By using the 2009–2016 NHANES, trends and subgroups with lower rates of meeting AAP vitamin D intake guidelines were examined.
Abstract
Video Abstract
BACKGROUND:
The American Academy of Pediatrics (AAP) revised its infant vitamin D intake guidelines in 2008. We aimed to examine previously unexplored trends in meeting vitamin D intake guidelines among US infants since 2009 and whether there were differences across demographic subgroups.
METHODS:
We analyzed dietary recall data for infants 0 to 11 months in the 2009–2016 NHANES. We estimated the percentage meeting 2008 AAP vitamin D guidelines, defined as consuming ≥1 L of infant formula and/or receiving a vitamin D supplement of ≥400 IU. We used Poisson regressions to assess trends over time and differences across demographic subgroups.
RESULTS:
Overall, 27.1% (95% confidence interval [CI]: 24.3%–29.8%) of US infants in 2009–2016 met vitamin D intake guidelines, with nonbreastfeeding infants (31.1% [95% CI: 27.6%–34.5%]) more likely to meet guidelines than breastfeeding infants (20.5% [95% CI: 15.4%–25.5%]; P < .01). From 2009–2010 to 2015–2016, overall and for both breastfeeding and nonbreastfeeding infants, there were no significant changes over time in the percentage of infants who met the guidelines (P > .05). Among breastfeeding infants, those with a family income ≥400% of the federal poverty level, with a college graduate head of household, and with private insurance were more likely to meet guidelines.
CONCLUSIONS:
Among US infants, we observed no increase in meeting AAP vitamin D intake guidelines since 2009. Less than 40% of infants met guidelines in nearly all demographic subgroups. These findings suggest renewed consideration of how to best meet vitamin D intake guidelines.
What’s Known on This Subject:
In 2008, the American Academy of Pediatrics revised its vitamin D intake guidelines. Studies from or before 2012 revealed that the rates of infants meeting the guidelines were low. Recent trends and subgroups at risk have not yet been examined.
What This Study Adds:
Since 2009, the percentage of infants meeting American Academy of Pediatrics vitamin D intake guidelines has not increased. Less than 40% of nearly all demographic subgroups met the guidelines. Among breastfeeding infants, lower socioeconomic status was associated with failing to meet the guidelines.
In 2008, the American Academy of Pediatrics (AAP), with the primary intention of preventing rickets, increased their recommended intake of vitamin D for infants <1 year of age from 200 to 400 IU daily.1 Specifically, the recommendations stated that exclusively or partially breastfeeding infants should be supplemented with 400 IU daily and that nonbreastfeeding infants should consume at least 1 L of formula daily. Federal regulations have long required that 1 L of infant formula contain at least 400 IU of vitamin D.1,2 For nonbreastfeeding infants consuming <1 L a day of formula, the AAP recommended supplementation as well.1 In 2011, the Institute of Medicine (now known as the National Academy of Medicine) concurred with this recommendation,3 and the AAP, through an endorsement of the Institute of Medicine report in 20124,5 and through a clinical report in 2014,6 reaffirmed its original 2008 recommendation.
However, vitamin D intake by US infants has fallen far short of these goals. Using data from the Infant Feeding Practices Study II, conducted in 2005–2007, Perrine et al7 showed that, among formula-fed infants, most infants (81%–98.2%, varying by month of age) met the lower intake recommended in the 2003 AAP guidelines (200 IU), but only 19% to 37% (varying by month of age) would have met the higher intake recommended in the 2008 AAP guidelines (400 IU). Among breastfeeding infants, only ∼10% to 12% of infants would have met the 2008 guidelines.7
We previously examined the rate of adherence with the 2008 AAP guidelines and found that from 2009 to 2012, only 27.4% of infants in the United States were meeting the new vitamin D intake recommendations, with 19.3% of breastfeeding infants and 31.4% of nonbreastfeeding infants meeting recommendations.8 Regional studies from the same time period published similar findings.9
Since 2012, trends in vitamin D intake among infants at a national level have not been well described. Because research suggests that there might be a substantial delay between guideline publication and clinical practice changes,10 continued examination of guideline adherence is warranted. In addition, since 2012, authors of several studies have reported on quality improvement initiatives to increase vitamin D intake for infants.11–16 Whether time and increased focus on quality improvement have increased the percentage of infants who meet the guidelines for vitamin D intake is unknown.
In addition, whether specific demographic subgroups are more likely to meet vitamin D intake guidelines has not been described. In our previous study, the statistical reliability of estimates for subgroups of the US population was limited, which prevented us from reporting these results. If certain demographic groups are less likely to meet vitamin D intake guidelines, public health programs and researchers could design interventions specifically targeting these subgroups.
In this study, we aimed to build on our previous work8 and examined trends in meeting vitamin D intake guidelines among infants in the United States since 2009, one year after the new guidelines were first published. In addition, we aimed to examine whether there were differences in meeting the guidelines across demographic subgroups.
Methods
We analyzed data from the 2009–2016 NHANES, a cross-sectional, continuous survey of noninstitutionalized persons in the United States. The sample of each 2-year cycle of the NHANES is nationally representative. In the NHANES, a complex, multistage, probability sampling design is used to select a sample representative of the civilian noninstitutionalized household population of the United States, and details of the NHANES methodology have been described elsewhere.17–19 The NHANES protocol was approved by the Research Ethics Review Board of the National Center for Health Statistics, and all participants provided informed consent. The Institutional Review Board of the University of Southern Maine determined this research to not be human subjects research.
