SUMMARY
The head and neck district represents one of the most frequent sites of cancer, and the percentage of metastases is very high in both loco-regional and distant areas. Prognosis refers to several factors: a) stage of disease; b) loco-regional relapses; c) distant metastasis. At diagnosis, distant metastases of head and neck cancers are present in about 10% of cases with an additional 20-30% developing metastases during the course of their disease. Diagnosis of distant metastases is associated with unfavorable prognosis, with a median survival of about 10 months. The aim of the present review is to provide an update on distant metastasis in head and neck oncology. Recent achievements in molecular profiling, interaction between neoplastic tissue and the tumor microenvironment, oligometastatic disease concepts, and the role of immunotherapy have all deeply changed the therapeutic approach and disease control. Firstly, we approach topics such as natural history, epidemiology of distant metastases and relevant pathological and radiological aspects. Focus is then placed on the most relevant clinical aspects; particular attention is reserved to tumours with distant metastasis and positive for EBV and HPV, and the oligometastatic concept. A substantial part of the review is dedicated to different therapeutic approaches. We highlight the role of immunotherapy and the potential effects of innovative technologies. Lastly, we present ethical and clinical perspectives related to frailty in oncological patients and emerging difficulties in sustainable socio-economical governance.
KEY WORDS: head and neck oncology, distant metastasis, radiotherapy, chemotherapy, immunotherapy, nanomedicine
RIASSUNTO
Il distretto testa e collo rappresenta una delle più comuni sedi di insorgenza di malattie oncologiche, con una percentuale di disseminazioni metastatiche elevata tanto a livello loco-regionale quanto a distanza. La prognosi di questi tumori è strettamente legata ad alcuni fattori principali: a) lo stadio della malattia; b) le recidive loco-regionali; c) le metastasi a distanza. Nei tumori della testa e del collo le metastasi a distanza sono presenti in circa il 10% dei casi al momento della prima diagnosi e si rendono evidenti nel corso della malattia in un ulteriore 20%-30% dei casi. Quando una metastasi a distanza a partenza da un tumore della testa e del collo si rende evidente, la prognosi viene usualmente considerata infausta, con una sopravvivenza media stimabile intorno ai 10 mesi. Scopo del presente lavoro è quello di fornire un up-todate aggiornato ed esaustivo in tema di metastasi a distanza in oncologia cervico-cefalica alla luce delle più recenti conoscenze. Concetti di recente acquisizione quali l’assetto molecolare dei tumori, le possibili interazioni tra cellule tumorali e tessuti, le peculiarità della malattia oligometastatica, il ruolo dell’immunoterapia… stanno profondamente cambiando l’approccio terapeutico in questi pazienti, con interessanti ricadute in tema di controllo di malattia. I primi capitoli sono dedicati alla storia naturale ed all’epidemiologia delle metastasi a distanza nei tumori della testa e del collo ed al loro inquadramento diagnostico anatomo-patologico e radiologico. Nei capitoli successivi vengono focalizzate le più rilevanti peculiarità cliniche con particolare attenzione agli argomenti di recente attualità quali le metastasi a distanza da tumori EBV ed HPV positivi ed il concetto di malattia oligometastatica. Ampio spazio viene destinato alle varie opzioni terapeutiche con particolare attenzione al sempre più rilevante ruolo dell’immunoterapia ed allo sviluppo di nuove tecnologie terapeutiche. In conclusione, vengono focalizzate le problematiche etico-cliniche legate al concetto di fragilità del paziente oncologico e le crescenti difficoltà di una sostenibile governance socio-economica.
PAROLE CHIAVE: oncologia testa e collo, metastasi a distanza, radioterapia, chemioterapia, immunoterapia, nanomedicina
LIST OF ACRONYMS AND ABBREVIATIONS
ACC: Adenoid Cystic Carcinoma
ACHT: Adjuvant ChemoTherapy
ADR: Adriamycin
AiCC: Acinic Cell Carcinoma
AIOCC: Italian Association of Head and Neck Oncology
AIOM: Italian Association of Medical Oncology
AJCC: American Joint Committee On Cancer
ALK: Anaplastic Lymphoma Kinase
APC: Antigen Presenting Cells
APM: Antigen Presenting Machinery Cells
ASCO: American Society of Clinical Oncology
ATC: Metastatic Anaplastic Thyroid Cancer
AuroLase®: silica-gold nanoshells coated with (poly) ethylene glycol (PEG)
BED: Biologically Effective Doses
BRAF: Human gene that encodes a protein called B-Raf
BSCC: Basaloid Squamous Cell Carcinoma
CAF: Cancer Associated Fibroblasts
CALAA-01: targeted nanocomplex that contains anti-R2 siRNA
CBDCA: Carboplatin
CCI: Charlson Comorbidity Index
CCRT: Concurrent Chemo-RadioTherapy
CCT/hnCT-MRI: chest CT/head and neck CT or MRI
CD44: Cell surface adhesion receptor
CDDP: Cisplatin
cEBRT: conventional External Beam Radiotherapy
CET:Cetuximab
CGA: Comprehensive Geriatric Assessment
CHT: Chemotherapy
CK: Cytokeratin
CK 7: Cytokeratin 7
CK19: Cytokeratin 19
CK 20: Cytokeratin 20
c-MET: tyrosine-protein kinase Met CNPs: Carbon Nanoparticles
CNS: Central Nervous System
Combidex®: Ferumoxtran-10
COX: Cyclooxygenase
CPS: Combined Positive Score
cRGDY: cyclo-[Arg-Gly-Asp-Tyr] peptides
CRT: Cancer Research Technology
CRUK: Cancer Research UK
CT: Computed Tomography
CTCs: Circulating Tumour Cells
CTx: Cancer Therapeutics CRC Australia
CXR/hnCT-MRI: chest XRay/head and neck CT or MRI
CYC: Cyclophosphamide
DC: Distant Control
DFI: Disease-Free Interval
DFS: Disease-Free Survival
DM: Distant Metastasis
DMFS: Distant Metastases-free survival
DNA: Deoxyribonucleic Acid
DOX: Doxorubicin
DP: Distant Progression
DSS: Disease-Specific Survival
DTX: Docetaxel
DWIBS: Diffusion-Weighted Imaging with background body signal suppression
DWMRI: diffusion-weighted MRI
EBRT: External Beam Radiotherapy
EBV: Epstein-Barr Virus
EC: Oesophageal Cancer
ECM: ExtraCellular Matrix
EFS: Edmonton Frailty Scale
EGFR: Epidermal Growth Factor Receptor
EMA: European Medicines Agency
EMT: Epithelial to Mesenchymal Transition
ENE: ExtraNodal Extension
EPR: Enhanced Permeability and Retention Effect
ER: Oestrogen Receptor
ESCs: Embryonic Stem Cells
ESMO: European Society of Medical Oncology
FDA: Food and Drug Administration
FDG PET: 18F-Fluorodeoxyglucose Positron Emission Tomography
FET: 18Fluoroethyltyrosine
FLT: 18Fluorothymidine
FLT-3: Fms related Tyrosine Kinase 3
FNAB: Fine Needle Aspiration Biopsy
FNAC: Fine Needle Aspiration Cytology
FU: Follow-Up
GATA-3: G-A-T-A binding protein 3
GEM: Gemcitabine
G- CSF: Granulocyte Colony-Stimulating Factor
GEJ :Gastro-oesophageal junction
GFI: Groningen Frailty Index
GP: Gemcitabine plus Cisplatin
GSEA: Gene Set Enrichment Analysis
HA: Hyaluronic acid
HDC: High Dose Cisplatin
HER 2: Human Epidermal Growth Factor Receptor 2
HGF: Hepatocyte Growth Factor
HGFR: Hepatocyte Growth Factor Receptor
HIF: Hypoxia Inducible Factor
HKLA: Human Leucocyte Antigen
HNC: Head and Neck Cancer
HNSCC: Head and Neck Squamous Cell Carcinoma
HNSTS: Head and Neck Soft Tissue Sarcomas
HPV: Human Papilloma Virus
HR: Hormone Receptor
HSA: Human Serum Albumin
ICIs: Immunocheckpoint Inhibitors
ICHT: Induction Chemotherapy
IDO: Indoleamine 2-3-dyoxigenase
IFN: Interferon
IGF-1R: Insulin-like Growth Factor-1
IMRT: Intensity-Modulated Radiotherapy
iPSCs: induced Pluripotent Stem Cells
IRML: International Registry of Lung Metastasis
ISTAT: Italian Institute of Statistics
IT: Immunotherapy
IV: Intravenously administration
LC: Langherhans Cells
LoC: Local Control
LMP1: Latent Membrane Protein 1
LN: Lymph Nodes
LPFS: Locoregional Progression Free Survival
LRF: Locoregional-Free Recurrence
Lu177: Lutetium177
MARCH: Meta-Analysis of Radiotherapy in Carcinomas of Head and Neck
MEC: Mucoepidermoid Carcinoma
mFI: modified Frailty Index
MHC: Major Histocompatibility Complex
Mid-EBV: Midpoint EBV-DNA
MMP: Matrix Metalloproteinase - (1-2-3-9)
MNO2: Manganese dioxide
MOA: Mechanism of Action
MPS: Mononuclear Phagocytic System
MRI: Magnetic Resonance Imaging
MSGT: Malignant Salivary Glands Tumours
mTID: metastatic Tumor-in-a-Dish
mTOR: Mammalian Target of Rapamycin
MTX: Methotrexate
NAB: Nanoparticle Albumin-Bound
NACHT: NeoadjuvantChemoTherapy
NCCN: National Comprehensive Cancer Network
ND: Neck Dissection
NK: Natural Killer
NIR: Near-Infrared
NIVO: Nivolumab
NMs: Nano-Materials
NOS: Reactive Nitrogen Species
NPC: Nasopharyngeal Carcinoma
NPs: Nanoparticles
NSCLC: Non-Small Cell Lung Cancer
NRTKs: Non-Receptor Protein Tyrosine Kinases
NRTKIs: Nonreceptor Tyrosine Kinase Inhibitors
NTRK: Neurotrophic Tyrosine Receptor Kinase
OECD: Organization for Economic Cooperation and Development
OM: Oligometastases
ONB: Olfactory Neuroblastoma
OOC: Organ-On-a-Chip
OPSCC: Oropharyngeal Squamous Cell Carcinoma
ORR: Observed Response Rate
OS: Overall Survival
OSCC: Oral Cavity Squamous Cell Carcinoma
PCR: Polymerase Chain Reaction
PD: Pharmacodynamic
PD-1: Programmed Death Receptor-1
PDC: Plasmacytoid Dendritic Cells
PDGFR: Platelet-derived Growth Factor Receptor
PD-L1: Programmed Death Ligand 1
PD-L2: Programmed Death Ligand 2
PDMS: Polydimethylsiloxane
PDOs: Patient-derived Organoids
PDT: Photosan-based Photodynamic Therapy
PEG: PolyEthylene Glycol
PEG-Si-Cornell Dots: Silica nanoparticles with, NIR fluorophore, PEG coating, 124I radiolabeled
PEMBRO: Pembrolizumab
PET: Positron Emission Tomography
PFS: Progression Free Survival
PIT: Photo-immunotherapy with EGFR Targeting Antibody
PK: Pharmacokinetic
PLGA: Poly(lactic-co-glycolic acid)
PLiD: multi-cellular lung organoid lung-in-a-dish
PM: Pulmonary Metastasis
PNI:Peri Neural Invasion
PR: Progesterone Receptor
Pre-EBV: pre-treatment plasma EBV-DNA
PS: Performance Status
PSA: Prostatic-Specific Antigen
PSMA: Prostate Specific Membrane Antigen
PTS: Patients
PTSD: Post-Traumatic Stress Disorder
PTSS: Post-Traumatic Stress Symptoms
PTT: Photothermal Therapy
PTX: Paclitaxel
QoL: Quality of Life
RNA: RiboNucleic Acid
RANK: Receptor Activator of NF-kB
RANKL: Receptor Activator of NF-kB ligand
RCC: Renal Cell Carcinoma
RES: Reticuloendothelial System
RFA: Radiofrequency Ablation
RKIP: Raf Kinase Inhibitory Protein
R/M-HNC: Relapsed/Metastatic Head and Neck Cancer
RM-NPC: Recurrent/Metastatic Nasopharyngeal Carcinoma
ROS: Reactive Oxygen Species
ROS-1: proto-oncogene tyrosine-protein kinase-1
RT: Radiotherapy
RTKIs: Receptor Tyrosine Kinase Inhibitors
RTKs: Receptor Tyrosine Kinases
R0: No Residual Tumour
R1: Microscopic Residual Tumour
R2: Macroscopic Residual Tumour
SABR: Stereotactic Ablative Body Radiotherapy
SAP: Survival After Progression
SBRT: Stereotactic Body Radiotherapy
SC: Supraclavicular
SCC: Squamous Cell Carcinoma
SCLC: Small Cell Lung Cancer
SLNs: Sentinel Lymph Nodes
SMA: Smooth Muscle Actin
SNEC: Sinonasal Neuroendocrine Carcinoma
SNUC: Sinonasal Undifferentiated Carcinoma
SRS: Stereotactic Radio-Surgery
STIR: Short Time Inversion-Recovery
SUV: Standardised Uptake Value
TAM: Tumour Associated Macrophages
TAX: Taxol
TBM: Temporal Bone Metastases
TDDS: Targeted Drug Delivery System
TDM1: Ado-TrastuzumabEmtansine 1
TKI: Tyrosine Kinase Inhibitor
TILS: Tumour Infiltrating Lymphocytes
TLR: Tool-Like Receptor
TME: Tumour Microenvironment
TM-LC: Treated Metastases Local Control
TN: Triple Negative
TNF: Tumour Necrosis Factor
TTF-1: Thyroid Transcriptor Factor-1
TRTP: Time To Progression
US: Ultrasound
VEGFA : Vascular Endothelial Growth Factor A
VEGFR: Vascular Endothelial Growth Factor Receptor
VMAT: Volumetric Modulated Arc Therapy
VNB: Vinorelbine
WB: Whole Body
WBRT: Whole Brain Radiation Therapy
5-FU: 5-Fluorouracil
3H1: monoclonal antibody anti-idiotype vaccine
1. Introduction
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common cancer worldwide, with more than 500,000 new cases each year.
Despite ongoing advances in surgery, radiotherapy and chemotherapy, 5-year survival rates still remain under 50%.
Prognosis is strictly conditioned by three main factors:
stage of disease;
loco-regional recurrence;
distant metastases.
Distant metastases (DM) in HNSCC have an incidence around 10% at initial clinical presentation, with an additional 20-30% of patients who will develop DM during the course of their disease.
When DM occur, prognosis in considered dismal, with median overall survival (OS) of around 10 months 1.
In the last decade, renewed knowledge has brought further advances in primary tumour biology, molecular basis of distant spread, diagnostic tools, therapeutic plans and disease control, with palliative intent and, in selected cases, even curative 2,3.
The aim of this review is to provide an updated focus on the emerging insights of biology, diagnosis and therapy of DM in head and neck cancer.
2. Epidemiology and natural history
Introduction
The study of neoplastic head and neck disease has always been the basis of the interpretation of clinical phenomenology. It represents the moment when dynamic aspects of immuno-biological order appear in their definitive state.
Metastatic disease cannot be easily defined because it is preceded and followed by phenomena originated by unforecastable biological reactions limiting or yielding neoplastic aggression.
Clinical diagnostic and therapeutic approaches are projected to performing a precision medicine dimension, that is increasingly effective.
Despite continuous progress with multimodal treatments that have demonstrated genuine improvement in metastatic control, OS and disease-specific survival have not undergone significant changes. New knowledge in neoplastic immune cellular defense and in the pre-clinical phase of the metastatic process is strongly expected.
In fact, in recent years, much progress has been achieved in understanding how biological metastases take place. All these efforts express the intent to identify genetic connections between host and tumour, risk factors that can lead to neoplastic transformation and attitude to local, regional and remote dissemination. Overall, metastatic disease represents the main prognostic factor in HNSCC.
HNSCC, assessed for all sites and all grades of T, demonstrates an index of lymphatic metastasis ranging from 25 to 45% 1. The invasion of the lymphatic network occurs with variable frequency depending on the site, T-stage and histopathological characteristics of the primary lesion (type, degree of differentiation, perineural invasion). Diffusion generally occurs progressively, from the lymph nodes closest to the primitive tumour to the most distant ones. Isolated localisations in lymph nodes distant from the primary lesion are not rare.
Only approximately 10% of patients have DM at the time of diagnosis 2. However, a substantial proportion develops metastases following the first line of treatment for locoregional disease.
It is widely believed that, in the early-stage disease (T1-2, N0), the main clinical problem is loco-regional control. The risk of DM is very low even if, for nasopharyngeal neoplasms and undifferentiated carcinomas, this eventuality must also be considered in the initial stages of the disease.
In the locally-advanced stages (stage III-IV, cM0) the problem becomes more relevant, especially following the therapeutic progress in the last few years on the loco-regional control of the disease.
In 1906, George Crile 3 supported a philosophy on cervical regional lymph nodes as ‘‘an extraordinary barrier through which cancer rarely penetrates.’’ This was a logical conclusion at the time based on the extant clinical data which suggested a rate of less than 1% of DM in over 4,000 autopsies in patients with HNSCC. The concept was simple: cancer cells, which were continuously shed from the primary tumour into draining regional lymphatic vessels, would become lodged in regional lymph nodes and grow just as they did at the primary tumour site. Supported by analogous conclusions about mechanisms of tumour spread in the melanoma and breast cancer literature at the time, the concept that cervical regional lymph nodes act as a filter to trap cancer cells trying to escape the confines of the head and neck was unchallenged for many decades and was also propagated by pioneers in head and neck surgery.
