Abstract
BACKGROUND
Transjugular intrahepatic portosystemic shunt (TIPS), splenectomy plus esophagogastric devascularization (SED) and endoscopic therapy + non-selective β-blockers (ET + NSBB) are widely applied in secondary prevention of recurrent gastroesophageal variceal bleeding in patients with liver cirrhosis. These different treatments, however, have not been compared in patients with idiopathic non-cirrhotic portal hypertension (INCPH).
AIM
To compare the outcomes of TIPS, SED and ET + NSBB in the control of variceal rebleeding in patients with INCPH.
METHODS
This retrospective study recruited patients from six centers across China. Demographic characteristics, baseline profiles and follow-up clinical outcomes were collected. Post-procedural clinical outcomes, including incidence of rebleeding, hepatic encephalopathy (HE), portal vein thrombosis (PVT) and mortality rates, were compared in the different groups.
RESULTS
In total, 81 patients were recruited, with 28 receiving TIPS, 26 SED, and 27 ET + NSBB. No significant differences in demographic and baseline characteristics were found among these three groups before the procedures. After treatment, blood ammonia was significantly higher in the TIPS group; hemoglobin level and platelet count were significantly higher in the SED group (P < 0.01). Rebleeding rate was significantly higher in the ET + NSBB group (P < 0.01). Mortality was 3.6%, 3.8% and 14.8% in the TIPS, SED and ET + NSBB groups, respectively, with no significant differences (P = 0.082). Logistic regression analysis showed that mortality was significantly correlated with rebleeding, HE, portal thrombosis and superior mesenteric vein thrombosis (P < 0.05).
CONCLUSION
In patients with INCPH, TIPS and SED were more effective in controlling rebleeding than ET + NSBB, but survival rates were not significantly different among the three groups. Mortality was significantly correlated with rebleeding, HE and PVT.
Keywords: Idiopathic non-cirrhotic portal hypertension, Transjugular intrahepatic portosystemic shunt, Splenectomy plus esophagogastric devascularization, Endoscopic therapy, Survival
Core tip: This is the first study to compare outcomes of transjugular intrahepatic portosystemic shunt, splenectomy plus esophagogastric devascularization and endoscopic therapy plus non-selective β-blockers in the control of recurrent variceal bleeding in patients with idiopathic non-cirrhotic portal hypertension.
INTRODUCTION
Idiopathic non-cirrhotic portal hypertension (INCPH) is a group of hepatic diseases characterized by portal hypertension (PHT) that occurs in the absence of cirrhosis and with patency of hepatic and extra-hepatic portal veins[1]. The etiology of this disorder is still unknown and differs greatly in western and eastern countries[2]. INCPH may be caused by intestinal infection, human immunodeficiency virus infection, drugs or toxins, genetic disorders as well as immunological or hematological disorders[2]. Pathological changes have been recently described by the International Pathology Study Group: obliteration of portal vein branches with or without thickening of the wall; a portal vein from the portal tract directly abutting the periportal parenchyma; and multiple thin-walled vascular spaces in the portal tract and thin-walled vascular spaces of different caliber outside but in close contact with the portal tract[3].
INCPH can lead to severe clinical complications, including variceal bleeding and sometimes ascites and thrombosis[4]. Although hepatic venous pressure gradient (HVPG) in patients with INCPH is normal or slightly increased, variceal bleeding in these patients can be fatal and needs appropriate treatment. Endoscopic therapy (ET), including endoscopic variceal ligation (EVL) and endoscopic injection sclerotherapy (EIS), with the addition of non-selective β-blockers (NSBBs), remains the prevalent method for treatment and secondary prevention of recurrent gastroesophageal variceal bleeding in patients with INCPH[5]. Transjugular intrahepatic portosystemic shunt (TIPS) is reported to be feasible for management of variceal bleeding in patients with INCPH, and post-TIPS complications are fewer than in patients with cirrhosis[6,7]. Surgery including splenectomy and esophagogastric devascularization (SED) is still widely performed in China and has fewer postoperative complications, such as portal vein thrombosis (PVT), in patients with INCPH compared with patients with cirrhosis[1]. Although these different procedures have been compared in portal hypertension due to cirrhosis, they have not been compared in INCPH.
Therefore, we carried out this retrospective study to compare the outcomes of TIPS, SED and ET + NSBB in controlling recurrent variceal bleeding in patients with INCPH.
