Abstract
The goal of this study was to illustrate the translation of our extant eHealth intervention (VIP) into an mHealth app for persons living with HIV (PLWH) with HIV-Associated non-AIDS (HANA) conditions, a new clinical problem. We integrated different quantitative and qualitative methodologies from different disciplines to accomplish the task of adapting an eHealth system for a new set of clinical problems. Building off of our past development of the VIP website, we used a multimodal, iterative user-centered design process to develop the VIP-HANA app. Our process was used to better understand the needs of a national sample of PLWH recruited online. Findings from the usability evaluation demonstrate a potentially useful and easy to use app. Integration of multi-modal methodologies from different fields to accomplish the tasks of adaptation and evaluation of a mobile app is an appealing, rigorous and useful approach.
Keywords: HIV, Mobile Applications, Symptoms
Introduction
Psychological theories often provide the guiding framework for eHealth interventions, yet the actual development process often relies on developer clairvoyance and the serendipity of the researcher in successfully communicating his/her goals to the software developer. This oftentimes arbitrary process is less than scientific and not ideally suited for efficient, rigorous and reproducible intervention development. The instantiation of behavioral health interventions delivered via technology and the expanded need for translating eHealth tools to a new clinical problem are the impetus for clearly outlining the development process of consumer health informatics tools. The goal of this paper is to illustrate the integration of multi-modal methodologies for adapting an extant intervention for new or growing clinical problems. Our multi-modal iterative development process was comprised of an online web-based survey, expert review, software development, and usability evaluation with experts and end users.
Background
HIV has evolved from an acute to a chronic illness largely due to advances in antiretroviral therapy (ART) [1]. As a result, persons living with HIV (PLWH) are living longer and about 50% of PLWH in the US are currently over 50 years old [2]. As PLWH age, they are developing chronic illnesses and co-morbid conditions at a younger age than individuals who are HIV negative [3, 4]. Fifty to sixty percent of deaths in PLWH occur from HIV associated non-AIDS (HANA) conditions (e.g., cardiovascular disease, liver disease, diabetes, and asthma) and people suffering from these conditions are more likely to be affected by adverse symptoms [5]. An individual’s ability to identify and self-manage symptoms of HIV has been shown to improve patient outcomes and quality of life [6–8]. Consequently, a team of researchers at UCSF School of Nursing developed a paper-based symptom management manual with self-care strategies for 21 common HIV/AIDS symptoms. The efficacy of this manual for improving symptoms was established in a 775-person randomized clinical trial (RCT) over three months at 12 sites [9].
To enhance uptake of these strategies by PLWH, we developed and pilot-tested the Video Information Provider (VIP), a web application (app) that delivered HIV-related symptom self-care strategies for PLWH (P30NR010677–03S1). Results from our 3-month pilot study (N=42) overwhelmingly demonstrated the feasibility of the system. Participants reported a decrease in HIV-related symptom frequency and intensity after using the VIP system for 12 weeks [10]. However, the UCSF symptom management manual and VIP were not developed for managing symptoms related to HANA conditions. Little is known about the symptom experience or self-care strategies used by PLWH with HANA conditions. Based on the existing evidence and our previous work, we sought to adapt the VIP system to include tailored self-care strategies to ameliorate HANA condition- related symptoms. Strategies are tailored based on the following characteristics: symptom, sex, race/ethnicity and HANA condition. Following our identification of the most useful self-care strategies for PLWH with HANA conditions, we sought to incorporate these strategies into a user-centered consumer health informatics app (VIP-HANA) to improve health outcomes.