According to several reviews on these topics, we can state that the natural history of HNSCC is essentially influenced by the following factors: primary lesion, lymphatic diffusion and DM.
2.1. Primary lesion
The size of the primary lesion and the potential spread of disease are closely related. The motto, “the larger the tumour, the worse the prognosis” is still valid. The thickness and depth of invasion of the primary tumour are the most important indications of the aggressive nature of the disease.
This is particularly true for cancers of the oral cavity, for laryngeal tumours and for those of the rhinosinusal district. However, carcinomas with a large superficial component appear to be only the superficial invasion of the lamina propria and are less likely to spread to the regional lymph nodes with a better prognosis than those that tend to be invasive.
On the other hand, nasopharyngeal, hypopharyngeal, laryngeal, oropharyngeal and supraglottic tumours show a tendency to lymphovascular invasion due to the rich presence of this system in these areas, leading to early and marked nodal involvement and early DM compared to other subsites (Fig. 2.1).
Figure 2.1.
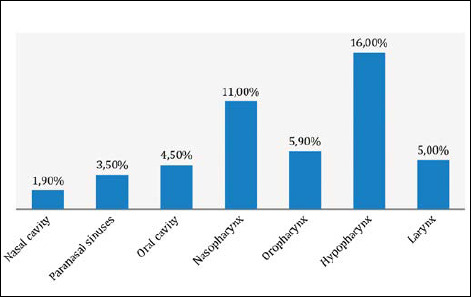
Overall percentage of DM incidence by subsite 11,12,22,23,29-31,35,41.
Although every anatomical subsite has its own unique neoplastic diffusion model, most cervical-cephalic malignancies begin as a superficial mucosal lesion, within which muscle invasion is the rule as is the tendency to spread along with the plane muscles at a considerable distance from the palpable to the visible lesion. A tumour can attach itself to the periosteum or perichondrium very early in the course of the disease, but the actual invasion of bone or cartilage is generally a late event. The periosteum and perichondrium act as a barrier to neoplastic diffusion, and these structures are generally spared while the tumour has explored easier growth paths, either alone (through the activation of osteoclast tumours) or along neural pathways. This model of local diffusion is typical of tumours of the oro-pharyngeal and laryngeal cavities.
Perineural invasion is an important pathway of neoplastic diffusion and is nowadays more than ever recognised as a disturbing sign that correlates with an increase in the incidence of local recurrence, loco-regional lymph node metastases, the availability of information on cranial base nerves and reduced survival. This is a sign of biological aggression of the tumour and is independent on the size of the primary lesion. Moreover, the neurological impact must be added, secondary to compression or entrapment rather than to the actual nervorum invasion 4.
Finally, it should be remembered that neoplastic diffusion also depends on tumour differentiation (classification), the model of tumour invasion and the inflammatory response to the tumour. The more poorly differentiated the tumour, the quicker the ability to metastasise compared to more differentiated tumours. Tumours with large masses are less likely to metastasise than smaller lesions, but with an invasive model.
2.2. Lymphatic spread
The regional state of lymph nodes is one of the most important parameters determining prognosis in patients with HNSCC. The presence of only one positive lymph node can decrease survival by up to 50% 5.
The risk of lymph node metastasis can be predicted in relation to differentiation of tumour (more poorly differentiated, the greater the risk), to the size and depth of the invasion and the availability of capillary lymphatics. Furthermore, the risk of lymphatic spread increases with tumour recurrence. Embryologically, the lymphatic system is formed from its germination from the venous system, and explains the close anatomical relationship between these two systems. Blood capillaries have tight endothelial junctions and normally do not reabsorb larger molecules and cells. However, lymphatic capillaries have relatively open endothelial junctions that allow molecules and larger cells to be more easily reabsorbed, explaining the reason for easier lymphatic than vascular propensity.
The lymphatic system of the head and neck is the region of the body composed by more lymphatic capillaries, lymphatic trunks and lymph nodes; epithelium, bone and cartilage are devoid of lymphatic capillaries, while a small minority is found in the periosteum and perichondrium. Lymph node arrangement is archetypal and each group receives drainage (directly or indirectly) from specific areas; in a deep cervical group (a terminal group for the head and region of the neck) before finally flowing into the lymphatic duct (right)/thoracic duct (left) or in the jugular-subclavian junction 5.
Due to the absence of lymphatic vessels in the epithelium, the tumour must penetrate the lamina propria before lymphatic invasion. In the superficial layer, the diameter of lymphatic capillaries is usually narrower than it is in the deeper layer. The richness of the capillary network in each subsite can increase the relative incidence of lymph node metastases. The nasopharynx, pyriform sinus (hypopharynx), supraglottic larynx and oropharynx have the most profitable network of capillary lymphatic vessels, which is the clinical reflection of the potential presence of neoplastic lymph nodes. Paranasal sinuses, middle ear and vocal folds have few or no capillary lymphatics, which is consistent with the low rate of lymph node metastases when the tumour is confined to these sites.
The involvement of lymph nodes usually follows an ordered progression and, rarely, skip nodal metastasis is revealed 6. Well lateralised lesions determine ipsilateral lymph node metastases. Lesions near the midline or lateral margin of tongue or nasopharyngeal lesions can also spread contralaterally or bilaterally, but generally, tend to spread from the side of the lesion. Patients with ipsilateral tumour nodal disease are at risk of contralateral disease, especially if the lymph node exceeds a certain size or if multiple lymph nodes are involved. Obstruction of lymphatic pathways caused by surgery or radiation therapy can divert lymphatic flow on the opposite side of the neck through anastomotic channels.
Finally, it should be remembered that metastases in cervical-cephalic district occur in approximately 10% of patients as neoplastic metastases from unknown primitive sites 7. The histopathology of these metastases is generally referable to squamous cell carcinomas in various degrees of differentiation, but metastases of adenocarcinomas, melanomas, or anaplastic tumours can also be found. The lymph node level is indicative of possible neoplastic origin.
DM in the absence of nodal metastasis is very rare in HNSCC. Untreated occult disease in the lymphatic venous system can produce DM while the lymph node is growing. Patients with advanced disease have a high incidence of DM, particularly in the presence of jugular vein invasion or extensive soft tissue disease in the neck. The rate of DM increases by up to 25-30% for N3 disease compared to 18-20% for N2 disease (Fig. 2.2) 7.
Figure 2.2.
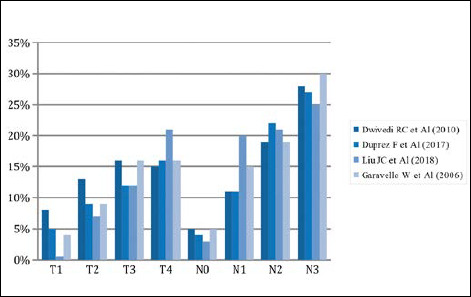
Overall risk percentage of DM according to T and N 7,11,12,46.
Although there is clear evidence on lymph node involvement with DM, presence of N+ in these patients remains controversial for some. Studies have documented the presence of clinically-evident DM in up to 15% of patients with HNSCC who had disease at the time of diagnosis and remained N0 throughout treatment 8.
A recent retrospective study of over 70,000 patients with HNSCC revealed that 2.8% had DM at presentation, and that the rate of DM ranged from 0.19% to 1.75% in patients who were clinically N0 9.
These studies measure the presence of clinical DM and have a large number of false negatives with regards to the presence of circulating tumour cells. Although patients present very frequently with N+ disease and very infrequently with clinically-detectable distant metastases, detection of distant micrometastases with sensitive molecular diagnostics, rather than histological methods, would likely yield a much higher rate of detection of metastasised cancer cells at the time of presentation.
Further research investigating the role of these processes and others may help to explain why patients with HNSCC so commonly initially present with clinically-evident neck disease and not clinically-evident distant metastatic disease.
2.3. Distant spread
DM is defined as tumour that has spread to other organ systems. This phenomenon requires several steps, including migration of cancer cells into blood vessels, survival of cancer cells in systemic circulation and transport to target organs, arrest of cancer cells in microcirculation, migration of cancer cells through the vessel wall into the interstitial space and proliferation of cancer cells in target organs. These steps involve complex biological mechanisms that include many chemotaxis mediators, cell-matrix chemical ligand-receptor interactions and intracellular signalling networks.
Tumour diffusion takes place as follows: 1) hematogenous spread towards distant organs (lung, skin, bone and liver); 2) lymphatic spread towards distant regional lymph nodes (mediastinal, abdominal and axillary nodes). Moreover, DM can occur at diagnosis or, more frequently, later in the course of the disease.
The incidence of head and neck DM at presentation is relatively low compared to other malignancies, but is more elevated in nasopharyngeal and hypopharyngeal cancer. The National Comprehensive Cancer Network (NCCN) currently recommends either a chest radiograph or pulmonary CT to stage patients with head and neck cancer (HNC). Pulmonary CT is strongly suggested in the presence of high metastatic risk. When dealing with aggressive metastatic tumours such as adenoid cystic carcinoma, basaloid squamous cell carcinoma and neuroendocrine carcinomas, an extensive metastatic work-up is widely justified 10.
Frequently, the prevalence or incidence of DM is reported briefly without uniform methodology and as part of secondary endpoints. In addition, information on risk factors for DM is extrapolated from patient follow-up studies after completion of curative treatment and there is no consensus on standard staging procedures for these patients, although accurate staging is very predictive of survival in the long term and the information is essential in the management of the individual patient with HNSCC.
The prevalence is reported to be 9.1%, 14.1% and 15.6% in patients with well (WHO grade 1), moderately (WHO grade 2) and poorly differentiated (WHO grade 3) HNSCC, respectively 11.
In locally-advanced HNSCC, 5-year locoregional control is limited to 50%, while distant control, also called distance metastasis freedom, is about 85% 12. The incidence rates reported in clinical studies fluctuate between 7% and 23%, while autopsy results can vary between 30% and 50% 7.
Due to the wide heterogeneity of HNSCC, the rate of metastasis can be influenced by the primary tumour site, stage at presentation, staging assessment, treatment modality and study population. Most DM occur within the first 2 years of initial diagnosis and, with development of DM, the chance of recovery is very low and survival decreases dramatically even with early diagnosis. Tumours of the hypopharynx, supraglottic larynx, nasopharynx and oropharynx are more likely to spread than those in the oral cavity, paranasal sinuses and glottic larynx. The percentages of DM reported for stages I, II, III, IVa and IVb are, respectively, 1%, 14%, 15%, 20% and 24% (Fig. 2.3) 7-9. The prevalence of DM is reported to be 11.9% and 32.0%, respectively, in the absence and presence of extranodal extension 11.
Figure 2.3.
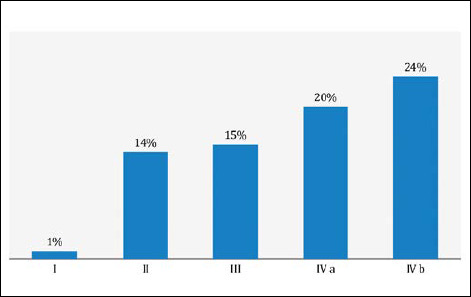
Overall percentages of DM in HNSCC for tumor stages 7-9.
There is no significant difference in the actuarial rate of distant control between the presence or absence of perineural invasion of tumour: 89% and 84% at 1 year, 77% and 78% at 2 years and 77% and 75% at 5 years, respectively 11. Data on lymphovascular invasion do not suggest any significant difference in the actuarial frequency of distant control between presence and absence of lymphovascular invasion. There is no significant difference in the prevalence between tumour-free margins and microscopic or macroscopic invasion 11.
Almost half of all DMs are clinically detected within 9 months of treatment, 80% within 2 years, 90% within 3 years and 99% within 5 years. Their presence is an unfavourable prognostic factor, since 90% of patients die within 2 years following detection of the first metastasis 7. The lung is the most common site of DM (50% -75% cases), while bone, liver, brain, skin and soft tissue represent 10-44%, 4-34%, 3-13%, 3-31% and 2-9%, respectively 10.
2.4. Oligometastatic disease
Hellman and Weichselbaum first proposed the concept of oligometastases (OM) in 1995 suggesting that there is a spectrum of metastatic diseases, some of which may still be considered localised 13.
Although oligometastatic tumour cells have all these characteristics, they appear to have a different genetic profile and may behave less aggressively than widespread metastatic carcinoma. As a result, they “sow” fewer sites and grow more slowly, providing better prognosis and making the tumour even more susceptible to local therapy.
In recent years, the concept of OM has been increasingly recognised and supported by clinical and biological data for several malignant tumours. OM-HNSCC is still a relatively underestimated entity. In this scenario, the most extensive data come from a small series of cases on the surgical management of metastases published over 3 decades. In addition to a few reports on liver injury, most of these retrospective studies refer to pulmonary metastasectomies 14.
Furthermore, OM has been shown to be a distinct clinical entity with respect to polymetastatic disease in other organ systems. In 2017, Albergotti showed a significant difference in survival in HPV-positive metastatic oropharyngeal SCC when stratified by oligometastatic status. Patients with 1-2 metastatic lesions had significantly prolonged OS with a 2-year survival rate of 81% compared to those with polymetastatic disease with a 2-year survival rate of 22% 15. Therefore, OM has been hypothesised to be a less aggressive phenotype, which still lends itself to local control.
In 2019, Bates reported a broader analysis of outcomes in patients with OM-HNSCC treated with stereotactic ablative body radiotherapy (SABR). They showed an encouraging OS rate of 43% at 2 years; however, DFS remained scarce, with only 14% of patients alive without disease progression at 2 years. Despite the non-optimal DFS rate, the results suggest that patients with OM-HNSCC may represent a more favourable subset of patients with metastatic HNSCC 16. The most frequent primary site was the oropharynx (48.1%). Most had metachronous metastases rather than synchronous (81.5%). Most patients had a relatively limited burden of metastatic disease, including 44.4% with solitary metastases, 44.4% with 2-3 metastases and only 11.1% with more than three sites of metastatic disease at the time of SABR. The most frequent site of metastatic disease was pulmonary; other positions of the metastatic disease included the spine, lymph nodes/soft tissues, non-spinal bone and liver 16.
2.5. District analysis
Nasal cavities and paranasal sinuses
Malignant neoplasms of the rhinosinusal district are uncommon diseases, estimated at around 0.8% of all malignant tumours and between 3-5% of head and neck malignancies, with a worldwide incidence of 1/100,000 inhabitants 17. The lymph nodes of levels I, II, parotid and retropharyngeal are the preferred metastatic areas.
Usually, adenopathy ranges between 5.4% and 21%; for squamous cell forms originating from the nasal passages it varies from 6.6% to 10.7% vs 2.6-22.2% for adenocarcinomas; if the origin is paranasal, the value varies from 3.7% to 19.1%; and the maxillary site determines a risk of between 3.9% and 21.4% 18,19. The undifferentiated forms (SNUC) metastasise in a more significant way compared to the differentiated forms: 16.7 vs 13.8% 20.
With respect to T stage, the percentage of lymph node involvement for the nasal cavity is: T1: 4%, T2: 9.8%, T3: 10.3%, T4a 22%; T4b 22.6%, vs. T1: 8.2%; T2: 18.6%; T3: 19.6%; T4a: 21.4%; T4b: 26.8% for the sinus district 21. DM from paranasal tumours is rare (4%); in SNUC, the rate in patients under surveillance is about 2.5%. In SCC of the nasal cavity, the rate is 1.9%, while the rate in SCC of the maxillary sinus is reported to be 6.8% in T4 tumours 22,23.
Risk factors are related to location (nasal floor and columella), size and number of positive lymph nodes.
Oral cavity
The local and distance metastatic tendency of squamous cell carcinomas of the oral cavity (OSCC) is directly related to the location, tumour size, pattern and depth of the invasion. As far as lip neoplasms are concerned, the underlying localisations concern about 95% of tumours showing a metastatic tendency considered to be low, in which the size of the tumour is always correlated with metastatic speed and tendency. In T1 and T2 lesions, metastatic loco regional data is limited to 30% while in T3 to T4 it increases up to 60% 24.
The lingual compartment is characterised by a greater component of lymphatics and neurovascular structures that amplify metastatic risk. In these circumstances, level I lymph nodes are mainly affected, while in tumours of the posterior compartment there is involvement of level II lymph nodes. In contrast to the diffusion model, tongue cancers are more frequent than oral cavity cancers (25-40%), and can also affect level IV lymph nodes in up to 10% of cases 25. A retrospective assessment of 277 tongue cancers showed metastases at level III and IV in 15.8% of cases without level I and II lymph node disease 26.
Overall, approximately 50% of patients with oral cancer reveal lymph node metastases, with an incidence of occult metastases in T1 and T2 tumours of approximately 30-40% 25.
A multivariate analysis of the tumour characteristics of lingual neoplasms has shown that only the depth of tumour has an absolute predictive value for cervical and DM 26. Despite being a randomised study, it indicated the usefulness of prophylactic neck dissection (ND) in case of T thickness > 3 mm, another meta-analysis better specified the relationship between the thickness of infiltration as a predictor of metastasis in tumours of the lingual body, identifying a 4 mm cut-off 27,28.
The presentation reported a lower incidence of DM between 1% and 8.8% for patients with OSCC. The most common metastatic sites are the lung, bone, liver and skin; 13.2% is the rate within 5 years of treatment 29.
When DM rates are directly considered, more than half of patients with contralateral neck metastases and one-third of patients with poorly differentiated tumours showed subsequent DM within 5 years after locoregional treatment with curative intent, and most experienced DM within 2 years 30.
