testing. Written informed consent was provided. At baseline, participants completed self-report measures and submitted a urine sample for toxicology testing. For the following 28 days, they reported on their sexual behaviors in response to daily text messages. Study procedures received Institutional Review Board approval from the University of Connecticut. The current analyses focus on 358 participants from the lead-in study.
Measures
Three measures of substance use were collected and coded to indicate substance use. First, two toxicology tests were conducted on urine samples collected at baseline. The Reditest Panel-Dip from Redwood Toxicology Laboratory35 assessed for 12 substances used in the past 6 h to 4 weeks (range varied by substance), including cannabis, cocaine, methamphetamine, amphetamine, benzodiazepine, ecstasy, opioids, oxycodone, phencyclidine, methadone, propoxyphene, and barbiturates. The EtG Alcohol Urine Test Dip Card (300 ng/mL cutoff) from Medical Dimensions36 assessed for alcohol used in the past 80 h. A sum of positive results spanning both tests was created for each participant, indicating the number of substances used. Second, participants completed the World Health Organization's Alcohol, Smoking, and Substance Involvement Screening Test 3.0 (ASSIST).37,38 The ASSIST screens for substance use severity in the past 3 months, including cannabis, tobacco, alcohol, cocaine, inhalants, amphetamine, sedatives, hallucinogens, opioids, and other drugs. Participants were additionally screened for severity of methamphetamine and erectile dysfunction medication use for a total of 12 substances screened. The World Health Organization recommends brief intervention or more intensive treatment for participants scoring at moderate or high risk, respectively. A sum of substances used at moderate or high risk was therefore created for each participant. Third, participants responded to daily text messages regarding their substance use and sexual behaviors for a period of 28 days following baseline. Each day, they reported whether they drank or used drugs before having sex on the previous day. A sum of times substances were used before sex in the previous month was created.
Participants additionally responded to self-report measures at baseline. Measures of internalized and enacted stigma were adapted from the HIV Stigma Mechanism Measure,15 with additional items generated based on preliminary data. Internalized stigma was measured with six items, including “I think less of myself because I have HIV.” Response options ranged from strongly disagree (1) to strongly agree (6). A mean score was created (Cronbach's α = 0.91). Enacted stigma was measured with 24 items, including “How often have people treated you differently because of your HIV status?” Response options ranged from never (0) to often (3). A mean score was created (Cronbach's α = 0.94). Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D).39 Items included “I was bothered by things that usually don't bother me,” and response options included 0 days (0), 1–2 days (1), 3–4 days (2), and 5–7 days (3). A sum score was created (Cronbach's α = 0.80). Scores above 16 are considered clinically significant in identifying depression. Participants also indicated several sociodemographic and HIV-related characteristics, including their gender identity, race/ethnicity, and number of years living with HIV.
Analysis strategy
First, descriptive statistics were explored to characterize participants' sociodemographic characteristics, experiences of stigma, depressive symptoms, and substance use severity. Second, bivariate correlations between stigma, depressive symptoms, and indicators of substance use severity were examined. Third, hypotheses were tested using path analysis in R40 with the OpenMX package.41 Path analysis accounts for associations between multiple indicators of substance use (which were expected to be correlated) and provides estimates of indirect effects between independent and dependent variables through mediating variables.42 We determined the parameter estimates with diagonally weighted least squares (DWLS) due to the non-normality and count nature of our data. The DWLS procedure uses the full weight matrix to compute robust standard errors (SEs) and a mean- and variance-adjusted test statistic.43,44 The adequacy of model fit was determined by several statistics: comparative fit index (CFI) >90, Tucker–Lewis index (TLI) >90, and root mean square error of approximation (RMSEA) <0.06.
Results
As shown in Table 1, most participants identified as men and African American or black and had been living with HIV for an average of 6.60 years (standard deviation [SD] = 1.13). Participants tested positive for an average of 1.24 substances used (SD = 1.13, range: 0–6), reported moderate to high risk on an average of 2.01 substances (SD = 1.60, range: 0–8), and reported using substances an average of 1.57 times before sex over 28 days (SD = 2.95, range: 0–20). On average, participants reported low internalized stigma, infrequent experiences of enacted stigma, and depressive symptoms above the threshold for clinical significance.