In the 2009–2016 NHANES, 1483 infants, 0 to 11 months of age, were examined. Of these, dietary recall information, including information on breastfeeding status, was available for the 1435 infants who made up our analytic sample. During an in person interview in the NHANES mobile examination center, an adult proxy (generally a parent) completed the dietary recall for participants, providing information about all food, beverages, and supplements consumed during the 24 hours (midnight to midnight) before the interview. All analyses accounted for the multistage, complex sampling design and used the day 1 dietary recall weights.
We estimated the percentage of infants meeting the 2008 AAP vitamin D guidelines on a given day, defined as either consuming at least 1 L of infant formula or receiving a supplement of at least 400 IU vitamin D or both. Formula intake was identified in the NHANES data by using food codes 11700000 to 11800000, and 1 g of fluid formula was assumed to be equivalent to 1 mL because it is mostly made up of water. Ten micrograms of vitamin D (vitamins D2 and D3) supplement was considered to be equivalent to 400 IU vitamin D.20 Vitamin D obtained from other sources (eg, cow’s milk, dairy food) was not reviewed for vitamin D content for this analysis because the AAP guidelines for infants <1 year of age only recommended formula intake or supplementation to meet guidelines1; in addition, cow’s milk is not recommended as a beverage for children until 1 year of age.21
Analyses were conducted across all infants 0 to 11 months of age as well as stratified by breastfeeding status. Breastfeeding was identified, per the NHANES definition, if an infant consumed any breast milk on either of the 2 possible days of dietary recall.22 Breastfeeding included both exclusive (breast milk only) and partial (breast milk plus formula, other liquid, and/or solid food). Breastfeeding and nonbreastfeeding groups were compared across the following demographic variables: age of infant (0–5, 6–11 months), sex, race and/or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other [ie, Asian, American Indian and Alaskan native, Native Hawaiian or Pacific Islander, and other, including multiracial]), receipt of benefits by the infant from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program during the last 12 months (data available for 2009–2014 only), family income expressed as a percentage of the federal poverty level (FPL) (also known as poverty-to-income ratio and calculated by using US Department of Health and Human Services poverty guidelines on the basis of family income, family size, year, and state23 [<100%, 100%–<200%, 200%–<400%, and ≥400%]), education of head of household (less than or equal to high school diploma, some college, and college graduate), and health insurance status (private insurance, other insurance, and uninsured). Other insurance included any nonprivate sources of insurance such as government programs, including Medicaid, State Children’s Health Insurance Programs, military health care, and the Indian Health Service. Comparisons by breastfeeding status were conducted by using the Rao-Scott χ2 test, a design-adjusted version of Pearson’s χ2 test, which accounts for complex survey design.24
The percentage of infants who met the 2008 AAP vitamin D recommendation was examined over time and by demographic subgroup. All analyses were conducted for the overall group and by breastfeeding status. Time trends were analyzed by using Poisson regression with robust variances, with a 2-year survey cycle as the independent variable (coded as a continuous variable). We then examined trends adjusted for potential changes in demographics over time by adding all the factors listed previously (with the exception of WIC participation; see what follows) to each of the regression models. Poisson regression with robust variances was used rather than logistic regression because logistic regression would have overestimated associations for common events.25,26 In addition, we examined whether the distribution of infants meeting the vitamin D recommendation varied by 2-year cycle using the Rao-Scott χ2 test. To examine differences in meeting the guidelines across demographic subgroups, we used Poisson regression models with robust variances and predictive margins. These models were also adjusted for all covariates with the exception of WIC participation. Because data for WIC participation were only available for 2009–2014, adjusted WIC participation estimates were obtained from separate models that included only data from 2009–2014 (Supplemental Table 4).
All analyses accounted for the population weights and complex design of the survey and were conducted in SAS version 9.4 with SUDAAN (SAS Institute, Inc, Cary, NC) and Stata SE version 16.0 (Stata Corp, College Station, TX). No adjustments were made for multiple comparisons.27 Regarding population estimates, we decided a priori to consider an estimate reliable if the relative SE (RSE) was <30% and unreliable, but presentable, if the RSE was between 30% and 40% (noted in the Results) and to suppress presentation of estimates with an RSE >40%.
Results
Among infants 0 to 11 months of age in the United States during 2009–2016, we found that demographic characteristics differed between breastfeeding and nonbreastfeeding infants (Table 1). As reported by caregivers for the dietary recall period assessed as part of the NHANES, 37.4% of infants were breastfeeding and 62.6% were not breastfeeding. Breastfeeding infants were more likely to be younger (0–5 months as compared with 6–11 months), non-Hispanic white, living in families with higher income, and living in families whose head of household was a college graduate, and they were more likely to have private insurance (P < .01 for all χ2 tests). Breastfeeding infants were also less likely to have received WIC benefits (P<0.01).
TABLE 1.