Anonymous Online Survey
Methods
To assess the frequency and severity of HANA symptoms, we distributed an anonymous online survey. Details on the methods and findings for the online survey have been published elsewhere [11]. In short, we posted banner advertisements on Craigslist, POZ.com, BGCLive.com, and Facebook.com to recruit 769 PLWH living in the US to participate. Those who clicked on the banner ad were directed to a study landing page hosted by Qualtrics software that allowed them to complete a screener to determine if they qualified for study participation. Inclusion criteria included: a) 18 years or older, b) having a HIV diagnosis, c) current US residence, d) a diagnosis of one of the following HANA conditions: arthritis, asthma, cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, liver disease, osteoporosis and renal failure, e) not being pregnant or breastfeeding, f) able to read and understand Spanish or English, and g) having at least one of 28 HANA symptoms. Those who qualified completed the consent form through a clickable link preceding the Qualtrics survey.
The survey assessed the frequency and bothersomeness of 28 symptoms: 1) anxiety, 2) change in appetite, 3) clumsiness, difficulty with balance, 4) difficulty concentrating, 5) constipation, gas, bloating, 6) cough, 7) depression, 8) decreased sex drive, 9) diarrhea, 10) difficulty remembering, 11) lightheadedness/ dizziness, 12) dry eyes, 13) thirst/ dry mouth, 14) difficulty falling asleep, 15) low energy/ fatigue, 16) fever, night sweats or chills, 17) heartburn, 18) problems achieving or maintaining an erection (males only), 19) muscle aches or pain, 20) neuropathy, 21) pain or discomfort during sex, 22) ringing in ears/ noise intolerance, 23) shortness of breath, 24) speech difficulties, 25) difficulty staying asleep, 26) difficulty with urination, 27) nausea/ vomiting, and 28) unplanned weight change. We included open-ended questions for participants to report self-care strategies used to ameliorate each symptom experienced, rate its degree of helpfulness and identify the information source for the strategy.
Results
Survey results yielded a total of 4,036 self-care strategies across the 28 symptoms. These survey findings provided additional information on the usefulness of each strategy as well as the information source for the strategy, which are reported elsewhere [11].
Coding and Analysis of the Self-Care Strategies
Methods
We used multiple steps to rank self-care strategies (very helpful, only a little helpful, etc.) that could then be used to tailor recommendations based on individual characteristics (using branching logic) to be integrated into the app. A qualitative data analytic approach was used to code and organize the 4,036 self-care strategies obtained in the anonymous online surveys. Open-ended responses were categorized into an overall heading. For example, open-ended survey responses included “take a nap,” “rest,” “rest in the afternoon,” and these were all categorized as “take a nap.” We then removed the self-care strategies that were rated as only a little helpful or not helpful at all. We also had a group of expert clinicians, HIV researchers, and nurses review each of the strategies to ensure their safety and legality. The purpose of this work was to identify helpful self-care strategies for future use by PLWH with HANA conditions and therefore we did not include strategies which were not helpful, not clinically advised (e.g., do nothing for a depressed patient), or potentially harmful (e.g., using illegal substances or gambling).
After consolidating initial codes of strategies on the basis of conceptual similarities and clinical significance, and after removing unhelpful, illegal and unsafe strategies, we had a final dataset of 728 self-care strategies. We then ranked the self-care strategies based on how frequently study participants rated the self-care strategy as being helpful and completing the review of all of the self-care strategies. Chi-square analysis was performed to test the association between the self-care strategies and each of the following dichotomized variables, which include race/ethnicity (white versus non-white), sex (male versus female), and status (Yes versus No) of each of the nine HANA conditions (Asthma, bronchitis, cardiovascular disease, COPD, diabetes, liver disease, osteoporosis, renal failure, and arthritis). Variables with p-value less than 0.05 were considered to be significantly associated with the frequencies of self-care strategies. If there were more than one single significant variables, then a second-step Chi-square analysis ensued: we first split the data into each category of variable with the lowest p-value from the firsts-step Chi-square, and then further Chi-square analysis was performed between the remaining significant variables and self-care strategies. We then ranked the strategies from the highest to lowest frequency stratified by significant variables identified from each step of Chi-square analysis. We repeated the procedures for each symptom. For example, for the self-care strategies of decreased sex drive, we first identified sex and race as variables significantly associated with this strategy and sex had the lowest p-value. We then split the data into male and female and performed a second-step Chi square analysis between race and self-care strategies of this symptom by male and female separately. Race was still significant for female participants, but not significant for male participants. Thus, we ranked the self- care strategies of this symptom from the highest to lowest frequency by three separate groups: male, female white, and female non-white. Strategies were further categorized when relevant by sex, race and HANA condition.
