Abstract
Epithelioid hemangioendothelioma (EHE) is a rare vascular tumor composed of dendritic and endothelial cells, and accounts for less than 1% of all vascular tumors. The tumor may arise from any location in the body, but it has a predilection for veins of the extremities, the liver, bone, and skin. Herein, we report a case of a 43‐year‐old man who presented with a chest mass accompanied by chest pain. Computed tomography (CT) scan of the chest showed a 3 cm × 2 cm sternal mass in the chest wall. We performed tumor resection and reconstruction of the chest wall. EHE was confirmed via postoperative pathology. The patient underwent postoperative adjuvant radiotherapy, and no evidence of tumor recurrence was discovered during the one‐year follow up.
Keywords: Epithelioid hemangioendothelioma, follow‐up, sternum, surgical resection
Introduction
Epithelioid hemangioendothelioma (EHE) is a rare sarcoma composed of dendritic and endothelial cells. The tumor is clinically and histologically intermediate between benign hemangioma and angiosarcoma and accounts for less than 1% of all vascular tumors. It is most commonly found in the liver, bone, and skin. EHE in the chest is extremely rare. This condition occurring in the sternum has not been reported until now. Given that EHE is aggressive, surgical resection with adjuvant chemotherapy and radiotherapy is recommended to prevent recurrence or metastasis.
Case report
A 43‐year‐old man presented to our hospital with a chest mass accompanied by chest pain for over five months. The patient complained of slight haphalgesia and apparent tenderness radiating into the neck and shoulders, which was relieved by administering fenbid. The patient denied any history of trauma, and had no relevant medical history. On physical examination, a tumor 3 cm in diameter was found in the anterior chest wall. The preoperative thoracic computed tomography (CT) scan revealed a 3 cm × 2 cm mass in the sternum manubrium (Fig 1a). In addition, three‐dimensional (3D) reconstruction of the chest CT confirmed the presence of a sternal tumor (Fig 1b). A percutaneous thin‐needle aspiration biopsy was performed before the operation, and the primary diagnosis was mesenchymal tumor. Considering the particularity of sternal site and function, resection of the sternal tumor and a 3D‐printed titanium alloy graft implantation was planned which was approved by the Institutional Review Board of West China Hospital (No. 2018–45). Informed consent of the patient was obtained before surgery and the design of the 3D‐printed graft was performed using 3D reconstruction of the preoperative chest CT (Fig 2a). Consequently, the patient underwent an enlarged excision of the manubrium sternum with the surrounding muscle tissues and reconstruction of the chest wall with 3D‐printed titanium alloy sternal prosthesis under general anesthesia. The 3D‐printed sternal prosthesis consisted of two pairs of transverse limbs and a body. The limbs were fixed in the clavicle and the second rib, respectively, and the body in the sternum with screws (Fig 2b). Postoperative pathological examination confirmed the diagnosis of EHE. Hematoxylin and eosin staining showed some dendritic and endothelial cells formed various size vessels with red blood cells contained (arrows). There was also a dense inflammatory infiltration in some areas. (Fig 3a). Immunohistochemical staining was positive for CAMTA1, CD31, and CD34 (Fig 3b–d). Postoperative chest radiographs showed that the metal graft was in a normal position (Fig 4). After a successful postoperative recovery, he underwent radiotherapy, and no evidence of tumor recurrence was discovered during the one‐year follow up.
Figure 1.
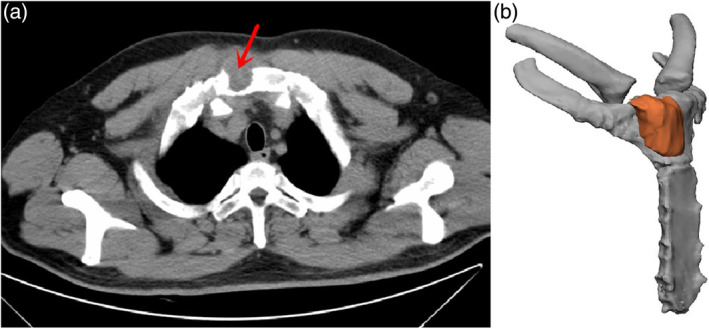
(a) The preoperative thoracic computed tomography (CT) scan revealed a 3 cm × 2 cm mass in the sternum manubrium (red arrow). (b) The 3D reconstruction of the tumor (orange) of the sternum.