Demographic Characteristics of US Infants by Breastfeeding Status, 2009–2016
| Total (N = 1435) | Breastfeeding Infants (n = 471) | Nonbreastfeeding Infants (n = 964) | |
|---|---|---|---|
| Age, moa | |||
| 0–5 | 46.1 (672) | 57.3 (282) | 39.4 (390) |
| 6–11 | 53.9 (763) | 42.7 (189) | 60.6 (574) |
| Sex | |||
| Male | 51.1 (699) | 50.2 (229) | 51.7 (470) |
| Female | 48.9 (736) | 49.8 (242) | 48.3 (494) |
| Race and/or ethnicitya | |||
| Non-Hispanic white | 52.1 (477) | 62.1 (186) | 46.1 (291) |
| Non-Hispanic black | 13.6 (266) | 7.4 (54) | 17.2 (212) |
| Hispanic | 25.4 (545) | 22.3 (175) | 27.2 (370) |
| Non-Hispanic other | 9.0 (147) | 8.2 (56) | 9.5 (91) |
| Family income expressed as a percentage of the FPL, %a,b | |||
| ≥400 | 21.9 (194) | 32.3 (107) | 15.7 (90) |
| 200–<400 | 25.6 (270) | 32.3 (116) | 21.5 (154) |
| 100–<200 | 24.0 (354) | 20.1 (99) | 26.4 (255) |
| <100 | 28.5 (503) | 15.4 (109) | 36.3 (394) |
| Education of head of householda,c | |||
| College graduate | 29.9 (306) | 47.6 (169) | 19.2 (137) |
| Some college | 30.2 (396) | 26.6 (128) | 32.4 (268) |
| Less than or equal to high school diploma | 39.9 (688) | 25.8 (162) | 48.5 (526) |
| Health insurancea | |||
| Private | 45.5 (483) | 60.0 (228) | 36.8 (255) |
| Other insurance | 50.5 (894) | 38.9 (217) | 60.5 (677) |
| Uninsured | 4.0 (58) | 6.1 (26) | 2.7 (32) |
| WIC benefit, childa,d | |||
| No | 50.1 (394) | 74.9 (192) | 37.3 (202) |
| Yes | 49.9 (702) | 25.1 (135) | 62.7 (567) |
Data presented as % (n).
Rao-Scott χ2 test P < .0001 for breastfeeding versus nonbreastfeeding infants comparison.
n = 1324 for analysis of poverty level because of missing data.
n = 1390 for analysis of education of head of household because of missing data.
n = 1096 for analysis of WIC benefit in last 12 mo because of missing data and data only available for 2009–2014.
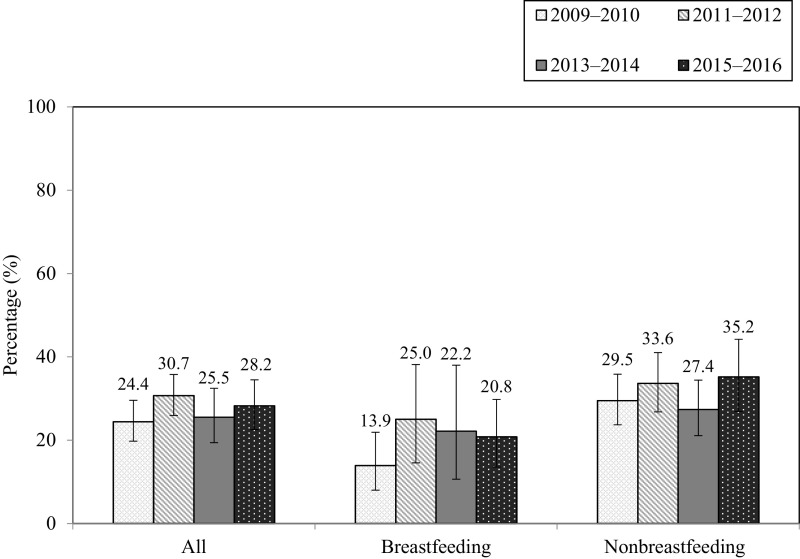
Overall, 27.1% (95% confidence interval [CI]: 24.3%–29.8%) of infants met the 2008 AAP vitamin D intake guidelines. Nonbreastfeeding infants were more likely to meet guidelines than breastfeeding infants (31.1% [95% CI: 27.6%–34.5%] vs 20.5% [95% CI: 15.4%–25.5%], respectively; P < .01). From 2009–2010 to 2015–2016, there was no significant linear trend over time in the percentage of infants who met the guidelines for vitamin D intake (see Fig 1). This was true, overall, among breastfeeding infants and among nonbreastfeeding infants as well as after adjusting for changes over time in demographic characteristics in each of these groups (P > .05 for all linear trend tests). Additionally, there was no significant variation by 2-year cycle in the percentage of infants who met vitamin D intake guidelines, overall, among breastfeeding infants, and among nonbreastfeeding infants (P > .05 for all χ2 tests). In the most recent 2-year cycle for which data were available (2015–2016) 28.2% (95% CI: 22.5%–34.5%) of infants overall met guidelines, 20.8% (95% CI: 13.5%–29.8%) of breastfeeding infants met guidelines, and 35.3% (95% CI: 26.9%–44.2%) of nonbreastfeeding infants met guidelines (P < .05).
FIGURE 1.
Percentage (and 95% CI) of US infants meeting the 2008 AAP recommended vitamin D intake guideline by NHANES cycle and breastfeeding status.