Results
Branching logic was developed based on this analysis and provided the knowledge base for the delivery of the self-care strategies to users. Most symptoms had branching logic associated with sex, race and HANA condition. Speech difficulties and pain/ discomfort during sex were the only symptoms with no branching logic. All participants would receive the same ranking and listing of self-care strategies. All other symptoms were tailored by at least one of the three characteristics (sex, race, or HANA condition). Examples of the branching logic are illustrated in Table 1.
Table 1.
Sample Self-Care Strategies for Anxiety, Sleep and Sex Drive Symptoms Tailored by HANA Condition, Sex, and Race
| Top 3 Ranked Self-Care Strategies for Symptoms of Anxiety tailored by HANA conditions | ||
|---|---|---|
| HANA Condition | Ranking | Self-Care strategy |
| Arthritis | 1 | Try breathing exercises to help with anxiety. An example would be taking a deep inhaled breath into your belly. |
| 2 | Try relaxation or stress-reducing activities, such as meditation, personal “quiet time,” or prayer. | |
| 3 | Try spending some time alone in a relaxed and calm environment. | |
| No Arthritis | 1 | Try relaxation or stress-reducing activities, such as meditation, personal “quiet time,” or prayer. |
| 2 | Try to prioritize more sleep if possible. A good night’s sleep is important. | |
| 3 | Try to live an active lifestyle and stay busy. Physical activity has been shown to reduce anxiety. | |
| Top 3 Ranked Self-Care Strategies for Symptoms of Difficulty Staying Asleep tailored by HANA conditions | ||
| HANA Condition | Ranking | Self-Care strategy |
| Renal Failure | 1 | Try making time for activities that you personally enjoy. |
| 2 | Don’t give up and keep trying different strategies to help you stay asleep. | |
| 3 | Some people who have dealt with this have found that taking time to wait while staying calm. | |
| No Renal Failure | 1 | Try a sleeping aid if you are having trouble falling or staying asleep. |
| 2 | Try to practice good sleep hygiene and relaxation techniques to improve your quality of sleep. | |
| 3 | Try making time for activities that you personally enjoy. | |
| Top 3 Ranked Self- Care Strategies for Decreased Sex Drive Tailored by Sex and Race | ||
| Sex/ Race | Ranking | Self-Care strategy |
| Female/ White | 1 | Try adding more physical activity to your life. Physical activity can increase blood flow and can help increase your sex drive. |
| 2 | Have an open and honest conversation with your partner about your symptoms and talk about strategies you can use together. | |
| 3 | Don’t give up and keep trying different strategies that may help you increase your sex drive. | |
| Female/ non- white | 1 | Some people who have dealt with this have found that taking time to wait or sleeping can help. |
| 2 | Try having sex when you are in different moods. Some people find sex more enjoyable after they’ve argued, while others find this more distracting. | |
| 3 | Try adding more physical activity to your life. Physical activity can increase blood flow. | |
| Male | 1 | Try using porn to increase your sex drive and increase your sexual desire. |
| 2 | Some people who have dealt with this have found that taking time to wait or sleeping can help. | |
| 3 | Try masturbating more often, which can boost your sex drive. | |
Development of the VIP-HANA system
Methods
Once the self-care strategies were finalized, we used Powtoons software to create animated videos (see sample screenshot of video in Figure 1) to illustrate each strategy which would later be integrated into the self-care strategy database. Ruby on Rails, an open source software framework that provides standardized structures for building was used to develop the web-app.
Figure 1.