Figure 2.
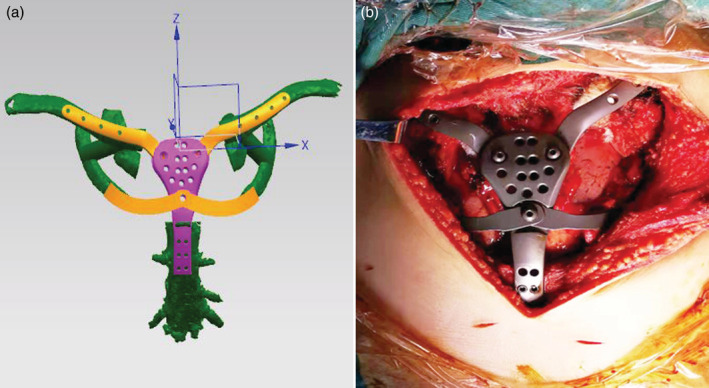
(a) The 3D printed design drawing before operation. (b) The 3D‐printed titanium alloy sternal prosthesis was implanted during the operation.
Figure 3.
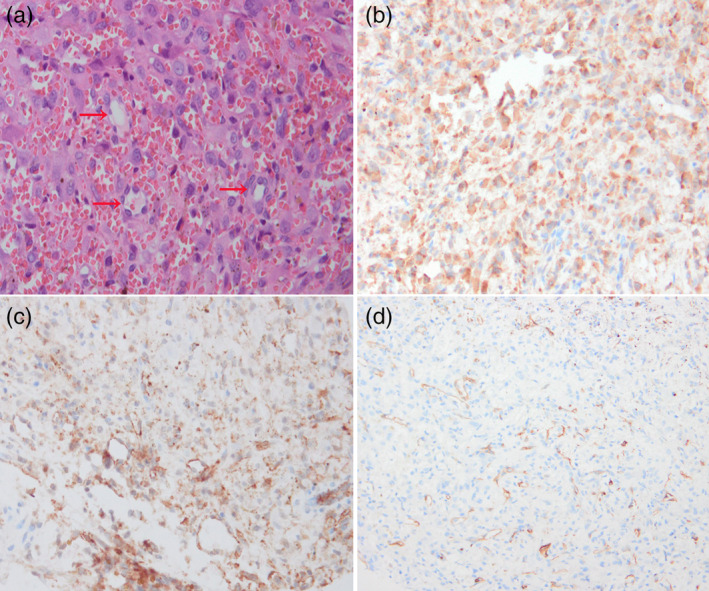
(a) Hematoxylin and eosin staining showed some dendritic and endothelial cells formed various size of vessels with red blood cells contained (arrows). There was also a dense inflammatory infiltration in some areas. (b–d) Immunohistochemical staining was positive for CAMTA, CD31 and CD34 proteins.
Figure 4.