MATERIALS AND METHODS
Study patients
From 1 January 2012 to 31 December 2015, all patients diagnosed with INCPH in six centers were retrospectively studied. This study was approved by the Ethics Committee of Beijing Shijitan Hospital, Capital Medical University.
The inclusion criteria were: (1) Variceal bleeding caused by INCPH; (2) Age 18-70 years; and (3) TIPS, SED or ET + NSBB performed after the index variceal bleeding. The patients with one or more of the following characteristics were excluded: (1) Complicated with hepatic, vena cava or portal vein thrombosis; (2) Complicated with malignant tumor in the liver or other sites; and (3) Underwent two or all three procedures of TIPS, SED or ET + NSBB.
Clinical management
All patients were hospitalized due to variceal bleeding. After admission, clinical data and laboratory profiles including routine blood, biochemistry and coagulation function tests were recorded for each patient. Abdominal ultrasonography, computed tomography and liver biopsy were performed. INCPH was diagnosed by clinical manifestations, laboratory tests, imaging examination and liver pathology, as described previously[3].
Therapeutic protocols
TIPS was performed in the Department of Interventional Therapy, Beijing Shijitan Hospital, Capital Medical University and Department of Gastroenterology, Nanjing Drum Tower Hospital. The procedure was performed under local anesthesia or sedation. The right jugular vein was punctured with a 10 F sheath of the Rösch-Uchida Transjugular Liver Access Set (Cook, Bloomington, IN, United States). The puncture needle was advanced from the hepatic vein or vena cava into the portal vein through the liver parenchyma, and a guide wire was placed in the portal vein. The shunt was dilated with an angioplasty balloon of 8 mm diameter and then a covered stent with a diameter of 8 mm was deployed. The varicose coronary gastric vein was embolized to prevent bleeding. Angiography of the portal vein was performed again, and the procedure was completed.
SED was performed in the Department of Hepatobiliary Surgery, The Fifth Medical Center of PLA General Hospital and Department of General Surgery, Beijing Ditan Hospital, Capital Medical University. Between 2012 and 2014, patients received open SED (OSED). In a later phase of the study, due to the progress of surgical techniques, laparoscopic SED (LSED) was performed.
ET + NSBB was performed in the Department of Gastroenterology, Beijing Youan Hospital, Capital Medical University. NSBB was titrated to a dose that decreased heart rate by 25% at rest but still at least 50 beats/min. Elective EVL or EIS was performed 1-2 wk after variceal bleeding and every 2 wk until eradication of varices. Endoscopy was repeated 3 and 6 mo later and EVL or EIS was performed if necessary.
Follow-up of patients
The patients were followed up every 6 mo after the procedures. The clinical data were recorded, and abdominal ultrasonography or computed tomography/magnetic resonance imaging were repeated at each time point. Laboratory investigations were also conducted at each follow-up point. Clinical events including recurrent variceal bleeding, hepatic encephalopathy (HE), PVT, hepatocellular cancer, tumor at other sites, and other complications were recorded. If the patient died before the 3-year follow-up, the clinical data at the last visit were used for analysis.
Statistical analysis
Numerical data were summarized as frequencies, and continuous variables were shown as mean ± standard deviation. Paired-sample t test or χ2 test was used for comparison of numerical or quantitative data. Logistic analysis was used to identify predictors of mortality. Data for survival were analyzed using the Kaplan-Meier method. P < 0.05 was considered to be significant. SPSS for Windows version 17.0 (Chicago, IL, United States) was used for statistical analysis.
RESULTS
Demographic and baseline clinical profiles
From 1 January 2012 to 31 December 2015, 125 patients in six centers were screened, and 81 patients (59 female/22 male) were recruited according to the inclusion and exclusion criteria. Of the 81 patients recruited, 28 patients (20 female/8 male) received TIPS, 26 (19 female/7 male) received SED and 27 (20 female/7 male) received ET + NSBB (P = 0.975).
No significant differences in demographic and baseline characteristics were found among the three groups before the procedures. These included age (P = 0.776), sex (P = 0.975), alanine transaminase (P = 0.874), albumin (P = 0.059), total bilirubin (P = 0.891), prothrombin time (P = 0.903), blood ammonia (P = 0.727), white blood cell count (P = 0.863), hemoglobin (P = 0.559), platelet count (P = 0.889), Child-Pugh score (P = 0.796) and Child-Pugh classification (P = 0.837, 0.848).