Self-Care Strategy Animated Video
Results
The final VIP-HANA app included the following components: (1) a user profile which collects information at baseline on sex, race, and HANA condition of the user (Figure 2a), (2) reminder system to use the app weekly, (3) weekly symptom assessment (Figure 2c), (4) avatar selection (Figure 2d), (5) an overview report of the recommended strategies (Figure 2e), (6) symptom reports (figure 2f) and (7) a back-end database that provides tailored strategies based on the user profile and their symptom assessment. Videos were hosted on Vimeo software and participants received a video illustrating the self-care strategy every time they used the app and reported a symptom.
Figure 2.
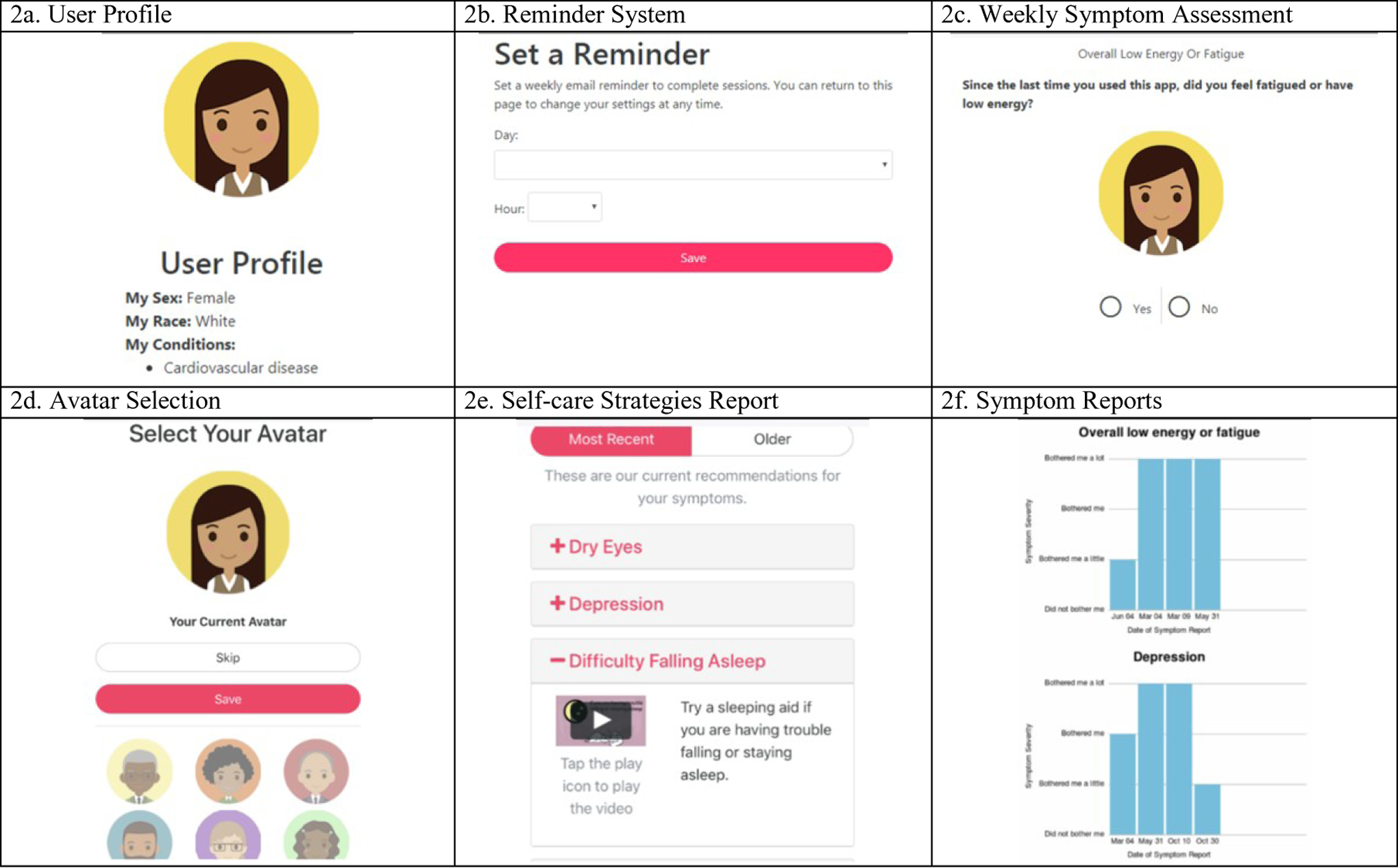
Screenshots of App Component
Usability Evaluation of the VIP-HANA system
Methods
The final component of our development process was a laboratory usability evaluation with experts in human computer interaction and PLWH with at least 1 HANA condition. Full details of the usability evaluation are published elsewhere [12]. In brief, participants were provided with a Beta version of the app and asked to use the app to complete a use-case scenario created by the research team. Participants were asked to think aloud as they used the app and Morae screen capture software was used to record the session.