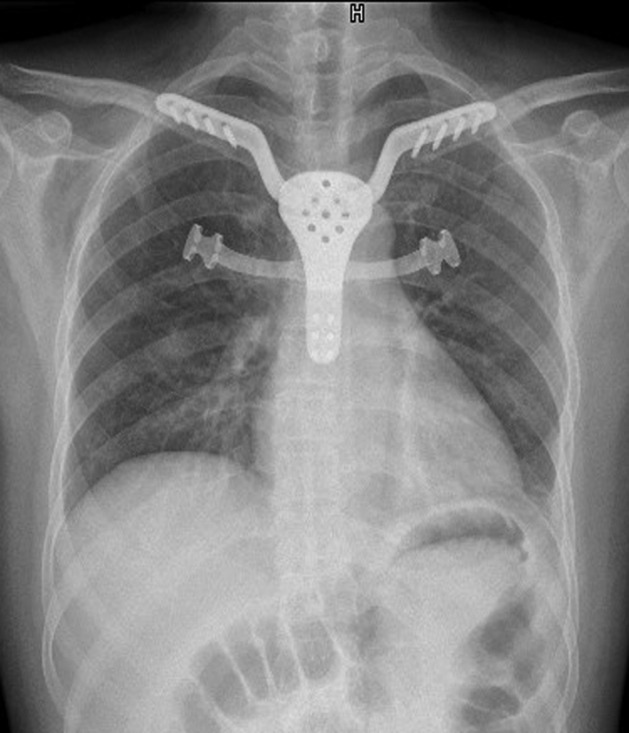
Postoperative chest radiographs showed that the metal graft was in a normal position.
Discussion
EHE, a rare low‐moderate malignant hemangioma, was first described by Weiss in 1982.1 Clinically and histologically, EHE is considered an intermediate malignancy between angiosarcoma and hemangioma. According to reports in the literature, the incidence is less than one in a million, 2 and it can occur at any age, especially in the 20s. Clinically, EHE mostly occurs in soft tissues, the liver, bone, and other organs.3 Review of the literature revealed rare involvement of the chest wall. To the best of our knowledge, our case is the first report of sternal EHE. The symptoms of EHE usually depend on the site of the disease, such as abdominal pain (liver) and dry cough (lung). The clinical presentation of sternal EHE is nonspecific and varies depending on the size of the tumor, which is similar to other common chest wall tumors. Patients may present with swelling and pain in the chest wall.
Radiological examination has great clinical value for the early discovery of ETE. The CT image of osseous EHE presents a multifocal lytic abnormality with osseous expansion, sclerotic margins, and a lack of periostitis. However, the diagnosis of EHE needs to be confirmed by pathology and immunohistochemistry. Pathologically, the tumor is composed of dendritic and endothelial cells with positive nuclear staining, and positive immunohistochemistry for vascular markers (CD31, CD34, and vimentin) can show better specificity. In addition, the WWTR1‐CAMTA1 characteristic fusion gene is regarded as an auxiliary diagnosis. The main differential diagnosis of EHE includes metastatic signet‐ring cell adenocarcinoma and epithelioid angiosarcoma.4
EHE in the chest is extremely rare. The literature review (Table 1) reveals that the most common sites in the chest are lungs, mediastinum, and pleura.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Rare cases occurring in the http://xueshu.baidu.com/usercenter/paper/show?paperid=7bd80dbe6b85c1871c62432d37adfb65&site=xueshu_se and the superior vena cava have also been reported.19, 20 To date, this condition occurring in the sternum has not been reported. Surgical resection is generally accepted as the definitive treatment of choice for tumor of the chest wall. After resection of the sternal tumor, sternal reconstruction is necessary to protect the exposed thoracic viscera, repair the appearance of the chest wall, and maintain arm function. Available materials include titanium mesh or plate, autogenous bone graft, cryopreserved sternal allograft, or homograft flap.21, 22 However, 3D‐printed titanium alloy grafts have the advantages of individualization, easy fixation, and light tissue rejection. The clinical course of EHE is usually somewhat indolent compared with other sarcomas, and the five‐year survival is about 73%. Postoperative adjuvant radiotherapy is usually required to prevent recurrence and metastasis.3, 23
Table 1.