Procedure outcomes
TIPS, SED and ET + NSBB were successfully performed in all patients. In the TIPS group, portal pressure gradient decreased from 29.2 ± 6.1 mmHg to 9.7 ± 5.2 mmHg (P < 0.01). Total procedure time was 88.7 min ± 32.2 min. In the SED group, 20 patients underwent OSED, and 6 underwent LSED. The mean operating time for OSED was 126.4 ± 47.2 min, and mean operating time for LSED was 157.7 ± 58.4 min (P = 0.078). In the ET + NSBB group, 27 patients underwent 131 upper endoscopies, including 67 sessions of EVL and eight sessions of EIS. NSBB was given to all patients.
Clinical outcomes and complications
All patients were followed up for 3 years or till death. No significant differences were found in laboratory profiles among the three groups 4 wk after the procedures including alanine transaminase (P = 0.067), albumin (P = 0.101), total bilirubin (P = 0.809), prothrombin time (P = 0.807) and white blood cell count (P = 0.061). However, blood ammonia was significantly higher in the TIPS group (P < 0.01). Hemoglobin level and platelet count increased to normal range in the SED group and were significantly higher than in the TIPS and ET + NSBB groups (P < 0.01).
In the TIPS group, shunt stenosis was found in 4 patients (14.2%), and recanalization was performed in 2 (7.1%). In the TIPS, SED and ET + NSBB groups, the rebleeding rates were 7.1%, 11.5% and 29.6%, respectively (P < 0.01). Rebleeding rate was significantly higher in the ET + NSBB group (P < 0.01), but no significant difference was found between the TIPS and ET + NSBB groups (P = 0.228). HE rate was 14.2%, 3.8% and 3.7% in the TIPS, SED and ET + NSBB groups, respectively, which did not differ significantly among these three groups (P = 0.229).
In the TIPS, SED and ET + NSBB groups, PVT was observed in 1 (3.6%), 5 (19.2%) and 2 patients (7.4%), respectively (P = 0.066), and superior mesenteric vein thrombosis (SMVT) was observed in 1 (3.6%), 3 (11.5%) and 2 patients (7.4%), respectively (P = 0.126). No significant differences were found among the 3 groups.
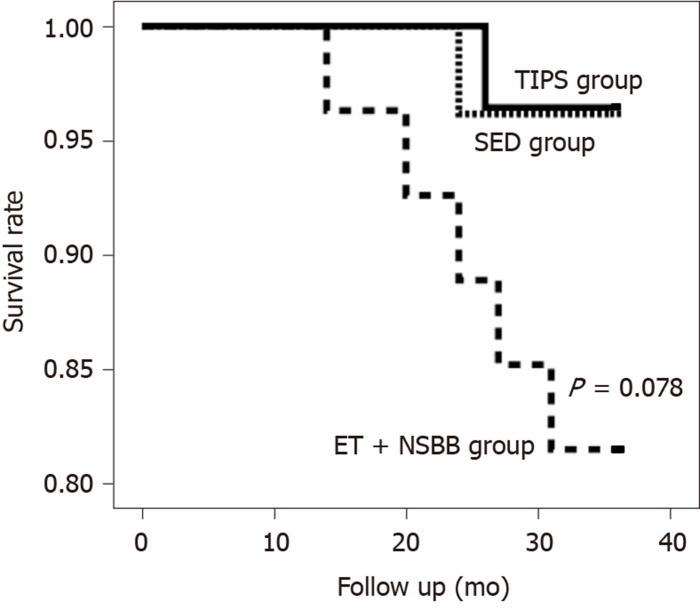
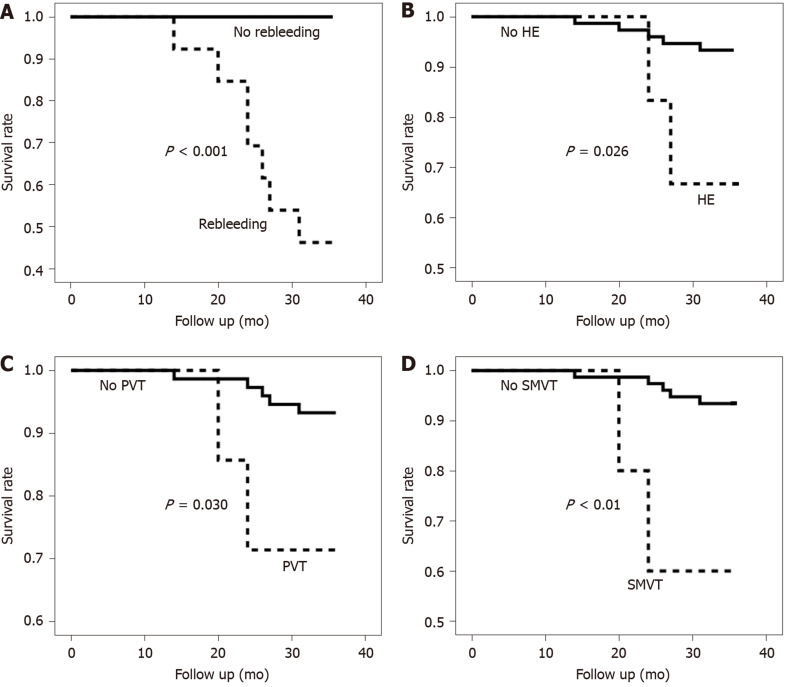
Accumulated mortality was 3.6%, 3.8% and 14.8% in the TIPS, SED and ET + NSBB groups, respectively, with no significant difference among the three groups (P = 0.082). Logistic regression analysis showed that mortality was significantly correlated with rebleeding, HE, PVT and SMVT (P < 0.05). Kaplan-Meier analysis is shown in Figures 1 and 2.