As for the prediction of DM based on tumour differentiation, the results are still controversial, but poorly differentiated tumours with infiltration thickness > 4 mm have higher rates of extranodal extension (ENE), perineural invasion (PNI) and lymphovascular invasion, and may also explain metastasis to the neck and subsequent DM 31.
Nasopharynx
Undifferentiated carcinoma is the most frequent nasopharyngeal tumour; it has a typical pathognomonic histological model, a close relationship with Epstein-Barr virus (EBV), a particular natural history and good prognosis. It has an early tendency to spread locally in the parapharyngeal space. Nodal involvement is very frequent (70-90%) and voluminous regardless of the size of the primary tumour 32.
The natural history of this neoplasm depends on its local growth capacity and its metastasizing potential. In particular, the keratinising histotype shows greater local aggressiveness than the non-keratinizing one, which tends more towards distant diffusion 33.
It must be considered that, since radiotherapy is the main treatment of this neoplasm, the metastatic pattern is essentially based on clinical-radiological data. Spread by the lymphatic system occurs in about 75% of cases (60% of cases with histotype I and 85-90% with histotype II) 33. The first stations involved are retropharyngeal, 94% of cases, followed by the jugular and spinal stations 33. Lymph node involvement represents the initial symptom in 37-49% of cases 34.
The literature reports up to 11% DM at presentation and up to 87% at autoptic studies 34. After treatment, DM develops in about 30% of patients within 5 years (40% in those with locoregional insufficiency and 29% in those with locoregional control) at a median time of 8 months. DM is observed mainly in bone (48%), lung (27%), liver (11%) and in the nodes above the clavicle (10%) 35.
Oropharynx
The lymphatic neoplastic spread of the oropharyngeal region is mainly present in lymph nodes of levels IIB, III and in retropharyngeal ones. In general, the overall N+ rate ranges from 40 to 80%, with lateral occult N+ approximately 8% and contralateral N+ 28.6% 36. At the time of diagnosis, approximately 70% of patients with oropharyngeal squamous cell carcinoma (OPSCC) have lymph node metastasis 37. The correlation with human papilloma virus (HPV), in particular with types 16-18, plays an important role for the development of a subgroup of tumours (about 50%) with different histopathological and morphological features, indicative of a distinct neoplastic diffusion model even in relation to metastatisation, and such as to justify a non-significant loco-regional diffusion associated with the increasing size of the T, which remains predictive only in order of metastatic extension in the N+ of tonsillar complex tumours and those of the base of the tongue (T1: 18%; T2: 24%; T3: 19%; T4; 5%) 38. At the prognostic level, the best loco-regional control secondary to the reduced perineural invasion model, perivascular infiltration and by virtue of tumour-correlatable immunological reactions of HPV-positive cells, explains the better prognosis vs. HPV negative tumours. Against an overall percentage of DM included within 5-7%, Duprez reported an overall prevalence of 12.9% 11.
Hypopharynx
With regards to the typical localisations such as the pyriform sinus, retro-cricoid area and posterior wall, neoplasms are more developed in the region of the pyriform sinus. Lesions that develop in the midline tend to metastasize on both sides of the neck, although there is not enough data to encode a dissemination scheme, particularly for contralateral lymph nodes. The clinical behaviour of these neoplasms is aggressive and is burdened by high locoregional metastatic risk. Considering diagnostic timing frequently in stage III or IV, the incidence of this diffusion varies from 65 to 80% at the time of diagnosis and from 30 to 40% in terms of apparent N0 39. Neoplastic involvement occurs mainly in the ipsilateral lymph nodes of levels II-A, III and rarely IV. Metastasis to the thyroid gland and to level VI lymph nodes is found in 30% of patients 40. This latter event occurs mostly in upper hypopharyngeal-laryngeal and hypopharyngeal-oesophageal tumours, particularly in patients with peristomal recurrence.
In accordance with histopathological and radiological findings, metastases to the retropharyngeal lymph nodes (Rouvière lymph nodes) are found in about 13% of patients, especially in the retro-cricoid localisations in the posterior wall 28. The involvement of these lymph nodes is expressive for a greater propensity to distance metastasisation and poor overall outcomes. For these tumours, besides a direct and significant relationship between tumour size and the incidence of metastasis, the depth of infiltration and degree of differentiation are determinants of metastatic propensity.
Spector reported an overall DM incidence of 16.1% in aryepiglottic folded carcinoma. The incidence of DM was correlated with an increase in TNM stage, locoregional insufficiency, reduction in recovery rates, delayed regional lymph node metastases and advanced regional node disease (N2 + N3). In pyriform sinus carcinoma, the overall incidence of distant metastasis is 17.1% and in the posterolateral hypopharyngeal wall carcinoma is reported at 17.6%. Statistically, the incidence of DM is positively correlated with regional metastatic disease (N + disease) and advanced primary disease (T4) 41.
Larynx
Neoplasms of the supraglottic areas display a greater propensity to lymph node-like neoplastic diffusion, but on par with the glottal region, and have a tendency to invade the lymph nodes of level II and III, while the subglottic areas have a propensity towards lymph nodes of levels III and IV. The involvement of lymph nodes of level I, IIB and V occurs more rarely, justifying surgical conduct aimed at their conservation in N0 cases 42.
In the anterior compartment, the involvement of the paratracheal lymph nodes amounts to 12.2%, especially in the case of anterior subglottic extensions; nevertheless, glottic tumours can rarely metastasize to such level, but generally only in advanced stage lesions (T3-T4) 43. The metastatic disease of these lymph nodes is generally associated with poor prognosis, a high rate of locoregional recurrences and DM.
Overall, about 40% of all supraglottic tumours have locoregional metastases at the time of diagnosis; 6-25% for T1, 30-70% for T2 and 65-80% for T3-T4 with a rate of occult metastases exceeding 20%. The involvement of a central part indicates a high risk of contralateral metastases, whose incidence is around 20% in lateral lesions, remaining infrequent in the absence of ipsilateral metastases 44.
Glottic tumours show a relatively low metastatic rate, which is probably related to the lower lymphatic density of the region. At this level, there is a significant correlation between vocal fold motility and the incidence of lymph node metastases. While vocal fold motility represents a dynamic barrier for lymphatic drainage, the increasing motor impairment (T2-T3) carries an unimpeded lymphatic flow in locoregional lymph nodes.
Extra-laryngeal growth is associated with a significant increase in metastatic tendency (T4). However, no lymphatic metastases are predictable in T1a of the vocal cords, while for T2 tumours the values are between 5 and 10%, in T3 between 10-20% and between 25-40% for T4 45.
Finally, glottal lesions have a low prevalence of contralateral metastases, even if the primary tumour goes beyond the midline 44.
Spector reported an incidence of DM in supraglottic carcinomas of 3.6%. These occurred at 1-75 months after treatment of the primary disease with an average of 23.3 months for central epiglottic tumours; 17.6 months for marginal supraglottic (lateral) tumours and 10 months for lesions extending to the vallecula or the base of the tongue. The incidence of DM is not related to the stage of the primary tumour (stage T) which was as follows: T1 0.9%, T2 5.7%, T3 2.2% and T4 5% 41. DM disease is correlated to the degree of regional lymph node involvement (N + disease) as follows: N0 2.3%, N1 1.3%, N2 6.4% and N3 20% 41.
The incidence of DM in patients with glottal carcinoma is reported to be 4.4%. The progression of tumour stage, a lower rate of locoregional control and a reduction in the recovery rate in stage IV disease significantly increased the overall incidence. The highest incidence is reported in T4N1 and T2-3N2-3 tumours and is significantly related to the higher incidence of regional lymph node metastases delayed in the stages of the disease T4N1, T4N2-3 and T2-3N2-3 41. In the subglottic area, the percentage of DM reported is 14.2% and is not related to the TNM stage 41.
3. Biological factors in metastatic dissemination of head and neck squamous cell carcinomas
It is well established that aggressiveness of head and neck tumours is manifested mainly as local recurrences and lymph node metastases more than distant diffusion. Many cases of local recurrences are due to a sort of biological “condemnation” of the mucosa known as field cancerisation 1, while the pathways of metastatic diffusion are explained by the molecular assets of the tumour or by complex interactions between neoplastic tissue and the tumour microenvironment 2.
In this review, we refer to well-known molecular pathways of local diffusion and metastasis of HNSCC, concerning both field cancerisation and the tissue microenvironment; moreover, we present some recent results of translational research.
3.1. Molecular mediators of lymph node metastasis in head and neck squamous cell carcinoma
Breakdown of cell-to-cell adhesion: E-cadherin /catenin
The Cadherin family of cell adhesion molecules mediates homotypic cell-to-cell adhesion within epithelial cells in a calcium dependent way by means of its extracellular domain and by forming complexes with the actin cytoskeleton through cytoplasmic catenin.
Downregulation or dysfunction of cadherin or catenin produces a loss of integrity in the cell-to-cell adhesion mechanism and subsequent dissociation of epithelial cells, being a prerequisite for active migration and metastasis.
In HNSCC with lymph node metastases, an association between loss of E-cadherin and the catenin complex and the presence of metastasis has been demonstrated. Expression of E-cadherin was significantly lost in the metastatic tissue in comparison to the primary tumour and surrounding normal mucosa 3. Reduced expression or aberrant localization of α-, β- and δ-catenin may be a useful tool to predict the risk of lymph node metastasis 4..
Integrins and cellular surface adhesion receptor (CD44)
Integrins are a family of heterodimeric transmembrane glycoproteins that function as cell surface receptors, composed of non-covalently associated α and β subunits involved in intercellular and cellular-extracellular matrix attachment, contributing to bidirectional exchange between the extra- and intracellular environment.
Aberrant integrin expression has been implicated in HNSCC tumour invasion and metastasis. The most commonly expressed integrin in the basal layer of the normal squamous cell epithelia is αvβ6 and its altered expression has been reported in the development of HNSCC 5.
CD44 is a glycosylated multifunctional cell surface protein that works as a receptor for hyaluronic acid in the extracellular matrix. Multiple isoforms exist due to a mechanism of post-transcriptional splicing. Predominant loss of expression in some isoforms (v4, v5, v6, v9) has been correlated with lymph node metastases 6,7.
Modulation of extracellular matrix and proteolytic enzymes: matrix metalloproteinases (MMP) and cathepsin D
Proteolytic enzymes are implicated in the degradation of extracellular matrix components such as fibronectin, collagen, laminin, glycoproteins and proteoglycans, and favour stromal invasion of tumour cells as well as vessel intravasation and extravasation.
MMPs, a family of zinc dependent endopeptidases secreted in an inactivated form, are involved in the metastatic process. Increased expression and activity of MMPs (the main variants involved are MMP-1, MMP-2 and MMP-9), associated with overexpression of epidermal growth factor receptor (EGFR), has been seen in both HNSCC tumour samples and in their metastases, and is predictive of poor prognosis 8,9.
Cathepsins are lysosomal endopeptidases overexpressed in various types of human carcinomas. In the head and neck area, high levels of Cathepsin-D correlate directly with the presence of lymph node metastases in oral carcinomas 10,11.
Molecular alterations favouring cell motility and tumour cell migration: MET oncogene and EGFR
MET is a proto-oncogene encoding a tyrosine kinase receptor for Scattered Factor also known as hepatocyte growth factor (HGF): it promotes cell proliferation, detachment and motility.
Oncogenically-activated MET can favour growth and give invasive and metastatic properties to clones of neoplastic cells, as demonstrated by the high level of mutant alleles of MET found in metastatic lymph nodes of HNSCC, in comparison to the barely detectable level seen in the corresponding primary tumour 12.
EGFR is a family of transmembrane proteins which includes four members (c-erbB-1/ EGFR, c-erbB-2/Her-2neu, c-erbB-3/Her-3 and c-erbB4/Her-4) that are involved in tumour growth and malignant transformation through their tyrosine kinase activity. The role of theEGFR family in HNSCC has been thoroughly investigated.
Several studies have reported an independent correlation of EGFR members with the presence of nodal metastases and poor clinical outcome, due to cooperative signalling of all EGFR receptor members. They enhance proliferation and invasion of HNSCC cells, by activating the MAPK and PI3K downstream signalling pathways involved in the transcriptional regulation of proteases and cytokines 13.
3.2. Biological aspects of the tissue microenvironment in head and neck squamous cell carcinoma and their influence on aggressiveness and metastatic behaviour
Genetic and epigenetic changes in normal squamous epithelium
A number of studies have demonstrated that genetic changes to the normal epithelium in the mucosa of the upper respiratory and digestive tract are associated with HPV infection (mainly strains 16, 18 and 31) and follow the same pathway described in cervical cancer, via E6 and E7 proteins.
In non-HPV-related HNSCC, the most frequent epithelial genetic change is mutation of the tumour-suppressor gene TP53, present in more than 50% of cases in malignant and pre-malignant lesions. Mutations in TP53 are associated with:
increased migration of cancer associated fibroblasts (CAF), favouring invasiveness and progression of neoplasia 14;
increased production of reactive oxygen species (ROS) and reactive nitrogen species (NOS) driving carcinogenesis via NF-kB and promoting abnormal tumour metabolism through the Warburg effect.
Mutations of NOTCH 1 (transmembrane receptor that regulates cell differentiation and embryonic development) contribute to proliferation and invasiveness through increasing the concentration of TNF by acting on Slug and Twist and its regulation over the epithelial to mesenchymal transition (EMT) 15.
EGFR gene is present in 10% of cases, but gene amplification and overexpression is present in almost 30% and 90% of cases, respectively, allowing for triggering of multiple intracellular signalling cascades that activate cell proliferation and survival, invasion, metastasis and resistance to radiotherapy, all of which are mechanisms that promote tumour aggressiveness 16.
Overexpression and mutation of transcription factors such as STAT3 are involved in EMT, proliferation, apoptosis and inflammation, assuring self-maintenance and renewal of cancer stem cells which helps in progression of cancer cells 17,18.
Epigenetic changes most commonly associated with HNSCC are DNA methylation, histone modification, microRNA and small interfering RNA.
Stromal components of tissue microenvironment that impact aggressiveness
These are mainly cancer associated fibroblasts, cells which are involved in immune response, metabolism, angiogenesis, inflammation, hypoxia and the EMT.
-
Cancer associated fibroblasts.
Fibroblasts, normally residing in the stroma underlying the epithelium of the upper aerodigestive tract, are responsible for the production of the basal membrane layer, collagen IV, laminin and numerous cytokine and paracrine signals 19. They are known to coevolve with the tumour, developing a characteristic phenotype called myofibroblastic (or active phenotype), due to the cytoplasmic ultrastructural accumulation of contractile proteins such as α-smooth muscle actin (SMA).
In addition to the accumulation of specific contractile proteins, CAF produce MMP which directly contributes to remoulding of the extracellular matrix 20.
In HNSCC, CAF show the myofibroblastic phenotype associated with expression of integrin α6, which is critical in maintenance of cell-to-cell adhesion and surface signalling.
It has been demonstrated that upregulation of both α-SMA and integrin α6 is correlated with poor prognosis in oral cancer, as α-SMA and integrin α6 bind laminins and interact with CDKN1A, altering cell cycle progression 21. Moreover, CAF secrete and express a variety of factors which promote cell motility by upregulating a number of cytokines, for instance paracrine motility factor, HGF, CXCL2, and TGF-β 22. HGF in turn promotes invasion and angiogenesis 23. The CXCL2 secreted by CAF binds CXXR4, and this interaction plays a role in the upregulation of MMP9, EMT and HIF-1α 24.
-
Immune response and immune surveillance.
Progression and metastatic dissemination in HNSCC can be objectively linked to the falling and malfunction of host antineoplastic immunity: T lymphocytes and antigen presenting machinery cells (APM) play a main role in this process 25.
APM is made up by dendritic cells, Langerhans cells, myeloid dendritic cells and plasmacytoid dendritic cells. All these elements interact with the neoplastic cells in a complex process which can be affected by down-regulation or loss of the HLA class I molecules expression: low survival rates and presence of regional lymph nodes metastasis in primary laryngeal carcinomas and oropharyngeal squamous cell carcinomas are associated to this pathway 26. Moreover, HNSCC can influence and modulate the circulating myeloid and plasmacytoid dendritic cells, so that the number of these cells is significantly lower in the HNSCC patients; this phenomenon seems to be reversible, and, for instance the number of circulating cells increases after removal of tumour.
LC are a particular type of dendritic cells representing 2-8% of the intraepidermal cells in upper respiratory and digestive mucosa: strong infiltration of LC, distributed both inside and outside the neoplastic sheet, is associated with a low incidence in cervical lymph node metastasis and, consequently, with better prognosis 27.
Plasmacytoid dendritic cells (PDC) are APM able to produce large amounts of interferons IFN-α in response to virus, having a reduced antigen capture potential compared to other APM. It has been demonstrated that HNSCC cells can negatively influence PDC function with a reduction in the secretion of interferon (IFN), through tumour-induced down regulation of toll-like receptor (TLR) as shown by Hartmann et al. 28.
PGE2 and TGF-β are two immunosuppressive factors found in tumour tissue. A recent study showed that TGF-β synergizsed with PGE2 inhibited IFN-α and tumour necrosis factor (TNF) production by TLR7- and TLR9-stimulated PDCs 29.
Finally, tumour associated macrophages (TAM) can contribute to the aggressiveness of HNSCC through their direct participation in angiogenesis and tumour progression.
There is a significant association between the number of TAM and microinvasion, microvessel density and positivity for angiogenic factors such as vascular endothelial growth factor (VEGF) 30; a direct correlation has been also observed between macrophage infiltration and proliferation index evaluated with the analysis of cell cycle (cyclin E a p53) and proliferation (Ki-67) markers, suggesting that TAM are linked to tumour progression 31. In laryngeal and hypopharyngeal carcinomas, the presence and concentration of macrophages is higher in areas of fibrin deposition: this may indicate that they participate in stabilising and remodelling the extracellular matrix, facilitating tumour matrix generation and angiogenesis 32. A significant, direct correlation between TAM and lymph node involvement has been demonstrated, with a higher concentration of TAM being linked not only to lymph node metastases but also to ENE 33.