Table 1.
Participant Characteristics, n = 358
| % (n) | M (SD) | Range | |
|---|---|---|---|
| Sociodemographics | |||
| Gender identity | |||
| Man | 89.1 (319) | ||
| Woman | 7.3 (26) | ||
| Transgender man | 0.6 (2) | ||
| Transgender woman | 2.2 (8) | ||
| Other | 0.9 (3) | ||
| Race/ethnicity | |||
| White | 2.2 (8) | ||
| African American or black | 86.6 (310) | ||
| Hispanic or Latino(a) | 9.2 (33) | ||
| Asian or Pacific Islander | 2.0 (7) | ||
| Years living with HIV | 6.60 (5.33) | 0–32 | |
| Substance use | |||
| # Substances used | 1.24 (1.13) | 0–6 | |
| Cannabis | 57.9 (208) | ||
| Alcohol | 24.2 (87) | ||
| Cocaine | 11.4 (41) | ||
| Methamphetamine | 9.7 (35) | ||
| Amphetamine | 8.1 (29) | ||
| Benzodiazepine | 4.2 (15) | ||
| Ecstasy (MDMA) | 3.1 (11) | ||
| Opioids | 1.9 (7) | ||
| Oxycodone | 1.4 (5) | ||
| Phencyclidine (PCP) | 0.6 (2) | ||
| Methadone | 0.6 (2) | ||
| Propoxyphene | 0.0 (0) | ||
| Barbiturates | 0.0 (0) | ||
| # Substances used at moderate or high risk | 2.01 (1.60) | 0–8 | |
| Cannabis | 57.9 (208) | ||
| Tobacco | 54.0 (194) | ||
| Alcohol | 33.4 (120) | ||
| Cocaine | 16.2 (58) | ||
| Inhalants | 13.1 (47) | ||
| Methamphetamine | 8.9 (32) | ||
| Amphetamine | 7.5 (27) | ||
| Sedatives | 2.8 (10) | ||
| Erectile dysfunction medication | 2.8 (10) | ||
| Other | 1.7 (6) | ||
| Hallucinogens | 1.1 (4) | ||
| Opioids | 0.9 (3) | ||
| # Times substances were used before sex in a month | 1.57 (2.95) | 0–20 | |
| Stigma | |||
| Internalized | 2.74 (1.58) | 1–6 | |
| Enacted | 0.45 (0.51) | 0–2.83 | |
| Depressive symptoms | 23.29 (8.98) | 0–46 | |
SD, standard deviation.
As shown in Table 2, internalized stigma and enacted stigma were positively correlated with each other and depressive symptoms. Depressive symptoms were positively correlated with the numbers of substances used and substances used at moderate to high risk. Depressive symptoms were positively correlated with the number of times substances were used before sex, but this correlation did not reach statistical significance (p = 0.08). Moreover, all indicators of substance use were correlated with each other.
Table 2.
Correlations Between Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Internalized stigma | — | |||||
| 2. Enacted stigma | 0.49** | — | ||||
| 3. Depressive symptoms | 0.31** | 0.39** | — | |||
| 4. # Substances used at moderate or high risk | 0.08 | 0.15** | 0.21** | — | ||
| 5. # Substances used | −0.05 | 0.03 | 0.14** | 0.52** | — | |
| 6. # Times substances were used before sex | −0.02 | 0.03 | 0.09+ | 0.41** | 0.29** | — |
p < 0.10; **p < 0.01.