Reported cases of epithelioid hemangioendothelioma (EHE) in the chest
| N | Author | Age | Sex | Location | Size (cm) | Symptoms | Treatment | Follow‐up |
|---|---|---|---|---|---|---|---|---|
| 1 | Kumar et al. 5 | 63 | M | Lung | 15 × 15 × 4 | Chest pain, cough | Surgical resection | No recurrence |
| 2 | Agaimy et al.6 | 62 | M | Mediastinum | 10 × 9 × 7 | Dyspnea, cough | Surgical resection | No recurrence |
| 3 | Isowa et al.7 | 41 | M | Mediastinum | 3.4 × 2.7 | No | Surgical resection | No recurrence |
| 4 | Val‐Bernal et al.8 | 69 | F | Heart | 4 × 3 × 2 | Dyspnea, orthopnea | Surgical resection | No recurrence |
| 5 | Lisy et al.9 | 61 | M | Heart | 3 × 3 | Abdominal pain | Surgical resection | No recurrence |
| 6 | Safirstein et al.10 | 51 | F | Heart | 5 × 4 × 4 | None | Surgical resection | No recurrence |
| 7 | Márquez‐Medina et al.11 | 85 | M | Pleura | 15 × 15 × 4 | Chest pain, cough | Surgical resection | No recurrence |
| 8 | Lee et al.12 | 31 | F | Lung, bone | 5 × 3 × 2.5 | Dull pain | Chemotherapy | No recurrence |
| 9 | Kim et al.13 | 46 | F | Pleura | No stated | chest discomfort, cough | Pleurectomy; Chemotherapy | Died after 23 months |
| 10 | Mizota et al.14 | 59 | F | Lung | 2.5 × 3.5 | Cough, dyspnea | Surgical resection; chemotherapy | Recurrence |
| 11 | Bansal et al.15 | 51 | F | Pleura | No stated | Chest pain, weight loss | Surgical resection; chemotherapy | Died after l4 months |
| 12 | Campos et al.16 | 36 | F | Mediastinum | 5.4 | Dyspnea, dry cough | Surgical resection | No recurrence |
| 13 | Kumar et al.17 | 33 | M | Mediastinum | 3.9 × 7.3 × 5.8 | Chest and back pain | No | Died |
| 14 | Wethasinghe et al.18 | 41 | M | Mediastinum | 1.2 × 2.5 | Chest pain, weight loss | radiotherapy | No recurrence |
In conclusion, EHE in the chest are extremely rare, and there are no cases in the sternum having been described in the literature to date. Preoperative diagnosis of sternal EHE is difficult, since clinical symptoms and radiology features overlap with other tumors arising from the chest wall. Here, we report a very rare case of EHE occurring in the sternum. Due to the lack of the evidence in the current literature, the therapeutic effect cannot be exactly assessed and close follow‐up is necessary.
Disclosure
The authors report that there are no conflicts of interest.
References
- 1. Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer 1982; 50: 970–81. [DOI] [PubMed] [Google Scholar]
- 2. Lau K, Massad M, Pollak C et al Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: Insights from an internet registry in the study of a rare cancer. Chest 2011; 140: 1312–8. [DOI] [PubMed] [Google Scholar]
- 3. Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M. Epithelioid hemangioendothelioma: An overview and update on a rare vascular tumor. Oncol Rev 2014; 8: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu X, Li B, Zheng C, Hong T, He X. Clinical characteristics of epithelioid hemangioendothelioma: A single‐center retrospective study. Eur J Med Res 2019; 24: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kumar RP, Smith DA, Hilton CJ, Parums DV. A case of epithelioid hemangioendothelioma (EHE) of the lung with bronchial brushing cytology. Cytopathology 1999; 10: 132–6. [DOI] [PubMed] [Google Scholar]