Figure 1.
Kaplan-Meier analysis of survival following idiopathic non-cirrhotic portal hypertension treated with transjugular intrahepatic portosystemic shunt, splenectomy plus esophagogastric devascularization and endoscopic therapy + non-selective β-blockers. TIPS: Transjugular intrahepatic portosystemic shunt; SED: Splenectomy plus esophagogastric devascularization; ET + NSBB: Endoscopic therapy + non-selective β-blockers.
Figure 2.
Kaplan-Meier analysis of survival following idiopathic non-cirrhotic portal hypertension with different complications. A: Rebleeding; B: Hepatic encephalopathy; C: Portal vein thrombosis; D: Superior mesenteric vein thrombosis. HE: Hepatic encephalopathy; PVT: Portal vein thrombosis; SMVT: Superior mesenteric vein thrombosis.
DISCUSSION
This study compared different treatments for controlling variceal bleeding in patients with INCPH. TIPS and SED were superior to ET + NSBB for secondary prevention of variceal bleeding but not in improving survival.
Although TIPS has been compared with ET and SED in patients with PHT due to liver cirrhosis[8,9], different treatment options and outcomes have not been compared in patients with INCPH[6,7]. We found that in patients with INCPH, TIPS and SED were more effective than ET + NSBB, with the latter being recommended as the treatment of choice by most clinical guidelines (Baveno VI).
In the current study, we found that patients with INCPH had better outcomes than patients with cirrhosis because of well-preserved liver function. Death was significantly correlated with variceal rebleeding, HE and PVT. In contrast, previous studies showed that the most common causes of death in patients with cirrhosis were hepatocellular cancer, liver failure and systemic infection[9,10]. This difference may be explained by the fact that liver function is normal or nearly normal, so liver failure is barely observed in patients with INCPH[11].
HE is a common complication of TIPS in patients with cirrhosis. In our study, post-TIPS HE rate in INCPH was significantly lower than that in patients with cirrhosis (up to 50%)[8]. Again, this may also have been caused by better liver function reserve in patients with INCPH than in those with cirrhosis. However, logistic regression analysis did show that HE after TIPS was associated with mortality.
SED has been reported to have similar efficacy for controlling rebleeding as TIPS in patients with Child-Pugh Class A and B cirrhosis[12]. Our study also showed that SED and TIPS had similar efficacy in controlling rebleeding in patients with INCPH, with all of the patients having liver function reserve of Child-Pugh Class A or B.
Postoperative PVT or SMVT is the main limitation of SED, which is still widely performed in China for secondary prophylaxis of variceal bleeding. Thrombosis can occur in 40%-50% patients with cirrhosis after SED, and high risk of PVT might be associated with hypercoagulability[13]. In our study, postoperative thrombosis rate in patients with INCPH was lower than that reported in patients with cirrhosis, and this might be due to normal coagulation and anti-coagulation status in patients with INCPH. However, mortality was significantly correlated with PVT and SMVT, which was higher in the SED group. Therefore, a future study with a larger number of patients may be needed to confirm whether thrombosis is a predictor of mortality.
In conclusion, in patients with INCPH, both TIPS and SED were more effective in controlling rebleeding than ET + NSBB was, but survival rates were not significantly different among the three procedures. Mortality was significantly correlated with rebleeding, HE and PVT.