-
T cells.
The response of the immune system against neoplastic cells is compromised in the presence of functional defects of T cells, both circulating and tumour infiltrating lymphocytes (TILS) 34.
A number of defects have been observed in T cells isolated from the tumour, including absence or low expression of CD3 zeta chain, decreased proliferation in response to mitogens, inability to kill tumour cell targets and imbalance in the cytokine profile with absence of IL2, which are all evidence of predominant apoptotic features 34. Moreover, HNSCC cells can autonomously produce TGF-β1 and subsequently generate a reduction in the expression of NK cell receptor NKG2D and CD16, inhibiting the biological function of natural killer (NK) cells.
Mature T lymphocytes (T lymphocytes leaving the thymus and reaching lymph nodes and spleen), are activated when contacted by antigen presenting cells (APC), through the sharing of two specific signals:
a link between major histocompatibility complex (MHC) on APC and T-cell receptors;
expression of co-stimulatory molecules (CD25 and FOX-P3).
When activated, T cells differentiate into effector cells (CD4 helper and CD8 cytotoxic), and into memory cells, which are able to induce a rapid immune response in case of second contact with a previously known antigen.
CD4 T cells (Treg) are important in self-tolerance, which means induction of tolerance to self antigens. The main immunophenotypic markers used for the identification of T cells are: CD45RO (naïve and memory T cells), CD69 (activated T cells), CD4 (helper T cells), CD8 (cytotoxic T cells), CD25 and FOXP3 (Tregs).
T lymphocytes in patients with HNSCC have shown a number of functional deficits at a loco-regional level (peritumoral infiltration) and on a systemic level, as a result of mechanisms which lead HNSCC to evade and suppress the cytotoxic T lymphocyte anti-tumoural response.
Circulating and tumour associated T lymphocytes can show increased apoptosis through different pathways, such as increased expression of FasL on the cell surface of HNSCC, which promotes apoptosis in peritumoral T lymphocytes through a Fas/FasL interaction 35. Other pathways are also implicated in T cell apoptosis via TRAI and TNFα as demonstrated on Jurkat cell lines 36.
Suppression of cytotoxic T lymphocytes response can develop through the increasing expression of PD-1 (programmed death 1 receptor) on T lymphocytes and its interaction with the corresponding ligand PD-L1 (expressed by neoplastic cells). This binding shows other adverse effects on antineoplastic immunity, for instance decreased secretion of cytotoxic mediators and increased apoptosis of peritumoral and intratumoural T CD8 lymphocytes 37.
This is the basis of modern therapeutic approaches using molecules that are able to block the interaction PD-1/PD-L1, but not yet validated for clinical purposes in head and neck tumours.
The immunophenotypic characterisation of TILS in HNSCC has a long story; in the past, it was mainly intended as a tool to establish the conditions for experimental therapies with modifiers of biological response 38; to date, some groups of T cell populations identified by immunohistochemistry (for instance CD4-CD69, CD4-CD25, CD4-FOXP3) seem to have prognostic significance; however, the role of FOXP3 positive T lymphocytes has not been conclusively defined: at present, this immunophenotypic class of lymphocytes seem to be associated with better OS and disease-free survival in some studies 39.
3.3. Interaction between angiogenesis, inflammation and hypoxia in tumour microenvironment
Intratumoural hypoxia, considered as < 2.5 mm Hg O2, is a peculiar characteristic of HNSCC, which contributes to its aggressiveness through resistance to both chemotherapy and radiotherapy 40. HIF is a transcription factor that interacts with more than 100 genes, and may be considered the most important and immediate adaptative response to hypoxia, being directly associated with poor prognosis. It interacts with CA9 and influences the pH of TME with subsequent alterations in the uptake of chemotherapeutic drugs, resulting in resistance to treatment.
Microvessel density, one of the findings in tumour angiogenesis, is known for a long time to be associated with poor prognosis in a number of head and neck tumours 41, through implication of several factors: for instance, lisyl oxidase catalyses the crosslinking of collagen and elastin, and its overexpression increases microvessel density. Moreover, a number of other factors derived from TME (VEGF, NF-KB, HIF-1α) participate in the process. VEGF binds to its receptor on tumour cells inducing expression of bcl2 with an anti-apoptotic effect, and of CXCL1 and CXCL8 in a paracrine fashion: as a consequence, they promote survival and proliferation of endothelial cells 42.
Chronic inflammation contributes to maintenance and progression of disease through ROS and cyclooxygenase (COX): COX enzymes catalyse the production of prostaglandins, in particular PGE2, which promotes angiogenesis and invasion, and inhibits apoptosis in cancer cells.
3.4. miRNA expression profiles
A further attempt to identify prognostic groups of patients has been recently reported in a study on miRNA expression profiles obtained from metastatic lymph nodes of non-HPV-correlated HNSCC 43. Huang et al. identified three different subtypes of metastatic HNSCC lymph nodes using miRNA expression profiles.
Gene set enrichment analysis (GSEA) was used to understand the distinct biological pathways characterising each subtype, defined as follows:
Immune subtype (Group 1): predominant signalling pathways were related to T cell receptor, chemokine receptor and pathways participating in allograft rejection. Consistent with its enrichment of immunological pathways, a higher estimated proportion of CD4+ B cells and CD8+ T cells.
Invasive subtype (Group 2): this subtype was associated with significantly worse prognosis, and its gene expression signature was of prognostic value across multiple cancer types.
Main biological pathways in this group were associated with the epithelial-mesenchymal transition, apical junction, TGF-beta signalling, angiogenesis, hypoxia, extracellular matrix receptor interaction, regulation of the actin cytoskeleton and focal adhesion, i.e. most gene sets involved in the interaction between cell membrane and extracellular matrix.
Metabolic/ proliferative subtype (Group 3): predominant signalling pathways were related to MYC targets, basal transcription factors and alterations in mismatch repair genes.
This prognostic classification, coming from translational research, can be applied to many other metastatic solid cancers: the main problem remains the multifaced pattern of tumour heterogeneity.
Conclusions
Our aim was to focus on clinical approaches with potential impact on the pathways involved in metastatic diffusion of head and neck cancers. To date, no prognostic or predictive tools (either molecular or immunohistochemical) have been definitively validated, although checkpoint inhibitors are in an advanced phase of study and are showing promising results.
APPENDIX: TNM Classification 8th Edition, 2017
In the diagnosis of head and neck tumours, the TNM staging remains the most reliable and reproducible prognostic tool. While the focus of this paper was metastatic dissemination, a brief comment on the recently published TNM classification 44 seems appropriate, especially in consideration that the changes made to staging of head and neck tumours are relevant. The main modifications can be summarised in the following points:
Extranodal spread of lymph node metastases (ENE): this is a well-known prognostic tool, used for many years in the postoperative therapeutic approach by oncologists and radiotherapists, which is now introduced in pTNM classification for all subsites. Moreover, the minimum number of sampled and examined lymph nodes is established at 10 for selective neck dissection and 15 for radical neck dissection.
-
p16 and EBV phenotype: many reports have indicated that immunohistochemically p16-positive oropharyngeal squamous cell carcinomas show epidemiological characters and clinical courses different from p16-negative lesions, and by consequence need different treatment approaches. The new TNM applies this assumption, especially in terms of lymph node staging (for instance, extra-nodal diffusion is not foreseen in p16-positive tumours).
EBV status (as well as p16 positivity) has to be determined in staging of lymph node metastases from unknown primary tumours in order to indicate a possible nasopharyngeal histogenesis. EBV can be demonstrated by DNA or RNA detection (the latter is more reliable in our experience).
Depth of invasion (more or less 10 mm) has been added among the characteristics of the tumour in the TNM staging of oral carcinoma.
Modifications have been implemented for staging of thyroid carcinoma, which now take into consideration the age of the patients affected by papillary and follicular carcinomas (under and older 55 years), and recommends different staging groups for medullary and anaplastic carcinoma.
In the TNM 8th edition 44, M staging is the same compared with the previous one.
M staging refers to M0 (no distant metastasis) and M1 (distant metastasis) classifications. MX classification is considered inappropriate.
pM classification stands for pM1 class (distant metastasis confirmed by microscopical examination). PM0 and pMX are not validated classes.
M1 and pM1 classes may be specified as reported in Table 3.I.
Table 3.I.
Metastatic localisation by site.
| Pulmonary | PUL (C34) | Bone marrow | MAR (C42.1) |
| OSS | (C40, 41) | Pleura | PLE (C38.4) |
| Hepatic | HEP (C22) | Peritoneum | PER (C48.1,2) |
| Brain | BRA (C71) | Adrenal | ADR (C74) |
| Lymph node | LYM (C77) | Skin | SKI (C44) |
| Other | OTH | ||
The prefix “a” indicates that the classification has been determined by autopsy.
In most HNC sites (oral cavity, oropharynx p-16 negative, hypopharynx, larynx, nasal cavity and paranasal sinuses, salivary glands) any T, any N and M1 classification leads to stage IVC.
In oropharyngeal p16-positive and nasopharyngeal cancers, any T, any N and M1 classification leads, respectively, to stage IV and IVB.
In lung and breast cancer, supraclavicular lymph nodes are considered loco-regional nodes. In lung cancer, the presence of metastatic supraclavicular is considered as N3 and leads to stage IIIB (T1a-c, T2a,b - N3 - M0) or IIIC (T3, T4 - N3 - M0).
In breast cancer, the presence of one or more ipsilateral supraclavicular lymph nodes yields a N3c classification for both cTNM and pTNM. Any T, N3, M0 status, is considered stage IIIC.
When head and neck metastatic diffusions are present from breast and renal cancer, the disease is classified as stage IV, any T and any N.
According to the TNM 8th edition, head and neck single or multiple metastasis from lung cancer are class M1c (multiple extrathoracic metastasis in single or multiple organs) and lead to a consequent staging IVB, any T and any N.
4. Diagnostic imaging of metastatic disease in head and neck malignancies
Introduction
A distinctive feature of HNC is the large variety of malignancies that arise from its various sites. This characteristic reflects the complexity of the tissues composing the head and neck region. In addition, malignancies sharing the same histotype, such as SCC, and even the same size, may result in a different clinical course. Hence, different treatment modalities may be required, which is often dictated by the specific site from where the neoplasm originates. Two main factors account for the latter aspect: sites and subsites of the head and neck are characterised by very different, complex functions 1; some sites and subsites have very close spatial relationships with vital structures, as the carotid artery.
Therefore, a key aspect in the head and neck oncology is the great variety of malignant tumours, their variable clinical manifestation and remarkably variable prognosis. All these factors are joined with the specific histopathological type and grading, site of origin of the neoplasm and local, regional and distant spread (T, N and M in the TNM classification).
In head and neck oncology, tumours arising from the mucosa covering the upper aerodigestive tract are the most frequent. Among these, SCC accounts for the majority.
In the last decades, in addition to categorisation into low, intermediate and high grade, it has become possible to separate (and grade) the same histological type on the basis of genomic and molecular receptor profiles.
This latter aspect has given rise to promising targeted therapies. It also supports specific research in circulating tumour cells, circulating tumour DNA and tumour-educated platelets with the acquisition of liquid biopsies: a minimally-invasive method for detecting and monitoring disease.
Moreover, recent studies have demonstrated that an increasing number of SCC arising near the lymphatic tissue of the oropharynx are related to viral infection by subtypes of HPV. Similarly, undifferentiated carcinomas of the nasopharynx have been linked to Epstein-Barr Virus infection. Both neoplasms show very high tumour sensitivity to radiation therapy.
Furthermore, HPV-positive SCC, despite characteristic and early lymph node metastasis, show a significantly better outcome and survival compared to HPV-negative SCC of the oropharynx. Based on individual “tumour ID cards” – i.e. histopathology, grading, site of origin, local extension – it is possible to stratify the risk of regional and distant metastasis, classifying patients into high and low risk classes.
A more precise stratification of risk is still hampered by the insufficient knowledge of the interaction of many parameters. In fact, analysis of the current literature reveals that most series are widely heterogeneous in terms of histology, grading, site of origin, extension, stage, type of treatment, timing of diagnosis of distant metastasis (at presentation vs. anytime in the course of the disease or at autopsy), locoregional control, staging techniques and duration of follow-up.
Despite this limitation, there is a general agreement that parameters of a specific “tumour ID card” should predict a greater or lesser probability of local recurrence/progression, regional and distant spread.
As a consequence, the weight of estimated risk needs to be utilised in different diagnostic algorithms at staging and follow-up.
Within this specific framework, histotype-label – written in the “tumour ID card” – should be carefully pondered. For example, among epithelial malignancies, basaloid SCC (a high grade variant of SCC) is expected to be more locally aggressive and to convey more nodal and distant metastasis than low grade SCC variants (e.g. verrucous SCC). Similarly, among glandular malignancies, high-grade tumours (e.g. high-grade mucoepidermoid carcinoma, salivary duct carcinoma) have a rate of lymph node metastasis at presentation that is greater than low grade-tumours (e.g. low-grade mucoepidermoid carcinoma, acinic cell carcinoma).
Furthermore, a histotype-label should highlight the singular behaviour that characterizes adenoid cystic carcinoma (ACC). ACC is expected to have a slow but generally relentless growth rate with overall treatment failure, loco-regional recurrence, and distant metastatic rates of 62%, 51% and 38%, respectively. Disease-specific survival is reported to be 89% at 5 years and 40% at 15 years. Metastases are rare at presentation, but occur in over 50% of patients over the course of the disease 2.
Concerning the site of origin label in the “tumour ID card”, SCCs originating from sites with a rich and dense lymphatic network will more probably exhibit nodal metastases (e.g. oro-hypopharynx vs. glottis).
How important is the status of neck nodes for occurrence of distant metastasis? Whereas in the past cancer research focused on the concept that cervical lymph nodes act as a filter to trap cancer cells trying to escape the confines of the head and neck, in recent years the relevance of the microenvironment has been increasingly recognised, and attention is now focused on stroma and patient-related factors as well as tumour-specific factors.
Nevertheless, in HNSCC, metastasis nearly always occurs first in neck lymph nodes before the development of distant metastasis. From an anatomic standpoint, the vascular and lymphatic systems are intimately associated with each other in both the primary tumour and regional lymph nodes. Ample opportunities for tumour cells to pass back and forth between the two systems exist 3.
Finally, the intrinsic tumour cell and extrinsic host biology that leads to circulating tumour cell engraftment in end-organ tissues to become a distant micrometastasis, and eventually a clinically detectable distant metastasis, is poorly understood.
It is clear that the process of metastasis is complex. The “selection” of a few of many subclones with varying invasive and metastatic properties is considered one of the major processes in the development of distant metastasis 3,4.
On the basis of clinical and epidemiological evidence, expert consensus and systematic review of the literature, scientific organizations, such as the NCCN, the Italian Association of Medical Oncology (AIOM) and the Italian Association of Head and Neck Oncology (AIOCC), work to develop a comprehensive set of guidelines addressing diagnosis, treatment and supportive care to guide the decision-making in management of head and neck cancer.
A sample of guidelines focusing on the role of imaging techniques both in the initial work-up and in the post-treatment follow-up of head and neck malignancies are summarized and compared in Tables 4.I, 4.II.
Table 4.I.
National Comprehensive Cancer Network (NCCN) guidelines on staging of head and neck tumours, compared with AIOCC (Italian Association of Head and Neck Oncology) and AIOM (Italian Association of Medical Oncology).
| Staging by imaging | NCCN guidelines version 1.2019 | AIOCC guidelines 2012 | AIOM guidelines 2018 |
|---|---|---|---|
| SCC oral cavity | As clinically indicated:
|
|
Local staging with:
|
| SCC oropharynx |
|
|
Local staging with:
|
| SCC hypopharynx |
|
|
Local staging with:
|
| Cancer of nasopharynx |
|
|
Local staging with:
|
| SCC glottic larynx |
|
|
Local staging with:
|
| SCC supraglottic larynx |
|
||
| Ethmoid sinus tumors |
|
|
|
| Maxillary sinus tumors |
|
||
| Salivary gland tumors |
|
|
|
| Mucosal melanoma |
|
1: Chest CT is recommended for advanced nodal disease to screen for distant metastasis and for selecting patients who smoke, to screen for lung cancer.
Table 4.II.
National Comprehensive Cancer Network (NCCN) guidelines on follow-up of head and neck tumors, compared with AIOCC (Italian Association of Head and Neck Oncology) and AIOM (Italian Association of Medical Oncology).
| Follow-up by imaging | NCCN guidelines version 1.2019 | AIOCC guidelines 2012 | AIOM guidelines 2018 |
|---|---|---|---|
| SCC oral cavity |
|
|
|
| SCC oropharynx |
|
After 2/3 months of conclusion of CHT/RT:
|
|
| SCC hypopharynx | Each 6-12 months:
|
|
|
| Cancer of nasopharynx | Between II-III month (post therapy), evaluation of response with:
|
After 3 months to CHT/RT evaluation of response with:
|
|
| SCC glottic and supraglottic larynx | Each 3 months for the first 2 years to treatment:
|
|
|
|
Sinonasal
tumours |
After 2 or 3 months of conclusion of therapy:
|
||
| Salivary gland tumours | After 2 or 3 months of conclusion of therapy:
|
Ultrasonography (US), computed tomography (CT), magnetic resonance (MRI), positron emission tomography/CT (PET/CT) and radionuclide imaging are the various modalities available for imaging and staging of head and neck malignancies. Emerging techniques are represented by whole body MRI and PET/MRI.