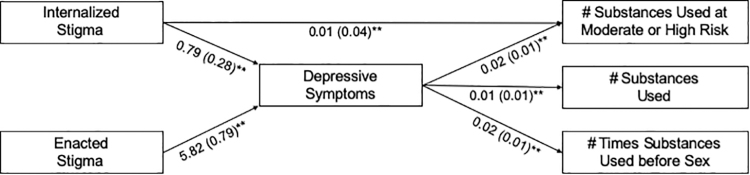
As shown in Fig. 1, internalized stigma and enacted stigma were associated with greater depressive symptoms. In turn, depressive symptoms were associated with greater numbers of substances used, substances used at moderate or high risk, and times substances were used before sex. Positive and statistically significant indirect effects through depressive symptoms were observed between internalized stigma and numbers of substances used [B (SE) = 0.02 (0.01), p = 0.03] and substances used at moderate or high risk [B (SE) = 0.02 (0.01), p = 0.02]. A positive, but nonsignificant, indirect effect was observed between internalized stigma and the number of times substances were used before sex [B (SE) = 0.01 (0.01), p = 0.06]. Additionally, positive and statistically significant indirect effects were observed through depressive symptoms between enacted stigma and numbers of substances used [B (SE) = 0.12 (0.04), p ≤ 0.01], substances used at moderate or high risk [B (SE) = 0.13 (0.04), p ≤ 0.01], and times substances were used before sex [B (SE) = 0.09 (0.04), p = 0.01]. Of the sociodemographic variables included in the path analysis as controls (i.e., gender identity, race/ethnicity, and years living with HIV), only male gender identity was associated with a variable included in the model. Participants identifying as men reported a greater number of substances used at moderate or high risk [B (SE) = 0.51 (0.22), p = 0.02]. All other associations with sociodemographic variables were nonstatistically significant. The path model demonstrated adequate fit to the data (RMSEA = 0.10, p = 0.02; CFI = 0.97, TLI = 0.93). Model fit was slightly diminished due to the inclusion of nonstatistically significant control variables within the model.
FIG. 1.
Results of path analysis. B (standard error) displayed; **p < 0.01; analyses controlled for gender identity, race/ethnicity, and years living with HIV.
Discussion
Results of the current study suggest that HIV stigma is related to substance use among PLWH. Specifically, internalized and enacted HIV stigma were associated with greater numbers of substances used and substances used at moderate or high risk, and enacted stigma was associated with a greater number of times substances were used before sex. Moreover, results provide insight into the processes whereby HIV stigma relates to substance use. Depressive symptoms partially mediated associations between both internalized stigma and enacted stigma with indicators of substance use.
Strengths of the study involve the inclusion of two HIV stigma mechanisms and three indicators of substance use. Stigma mechanisms span stigma directed toward the self and experienced from others, and substance use indicators span those with implications for HIV treatment (i.e., substances used at moderate to high risk) and prevention (i.e., substances used before sex). Indicators of substance use included a biological measure and a prospective measure, strengthening confidence in the validity of results. Taken together, results suggest that the association between HIV stigma and substance use is both robust and multifaceted. Future work may expand on these findings by including additional measures of HIV stigma mechanisms (e.g., anticipated stigma), accounting for intersectionality of stigma experiences (e.g., racism), and adopting more nuanced indicators of substance use (e.g., latent profiles indicating severity of substance use).
Limitations of the study involve the cross-sectional measurement of HIV stigma with depressive symptoms and two indicators of substance use. Past longitudinal studies suggest that experiences of HIV stigma predict subsequent depressive symptoms30,31 and depressive symptoms predict subsequent substance use.45 Yet, longitudinal studies also suggest that substance use may predict subsequent depressive symptoms46 and depressive symptoms may predict subsequent internalized stigma.47 Cyclical relationships between stigma, depressive symptoms, and substance use may exist. Future work examining these associations should adopt scientifically rigorous longitudinal approaches to elucidate causal, and possible cyclical, paths between them. Longitudinal studies should also include additional measures of substance use, such as the amount and types of substances used per day. The sample included mostly black men living with HIV. This is an important population to study given that black men are disproportionately affected by HIV in the United States. Yet, future studies should include more diverse samples, including people who may not own a cell phone, to explore the generalizability of these findings.