ARTICLE HIGHLIGHTS
Research background
Different treatment strategies for recurrent gastroesophageal variceal bleeding in patients with liver cirrhosis include transjugular intrahepatic portosystemic shunt (TIPS), splenectomy plus esophagogastric devascularization (SED) and endoscopic therapy + non-selective β-blockers (ET + NSBB). These three treatments have not been compared in idiopathic non-cirrhotic portal hypertension (INCPH).
Research motivation
The motivation of this study was to provide suggestions for clinical practitioners when treating patients with INCPH.
Research objectives
This study compared the outcomes of TIPS, SED and ET + NSBB in the control of variceal rebleeding in patients with INCPH.
Research methods
This study retrospectively recruited patients from six centers across China. Clinical data and outcomes were collected. Complications including incidence of rebleeding, hepatic encephalopathy (HE), portal vein thrombosis (PVT) and mortality rates were compared in different groups.
Research results
Eight-one patients were recruited, with twenty-eight receiving TIPS, twenty-six SED and twenty-seven ET + NSBB. Rebleeding rate was significantly higher in the ET + NSBB group (P < 0.01). Mortality was 3.6%, 3.8% and 14.8% in the TIPS, SED and ET + NSBB groups, respectively, and the differences were not significantly different (P = 0.082). Logistic regression analysis showed that mortality was significantly correlated with rebleeding, HE, portal thrombosis and superior mesenteric vein thrombosis (P < 0.05).
Research conclusions
In patients with INCPH, TIPS and SED were more effective in controlling rebleeding than ET + NSBB, but survival rates were not significantly different among the three groups. Mortality was significantly correlated with rebleeding, HE and PVT.
Research perspectives
This study showed that TIPS and SED were more suitable in controlling rebleeding in patients with INCPH. In the future, more patients should be included and the follow-up period should be prolonged to examine further the long-term results.
Footnotes
Institutional review board statement: This study was reviewed and approved by the Ethics Committee of Beijing Shijitan Hospital, Capital Medical University.
Informed consent statement: All patients signed informed consent to the study.
Conflict-of-interest statement: We have no conflict-of-interest to disclose.
Data sharing statement: No additional data are available.
Manuscript source: Unsolicited manuscript
Peer-review started: February 4, 2020
First decision: March 18, 2020
Article in press: April 15, 2020
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Andrade FT, Elkrief L S-Editor: Wang YQ L-Editor: Filipodia E-Editor: Liu JH
Contributor Information
Fu-Liang He, Department of Hepatology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China.
Rui-Zhao Qi, Department of General Surgery, Fifth Medical Center of PLA General Hospital, Beijing 100039, China.
Yue-Ning Zhang, Department of Gastroenterology, Beijing You’an Hospital, Capital Medical University, Beijing 100069, China.
Ke Zhang, Department of General Surgery, Beijing Ditan Hospital, Capital Medical University, Beijing 100102, China.
Yu-Zheng Zhu-Ge, Department of Gastroenterology, Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School, Nanjing 210008, Jiangsu Province, China.
Min Wang, Department of Hepatology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China.
Yu Wang, Department of Hepatology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China.
Ji-Dong Jia, Department of Hepatology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China.
Fu-Quan Liu, Department of Interventional Therapy, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China. liufq_sjt@163.com.