In unadjusted analyses, across all infants 0 to 11 months of age, non-Hispanic white infants were less likely than non-Hispanic black and non-Hispanic other infants to meet vitamin D intake guidelines (23.4% vs 33.1% and 37.7%, respectively; P < .05 and P < .01, respectively; Table 2). No differences were observed in the percentage meeting guidelines by age, sex, family income, education level of the head of household, receipt of WIC benefits, or health insurance status.
TABLE 2.
Unadjusted Percentage of US Infants Meeting the 2008 AAP Recommended Vitamin D Intake Guideline by Breastfeeding Status and Selected Demographic Characteristics, 2009–2016
| Total (N = 1435) | Breastfeeding Infants (n = 471) | Nonbreastfeeding Infants (n = 964) | |
|---|---|---|---|
| Total | 27.1 (24.3–29.8) | 20.5 (15.4–25.5) | 31.1 (27.6–34.5) |
| Age, mo | |||
| 0–5 (ref) | 29.5 (25.5–33.5) | 21.9 (15.9–27.8) | 36.1 (30.4–41.9) |
| 6–11 | 25.0 (21.3–28.7) | 18.6 (10.6–26.7) | 27.7 (23.0–32.4)* |
| Sex | |||
| Male (ref) | 28.7 (25.1–32.4) | 23.1 (16.5–29.7) | 32.0 (26.9–37.1) |
| Female | 25.4 (21.1–29.7) | 17.8 (11.0–24.6) | 30.0 (24.9–35.2) |
| Race and/or ethnicity | |||
| Non-Hispanic white (ref) | 23.4 (19.3–27.6) | 20.1 (13.2–26.9) | 26.1 (20.5–31.8) |
| Non-Hispanic black | 33.1 (26.7–39.4)* | 23.9 (13.3–34.4) | 35.5 (28.1–42.8) |
| Hispanic | 27.7 (22.9–32.5) | 18.9 (10.3–27.5) | 32.0 (26.5–37.5) |
| Non-Hispanic other | 37.7 (27.3–48.2)** | 25.0 (9.4–40.7) | 44.3 (32.6–56.0)** |
| Family income expressed as a percentage of the FPL, %a | |||
| ≥400 (ref) | 30.4 (23.4–37.4) | 30.5 (18.9–42.1) | 30.3 (19.6–41.0) |
| 200–<400 | 21.6 (15.6–27.5) | 15.5 (7.3–23.7)* | 27.0 (17.8–36.2) |
| 100–<200 | 25.9 (20.9–30.9) | 13.8 (5.0–22.7)*,b | 31.8 (25.4–37.4) |
| <100 | 32.3 (27.9–36.8) | 14.2 (6.0–22.4)* | 36.9 (31.5–42.4) |
| Education of head of householdc | |||
| College graduate (ref) | 27.8 (22.2–33.4) | 26.2 (17.9–34.5) | 30.2 (21.1–39.2) |
| Some college | 29.0 (23.9–34.2) | 20.6 (12.8–28.5) | 33.2 (26.8–39.8) |
| Less than or equal to high school diploma | 25.7 (22.1–29.3) | 10.7 (4.9–16.6)** | 30.5 (26.3–34.8) |
| Health insurance | |||
| Private (ref) | 26.4 (22.2–30.6) | 24.4 (17.3–31.4) | 28.4 (22.1–34.6) |
| Other insurance | 27.9 (24.8–31.0) | 13.1 (8.4–17.8)** | 32.9 (29.2–36.5) |
| Uninsured | 25.0 (12.3–27.8) | 23.2 (4.9–41.5)b | 27.5 (8.3–46.7)b |
| WIC benefit, childd | |||
| No (ref) | 25.5 (20.9–30.2) | 23.1 (14.7–31.4) | 28.1 (20.6–35.6) |
| Yes | 28.0 (24.6–31.3) | 12.2 (5.9–18.6) | 31.2 (27.3–35.1) |
Data presented as % (95% CI). ref, reference group.
n = 1324 for analysis of poverty level because of missing data.
RSE >30% and <40%.
n = 1390 for analysis of education of head of household because of missing data.
n = 1096 for analysis of WIC benefit in last 12 mo because of missing data and data only available for 2009–2014.
P < .05 in comparison with reference group.
P < .01 in comparison with reference group.
Among breastfeeding infants, those in families ≥400% of FPL were approximately twice as likely to meet guidelines compared with those in any other income group (30.5% vs 15.5% for 200%–<400%, 13.8% for 100%–<200%, and 14.2% for <100%; P < .05 for all pairwise comparisons). Breastfeeding infants in families with a head of household who was a college graduate were more likely than those in families with a head of household with less than a high school education to meet guidelines (26.2% vs 10.7%; P < .05), and breastfeeding infants with private insurance were more likely than those with other insurance (ie, government programs) to meet guidelines (24.4% vs 13.1%; P < .05). No differences were seen in the percentage of breastfeeding infants meeting guidelines by age, sex, race/ethnicity, or receipt of WIC benefits.
Among nonbreastfeeding infants, infants 0 to 5 months of age were more likely to meet guidelines than infants 6 to 11 months of age (36.1% vs 27.7%; P < .05). Also, non-Hispanic other nonbreastfeeding infants were more likely to meet guidelines compared with non-Hispanic white nonbreastfeeding infants (44.3% vs 26.1%, respectively; P < .01). There were no differences in the percentage of nonbreastfeeding infants meeting guidelines by sex, family income, education level of head of household, health insurance status, or receipt of WIC benefits.