- 6. Agaimy A, Kaiser A, Wünsch PH. Epithelioid hemangioendothelioma of the heart in association with myelodysplastic syndrome. Z Kardiol 2002; 91: 352–6. [DOI] [PubMed] [Google Scholar]
- 7. Isowa N, Hasegawa S, Mino M, Morimoto K, Wada H. Mediastinal epithelioid hemangioendothelioma resected by hemi‐plastron window technique. Ann Thorac Surg 2002; 74: 567–9. [DOI] [PubMed] [Google Scholar]
- 8. Val Bernal JF, Garcia Alberdi E, Gutierrez JA, Garijo MF. Incidental in vivo detection of an epithelioid hemangioendothelioma of the mitral valve. Pathol Int 2005; 55: 644–8. [DOI] [PubMed] [Google Scholar]
- 9. Lisy M, Beierlein W, Müller H, Bültmann B, Ziemer G. Left atrial epithelioid hemangioendothelioma. J Thorac Cardiovasc Surg 2007; 133: 803–4. [DOI] [PubMed] [Google Scholar]
- 10. Safirstein J, Aksenov S, Smith F. Cardiac epithelioid hemangioendothelioma with 8‐year follow‐up. Cardiovas Pathol 2007; 16: 183–6. [DOI] [PubMed] [Google Scholar]
- 11. Márquez‐Medina D, Samamé‐Pérez‐Vargas JC, Tuset‐Derabrain N, Montero‐Fernández A, Taberner‐Bonastre T, Porcel JM. Pleural epithelioid hemangioendothelioma in an elderly patient. A case report and review of the literature. Lung Cancer 2011; 73: 116–9. [DOI] [PubMed] [Google Scholar]
- 12. Lee YJ, Chung MJ, Jeong KC et al Pleural epithelioid hemangioendothelioma. Yonsei Med J 2008; 49: 1036–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim EA, Lele SM, Lackner RP. Primary pleural epithelioid hemangioendothelioma. Ann Thorac Surg 2011; 91: 301–2. [DOI] [PubMed] [Google Scholar]
- 14. Mizota A, Shitara K, Fukui T. Bevacizumab chemotherapy for pulmonary epithelioid hemangioendothelioma with severe dyspnea. J Thorac Oncol 2011; 6: 651–2. [DOI] [PubMed] [Google Scholar]
- 15. Bansal A, Chawla M, Cohen PJ, Kwon JS. Pleural epithelioid hemangioendothelioma. Lung 2012; 190: 469–70. [DOI] [PubMed] [Google Scholar]
- 16. Campos J, Otero E, Dominguez MJ, Gonzalez‐Quintela A. Epithelioid hemangioendothelioma in the posterior mediastinum. Eur J Intern Med 2007; 18: 331–2. [DOI] [PubMed] [Google Scholar]
- 17. Kumar A, Lopez YK, Arrossi AV, Rubin B, Ashton R. Mediastinal epithelioid hemangioendothelioma. Am J Respir Crit Care Med 2016; 193: e7–8. [DOI] [PubMed] [Google Scholar]
- 18. Wethasinghe J, Sood J, Walmsley R, Milne D, Jafer A, Gordon‐Glassford N. Primary pleural epithelioid hemangioendothelioma mimicking as a posterior mediastinal tumor. Respirol Case Rep 2015; 3: 75–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Long K, Skinner S, Martin J. Epithelioid hemangioendothelioma encasing the left brachiocephalic vein. J Surg Case Rep 2014; 2014: rju057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ferretti G, Chiles C, Woodruff R, Choplin RH. Epithelioid hemangioendothelioma of the superior vena cava: Computed tomography demonstration and review of the literature. J Thorac Imaging 1998; 13: 45–8. [DOI] [PubMed] [Google Scholar]
- 21. Nosotti M, Rosso L, Mendogni P et al Sternal reconstruction for unusual chondrosarcoma: Innovative technique. J Cardiothorac Surg 2012; 7: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Seder CW, Rocco G. Chest wall reconstruction after extended resection. J Thorac Dis 2016; 8: S863–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kulkarni KR, Jambhekar NA. Epithelioid hemangioendothelioma of bone‐a clinicopathologic and immunohistochemical study of 7 cases. Indian J Pathol Microbiol 2003; 46: 600–4. [PubMed] [Google Scholar]