References
- 1.Elkrief L, Ferrusquia-Acosta J, Payancé A, Moga L, Tellez L, Praktiknjo M, Procopet B, Farcau O, De Lédinghen V, Yuldashev R, Tabchouri N, Barbier L, Dumortier J, Menahem B, Magaz M, Hernández-Gea V, Albillos A, Trebicka J, Spahr L, De Gottardi A, Plessier A, Valla D, Rubbia-Brandt L, Toso C, Bureau C, Garcia-Pagan JC, Rautou PE for VALDIG, an EASL consortium. Abdominal Surgery in Patients With Idiopathic Noncirrhotic Portal Hypertension: A Multicenter Retrospective Study. Hepatology. 2019;70:911–924. doi: 10.1002/hep.30628. [DOI] [PubMed] [Google Scholar]
- 2.Gioia S, Nardelli S, Pasquale C, Pentassuglio I, Nicoletti V, Aprile F, Merli M, Riggio O. Natural history of patients with non cirrhotic portal hypertension: Comparison with patients with compensated cirrhosis. Dig Liver Dis. 2018;50:839–844. doi: 10.1016/j.dld.2018.01.132. [DOI] [PubMed] [Google Scholar]
- 3.Guido M, Alves VAF, Balabaud C, Bathal PS, Bioulac-Sage P, Colombari R, Crawford JM, Dhillon AP, Ferrell LD, Gill RM, Hytiroglou P, Nakanuma Y, Paradis V, Quaglia A, Rautou PE, Theise ND, Thung S, Tsui WMS, Sempoux C, Snover D, van Leeuwen DJ International Liver Pathology Study Group. Histology of portal vascular changes associated with idiopathic non-cirrhotic portal hypertension: nomenclature and definition. Histopathology. 2019;74:219–226. doi: 10.1111/his.13738. [DOI] [PubMed] [Google Scholar]
- 4.Schouten JN, Verheij J, Seijo S. Idiopathic non-cirrhotic portal hypertension: a review. Orphanet J Rare Dis. 2015;10:67. doi: 10.1186/s13023-015-0288-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khanna R, Sarin SK. Noncirrhotic Portal Hypertension: Current and Emerging Perspectives. Clin Liver Dis. 2019;23:781–807. doi: 10.1016/j.cld.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Bissonnette J, Garcia-Pagán JC, Albillos A, Turon F, Ferreira C, Tellez L, Nault JC, Carbonell N, Cervoni JP, Abdel Rehim M, Sibert A, Bouchard L, Perreault P, Trebicka J, Trottier-Tellier F, Rautou PE, Valla DC, Plessier A. Role of the transjugular intrahepatic portosystemic shunt in the management of severe complications of portal hypertension in idiopathic noncirrhotic portal hypertension. Hepatology. 2016;64:224–231. doi: 10.1002/hep.28547. [DOI] [PubMed] [Google Scholar]
- 7.Lv Y, Li K, He C, Luo B, Zhang B, Liu H, Wang Z, Guo W, Wang Q, Chen H, Bai W, Yuan X, Yu T, Li X, Yuan J, Han N, Zhu Y, Niu J, Xie H, Wang J, Chen L, Yin Z, Fan D, Li Z, Han G. TIPSS for variceal bleeding in patients with idiopathic non-cirrhotic portal hypertension: comparison with patients who have cirrhosis. Aliment Pharmacol Ther. 2019;49:926–939. doi: 10.1111/apt.15186. [DOI] [PubMed] [Google Scholar]
- 8.Holster IL, Tjwa ET, Moelker A, Wils A, Hansen BE, Vermeijden JR, Scholten P, van Hoek B, Nicolai JJ, Kuipers EJ, Pattynama PM, van Buuren HR. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding. Hepatology. 2016;63:581–589. doi: 10.1002/hep.28318. [DOI] [PubMed] [Google Scholar]
- 9.Zhou J, Wu Z, Wu J, Wang X, Li Y, Wang M, Yang Z, Peng B, Zhou Z. Transjugular intrahepatic portosystemic shunt (TIPS) versus laparoscopic splenectomy (LS) plus preoperative endoscopic varices ligation (EVL) in the treatment of recurrent variceal bleeding. Surg Endosc. 2013;27:2712–2720. doi: 10.1007/s00464-013-2810-1. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt-Martin D, Armstrong MJ, Rowe IA. Transplant-Free Survival Rates After Covered Transjugular Intrahepatic Portosystemic Shunt. Gastroenterology. 2017;153:869–870. doi: 10.1053/j.gastro.2017.02.051. [DOI] [PubMed] [Google Scholar]
- 11.Zuo C, Chumbalkar V, Ells PF, Bonville DJ, Lee H. Prevalence of histological features of idiopathic noncirrhotic portal hypertension in general population: a retrospective study of incidental liver biopsies. Hepatol Int. 2017;11:452–460. doi: 10.1007/s12072-017-9801-6. [DOI] [PubMed] [Google Scholar]
- 12.Su AP, Zhang ZD, Tian BL, Zhu JQ. Transjugular intrahepatic portosystemic shunt versus open splenectomy and esophagogastric devascularization for portal hypertension with recurrent variceal bleeding. Hepatobiliary Pancreat Dis Int. 2017;16:169–175. doi: 10.1016/s1499-3872(16)60129-7. [DOI] [PubMed] [Google Scholar]
- 13.Wang M, Ding L, Xu M, Xie J, Wu S, Xu S, Yao Y, Liu Q. A novel method detecting the key clinic factors of portal vein system thrombosis of splenectomy & cardia devascularization patients for cirrhosis & portal hypertension. BMC Bioinformatics. 2019;20:720. doi: 10.1186/s12859-019-3233-3. [DOI] [PMC free article] [PubMed] [Google Scholar]