In different cancers and in specific situations, certain imaging modalities are superior to others. Each single modality has its own advantages and limitations 1.
Imaging in HNC has significantly progressed in the last decades.
As a core member of a multidisciplinary team, the radiologist has a key role in identifying relevant findings that map the extent of the neoplasm, help with surveillance and highlight pertinent comorbidities.
The areas that the radiological assessment should focus on are:
local extent of the primary tumour;
spread to locoregional cervical lymph nodes;
detection of metastatic disease and synchronous/metachronous primary tumours 5.
4.1. Imaging modalities
Computer Tomography
CT is the mainstay for imaging most primary neoplasms in the head and neck, particularly those arising from infra-hyoid neck structures. It is fast, widely available and well established. It provides high spatial resolution, but enables a relatively limited soft tissue contrast resolution compared to MR. While this limitation may result in difficult discrimination between vascularised scar tissue from a recurrent tumour, it is adequate to assess the presence of metastasis in the chest and abdomen.
Modern multidetector CT technology allows fast acquisition of images without relevant movement artefacts. This is particularly important after surgery and/or radiation-therapy as patients with HNC may have difficulties with breathing and swallowing secretions, particularly when lying flat 5.
A plain CT may be sufficient (clavicles to diaphragm) during follow-up of neoplasms with an increased risk of lung metastasis or with risk factors for the development of synchronous/metachronous non-small cell lung cancer. Conversely, the administration of contrast agent is recommended if the abdomen or the mediastinum is examined. CT may also be used to guide the biopsy of suspected chest, bone or abdominal metastases. This is particularly useful to differentiate metastatic disease from synchronous/metachronous primary tumours.
Although CT is more sensitive than conventional radiology in detection of early metastases to bone, it is far less sensitive than nuclear medicine techniques.
CT guided needle-biopsies are also possible to obtain histological and genetic/molecular characterisation of a suspected lesion that is not accessible by US guided biopsy, thus allowing for targeted therapies.
Magnetic resonance
The intensity of the signal in MRI imaging reflects specific tissue characteristics. It is largely dependent on proton density (free and bound water within tissues) and by the paramagnetic properties of macromolecules and substances included in the volume of study.
During the MRI examination, a combination of static and specific transient magnetic gradients (sequences) discriminate pathological changes from normal surrounding tissues 5. When used to study the primary tumour, MRI has been shown to be superior to CT in obtaining excellent soft tissue contrast and to provide images of good quality even in the presence of dental hardware 6.
Conventional MRI sequences are superior to CT for a variety of additional findings that may influence the treatment choice such as laryngeal cartilage invasion, invasion of the skull base, perineural spread, detection of retropharyngeal lymph nodes in nasopharyngeal carcinoma, extranodal spread in metastatic neck nodes, vascular and lymphatic invasion and detection of occult pathologies 5,6. The introduction of more refined MRI criteria based on the analysis of signal intensity and enhancement patterns after injection of gadolinium chelates has had a major impact on the assessment of deep tumour spread. It has to be underlined that during examination of a head and neck primary tumour, MRI may detect asymptomatic brain, dural, calvarial, skull base or bone metastasis included in the volume of study. Certainly, one limitation of MRI is that scan times (minutes) are much longer than CT (seconds), and can vary from 2-5 minutes for each sequence, during which the patient must keep as still as possible 5.
Whole body MRI (WB-MRI)
The recent introduction of multi-channel receiver MRI has made WB-MRI examination clinically feasible, with substantially reduced examination times.
Commonly used WB-MRI sequences such as T2-weighted, and short time inversion-recovery (STIR) imaging allow for evaluation of anatomic and pathologic changes because of their excellent soft tissue contrast.
Moreover, a newer WB-MRI technique is WB diffusion-weighted MRI (DW-MRI). A potential advantage of WB-DW-MRI over standard anatomical WB-MRI sequences is a higher lesion-to-background contrast, which eliminates the need for gadolinium-enhanced sequences.
The advantages of WB-MRI over FDG-PET/CT are its lower costs and absence of ionizing radiation, since WB-FDG-PET/CT is accompanied by a substantial radiation dose and (secondary) cancer risk 7.
Technical improvements like diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) and experience in WB-MRI had increased the accuracy of this technique.
Ng et al. 8, comparing WB-MRI and FDG-PET-CT, found similar sensitivity, specificity, positive predictive value and negative predictive value, but concluded that combined interpretation of WB-MRI and FDG-PET/CT showed slightly (non-significant) benefit over either technique alone.
Moreover, in assessing for the presence of lung metastasis, MRI is significantly less sensitive than CT.
Positron Emission Tomography (PET) combined with CT (PET/CT)
PET/CT whole-body imaging uses various radioactive-labelled tracers to fuse the anatomical CT map with a “functional map” of the disease process. This is conducted on a single gantry at a single appointment. The most common tracer is FDG, which is preferentially transported and trapped into hypermetabolic neoplastic or inflamed tissues. Other tracers are currently available. They may track tumour cell proliferation such as the 18fluorothymidine (FLT), or tumour growth measured by protein synthesis with 18fluoroethyltyrosine (FET). Overall, image acquisition takes 30-45 minutes.
Modern scanner design accurately co-registers metabolic tissue activity with its precise CT anatomical location 5.
PET/CT has established itself as a robust, rapid and reliable technique providing reproducible data even in patients with limited cooperation.
The combination of PET and CT is highly synergistic, resulting in increased sensitivity and specificity for tumour staging as well as for effective patient management in routine practice.
The metabolic information from PET radiotracers can be complemented by the full diagnostic capability of contrast-enhanced CT during the same session, although this may not be done in a majority of institutions 6.
PET combined with CT is also valuable in assessment of suspected recurrences of HNC when there are extensive, confounding post-treatment changes on conventional imaging modalities 5.
The most significant limitations of FDG PET/CT are its threshold-size limit, below which lesions are undetected (e.g. early stage DM may be missed in the initial cancer work-up) and lack of specificity for malignancies, potentially resulting in false positives.
PET/MRI
Given that PET and MRI can both detect DM, a combination of the two techniques PET/MRI is expected to further improve detection of DM. Actually, the images obtained by PET-MRI show higher detailed resolution and greater contrast resolution compared to PET/CT. However, combining the two imaging technologies without degrading their original optimum performance is challenging 7.
All currently available first-generation PET/MRI systems use standard clinical 3-T MRI scanners 6.
There is evidence to suggest that FDG PET/MRI is superior than FDG PET/CT for staging in nasopharyngeal cancer and in advanced breast cancer, detection of local cervical cancer invasion, detection of local recurrence in prostate cancer, detection of liver metastases and staging in colorectal cancer. FDG PET/MRI tends to be inferior compared to FDG PET/CT for the detection of lung metastases 9.
Although the integration of PET and MRI remains technically complex, this new hybrid imaging modality holds promise because it can combine morphological, functional and molecular information at the same time 6.
Ultrasonography (US)
US, alongside fine needle aspiration cytology or core biopsy, allows rapid imaging assessment for a neck lump or suspected metastatic disease in the neck. US may also guide core biopsy of suspected metastases in any body district adequately explorable (i.e. abdomen, chest wall, superficial soft tissues, etc.). Though the success of the procedure can be operator dependent, US has no detrimental patient effects, except potential complications due to iatrogenic lesions of surrounding structures during fine needle aspiration cytology (FNAC)/core biopsy.
4.2. Head and neck squamous cell carcinoma
The burden of loco-regional and distant metastases
In head and neck SCC, the prevalence of clinically identified DM at presentation varies noticeably in the literature. Both De Bree et al 7 and the SEER registry report a range between 4% to 24%. Higher rates have been reported after extensive diagnostic work-up and in high risk patients with advanced disease. A more ample range - from 3% to 50% has been described by other authors 4. This greater amplitude may be explained by the fact that the series included patients with widely different characteristics regarding the primary tumour site, stage of disease, type of treatment, timing of diagnosis of distant metastasis (at initial presentation, anytime in the course of the disease, or at autopsy), locoregional control, staging techniques and duration of follow-up.
The relationship between regional metastatic burden and the presence of DM, at presentation or during the course of the disease, has been largely explored. There is a general agreement about the significant relationship between lymph node status and incidence of metastasis.
The risk for distant metastasis has been reported to increase in case of:
3 or more cervical nodes (N2b or c);
bilateral metastatic nodes (N2c);
node(s) ≥ 6 cm (N3);
node(s) low in the neck (low jugular lymph nodes);
locoregional tumoral recurrence;
second primary tumour;
≥ 1 capsule rupture and/or lymphatic and perineural emboli on histology;
according to histologic type: basaloid squamous cell carcinoma (BSCC) is associated with elevated rates of metastases, which is the prime cause of mortality in this histologic type, implicated in 45-65% of deaths 10,11.
Takes et al. 4 found that the most frequently identified clinical risk factors for distant metastasis in HNSCC appeared to be locoregional control and nodal status (N-classification). Other important factors included tumour site and size (T-classification), histological grade of differentiation and age at diagnosis. In their review, Takes et al. divided risk factors in clinical, radiological, histopathological and molecular and concluded that, based on published series, the most important predictive factors for distant metastasis appeared to be:
primary tumour site (hypopharynx in particular);
advanced T- and N-classification;
locoregional control;
histologic grade (poor differentiation of primary tumour);
age of diagnosis (in some series age < 40-45 years correlated with higher risk of distant metastasis).
Moreover, metastasis of HNSCC to regional lymph nodes can be thought of as an indicator, rather than purely an initiator, of distant metastatic disease. As a consequence, the 50% decrease in survival documented in N positive versus N0 HNSCC may be seen as an indicator of both a more aggressive primary disease and net systemic susceptibility of the host to metastasis.
In addition, regional and DM represent similar biologic processes and may be concurrent or even independent events in progression of HNSCC.
Tumour metastatic potential may differ within HNSCC themselves, with some having inherent metastatic potential and others acquiring the capacity during progression.
Patients with HPV-associated oropharyngeal SCC generally tend to develop early and aggressive metastases to cervical regional lymph nodes, but develop DM less frequently compared to HPV-negative HNSCC 3,12.
Though a large fraction of patients with squamous cell carcinoma of the head and neck present with advanced local and regional disease, improvements in multimodal treatment have permitted superior locoregional control. This achievement is not sufficient for long-term disease-free survival, however, as long-term survivors are at risk of developing DM 13.
In addition, there is the possibility that distant micrometastases, clinically and radiologically undetectable, but present at diagnosis and not addressed by aggressive treatment of locoregional disease, act as the source of distant treatment failure.
Finally, factors such as occurrence of DM combined with presence of certain patient-related features, such as smoking and alcohol-related illness, may explain why OS has not ameliorated in line with improvements in locoregional control of HNSCC 4.
After treatment completion, distant metastasis during the course of the disease ranges between 10% and 40% depending on the population, cancer stage, duration of follow-up and local and regional control 4. Generally, if a distant metastasis is not present at initial presentation and treatment, up to 95% of metastases are diagnosed within 2 years from primary diagnosis. Median time to onset of the first location is 10 months. In about 50% of cases, metastases are associated with persistent locoregional HNSCC.
Up to 80-85% of metastases from HNSCC are observed in the lungs (Fig. 4.1) and bone metastases account for 15-39% (Fig. 4.2), while the liver is a target in 10-30% of cases (Fig. 4.3).
Figure 4.1.

CT demonstration of multiple cavitated (straight arrows) and solid (curved arrows) pulmonary metastases from a recurrent squamous cell carcinoma of the tongue at 8 weeks after completion of chemotherapy.
Figure 4.2.
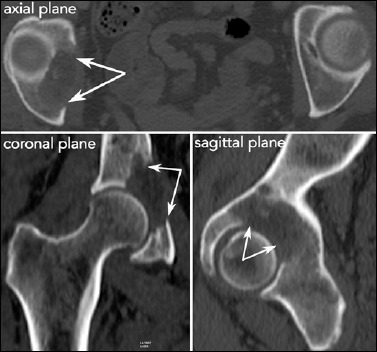
Bone metastasis replacing a large portion of the right acetabulum (arrows) imaged by multidetector CT in the axial plane and precisely mapped through multiplanar reconstructions obtained in the coronal and sagittal planes. The patient underwent RT.
Figure 4.3.
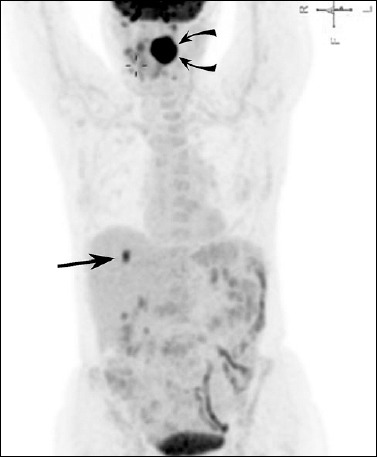
FDG-PET shows a metastasis within the right lobe of the liver (straight arrow) from a HPV-positive squamous cell carcinoma of the left palatine tonsil (curved arrows).
The incidence of intracranial metastases is low (0.4%), but if DM are already present in other body sites, the rate increases to 2-8% 14.
Metastatic disease to intracranial dura, calvarium and skull base is relatively uncommon, but presents unique diagnostic and management challenges 15. Modern imaging techniques have improved detection of non-symptomatic intracranial tumour deposits, a factor that accounts for the (relatively) increased incidence.
Some issues regarding “intensity” of both clinical and imaging-based follow-up of HNSCC patients are still open. Which risk classes will actually benefit from follow-up screening for distant metastasis (Tab. 4.III)?
Table 4.III.
High risk factors for distant metastases in HNSCC (from de Bree et al., 2018 7, mod.).
| Three or more cervical lymph node metastases |
| Extra-nodal spread |
| Low jugular lymph node metastases |
| Lymph node metastases greater than 6 cm |
| Bilateral cervical node metastases |
| Second primary head and neck tumour(s) |
| Regional recurrence |
| Primary tumour of the pharynx |
| T-stage (T3-T4) |
Allen et al. 3 noticed that given the extreme complexity of metastatic processes, at present it is difficult to identify reliable biomarkers for prediction of distant metastasis. Nevertheless, they forecasted a future role for predictors. A second issue regards which imaging technique should be used to screen patients. Should the chest be the only site to be screened in non-symptomatic patients?
A third issue in designing imaging-based follow-up in HNSCC patients takes into account the greater risk in this group to develop a synchronous or metachronous second cancer (lung and/or oesophagus) 16. Hence, the first 2/3 years of follow-up after primary treatment show a prevailing risk of locoregional recurrence and metastasis, whereas in the subsequent years the risk for a metachronous cancer predominates 16,17. Risk of a second cancer is higher in patients who continue active smoking and/or alcohol abuse after primary treatment 11,16.
Pre-post treatment work-up and head and neck squamous cell carcinoma staging: a “change of landscape”
In general, distant metastatic disease from HNC is considered incurable, and patients have a variable prognosis depending on tumour histology, performance status and comorbidities. Individuals with metastatic HNSCC often have a poor life expectancy, measured in months. Indeed, around 88% of patients with HNSCC distant metastasis die within 12 months 18.
Therefore, pre-treatment screening for DM is currently performed mainly to avoid unnecessary extensive locoregional treatments, preventing both inappropriate and disproportionate impact on the quality of life and inconsequential cost-effectiveness. Recently, a treatment concept in OM, which proved to be successful in other neoplasms, has been re-introduced in HNSCC.
When locoregional disease is controlled, or resected, and metastases at distant sites (a very limited number of isolated well-defined metastatic lesions) are surgically treated/excised or ablated with stereotactic body radiotherapy, prolonged disease-free interval, and possible cure, may be achieved. In order to be successful, this strategy requires that the diagnostic tool used should be characterized by the least rate of false negatives.
Ruling out DM at presentation. In the pre “PET-era”, the incidence of DM at staging in high risk HNSCC, scheduled for major surgery, was reported to be 17% after extensive diagnostic work-up: chest CT, bone scintigraphy, liver US and/or abdomen CT 10,19. With the introduction of PET/CT, the DM rate detected at presentation increases to 24%. Though this figure can be considered a significant improvement, incidences of DM up to 57% have been reported at autopsy 18. Low sensitivity of PET/CT for small sized lesions (diameters lower than 8mm) is its major limitation.
As a result, the diagnostic yield of PET/CT is, usually, lower in ruling out DM in early-stage disease, when distant deposit may be very small, and therefore undetected. On the other hand, PET/CT has a greater role in pre-treatment evaluation of advanced-stage (III/IV) and recurrent HNSCC 18,20.
In their review in 2018, de Bree et al. 7 concluded that since the reported prevalence of clinically-identified DM in HNSCC patients is too low (from 4% to 24% at presentation) to warrant routine screening of all patients, only those with high risk factors (factors reported in Table 4.III with emerging, increasing role of molecular characterization etc.) should be selected for screening for DM.
Ruling out DM during follow-up. At present, there are no data in favour of any specific post-therapeutic surveillance strategy. Some authors suggest that post-treatment screening for DM could be limited to the first 2 years, when most distant metastasis are detected.
De Bree et al. suggest that cost-effective follow-up screening should enrol only high-risk patients with good performance status, e.g., generally patients with HPV-related HNSCC 7.
In a previous review (2013), Digonnet et al. 21 concluded that classes of patients who would benefit from a post-treatment imaging study (CT or MRI) at follow-up should include:
advanced stage HNSCC at sites not easily accessible to physical or fibre optic examination;
lesions requiring assessment of treatment response.