In adjusted analyses, the percentages in each category meeting guidelines and differences observed between categories were generally similar to those found in unadjusted analyses, although some unadjusted differences were no longer statistically significant (Table 3). Overall, nonbreastfeeding infants were still more likely to meet guidelines than breastfeeding infants (33.4% vs 19.2%, respectively; P < .01), and non-Hispanic other infants remained more likely than non-Hispanic white infants to meet guidelines (36.7% vs 24.4%, respectively; P < .05). However, the percentage meeting guidelines was no longer significantly greater for non-Hispanic black infants compared with non-Hispanic white infants. Among breastfeeding infants, infants in families with a head of household who was a college graduate were still more likely than those in families with a head of household with less than a high school education to meet guidelines (24.4% vs 9.7%; P < .05). However, differences observed in the unadjusted analysis by family income and health insurance status were no longer statistically significant. Among nonbreastfeeding infants, non-Hispanic other nonbreastfeeding infants remained more likely to meet guidelines compared with non-Hispanic white nonbreastfeeding infants (46.0% vs 28.0%, respectively; P < .05), but infants 0 to 5 months of age were not more likely to meet guidelines than infants 6 to 11 months of age.
TABLE 3.
Adjusted Percentage of US Infants Meeting the 2008 AAP Recommended Vitamin D Intake Guideline by Breastfeeding Status and Selected Demographic Characteristics, 2009–2016
| Total (N = 1299) | Breastfeeding Infants (n = 425) | Nonbreastfeeding Infants (n = 874) | |
|---|---|---|---|
| Breastfeeding status | |||
| Breastfeeding (ref) | 19.2 (14.3–24.2) | N/A | N/A |
| Nonbreastfeeding | 33.4 (29.3–37.4)** | N/A | N/A |
| Age, mo | |||
| 0–5 (ref) | 31.0 (26.3–35.7) | 20.2 (14.6–25.9) | 37.4 (31.2–43.6) |
| 6–11 | 25.2 (21.2–29.2) | 19.8 (12.0–27.6) | 29.2 (24.2–to 34.2) |
| Sex | |||
| Male (ref) | 29.3 (25.1–33.5) | 22.2 (15.2–29.3) | 33.6 (28.0–39.1) |
| Female | 26.3 (22.0–30.6) | 17.9 (11.3–24.6) | 31.4 (26.1–36.6) |
| Race and/or ethnicity | |||
| Non-Hispanic white (ref) | 24.4 (20.1–28.6) | 18.1 (12.2–23.9) | 28.0 (22.0–34.0) |
| Non-Hispanic black | 31.9 (25.2–38.5) | 27.8 (13.3–42.3) | 34.9 (27.0–42.8) |
| Hispanic | 29.2 (23.5–34.9) | 23.0 (11.4–34.7) | 33.4 (27.1–39.7) |
| Non-Hispanic other | 36.7 (26.3–47.1)* | 25.0 (10.7–39.3) | 46.0 (32.8–59.2)* |
| Family income expressed as a percentage of the FPL, % | |||
| ≥400 (ref) | 30.3 (21.8–38.8) | 25.0 (15.4–34.7) | 30.7 (18.1–43.2) |
| 200–<400 | 22.4 (15.8–29.0) | 15.0 (7.4–22.6) | 27.6 (18.1–37.1) |
| 100–<200 | 25.7 (20.2–31.3) | 17.3 (5.6–29.0) | 30.7 (24.2–37.1) |
| <100 | 32.3 (25.2–39.5) | 21.7 (5.7–37.8) | 37.7 (30.2–45.1) |
| Education of head of household | |||
| College graduate (ref) | 32.8 (25.0–40.6) | 24.4 (16.4–32.4) | 34.9 (23.1–46.8) |
| Some college | 29.3 (23.7–34.8) | 20.0 (12.3–27.8) | 34.9 (28.5–41.3) |
| Less than or equal to high school diploma | 23.7 (19.9–27.6) | 9.7 (3.0–16.4)* | 30.1 (25.5–34.8) |
| Health insurance | |||
| Private (ref) | 29.0 (23.8–34.1) | 21.2 (14.3–28.1) | 33.0 (25.7–40.4) |
| Other insurance | 26.7 (22.9–30.5) | 14.8 (5.2–24.5) | 32.4 (27.6–37.2) |
| Uninsured | 29.4 (13.8–44.9) | 28.0 (4.1–5.2) | 28.0 (7.9–48.1) |
| WIC benefit, childa | |||
| No (ref) | 28.5 (22.1–34.9) | 20.7 (13.6–27.9) | 33.1 (22.9–43.4) |
| Yes | 27.2 (22.6–31.7) | 15.9 (6.7–25.0) | 31.2 (26.2–36.2) |
Data presented as % (95% CI). Adjusted models are adjusted for all other covariates presented. N/A, not applicable; ref, reference group.
Estimates for meeting vitamin D guidelines by WIC status are from separate models with data available for 2009–2014 only. Complete results for this model are available in Supplemental Table 4. Sample size for models used to obtain estimates by WIC status: overall N = 989; for breastfeeding infants n = 292; and for nonbreastfeeding infants n = 697.