Results
Informatics experts (N=5) and end-users (N=20) rated the VIP- HANA app as a highly usable system. Yet they did make useful recommendations which we incorporated into the system as part of the app development and prior to our trial. End-users had difficulty completing advanced app functions, such as changing their avatar, emailing symptom reports, setting weekly reminders and enlarging videos. Experts and end-users agreed that the app needed to provide more instructions. Experts suggested that this be accomplished through a help button and end-users recommended including in-app instructions with straightforward and simple language. End-users also wanted to see features in big, bright, and bold text with a clear font.
VIP-HANA Trial
Following the implementation of the recommended changes from the usability testing, the software development company updated the app in preparation for a systematic evaluation. Currently, we are conducting a randomized trial with 100 PLWH with HANA conditions living in New York City. The goal of the trial will be to examine the effect of the VIP-HANA app on symptom burden, quality of life and frailty over a 6- month period (NCT03182738).
Discussion
This study demonstrated the ability to successfully translate our extant eHealth intervention for a growing clinical problem, HANA conditions. We incorporated quantitative and qualitative methods to better understand the needs of our target population and then successfully integrated these findings into our VIP eHealth platform, conducted usability testing and then conducted an RCT. Notably, our study population of PLWH with HANA conditions have unmet needs and we had the opportunity to advance our VIP intervention for a new set of users. With the proliferation of eHealth interventions, the aging of the US population and the reduction of healthcare services, there will likely be an increasing need for this translating and adapting eHealth interventions. Our study population is unique in that they are comprised of PLWH who are predominately low-income racial ethnic minorities, suffer from a chronic illness and also an infectious disease. Given the high needs of our study population in terms of social, physical and psychological support and their low socioeconomic status, development of informatics tools that can be used in these persons’ everyday settings have the potential to dramatically improve clinical outcomes and quality of life, while also providing savings to our over-burdened healthcare system.
Building on our past approaches to developing mobile technology using end-user feedback and an iterative approach [13–16], this paper presents the integration of innovative methods for the creation of consumer health informatics tools. Notably, our approach included a large national US survey, clinician and expert review of the content, translation of survey data into a database which is the knowledge system of a patient- facing tool and a rigorous usability evaluation. Moreover, our study methods paid close attention to the needs of our study population by developing videos to maintain consumer engagement in the app.
Further, development of consumer health informatics tools can be complicated because of the need to integrate patient preferences, user-centered design principles, the limitations of software tools and the safety and potential efficacy from clinician experts. Given the complex integration of sources, there is a strong need for the development and dissemination of iterative development processes which integrate multiple stakeholders and result in usable and useful health information technology [17]. Finally, this paper illustrates the development of a practical and useful tool with immediate application that enables improvement in population-level quality of life. There is promising potential for integration of these tools to wider popular platforms.
Conclusions
This paper illustrates the development of a consumer health informatics app for ameliorating symptoms in PLWH with HANA conditions. We successfully completed a multi-modal development process incorporating the critical elements of user-centered design to build our app. Findings from the usability evaluation demonstrate a potentially useful and easy to use app. Integration of different quantitative and qualitative methods from different disciplines to accomplish the task of adaptation and evaluation of a mobile app is an appealing, rigorous and useful approach.