To be effective, this strategy needs a baseline study performed within 3-6 months after completion of primary therapy. Additional imaging examinations should be performed based on clinical signs and symptoms. They also concluded that PET/CT provides high accuracy in detecting residual disease and should be performed at 12 weeks after treatment in patients who have undergone definitive chemo-radiotherapy. They found that the value of additional PET/CT evaluations for detection of loco-regional and distant recurrences was debatable, since its impact on survival remained to be evaluated, and concluded that screening of distant lung lesions may be performed by annual chest CT for the first 2 years in high-risk patients 21.
Lung metastasis can sometimes be very difficult to distinguish from a synchronous/metachronous primary lung cancer on chest CT. Even well-established imaging criteria may be insufficient, since lung metastases are usually round/smoothly defined and sub-pleurally/peripheral located, multiple and situated at the ends of blood vessels, while primary bronchogenic carcinomas are usually solitary, spiculated, with irregular margins, and centrally located lesions. Further work-up is, therefore, necessary (e.g. CT guided needle-biopsy or follow-up scans) 18.
The NCCN 2019 guidelines 22 for head and neck cancers recommend acquiring:
a post treatment baseline study of the primary tumour (and the neck, if treated) within 6 months of treatment;
chest CT without/with contrast agent administration in patients with history of smoking.
Further reimaging is indicated on the basis of worrisome or equivocal signs/symptoms. Routine annual reimaging (repeat use of pre-treatment imaging modality) may be indicated in areas that are difficult to visualise.
4.3. Main histotypes of head and neck tumours other than HNSCC
Head and neck cancers other than upper aerodigestive tract SCC comprise a heterogeneous group of tumours with wide variability in prognosis; histological type and grade is a significant prognostic factor, especially in sarcomas.
Pre-therapy staging in patients with these tumours is necessary for appropriate therapeutic planning.
Post-therapy follow-up for patients with this malignancy should meet several objectives, among which, to detect recurrences, be it local, regional and/or metastatic, and to evaluate acute and chronic treatment-related side effects, guiding the rehabilitation process.
Digonnet et al., in a 2013 review 23, analysed the most frequent main histotypes of head and neck malignancies other than HNSCC and summarised the best post-therapy follow-up strategies.
In 2019, the NCCN revised follow-up recommendations for all types of HNC and advised scheduled visits at intervals of 1-3 months for the first year, 2-6 months for the second year, 4-8 months for years 3-5 and annually thereafter 22.
Nasopharyngeal undifferentiated carcinoma (NPC)
The main prognostic indicators at diagnosis are T and N stages and tumour histotype.
Currently, both head and neck MRI and whole-body FDG PET/CT are recommended for staging of patients with primary NPC according to NCCN guidelines.
CT or MR of the head and neck are usually acquired for loco-regional assessment. At present, FDG PET/CT is routinely performed in many institutions for diagnosis, initial staging, follow-up and recurrence (Fig. 4.4).
Figure 4.4.
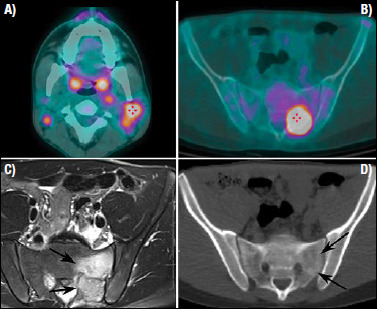
Nasopharyngeal undifferentiated carcinoma in a young patient. (A) The FDG-PET/CT shows a metabolic active adenopathy at level 2b, on the left side of the neck, and a large bone metastases (B) in the left ala of the sacrum, both showing a high metabolic activity. While the CT image obtained during the PET/CT study does not demonstrate sufficient changes of the bony architecture (D), the MRI examination clearly defines the metastasis replacing the posterior aspect of the ala of the sacrum (arrows) and the peritumoural bone oedema (C).
FDG PET/CT is also used to evaluate local residual disease and treatment response 23.
Malignant salivary gland tumours (MSGT)
MSGT are rare: the annual incidence rate is estimated to be less than 2 per 100,000. MSGT types have different growth patterns and show a wide range of biological behaviour. Five-year survival varies from 23% to 100%, mostly depending on the histological type, with a risk of recurrence ranging from 15% to 80% 23. Invasiveness is related to histopathological grade and accounts for risk of local recurrence and distant metastasis (Fig. 4.5).
Figure 4.5.
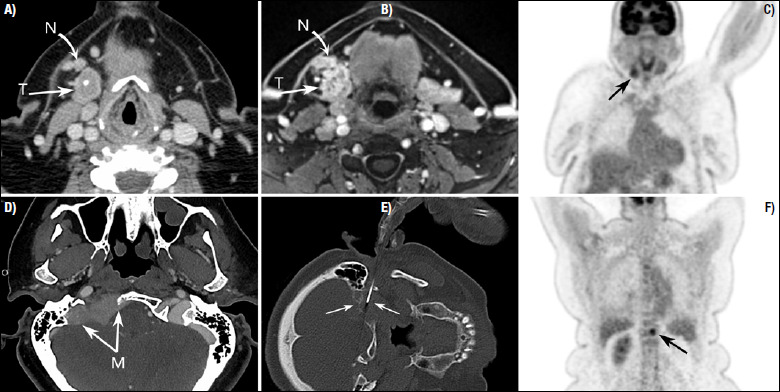
Adenosquamous carcinoma of the right submandibular gland. Contrast enhanced CT (A) and the gradient-echo fat-saturation T1 weighted MRI post gadolinium (B) show a solid lesion arising from the right submandibular gland. The intra-glandular calcification demonstrated by CT falsely suggested chronic inflammation. A destructive and enhancing bone metastasis replacing a large portion of the right basiocciput is demonstrated by CT (D). CT-guided biopsy of the destructive bone metastasis (E). The staging was completed by a whole-body FDG-PET/CT that showed the primary tumour (arrow on C) and a synchronous metastasis of the spine (arrow in F).
The most common histotypes are mucoepidermoid carcinoma (low/high grade), adenoid cystic carcinoma and acinic cell carcinoma; they usually grow slowly and may frequently be mistaken for benign lesions.
Low-grade MSGT have less than a 15% incidence of spread to regional lymph nodes, and DM are uncommon.
Parotid gland adenoid cystic carcinoma – regardless of grade – is unfrequently associated with lymph node metastasis. High-grade MSGT have the worst prognosis, and the rate of lymph node metastases is greater than 30% at the time of presentation.
The most common sites of DM are the lungs (80%), followed by bone (15%), liver and other sites (5%) 21.
Staging and ruling out DM at presentation. NCCN guidelines version 1.2019(22) suggest the use of contrast-enhanced MRI or CT (skull base to clavicle) to stage locoregional extent. Chest CT is recommended to screen for distant metastasis, eventually requiring contrast agent administration in smoking patients to screen for lung cancer (Tab. 4.I).
Ruling out DM during follow-up. NCCN guidelines (22) provide a generic follow-up strategy (common for all head and neck malignancies, regardless of histology). Chest CT is indicated for initial staging. Further imaging is indicated in the presence of worrisome or equivocal signs/symptoms, smoking history and areas inaccessible to clinical examination. AIOCC guidelines suggest performing yearly chest-CT (Tab. 4.II).
Among MSGT, adenoid cystic carcinoma, adenocarcinoma not otherwise specified and carcinoma ex-pleomorphic adenoma have the highest rates of distant metastasis 21. In particular, lung metastasis from adenoid cystic carcinoma represents a peculiar oncological condition: metastases are rare at presentation, but occur in over 50% of patients during the course of the disease (Fig. 4.6) 2. Usually, ACC metastases have slow but relentless growth. Survival may reach up to 20 years 23.
Figure 4.6.
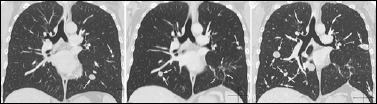
Adenoid cystic carcinoma of the parotid gland (solid component > 30%, perineural spread). Left image: at initial staging the chest CT (coronal MPR) demonstrates two metastases within the left lower lobe (arrows). Central image: follow up CT 3 years after radical parotidectomy with facial nerve sacrifice, lymphadenectomy, CHT-RT and wedge resections of lungs nodules. New nodules and the sequelae of previous surgery are present. Right image: the CT follow-up at 1 year shows the progression of size of lung metastases and appearance of new ones (arrows).
Taking into account the slow progression of ACC, an annual chest-CT can be adopted to rule out asymptomatic lung metastasis during lifetime follow-up 23. If a single metastasis is identified, chest CT can be used to plan metastasectomy. In case of multiple metastases, as no curative options are usually available, chest CT can be used to monitor treatment response to palliative chemotherapy.
In the follow-up of ACC, the use of FDG PET/CT for detecting DM remains debatable because a considerable fraction of ACC have a low metabolic rate, and thus the tumour tissue has a poor avidity for radioactive FDG.
Overall, there are no robust data supporting the use of PET/CT during follow-up of patients treated for MSGT. Its major role appears to be exclusion of metastatic disease before deciding on therapy with primary curative intent 23.
Soft tissue sarcomas of the head and neck
Head and neck soft tissue sarcomas (HNSTS) account for less than 1% of all neoplasms occurring in this region.
HNSTS display several histology arrays and a wide spectrum of clinical behaviour, ranging from relatively slow-growing lesions to aggressive and local regionally-invasive lesions with a potential for distant metastasis. HNSTS is usually associated with poor prognosis, with 5-year OS ranging from 32% to 87% 23. The absence of distant metastasis is considered among the primary factors that determine long-term survival 23.
In patients with stage I tumours, chest CT every 12 months for the first 5 years is recommended. In stages II–IV, a chest CT should be obtained more frequently: every 2-3 months for the first 2-3 years, then every 6 months for the next 2 years, and then annually.
Currently, there is no recommendation for use of PET/CT in routine follow-up of HNSTS 23.
Melanoma of the head and neck
Head and neck melanomas encompass two distinct entities: mucosal melanoma and cutaneous melanoma. Mucosal melanoma arising from the upper aerodigestive tract comprises less than 1% of all diagnosed melanoma. Its prognosis is poor (5-year OS from 17% to 38%). Melanomas arising from the sinonasal mucosa have the worst prognosis (5-years survival ranging from 0 to 5%). They are usually diagnosed in a locoregionally advanced clinical stage, with a rate of 5-48% of regional and 4-14% of distant dissemination.
Primary cutaneous melanoma of head and neck accounts for 25-30% of all melanoma, despite the head and neck surface is only 9% of the total body surface. Although 5-years overall survival of all patients with head and neck cutaneous melanoma is 88%, survival rates with advanced-stage disease remain low: stage IV melanoma patients have 5-years survival rates ranging from 8% to 18%. Survival rate in advanced stage (III-IV) is conditioned by both presence of nodal micro and macrometastases and by number of invaded lymph nodes.
No specific follow-up schedule has demonstrated its superiority.
Ruling out DM at presentation in mucosal melanoma. NCCN guidelines 22 suggest chest-CT, 18FDG-PET/CT or chest/abdominal/pelvic CT with contrast agent, and brain MR (with and without contrast) to rule out metastatic disease (Tab. 4.I).
Ruling out DM in the follow up. NCCN guidelines 22 provide generic follow-up strategy (common for all head and neck malignancies, regardless of histology) (Tab. 4.II).
As it concerns sinonasal melanoma, some Authors conclude that use of imaging during follow-up remain questionable, because of very poor prognosis 23.
Sinonasal adenocarcinoma, sinonasal neuroendocrine carcinoma (SNEC) and sinonasal undifferentiated carcinoma (SNUC)
SNEC and SNUC are considered as being part of a spectrum of neuroendocrine-type tumors, with olfactory neuroblastoma (ONB) representing the most specialized and differentiated neuroendocrine tumors and SNUC having dubious or weak neuroendocrine qualities. Most SNEC/SNUC tumors occur in the same sites as ONB (superior nasal cavity, superior turbinates, ethmoid). These tumors tend to present early metastases involving lymph nodes, brain, spine, lungs and bones.
Outcomes for SNUC have been reported to be generally poor.
Ruling out DM at presentation. For ethmoid and maxillary sinuses tumours the NCCN guidelines 22 suggest (as clinically indicated) chest CT (with or without contrast) and consider FDG PET/CT for advanced nodal disease, to screen for distant metastasis and for selected smoking patients, to screen for lung cancer (Tab. 4.I).
Ruling out DM in the follow up. NCCN guidelines 22 provide generic follow-up strategy (common for all head and neck malignancies, regardless of histology) (Tab. 4.II).
Lymphoma of head and neck
Lymphoma is the second most common neoplasm in the head and neck and the most common diagnosis for unilateral neck masses in patients aged 21 to 40 years. Head and neck may be involved both by primary and secondary lymphoma.
Primary lymphoma is defined as disease confined to a subsite (isolated involvement) without other sites of lymphoma.
Secondary lymphoma implies focal lymphomatous lesion in presence of disease in near area or systemic involvement (disease outside the region of interest). Secondary involvement of head and neck subsites (usually asymptomatic) by systemic lymphoma is believed to be more common than may appear from isolated cases of primary lymphoma described in Literature 25.
MR imaging, CT, and PET are currently used for staging and surveillance imaging. CT is routinely performed to evaluate nodal involvement (neck, chest, abdomen, and pelvis), but offers only morphological information (size and morphological criteria) and cannot distinguish post-treatment fibrosis from residual active tumour.
FDG-PET complements these studies by adding useful data about metabolic activity using standardised uptake values (SUVs).
Therefore, PET surveillance after treatment is the key to finding residual or recurrent disease that can be nonspecific on anatomic imaging. Specifically, FDG-PET/CT can help to distinguish post-treatment fibrosis from active residual tumour and may also be useful for early prediction of treatment response. Watal et al. concluded that FDG-PET/CT is the imaging modality of choice for initial staging, post-treatment response assessment, surveillance and restaging of lymphomas 25.
5. Head and neck cancer distant metastases
DM represent the main variable in both the therapeutic decision and prognosis of patients with HNSCC 1,2. Patients presenting with DM at diagnosis are generally considered incurable and treated in a palliative manner with notable worsening of survival, even with the best systemic therapies 3.
Unnecessary aggressive treatments can be avoided with identification of risk factors for DM and investigation of possible DM during initial diagnostic work-up.
The incidence of DM in subjects with SCC, reported in several retrospective clinical studies, is relatively low, ranging from 2.8% to 26%; while studies based on autopsy findings showed higher percentage, varying between 37% and 57% of cases 1,4,5.
When DM are analysed at presentation and during follow-up, there were no significant differences in the percentages seen (Tabs. 5.I, 5.II), even though the data appear to be significantly influenced by the extent of disease 4-25.
Table 5.I.
Prevalence of DM in HNSCC.
| Authors | Year | % DM |
|---|---|---|
| Leon et al. 4 | 2000 | 5.1 |
| Fortin et al. 6 | 2001 | 8.9 |
| Spector et al. 7 | 2001 | 8.5 |
| Al-Othman et al. 8 | 2003 | 11.0 |
| Carvalho et al. 9 | 2003 | 4.8 |
| Kowalski et al. 10 | 2005 | 3.5 |
| Garavello et al. 11 | 2006 | 9.2 |
| Bourhis et al. 12 | 2006 | 8.0 |
| Lim et al. 13 | 2010 | 9.4 |
| Van der Schroeff et al. 14 | 2012 | 10.9 |
| Kiems et al. 15 | 2016 | 11.6 |
| Duprez et al. 16 | 2017 | 13.7 |
Table 5.II.
Distant metastasis at presentation.
| Authors | Year | Number of cases | % DM |
|---|---|---|---|
| Black et al. 18 | 1984 | 121 | 12.3 |
| Bhatia et al. 25 | 1987 | 1,127 | 1.2 |
| Jackel et al. 20 | 1999 | 1,087 | 1.5 |
| De Bree et al. 19 | 2000 | 101 | 16.8 |
| Kuperman et al. 1 | 2011 | 73,247 | 2.82 |
| Haerle et al. 22 | 2011 | 299 | 10.0 |
| Fogh et al. 23,* | 2012 | 182 | 5.0 |
| Li et al. 21,** | 2019 | 1,780 | 6.5 |
| Grisanti et al. 24 | 2019 | 192 | 23.0 |
| Liu et al. 17 | 2019 | 151,730 | 3.0 |
*: only hypopharyngeal carcinomas
**: only stage III IV.
The mean time to detect DM after initial diagnosis is approximately 16 months: Duprez found 70% of the DM in the first year after treatment and 89% in the second year 16. Similar results were reported by Leon, who detected the appearance of DM in 84% of cases by the second year and in 100% after 4 years 4.
The most common metastatic sites are lung and bone, followed by the liver, brain and skin (Tab. 5.III). An inverse behaviour is observed for nasopharyngeal carcinoma, showing a higher frequency of DM to bone: 50.2% compared to 32.8% of lung metastases 17.
Table 5.III.
Organ distribution of DM.
In HNSCC, the risk of DM is due to many factors: tumour site, T and N stage, histological tumour differentiation, residual disease and ENE.
T site is reported as an important risk factor: hypopharynx has the highest frequency of DM, followed by the oropharynx. T sites with the lowest risk of developing DM are the lip (0.35%) and glottic larynx (0.66%), while DM in supraglottic and subglottic laryngeal tumours is significantly higher (3%) (Tab. 5.IV).
Table 5.IV.
DM according to primary site.
In recent years, a remarkable increase of HPV-related oropharyngeal carcinomas has been suggested, and studies on these tumours have pointed out their features and clinical peculiarity. On these results, HPV-related oropharyngeal carcinoma has been distinguished from non-HPV oropharyngeal carcinoma as stated in the latest TNM classification edition. Moreover, HPV+ oropharyngeal carcinomas behave less aggressively and have a lower incidence of DM.