P < .05 in comparison with reference group.
P < .01 in comparison with reference group.
Discussion
In this study, we did not observe any increase in meeting the guidelines for vitamin D intake among US infants from 2009–2010, right after the new AAP vitamin D intake guidelines were first released, to 2015–2016, the most recent years of data available. Indeed, the overall rate of meeting the guidelines in 2015–2016 is only 28.2%, with 20.8% of breastfeeding infants and 35.3% of nonbreastfeeding infants meeting guidelines. In addition, the lack of an increase over time in the percentage of infants who meet guidelines does not appear to be attributable to temporal shifts in demographics or breastfeeding rates. In addition, we identified only one demographic subgroup to have >40% of infants meeting the guidelines: nonbreastfeeding infants of non-Hispanic other race and/or ethnicity, who comprise only 6% of the infant population. This group includes Asian, American Indian and Alaskan native, Native Hawaiian or Pacific Islander, and other (including multiracial) infants.
All guidelines published since 2010 worldwide suggest that infant vitamin D intake should be 400 IU per day.28 However, authors of few population studies have examined infant vitamin D intake. One nationally representative study from Canada in 2003 revealed that ∼50% of infants who were breastfeeding at 6 months were being supplemented.29 However, more recent regional studies from Canada suggest higher rates. A cohort study of infants born at a hospital in Montreal in 2007–2008 revealed that 74% of breastfeeding infants met vitamin D intake guidelines (400 IU per day),30 and a more recent larger study from Vancouver revealed that nearly 90% of breastfeeding infants received vitamin D supplementation.31 These rates are far above those found for the United States in our study.
Reasons for low rates of meeting guidelines in the United States and little improvement over time are not fully known. One factor may be that the impact of low vitamin D in infancy is not highly visible to physicians because rickets is an uncommon diagnosis in the United States.32 In addition, enthusiasm for clinically assessing adherence may be limited because there is conflicting evidence for the effect of low vitamin D in infancy on some health outcomes, such as atopic diseases,33,34 and for outcomes with stronger causal evidence, such as type I diabetes mellitus, there is a delay in onset from the time of infancy.3,33–36 Other reasons may include a lack of physician awareness or disagreement with guidelines,37,38 inadequate physician communication to caregivers,39 or failure to adhere to physician recommendations by caregivers.40 Although extensive research has been conducted in the area of guideline implementation science,41 the expected time lag between guideline publication and implementation at a national level is not well described, although this lag is thought to take several years and likely varies by the type of guideline.10 Nonetheless, if the United States was moving toward higher rates of meeting infant vitamin D intake guidelines, we would have expected to observe some improvement during the study period.
Overall, among sociodemographic factors examined, only race and/or ethnicity was related to meeting the vitamin D intake guidelines, with non-Hispanic black and non-Hispanic other infants meeting guidelines at a higher rate than non-Hispanic white infants, and this is due to higher intake of formula among these race and/or ethnicity groups.
We found distinct demographic patterns after stratification by breastfeeding status. Among breastfeeding infants, infants in families of lower socioeconomic status (lower income, nonprivate insurance, and with caregivers with less than a high school education) were less likely to meet guidelines for intake. Of note, even after controlling for health insurance status and family income, lower education of the head of household was still a predictor of failing to meet guidelines, whereas health insurance status and family income were not. This may suggest that education level is the most important factor in receipt of supplementary vitamin D among breastfeeding infants. However, other factors associated with education that we did not include in our analysis may also have contributed to the observed effect. These findings appear to be novel. The aforementioned Vancouver study revealed higher vitamin D supplementation with increasing family income among breastfeeding infants (nonsignificant), but it did not find any relationship with parental education level.31
In contrast, among nonbreastfeeding infants, meeting intake guidelines did not differ by socioeconomic factors. This suggests that although infants in families with lower socioeconomic status are less likely to be given supplements to meet guidelines, they are not less likely to be given enough formula to meet guidelines. Overall, our findings support incorporating breastfeeding status and socioeconomic status into the design considerations of future efforts to help infants meet vitamin D intake guidelines.
This study has limitations. In previous research, authors have explored alternative approaches of providing breastfed infants with adequate levels of vitamin D, including bolus doses of vitamin D to infants42 and supplementing nursing mothers with large doses of vitamin D (self-supplementation).43–45 In one study, mothers stated that they would prefer the approach of self-supplementation to infant supplementation, most often because mothers believed it was safer for their infant.40 One limitation of our study was that it would not have captured these approaches, although neither were in widespread use during 2009–2016 in the United States. Our study also would not capture vitamin D supplementation or formula intake for days other than the single 24-hour period of intake assessed in the day 1 dietary recall; therefore, results based on usual intake may differ. In addition, in our analysis, we did not take into account food or cow’s milk sources of vitamin D. Despite AAP recommendations that cow’s milk not be given before 1 year of age,21 an analysis of NHANES data from 2003 to 2010 revealed that nearly 13% of infants <1 year of age drank regular nonformula milk products.46 Although accounting for cow’s milk consumption may have resulted in an increase in the percentage of infants meeting an intake of at least 400 IU per day, particularly as they age closer to one year, these same infants would be at risk for iron-deficiency anemia, lack of ideal nutritional intake, and a possible increase in risk for type 1 diabetes mellitus.47 In addition, they would not be adherent to the AAP guideline to introduce cow’s milk beverages after 1 year of age.21 Another limitation of our study was that parents may have inaccurate recall, and recall bias could exist because of the social desirability of adhering to guidelines. Also, in our study, we examined adherence with vitamin D intake guidelines for infants rather than serum 25 hydroxy vitamin D levels, which were not collected in the NHANES for participants <1 year of age. However, if serum levels were available for participants <1 year of age, understanding the relationship between adherence with guidelines and 25 hydroxy vitamin D levels would have been of great value.