Acknowledgements
Research reported in this publication was supported by National Institute of Nursing Research of the National Institutes of Health under award number R01NR015737. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors had full access to all the data and had final responsibility for the decision to submit for publication.
References
- [1].Deeks SG, Lewin SR, and Havlir DV, The end of AIDS: HIV infection as a chronic disease, Lancet 382 (2013), 1525–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Centers for Disease Control and Prevention, HIV Among People Aged 50 and Older 2018, available from: https://www.cdc.gov/hiv/group/age/olderamericans/index.html
- [3].Justice AC and Braithwaite RS, Lessons learned from the first wave of aging with HIV, AIDS (London, England) 26 Suppl 1 (2012), S11–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Neuhaus J, Angus B, Kowalska JD, La Rosa A, Sampson J, Wentworth D, et al. , Risk of all-cause mortality associated with nonfatal AIDS and serious non- AIDS events among adults infected with HIV, AIDS (London, England) 24 (2010), 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].High KP, Brennan-Ing M, Clifford DB, Cohen MH, Currier J, Deeks SG, et al. , HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and Aging Working Group, J Acquir Immune Defic Syndr (1999) 60 Suppl 1 (2012), S1–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Nicholas PK, Kirksey KM, Corless IB, and Kemppainen J, Lipodystrophy and quality of life in HIV: symptom management issues, Appl NursRes 18 (2005), 55–58. [DOI] [PubMed] [Google Scholar]
- [7].Dodd MJ, Miaskowski C, and Paul SM, Symptom clusters and their effect on the functional status of patients with cancer, Oncol Nurs Forum 28 (2001), 465–470. [PubMed] [Google Scholar]
- [8].Schnall R, Cho H, Mangone A, Pichon A, and Jia H, Mobile health technology for improving symptom management in low income persons living with HIV, AIDS Behav 22 (2018), 3373–3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wantland DJ, Holzemer WL, Moezzi S, Willard SS, Arudo J, Kirksey KM, et al. , A randomized controlled trial testing the efficacy of an HIV/AIDS symptom management manual. J Pain Symptom Manage 36 (2008), 235–246. [DOI] [PubMed] [Google Scholar]
- [10].Schnall R, Wantland D, Velez O, Cato K, and Jia H, Feasibility testing of a web-based symptom self- management system for persons living with HIV, J Assoc Nurses AIDS Care 25 (2014, 364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Iribarren S, Siegel K, Hirshfield S, Olender S, Voss J, Krongold J, et al. , Self-management strategies for coping with adverse symptoms in persons living with HIV with HIV associated non-AIDS conditions. AIDS Behav 22 (2018), 297–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Stonbraker S, Cho H, Hermosi G, Pichon A, and Schnall R, Usability testing of a mHealth app to support self- management of HIV-associated non-AIDS related symptoms, Stud Health Technol Inform 250 (2018), 106–110. [PMC free article] [PubMed] [Google Scholar]
- [13].Schnall R, Rojas M, Bakken S, Brown III W, Carballo-Dieguez A, Carry M, et al. , A user-centered model for designing consumer mobile health (mHealth) applications (apps), J Biomed Inform 60 (2016), 243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Schnall R, Rojas M, Travers J, Brown III W, and Bakken S, Use of design science for informing the development of a mobile app for persons living with HIV, AMIA Annu Symp Proc 2014 (2014), 1037–1045. [PMC free article] [PubMed] [Google Scholar]
- [15].Schnall R, Bakken S, Rojas M, Travers J, and Carballo-Dieguez A, mHealth technology as a persuasive tool for treatment, care and management of persons living with HIV, AIDS Behav, 19 (2015), 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cho H, Yen P-Y, Dowding D, Merrill JA, and Schnall R, A multi-level usability evaluation of mobile health applications: a case study. J Biomed Inform, 86 (2018), 79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yen P-Y and Bakken S, Review of health information technology usability study methodologies, J Am Med Inform Assoc, 19 (2012), 413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]