In a case study of 20,180 cases of oropharyngeal carcinoma, Liu 17 reported the frequency of DM in HPV+ oropharyngeal tumours was 2.1% compared to 4% in HPV- forms, as confirmed by other authors in recent publications 16,18-29.
T stage represents a risk factor for DM in all head and neck sites with a clear prevalence in T3 and T4 cases (Tab. 5.V).
Table 5.V.
DM according to T stage.
Kuperman compared the percentage of DM to the maximum size of T, detecting a frequency of 1%, 2.26% and 5.04%, respectively, for neoplasms with a maximum diameter < 2, > 2.1 - < 4 and > 4 cm 1.
Histological grading represents another risk indicator for DM with a slight increase in moderately and poorly differentiated forms (grades 2 and 3) compared to well-differentiated ones (15% vs 9%) 6-16.
In surgically-treated patients, the involvement of resection margins and the finding of perineural and vascular invasion do not represent a risk indicator for DM. In a series of 1,022 cases, Duprez observed DM in 17.6% of R0 (no residual tumour) cases and in 13.1% in R1 (microscopic residual tumour) - R2 (macroscopic residual tumour) cases 16.
An important risk factor for DM is represented by N stage. Stages N2b and N3 are highly predictive of DM compared with T stage (Tab. 5.VI).
Table 5.VI.
DM according to N stage.
In a series of 73,247 cases, Kuperman 1 reported significant differences (p < 0.0001) in the incidence of DM between N0/N1, N1/N2 and N2/N3 tumours. Radiological or histological findings of N+ with extranodal extension (ENE) after surgical treatment is a relevant factor for predicting the risk of DM.
Duprez reported a DM rate of 32% in cases with ENE compared to 11.9% in patients without ENE 16.
N as risk factors for DM is well recognized by several authors: Senft and Deurvorst have identified the following characters of N as high risk predictor 2,30:
three or more metastatic lymph nodes;
bilateral metastatic lymph nodes;
metastatic lymph nodes with diameter > 6 cm;
metastatic lymph nodes in the lower jugular chains (levels IV and V);
ENE;
loco-regional recurrence.
Moreover, age and race are reported as potential risk factors for DM with a higher incidence in black and advanced age patients.
Finding DM at diagnosis and during follow-up of high-risk patients with head and neck SCC is definitely linked to diagnostic tools, and must be particularly scrupulous to optimise the therapeutic approach. Diagnostic standards at diagnosis and during follow-up (FU) include standard chest radiography and neck CT or MRI. The European guidelines of the European Head and Neck Society and of the European Society for Medical Oncology 31 still recommend this standard guidance, but advise considering a chest CT and CT or MRI of the head and neck in advanced cases and for those at risk of DM. The guidelines of the NCCN 32 recommend performing a chest CT and MRI of the head and neck in all neoplasms.
FDG PET can be useful to detect DM more than pulmonary CT. The combination of FDG total body PET and CT has shown a greater sensitivity compared to the two individual methods alone 2, and in several recent studies this combination was the most sensitive imaging technique in screening for DM 2,33.
Table 5.VII and Table 5.VIII show the percentages of accuracy that different diagnostic tools can grant in finding DM, and show a clear diagnostic improvement with by combining FDG PET and CT.
Table 5.VII.
True detection rate of DM with different diagnostic methods.
Table 5.VIII.
True detection rate of DM for different site of T with different diagnostic methods.
| Side | Number of cases | PET/CT | CXR/hnCT-MRI | CCT/hnCT-MRI |
|---|---|---|---|---|
| Oral cavity | 357 | 2.8% | 0.2% | 2.0% |
| Pharynx | 404 | 6.0% | 2.2% | 4.7% |
| Larynx | 269 | 1.9% | 1.1% | 1.5% |
| Total | 1030 | 3.8% | 1.3% | 2.9% |
A cost-effectiveness analysis in using FDG PET and CT in the screening for DM showed that it is expensive, but without any doubt, is useful to reduce the number of unnecessary invasive treatments 2.
OS in patients with DM is significantly worse than in patients without DM, with mean survival varying from 1 to 12 months 1. The presence of single metastasis compared to multiple metastatic sites has not proven to be predictive of longer life expectancy. In addition, patients with DM at diagnosis have a worse life expectancy than patients with DM diagnosed during follow-up (7 months vs 16 months) 2,33.
The metastatic site has no impact on prognosis or the therapeutic approach; it is generally handled with palliative chemotherapy, not excluding combination with surgery whenever possible. The results of palliative chemotherapy are not satisfactory and are burdened by major toxicity, and thus this treatment is allowed only for patients in good condition, granting lasting life expectancy. Combination of palliative chemotherapy and surgery on a single metastatic site has shown a good impact on survival, even though in long term the impact of solitary metastases remains unknown 26.
DM in HNSCC represents an important factor for patient survival and the therapeutic approach.
Identification of risk factors for DM are fundamental and a recent literature analysis suggests the following order of importance:
T site: hypopharyngeal and oropharyngeal cancers represent the main site with more DM at diagnosis and during follow-up;
N stage: the associated factors are low latero-cervical side, number of metastatic lymph nodes and extranodal extension 2,30;
T stage: in relation to the involvement of several sub-sites.
6. Distant metastases in EBV- and HPV-related squamous cell carcinomas
EBV- and HPV-related squamous cell carcinomas are cancers related to viral infection and share distinct clinical features. Despite frequent expression of clinical aggressiveness, EBV+/ HPV+ head and neck SCC have superior loco-regional control and survival following RT or CHT compared to their EBV-/HPV- counterparts. Nevertheless, some EBV +/ HPV+ SCC patients suffer from poor outcomes, mainly related to development of distant metastases, which is the dominant pattern of failure.
6.1. EBV-related squamous cell carcinoma
EBV infection is a well-recognized carcinogenic factor that has been implicated in the aetiology of several malignancies of both lymphoid and epithelial tissues, including Burkitt’s lymphoma, Hodgkin lymphoma, gastric cancer and NPC.
EBV plays an important role in head and neck carcinogenesis, especially in the non-keratinising subtype of NPC (NKC according to WHO), an endemic malignant tumour in South China and South Asia where the incidence remains consistently high. In non-endemic areas (Europe and USA), NPC is a rare disease with a prevalence in Italy of about 1.4 per 100,000 inhabitants. Several studies have identified that a combination of genetic, ethnic and environmental factors are implicated in the pathogenesis of NPC 1. EBV-related undifferentiated NPC is an aggressive and metastatic malignancy, but highly responsive to radiotherapy and chemotherapy. However, the low incidence of EBV-associated NPC in a non-endemic population has a favourable prognosis compared to EBV-negative tumours 2.
The high propensity to distant spread represents a typical feature of NPC. The presence of DM classify NPC to stage IVB according to the updated 8th edition of the TNM 3 staging system. Data from literature studies report that 5-15% of patients develop DM at the time of clinical presentation of NPC and 50-60% during the course of disease. With improved loco-regional control of disease, thanks to current protocols, DM has become the main cause of failure in NPC patients. Even if 5-year survival rates have significantly improved in recent years, DMs to bone, liver and lung are the main factors determining treatment failure and death in loco-regionally advanced NPC. Bone is the most frequently involved site of metastases with an estimated incidence of 54-80% 1.
Traditional pathological and clinical factors predicting DM are TNM stage and treatment failure. However, considering the different biological behaviour of NPC with variable tendency to DM, identification of molecular markers is crucial to stratify loco-regionally advanced NPC in order to adopt tailored oncological therapy.
Quantitative plasma EBV-DNA expression is considered to be a sensitive and highly specific biomarker for screening, monitoring and prediction of disease recurrence and clinical outcomes in NPC 4, but controversy still exists for its optimal clinical use. EBV-induced carcinogenesis depends on the expression of latent membrane protein (LMP1), an oncoprotein encoded by EBV, that is positively associated with metastatic status of NPC 5 (Fig. 6.1). Moreover, a gene expression-based signature was recently developed and validated to predict DM in loco-regionally advanced NPC 1.
Figure 6.1.
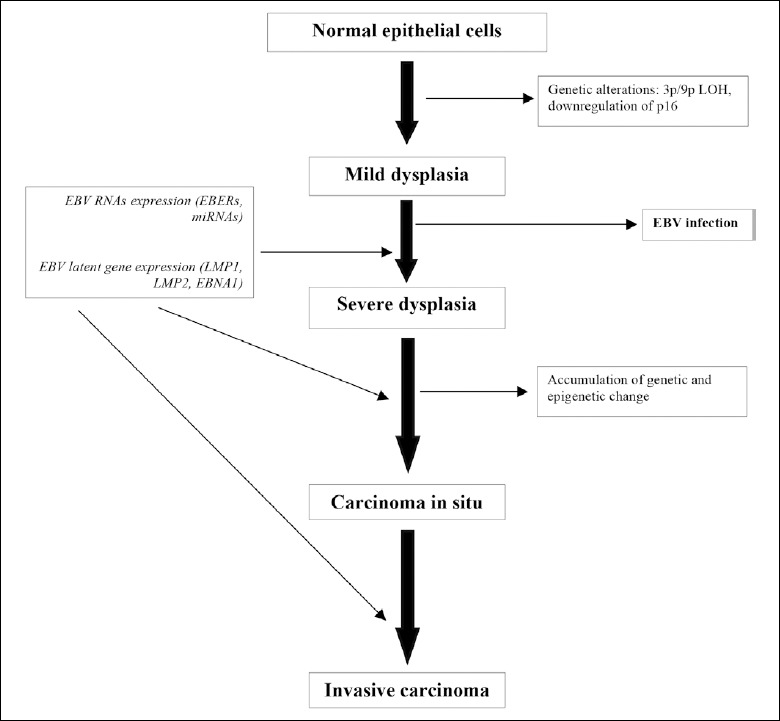
Role of genetic alterations and EBV infection in NPC progression (from Nakanishi et al.,2017 5, mod.).
EBV-DNA levels can be easily evaluated by real-time polymerase chain reaction (PCR), but different cut-off values are reported in the literature and assay standardisation is still lacking. Furthermore, data from early studies were heterogeneous and sometimes inconsistent. A comprehensive meta-analysis published by Zhang based on a large pool of clinical studies including 10,732 patients showed that detection of EBV-DNA at different cut-off values can be considered as an effective prognostic factor of NPC, as high expression levels predicting poor prognosis. It was suggested that > 1,500 copies/mL is a reasonable cut-off value for EBV-DNA 6.
An EBV-DNA assay can be employed to predict progression of disease and monitor NPC during therapy. Pre-treatment plasma EBV-DNA (pre-EBV) expression is an important prognostic factor for OS and distant metastases-free survival (DMFS) 7. Si-Wei and coll. demonstrated that patients with high expression of Raf kinase inhibitory protein (RKIP), a metastatic suppressor protein, and concurrent low EBV-DNA levels showed better response to inductive chemotherapy combined with radiotherapy and longer 5-year DMFS in loco-regionally advanced NPC 8. As confirmed by a recent meta-analysis, persistent post-treatment high levels of EBV-DNA are associated with an increased risk of disease progression and DM in NPC 9.
Role of pre-treatment, midpoint and post-treatment EBV-DNA as predictive tools
A correlation between plasmatic EBV-DNA and tumour burden of NPC has previously been reported 10. Likewise, the predictive value of pre-treatment EBV-DNA (pre-EBV-DNA) levels and tumour volume in NPC have also been assessed in several studies 11. Pre-EBV-DNA is an effective prognostic factor for predicting loco-regional progression of disease and risk of developing distant relapse 11. High pre-treatment EBV levels are associated with the risk of DM. Accordingly, EBV-DNA expression is strictly correlated with progression-free survival (PFS) and DMFS 11.
A negative prognostic value of pre-EBV DNA viral load was reported by Alfieri et al. even in patients from a non-endemic area. In a study on 130 loco-regionally advanced NPC patients, viral load was positively related with T-stage, recurrence of loco-regional and/or distant disease and survival 12.
Stratification of risk based on overall TNM stage without distinction between T and N features has to be considered unsatisfactory. Quantitative EBV-DNA expression in NPC seems to be related to both anatomic and volumetric parameters of the primary tumour and metastatic lymph nodes. However, pre-EBV DNA levels seem to be mainly related to metastatic lymph node volume rather than primary tumour expansion 10. This observation may be explained by a greater share of cell-free EBV-DNA related apoptosis and necrosis in metastatic lymph nodes, especially in the presence of ENE. Zhou et al. recently proposed an integrative risk stratification model based on EBV-DNA levels, tumour anatomic features and tumour volume in order to predict the probability of DM. According to the authors, nodal volume, skull base invasion and supraclavicular fossa lymph node metastases with EBV-DNA expression were all independent predictive factors that are significantly related to DMFS 10.
Plasma EBV-DNA load at the midpoint of chemo-radiation (4th week) predicts loco-regional disease and distant failure. A meta-analysis of 7,836 cases by Zhang confirmed the prognostic value of midpoint EBV-DNA (mid-EBV-DNA) on OS, PFS and DMFS 13. However, in the same study, detection of post-EBV-DNA was a stronger prognostic factor 13. Mid-EBV expression could be used to predict clinical outcomes and adapt treatment according to risk.
Plasma EBV-DNA expression during post-treatment follow-up (post-EBV-DNA) is considered to be a good prognostic factor, especially for prediction of DM in NPC patients. EBV-DNA can be detected in 86-96% of patients who develop DM, regardless of loco-regional relapses. Given that EBV-DNA can be released from sub-clinical micro-metastases that are not detectable by imaging, it should be considered a good marker for early detection of metastatic disease. Persistent detectable plasma EBV-DNA detection after completion of chemo-radiation is significantly related to worse prognosis 12. Since plasma EBV-DNA is highly accurate in detecting disease recurrence and distant metastases, all patients with advanced NPC should be regularly monitored by serological tests 4.
Role of FDG PET/TC
FDG PET/TC parameters, and especially SUV-max, are considered significant prognostic factors in NPC. High values of pre-treatment SUV-max are related to an increased risk of adverse events and predict poor prognosis 14. In a study on 294 loco-regionally advanced NPC (stage III-IVB according to the 7th edition of AJCCsystem) 15, a significant correlation between standardised uptake value for neck lymph nodes (SUV max-N) in FDG PET/TC and DMFS was reported. The authors developed a prognostic model combining SUV max-N and clinical stage to stratify the risk of DM and predict survival outcomes. At multivariate analysis, SUV max-N and this prognostic model were independent prognostic factors for DMFS 16. Moreover, the SUV value of the farthest lymph node station at pre-treatment FDG PET/TC seems to be a significant predicting factor for DM.
Therapy
Application of intensity-modulated radiotherapy (IMRT) and updated CHT (induction, concurrent and adjuvant) strategies have contributed to improve survival outcomes and reduce toxicities in NPC patients 1. RT in combination with concurrent CHT-RT is considered the mainstay treatment for advanced-stage disease. Despite the availability of standardized therapeutic protocols, DM are still the major cause of treatment failures in NPC. Chemotherapy with gemcitabine plus cisplatin has been established as the standard first-line treatment in recurrent or metastatic NPC (RM-NPC) 17.
In addition to TNM stage, plasma EBV-DNA levels can help to stratify patients into different classes of risk for distant failure 18. A recent large retrospective study explored the value of neoadjuvant chemotherapy (NACHT) or adjuvant chemotherapy (ACHT) added to concurrent chemo-radiotherapy (CCRT) in 2,263 patients with stage III-IVB NPC based on pretreatment EBV-DNA classes of risk (low and high groups with a cut-off value of 4000 copies/mL). Patients with NPC in the low-risk group treated with NACHT followed by CCRT achieved significantly better 5-year DMFS compared to CCRT alone. NACHT was the only independent prognostic factor for DMFS at multivariate analysis 18. Therefore, pre-EBV DNA may be a useful predictive factor to plan individualised treatment for NPC patients.
Recently, two phase 3, multicentre, randomised, controlled trials demonstrated that induction chemotherapy (ICHT) with docetaxel, cisplatin and fluorouracil followed by CCRT can significantly improve 5-year OS and DMFS in loco-regionally advanced NPC 1. Other studies confirmed a survival advantage of ICHT when added to CCRT, mainly due to improved distant control of disease. ICHT plus CCRT should be administered to patients with a high risk of DM (level 2A). Pre-treatment EBV-DNA detection may better predict optimal tumour response to ICHT 1.
Plasma EBV DNA detection after completing chemo-radiotherapy was used as a predictive biomarker to identify patients with high relapse risk for adjuvant chemotherapy. However, the authors did not observe better results in relation to 5-year relapse-free or OS 1.
Whereas survival times of NPC patients diagnosed as stage M1 vary widely, reliable prognostic risk factors are needed to optimise and personalise treatment. Sun et al. in a study on 226 patients with bone metastases at primary diagnosis reported the number of metastatic lesions and EBV-DNA levels after palliative CHT as independent prognostic factors for OS. Stratifying patients according to these factors, a survival benefit was observed in low and intermediate risk groups treated with CHT combined with loco-regional RT. RT of oligometastatic lesions, even in low risk patients, did not lead to increased survival 19.
The similarity in pathological features and clinical behaviour of HPV-related OPSCC and EBV-associated NPC mean that common molecular pathways are linked to the host immune response. Recently, a possible role of deregulation of the inflammatory process in NPC tumour progression was hypothesised. EBV-associated NPC can be considered an “inflamed” tumour characterised by a rich lymphocytic infiltrate and increased PD-L1 expression. These evidences have suggested an immunotherapeutic approach even in locally advanced NPC with a high risk of systemic metastatic relapses 2.