Conclusions
In this study, we found that there was no improvement in the rates of meeting the AAP vitamin D intake guidelines for infants during the first 8 years after their release in 2008. Additionally, although <40% of infants met guidelines in nearly all demographic subgroups, among breastfeeding infants, lower socioeconomic status was associated with increased risk of failing to meet the vitamin D intake guidelines. These findings suggest that renewed consideration of how to best meet vitamin D intake guidelines is warranted.
Glossary
- AAP
American Academy of Pediatrics
- CI
confidence interval
- FPL
federal poverty level
- RSE
relative SE
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institutes of Health.
Dr Simon drafted the initial manuscript; and all authors conceptualized and designed the study, conducted the analysis, reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Ahrens is supported by a faculty development grant from the Maine Economic Improvement Fund. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Wagner CL, Greer FR; American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee on Nutrition . Prevention of rickets and vitamin D deficiency in infants, children, and adolescents [published correction appears in Pediatrics. 2009;123(1):197]. Pediatrics. 2008;122(5):1142–1152 [DOI] [PubMed] [Google Scholar]
- 2.US Food and Drug Administration.Nutrient specifications, 21 CFR §107.100 (2019). Available at: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=107.100. Accessed October 16, 2019
- 3.Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D and Calcium In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds.. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academies Press; 2011 [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics Dietary reference intakes for calcium and vitamin D. Pediatrics. 2012;130(5). Available at: www.pediatrics.org/cgi/content/full/130/5/e1424 [Google Scholar]
- 5.Abrams SA. Dietary guidelines for calcium and vitamin D: a new era. Pediatrics. 2011;127(3):566–568 [DOI] [PubMed] [Google Scholar]
- 6.Golden NH, Abrams SA; Committee on Nutrition . Optimizing bone health in children and adolescents. Pediatrics. 2014;134(4). Available at: www.pediatrics.org/cgi/content/full/134/4/e1229 [DOI] [PubMed] [Google Scholar]
- 7.Perrine CG, Sharma AJ, Jefferds ME, Serdula MK, Scanlon KS. Adherence to vitamin D recommendations among US infants. Pediatrics. 2010;125(4):627–632 [DOI] [PubMed] [Google Scholar]
- 8.Ahrens KA, Rossen LM, Simon AE. Adherence to vitamin D recommendations among US infants aged 0 to 11 months, NHANES, 2009 to 2012. Clin Pediatr (Phila). 2016;55(6):555–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor JA, Geyer LJ, Feldman KW. Use of supplemental vitamin D among infants breastfed for prolonged periods. Pediatrics. 2010;125(1):105–111 [DOI] [PubMed] [Google Scholar]
- 10.Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watnick CS, Binns HJ, Greenberg RS. Improved vitamin D supplementation in hospitalized breastfed infants through electronic order modification and targeted provider education. Hosp Pediatr. 2015;5(3):119–126 [DOI] [PubMed] [Google Scholar]
- 12.Le B. Vitamin D patient education with a provided prescription prior to newborn discharge improves adherence to vitamin D recommendation in infants returning to clinic for follow-up [abstract]. Pediatrics. 2019;144(2, Meeting Abstract):162 [Google Scholar]
- 13.Drake A, Lustik M, Sampert C. Improving vitamin D supplementation rates in the neonate [abstract]. Pediatrics. 2018;142(1, Meeting Abstract):603 [Google Scholar]
- 14.Kadakia S, Cabasso A, Siu A, St Fleur R. Improving vitamin D administration to breastfeeding newborns using a quality improvement model* [abstract]. Pediatrics. 2018;141(1, Meeting Abstract):290 [Google Scholar]
- 15.Shaikh U, Natale JE, Nettiksimmons J, Li ST. Improving pediatric health care delivery by engaging residents in team-based quality improvement projects. Am J Med Qual. 2013;28(2):120–126 [DOI] [PubMed] [Google Scholar]
- 16.Patel RA, Zargham S. Quality improvement: vitamin D supplementation in breastfeeding infants in a pediatric resident continuity clinic. In: AAP Experience National Conference and Exhibition; October 11–14, 2014; San Diego, CA: Available at: https://aap.confex.com/aap/2014/webprogrampress/Paper26404.html. Accessed October 9, 2019 [Google Scholar]
- 17.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. Vital Health Stat 2. 2014;(162):1–33 [PubMed] [Google Scholar]
- 18.Curtin LR, Mohadjer LK, Dohrmann SM, et al. National Health and Nutrition Examination Survey: sample design, 2007–2010. Vital Health Stat 2. 2013;(160):1–23 [PubMed] [Google Scholar]
- 19.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National Health and Nutrition Examination Survey: plan and operations, 1999–2010. Vital Health Stat 1. 2013;(56):1–37 [PubMed] [Google Scholar]