The current study draws attention to the role of HIV stigma in substance use. It may be important to address HIV stigma within interventions to prevent and treat substance use problems among PLWH. Researchers have identified efficacious strategies to reduce stigma that targets PLWH (e.g., expressive writing and cognitive behavioral therapy), community members (e.g., intergroup contact and education), and structures and organizations (e.g., policy change and mass media campaigns).48,49 In the midst of a substance use crisis in the United States, research is needed to continue to understand why substance use problems develop among PLWH, how they affect HIV treatment and prevention efforts, and how to best intervene in them.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was supported by the National Institute on Drug Abuse (NIDA; R01DA043068, K01DA042881, K01DA047918), National Institute of Allergy and Infectious Diseases (T32AI102623), and National Institute on Alcohol Abuse and Alcoholism (K24AA022136). Funders were not involved in the study design; collection, analysis, or interpretation of data; write up of the report; or decision to submit the article for publication.
References
- 1. Substance Abuse and Mental Health Services Administration. The National Survey on Drug Use and Health Report: HIV/AIDS and Substance Use. Rockville MD; 2010. Available at: https://www.samhsa.gov/sites/default/files/hiv-aids-and-substance-use.pdf (Last accessed September24, 2019).
- 2. Office of the Surgeon General. Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health. Washington, D.C.; 2016. Available at: https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf (Last accessed September24, 2019). [Google Scholar]
- 3. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy, and health care utilization. Drug Alcohol Depend 2010;112:178–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bonn-Miller MO, Oser ML, Bucossi MM, Trafton JA. Cannabis use and HIV antiretroviral therapy adherence and HIV-related symptoms. J Behav Med 2014;37:1–10 [DOI] [PubMed] [Google Scholar]
- 5. Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet 2010;376:367–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gordin FM, Roediger MP, Girard P, et al. Pneumonia in HIV-infected persons: Increased risk with cigarette smoking and treatment interruption. Am J Respir Crit Care Med 2008;178:630–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Browning KK, Wewers ME, Ferketich A, Diaz P. Tobacco use and cessation in HIV-infected individuals. Clin Chest Med 2013;34:181–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baum MK, Rafie C, Lai S, Sales S, Page B, Campa A. Crack—Cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. J Acquir Immune Defic Syndr 2009;50:93–99 [DOI] [PubMed] [Google Scholar]
- 9. Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: Review and meta-analysis. AIDS Behav 2009;13:1021–1036 [DOI] [PubMed] [Google Scholar]
- 10. Semple SJ, Zians J, Strathdee SA, Patterson TL. Sexual marathons and methamphetamine use among HIV-positive men who have sex with men. Arch Sex Behav 2009;38:583–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav 2009;13:1160–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J Int AIDS Soc 2013;16(Suupl 2):18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open 2016;6:e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV medication adherence: A systematic review and synthesis of the literature. AIDS Behav 2016;20:29–50 [DOI] [PubMed] [Google Scholar]
- 15. Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: A test of the HIV Stigma Framework. AIDS Behav 2013;17:1785–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Earnshaw VA, Bogart LM, Laurenceau J-P, et al. Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: Exploring avoidant coping as a longitudinal mediator. J Int AIDS Soc 2018;21:e25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Earnshaw VA, Lang SM, Lippitt M, Jin H, Chaudoir SR. HIV stigma and physical health symptoms: Do social support, adaptive coping, and/or identity centrality act as resilience resources? AIDS Behav 2015;19:41–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bird ST, Bogart LM, Delahanty DL. Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care STDS 2004;18:19–26 [DOI] [PubMed] [Google Scholar]
- 19. McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am J Public Health 2010;100:1946–1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. J Sex Res 2015;52:243–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reisner SL, Pardo ST, Gamarel KE, Hughto JMW, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among U.S. female-to-male trans masculine adults. LGBT Health 2015;2:324–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med 2009;32:20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol 2006;35:888–901 [DOI] [PubMed] [Google Scholar]
- 25. Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med 2013;95:115–127 [DOI] [PubMed] [Google Scholar]
- 26. Felker-Kantor EA, Wallace ME, Madkour AS, Duncan DT, Andrinopoulos K, Theall K. HIV stigma, mental health, and alcohol use disorders among people living with HIV/AIDS in New Orleans. J Urban Health 2019;96:878–888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Glynn TR, Llabre MM, Lee JS, et al. Pathways to health: An examination of HIV-related stigma, life stressors, depression, and substance use. Int J Behav Med 2019;26:286–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lunze K, Lioznov D, Cheng DM, et al. HIV stigma and unhealthy alcohol use among people living with HIV in Russia. AIDS Behav 2017;21:2609–2617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Earnshaw VA, Kidman RC, Violari A. Stigma, depression, and substance use problems among perinatally HIV-infected youth in South Africa. AIDS Behav 2018;22:3892–3896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS 2019;33:571–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kemp CG, Lipira L, Huh D, et al. HIV stigma and viral load among African-American women receiving treatment for HIV. AIDS 2019;33:1511–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among Black men with HIV. Cultur Divers Ethnic Minor Psychol 2011;17:295–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Berg CJ, Michelson SE, Safren SA. Behavioral aspects of HIV care: Adherence, depression, substance use, and HIV-transmission behaviors. Infect Dis Clin North Am 2007;21:181–200 [DOI] [PubMed] [Google Scholar]
- 34. Edelman EJ, Cole CA, Richardson W, Boshnack N, Jenkins H, Rosenthal MS. Stigma, substance use and sexual risk behaviors among HIV-infected men who have sex with men: A qualitative study. Prev Med Rep 2016;3:296–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Redwood Toxicology Laboratory. Panel-Dip Drug Screen. Available at: https://www.redwoodtoxicology.com/devices/doa_panel-dip (Last accessed September24, 2019)
- 36. Medical Dimensions. Urine Drug Testing Kits. Available at: http://medicaldimensions.us/urine-drug-testing-kits/ (Last accessed September24, 2019)
- 37. World Health Organization ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction 2002;97:1183–1194 [DOI] [PubMed] [Google Scholar]
- 38. World Health Organization ASSIST Working Group. The ASSIST screening test version 3.0 and feedback card. Available at: https://www.who.int/substance_abuse/activities/assist_test/en/ (Last accessed August21, 2019)
- 39. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 40. R Core Team. R: The R Project for Statistical Computing. Available at: https://www.r-project.org/ (Last accessed September24, 2019)
- 41. Neale MC, Hunter MD, Pritikin JN, et al. OpenMx 2.0: Extended structural equation and statistical modeling. Psychometrika 2016;81:535–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shipley B. Cause and Correlation in Biology: A User's Guide to Path Analysis, Structural Equations and Causal Inference with R. Cambridge, UK: Cambridge University Press, 2016 [Google Scholar]
- 43. Joreskog KG. New developments in LISREL: Analysis of ordinal variables using polychoric correlations and weighted least squares. Qual Quant 1990;24:387–404 [Google Scholar]
- 44. Distefano C, Morgan GB. A comparison of diagonal weighted least squares robust estimation techniques for ordinal data. Struct Equ Modeling 2014;21:425–438 [Google Scholar]
- 45. Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat 2016;37:127–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lev-Ran S, Roerecke M, Le Foll B, George TP, Mckenzie K, Rehm J. The association between cannabis use and depression: A systematic review and meta-analysis of longitudinal studies. Psychol Med 2019;44:797–810 [DOI] [PubMed] [Google Scholar]
- 47. Earnshaw VA, Reed NM, Watson RJ, Maksut JL, Allen AM, Eaton LA. Intersectional internalized stigma among Black gay and bisexual men: A longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol January 1, 2019. DOI: 10.1177/1359105318820101 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: A multilevel approach to stigma and public health. Soc Sci Med 2014;103:101–109 [DOI] [PubMed] [Google Scholar]
- 49. Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, Go VF. A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Med 2019;17:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]