- 20.National Institutes of Health Office of Dietary Supplements; US Department of Agriculture. Dietary supplement ingredient database. 2019. Available at: https://dietarysupplementdatabase.usda.nih.gov/Conversions.php. Accessed October 15, 2019
- 21.American Academy of Pediatrics Committee on Nutrition The use of whole cow’s milk in infancy. Pediatrics. 1992;89(6 pt 1):1105–1109 [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. National Health and Nutrition Examination Survey: 2015-2016 data documentation, codebook, and frequencies: dietary interview - total nutrient intakes, first day (DR1TOT_I). Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/DR1TOT_I.htm#DRABF. Accessed October 17, 2019
- 23.National Center for Health Statistics. National Health and Nutrition Examination Survey: 2015-2016 data documentation, codebook, and frequencies: demographic variables and sample weights (DEMO_I). 2017. Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/DEMO_I.htm. Accessed October 29, 2019
- 24.Rao JNK, Scott AJ. On simple adjustments to chi-square tests with survey data. Ann Stat. 1987;15(1):385–397 [Google Scholar]
- 25.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 26.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160(4):301–305 [DOI] [PubMed] [Google Scholar]
- 27.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46 [PubMed] [Google Scholar]
- 28.Pludowski P, Holick MF, Grant WB, et al. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125–135 [DOI] [PubMed] [Google Scholar]
- 29.Millar WJ, Maclean H. Breastfeeding practices. Health Reports. 2005;16:23–3116190322 [Google Scholar]
- 30.Gallo S, Jean-Philippe S, Rodd C, Weiler HA. Vitamin D supplementation of Canadian infants: practices of Montreal mothers. Appl Physiol Nutr Metab. 2010;35(3):303–309 [DOI] [PubMed] [Google Scholar]
- 31.Crocker B, Green TJ, Barr SI, et al. Very high vitamin D supplementation rates among infants aged 2 months in Vancouver and Richmond, British Columbia, Canada. BMC Public Health. 2011;11:905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singleton R, Lescher R, Gessner BD, et al. Rickets and vitamin D deficiency in Alaska native children. J Pediatr Endocrinol Metab. 2015;28(7–8):815–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saggese G, Vierucci F, Boot AM, et al. Vitamin D in childhood and adolescence: an expert position statement. Eur J Pediatr. 2015;174(5):565–576 [DOI] [PubMed] [Google Scholar]
- 34.Yepes-Nuñez JJ, Brożek JL, Fiocchi A, et al. Vitamin D supplementation in primary allergy prevention: systematic review of randomized and non-randomized studies. Allergy. 2018;73(1):37–49 [DOI] [PubMed] [Google Scholar]
- 35.Kulie T, Groff A, Redmer J, Hounshell J, Schrager S. Vitamin D: an evidence-based review [published correction appears in J Am Board Fam Med. 2010;23(1):138]. J Am Board Fam Med. 2009;22(6):698–706 [DOI] [PubMed] [Google Scholar]
- 36.Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: a systematic review and meta-analysis. Arch Dis Child. 2008;93(6):512–517 [DOI] [PubMed] [Google Scholar]
- 37.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465 [DOI] [PubMed] [Google Scholar]
- 38.Sherman EM, Svec RV. Barriers to vitamin D supplementation among military physicians. Mil Med. 2009;174(3):302–307 [DOI] [PubMed] [Google Scholar]
- 39.Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication. Patients’ response to medical advice. N Engl J Med. 1969;280(10):535–540 [DOI] [PubMed] [Google Scholar]
- 40.Umaretiya PJ, Oberhelman SS, Cozine EW, Maxson JA, Quigg SM, Thacher TD. Maternal preferences for vitamin D supplementation in breastfed infants. Ann Fam Med. 2017;15(1):68–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, Benrimoj SI. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Syst. 2015;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huynh J, Lu T, Liew D, et al. Vitamin D in newborns. A randomised controlled trial comparing daily and single oral bolus vitamin D in infants. J Paediatr Child Health. 2017;53(2):163–169 [DOI] [PubMed] [Google Scholar]
- 43.Oberhelman SS, Meekins ME, Fischer PR, et al. Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1378–1387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wagner CL, Hulsey TC, Fanning D, Ebeling M, Hollis BW. High-dose vitamin D3 supplementation in a cohort of breastfeeding mothers and their infants: a 6-month follow-up pilot study. Breastfeed Med. 2006;1(2):59–70 [DOI] [PubMed] [Google Scholar]
- 45.Basile LA, Taylor SN, Wagner CL, Horst RL, Hollis BW. The effect of high-dose vitamin D supplementation on serum vitamin D levels and milk calcium concentration in lactating women and their infants. Breastfeed Med. 2006;1(1):27–35 [DOI] [PubMed] [Google Scholar]
- 46.Rossen LM, Simon AE, Herrick KA. Types of infant formulas consumed in the United States. Clin Pediatr (Phila). 2016;55(3):278–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leung AK, Sauve RS. Whole cow’s milk in infancy. Paediatr Child Health. 2003;8(7):419–421 [DOI] [PMC free article] [PubMed] [Google Scholar]