Several clinical trials have been conducted to test the efficacy of an immune-therapeutic approach in advanced NPC. Preliminary results seem to support a therapeutic role for immunotherapy (IT) in combination with RT and CHT to treat advanced and metastatic NPC 2. In NPC patients with refractory-recurrent disease, modest response rates (20-30%) were obtained with anti-PD-1 antibodies nivolumab and pembrolizumab. Lv and co-authors conducted a comparative study on the safety and efficacy profiles of anti-PD-1 agents with/without CHT in RM-NPC. The observed response rate (ORR) of anti-PD-1 first-line therapy ranged from 19% to 34.1%, higher for camrelizumab. First-line camrelizumab plus CHT achieved a significantly increased ORR compared with CHT alone (90.9% vs 64.1%). These studies are summarised in Table 6.I 20.
Table 6.I.
Clinical trials in advanced NPC.
| KEYNOTE-028 | NCI-9742 | CheckMate-358 | JS001 | SHR-1210 (mono) | GEM20110714 | SHR-1210 (comb) | |
|---|---|---|---|---|---|---|---|
| Country | Taiwan | International collaboration | International collaboration | Mainland China | Mainland China | Mainland China | Mainland China |
| Inclusion period | 2014-2016 | 2015-2016 | 2015-2017 | 2016-2018 | 2016-2017 | 2012-2015 | 2017 |
| Phase | 1 | 2 | 1,2 | 2 | 1 | 3 | 1 |
| Key eligibility criteria | recurrent/metastatic NPC; failure on prior standard therapy; PD-L1 ≥ 1% | recurrent/metastatic NPC; failure on at least one prior line of Pt-based chemotherapy | recurrent/metastatic NPC;
≤ 2 prior systemic therapies |
recurrent/metastatic NPC; failure on at least one prior line of Pt-based chemotherapy | recurrent/metastatic NPC; failure on at least one prior line of Pt-based chemotherapy | treatment-naive recurrent/metastatic NPC | treatment-naïve recurrent/metastatic NPC |
| Experimental regimen | Pembrolizumab | Nivolumab | Nivolumab | JS001 | Camrelizumab | Gemcitabine
+ cisplatin |
Camrelizumab
+ gemcitabine + cisplatin |
| Sample size | 27 | 45 | 24 | 143 | 93 | 181 | 23 |
| Median age | 52 | 57 | 51 | 46 | 45 | 47 | 44 |
| Male (%) | 77.8 | 77.8 | 88 | 84.6 | 81 | 83.1 | 74 |
| Pd-l1 expression ≥ 1% (% ) | 100 | 42,9 | - | 44,1 | - | - | - |
| Median follow-up (months) | 20 | 12.5 | 26 | - | 9,9 | 22 | 10,2 |
| Objective response rate (%) | 26.8 | 20.5 | 20.8 | 23.2 | 34.1 | 64.1 | 90.9 |
| Overall survival median (months) | 16,5 | 17,1 | - | - | - | 29.1 | - |
| Os 1-year rate (%) | 63 | 59 | - | - | - | 83.2 | - |
| Progression free survival median (months) | 6.5 | 2.8 | 2.4 | - | 9.9 | 7 | 10.2 |
| Pfs 1-year rate (%) | 33.4 | 19.3 | - | - | 27.1 | 19.6 | 61.4 |
| All grade adverse events (%) | 74.1 | - | 54.2 | 92.3 | 96.8 | 91.7 | 100 |
| Grade 3-5 adverse events (%) | 29.6 | 22.2 | 8.3 | 24.5 | 16.1 | 42.8 | 87 |
Moreover, high expression by immunohistochemical staining of receptor activator of NF-kB (RANK) and its ligand (RANKL), key regulators of bone metabolism, was documented in metastatic specimens of EBV related NPC. The authors hypothesised the implication of RANK pathway in NPC cancer progression and metastatic spread and suggested possible future treatment with denosumab, a clinically approved monoclonal antibody for bone metastases 21.
Further studies are needed to understand if vaccines may be of benefit in patients with EBV positive malignancies in improving outcomes, especially in advanced and refractory disease.
While combination chemo-radiation therapy increases response rates, DM constitute the main cause of failure for advanced NPC. Plasma EBV-DNA expression is currently considered a reliable prognostic biomarker that can be employed to elaborate risk stratification models to predict and monitor responses to treatment and oncological outcomes in NPC. Future RCTs and validated clinical trials are needed to develop tailored treatment strategies in loco-regionally advanced and metastatic NPC.
6.2. HPV-related squamous cell carcinoma
OPSCC is a specific clinical entity with a reported worldwide incidence of about 100,000 new cases/year. In Italy, there is a reported incidence of about 1,000 new cases/year, with a male prevalence of about 70%; 30.8% of new cases of OPSCC can be considered to be related to HPV infection. In developed countries, HPV-related OPSCC show an incidence of 45-50%.
HPV includes a family of DNA viruses that infect basal epithelial cells, causing benign and malignant lesions of the skin and mucosae of the upper aero-digestive and ano-genital tracts. In head and neck cancer, three sites have been associated with HPV: oropharynx, oral cavity and larynx. There are several known types of HPV and only some have been recognized as carcinogenic. Types 16 and 18 are globally responsible for 85% of HPV-related cancers of the head and neck, while the relative contribution of HPV 6/11/16/18/31/33/45/52/58 is 90% 22.
HPV-related OPSCC has a different epidemiological profile compared to tobacco- and alcohol-associated OPSCC. HPV-positive patients are commonly younger, with a shorter smoking history, lower T-stage but higher N-stage and better performance status.
HPV-related OPSCC also appear to be more responsive to treatment and have better survival rates. In a population-based study of 1,542 consecutive patients by Larsen et al. 23, HPV/p16 status emerged as an independent predictor for OS even when adjusted for T stage, N stage, treatment, smoking history, age and performance status (5-year OS 77% in HPV+/p16+ group vs 30% in HPV-/p16- group). The authors found a significant difference in progression (19% of patients in HPV+/p16+ group vs 36% in HPV-/p16- group) and time to progression (TTP) (14 months in HPV+/p16+ group vs 8.5 months in HPV-/p16- group). Survival after progression (SAP) was also improved by HPV status (median SAP 13 months in HPV+/p16+ group vs 6 months in HPV-/p16- group).
Distant progression (DP) in OPSCC also seems to differ between HPV+ and HPV- tumours. A systematic review and meta-analysis by Tiedemann et al. 24 confirmed a different epidemiology profile in HPV+ patients: HPV+ OPSCC have a tendency (even if not statistically significant) of presenting longer time to DP (0.2 to 106 months in HPV+ tumours vs 0.2 to 33 months in HPV-tumours) and multiple sites of DP (36% of patients in HPV+ group vs 2% in HPV- group; RR = 16.49, 95% CI 2.33; 116.51). An important observation was that DP to non-regional lymph nodes was almost exclusively observed among patients with HPV+ tumours (RR = 4.7, 95% CI 1.51; 15.21). It is also reported that DP in HPV+ OPSCC can still be detected up to 5 years of follow-up, while DP rates in HPV- HNSCC are stable after 2 years 25.
The different epidemiological profiles are summarised in Table 6.II.
Table 6.II.
Epidemiological profiles of HPV+/p16+ OPSCC vs HPV-/p16- OPSCC (from Resteghini et al., 2017 21; de Montel et al., 2017 22, mod.).
| HPV+/p16+ | HPV-/p16- | ||
|---|---|---|---|
| 5-year overall survival (OS) | 77% | 30% | |
| Local progression | Rate
Time to progression Survival after progression |
19%
14 months 13 months |
36%
8.5 months 6 months |
| Distant progression (DP) | Time to DP
Multiple sites of DP |
Up to 106 months
36% |
Up to 33 months
2% |
DM in HPV-related OPSCC may occur at unexpected sites and after long intervals. Distant metastatic progession in p16-positive OPSCC more often exhibits a “disseminating” pattern (Tab. 6.III) 26,27.
Table 6.III.
| Oligometastasis | limited to 1-2 anatomic sites or ≤ 3 metastatic foci in one anatomic site |
| Disseminating | > 2 anatomic sites |
| Explosive | ≥ 4 foci of metastasis at one anatomic site |
Trosman et al. 28 observed that DM in HPV+ disease appear to involve a greater number of subsites than in HPV- disease. In addition, they found a tendency towards dissemination to unusual distant sites and increased rates of non-regional lymphatic metastases in the in HPV+ group, as summarised in Table 6.IV.
Table 6.IV.
Metastatic sites (from Trosman et al., 2015 28, mod.).
| Site of metastatic disease | % of metastatic sites | |
|---|---|---|
| HPV- status | HPV+ status | |
| Lung | 58.3 | 40.4 |
| Bone | 16.7 | 21.1 |
| Brain | 16.7 | 3.5 |
| Liver | 8.3 | 12.3 |
| Intra-abdominal lymph nodes | 0 | 5.3 |
| Axillary lymph nodes | 0 | 3.5 |
| Kidney | 0 | 3.5 |
| Muscle | 0 | 3.5 |
| Skin | 0 | 3.5 |
| Pericardium | 0 | 1.8 |
| Peritoneum | 0 | 1.8 |
All these data suggest different dissemination patterns between HPV positive and negative OPSCC. Dok et al. 29 found reduced invasion abilities of HPV/p16 positive cells in vitro compared to HPV/p16 negative cells. Significantly lower expression of vascular endothelial growth factor A (VEGFA) was found in HPV+ patients, leading to reduced angiogenesis. The authors also found a higher percentage of alpha 4 beta 1 integrin in HPV+ cells, an integrin considered to be important modulator of lymphoangiogenesis. Even if based only on in vitro data, this study suggests a role for HPV/p16 expression in different dissemination patterns between HPV positive and negative OPSCC by control on angiogenesis and lymphogenesis. On one hand, reduced angiogenesis in HPV+ could lead to lower T stage. On the other, improved lymphogenesis in HPV+ could lead to higher N stage and different rates of distant progression.
Therapy
Management decisions regarding OPSCC have to take in account treatment toxicities and long-term functional outcomes, not only for disease control but also survival. Open surgery in oropharyngeal cancer has significant morbidity, especially in terms of speech and swallowing.
In early stage disease, the data suggest comparable locoregional control and survival between surgery and RT, but with lower rates of severe complications in non-surgical treatment 30. The Meta-Analysis of Radiotherapy in Carcinomas of Head and Neck (MARCH) trial demonstrated that altered fraction radiotherapy is associated with improved OS and PFS compared to conventional fractionation radiotherapy 31,32. This p16-status and smoking history oriented meta-analysis 32 showed no interaction between p16 status and the benefit of altered fractionation regimen, so that p16 status cannot be used to assign patients to a specific type of RT fractionation. This study demonstrated that altered fractionation RT is associated with a small but significant improvement in OS compared with standard fractionation, and that the improvement is more pronounced in the hyperfractionated RT group. Smoking patients with p16-positive tumours represent a clinical challenge due to their intermediate prognosis and significantly worse RT outcomes compared to p16-positive patients with a history of never or less heavy smoking 33. Transoral robotic surgery, being a minimally-invasive technique, seems to have encouraging oncologic, functional and quality of life outcomes in patients with early T classification. More clinical trials are needed to establish if transoral robotic surgery is preferable to RT treatment.
The optimal treatment of patients with locally-advanced disease involves any given combination and sequence of surgery, RT and CHT. Considering the significant acute and long-term toxicities of CCRT and good prognosis of HPV positive OPSCC, clinical trials are investigating deintensification treatment strategies 32.
Nowadays, good rates of locoregional control has shifted the pattern of failure toward distant metastasis, which has doubled in the past 20 years and accounts for approximately 45% of deaths. This evidence led the need to evaluate prognostic markers of DM in order to identify patients with higher clinical risk, who are not suitable for deintensification therapy.
In the recent literature, several prognostic markers have been evaluated including miRNA expression, advanced T and N classification and active smoking status. In 2016, Weller et al. 34 demonstrated that patients with HPV-positive oropharyngeal cancer at high risk of distant failure (T4 disease, active smokers and use of cetuximab in place of cytotoxic CHT) developed DM rates greater than 20%.
Actually, growing interest is focused on the potentially predictive role of “matted nodes” and HPV DNA/p16 status.
The term “matted nodes” identifies a condition of at least three nodes abutting one another with loss of intervening fat plane that is replaced with radiologic evidence of ENE 35.
Even if the predictive value of matted nodes is probably independent of HPV status 35, in HPV+ OPSCC it appears to be the strongest predictor for distant failure, any failure, cause-specific mortality and OS. The presence of matted nodes in patients with HPV+ OPSCC identifies patients with > 60% risk of distant failure, whereas the absence of matted nodes is associated with minimal risk of distant failure 36.
Rasmussen 37, in a recent analysis of 1,243 patients, by combining HPV DNA detection with p16 status, showed that HPV-/p16+ is a significant predictor for M-site recurrence and patients with HPV-/p16+ tumours have a significantly higher risk for M-site recurrence. The risk of M-site recurrence is twice that for patients with HPV-/p16+ tumours compared with the other combination of HPV DNA and p16 status.
In locally-advanced disease, standard treatment does not differentiate between HPV-positive and HPV-negative tumours and consists of either primary cisplatin-based chemoradiation or adjuvant chemoradiation after surgery. Starting from the observation that in advanced HNSCC the combination of RT with cetuximab offers superior locoregional control and OS compared to radiation alone without increasing toxicity, recent trials compared high dose cisplatin (HDC) chemoradiation to cetuximab chemoradiation. Data from the phase 3 trials De-ESCALaTE HPV and RTOG-1016 provided very strong evidence for cetuximab being inferior to cisplatin when combined with RT in HPV-related OPSCC (Tabs. 6.V, 6.VI) 38,39.
Table 6.V.
Phase III De-ESCALaTE HPV trial.
| Cisplatin | Cetuximab | ||
|---|---|---|---|
| 2-year OS | 97.5% | 89.4% | p = 0.0012 |
| 2-year recurrence rate | 6% | 16.1% | p = 0.0007 |
| Stage I/II OS | 98.4% | 93.2% | p = 0.048 |
| Stage III OS | 93.3% | 67.1% | p = 0.0304 |
Table 6.VI.
Phase III RTOG-1016 trial.
| Cisplatin | Cetuximab | ||
|---|---|---|---|
| 5-years OS | 84.6% | 77.9% | p = 0.0163 |
| Progression-free survival | 78.4% | 67.3% | p = 0.0002 |
| Locoregional failure | 9.9% | 17.3% | p = 0.0005 |
As demonstrated by many authors, immune system disfunction plays a role in both the development and progression of head and neck cancer, mostly in virus-associated cancers such as those caused by HPV and EBV.
Tumour IT aims to induce or enhance a tumour antigen specific immune response that is capable of killing tumour cells. HPV-related cancers are ideal candidates for IT since high risk-HPV transformed cells express E6 and E7 non-structural proteins. These oncoproteins are not only related to carcinogenetic processes induced by HPV infection, but could also be utilised as foreign antigens targets for IT 40,41.
Immune checkpoint inhibitors, such as nivolumab and pembrolizumab, have recently emerged as promising therapeutics in oncology.
In recent randomised, open-label, phase II and III trials (KEYNOTE-040, KEYNOTE-012, KEYNOTE-055 and CheckMate 141), the role of the PD-1 inhibitors pembrolizumab and nivolumab was compared with standard of care with methotrexate, docetaxel, or cetuximab in recurrent or metastatic head and neck SCC.
In these studies, pembrolizumab provided a clinically meaningful prolongation of OS in patients with PD-L1 expression by > 50% and a favourable safety profile when compared with standard therapies, without significant differences between HPV+ and HPV- patients 42-44.
Otherwise, in a post hoc exploratory analysis, OS was significantly increased in patients with HPV+ tumours treated with nivolumab, while OS was not statistically significant in those with HPV- tumours 45.
Starting from the observation that HPV-related intraepithelial neoplasia or cancers are ideal candidates for cancer IT, recent early stage clinical trials demonstrated encouraging results by combining a cancer vaccine and a checkpoint inhibitor for treating HPV-related cancers 40.
7. Cervical lymph nodes metastases from distant infraclavicular tumours
Neck masses are quite common in humans; many aetiologic factors can lead to the development of a congenital, inflammatory, or neoplastic neck mass, so inducing relevant problems in differential diagnosis. If we consider the oncological origin of a neck mass, the most common aetiology is a metastatic adenopathy from a HNSCC, followed by a lymphoma. When the primary tumour cannot be identified despite extensive diagnostic work-up, the neck lymphoadenopathy represents a diagnostic dilemma. In this case, the chance that the metastatic neck adenopathy (especially when located in the supraclavicular fossa) could have risen from an infraclavicular primary tumour has to be taken into account. For this reason, it is very important to know which tumours have a proneness to metastasise to cervical lymph nodes and how this eventuality should be managed.
Globally, metastatic tumours to the head and neck represent a rare pathological entity with an incidence of about 1% of the total number of malignant tumours in this area 1. However, an incidence up to 24% of primary tumours located below the clavicles has been reported in patients with cervical lymph node metastases from unknown primaries 2. If we consider all the metastases to the head and neck area from distant primary tumours, the bony structures (mandible and maxilla) of the facial skull are the most frequent locations, followed by the cervical lymph nodes. The most common primary tumours metastasising to the head and neck region are lung cancer in men and breast cancer in women, but gastrointestinal tract cancers and genitourinary tract cancers must also be kept in consideration as possible primary tumours. The prevalent site of metastatic lymph nodes from a primary tumour located below the clavicles is the supraclavicular (SC) fossa, more frequently on the left side, while metastases are more rarely found at a higher level in the neck (II or III level). Franzen et al. recently found in 94 of 211 cases (44.5%) of biopsy of a larger than 1 cm supraclavicular mass, a metastasis originating in a primary tumour located below the clavicle; the side of the metastatic lymph node was the same of the primary tumour in lung and breast cancers, while the left side of the neck was significantly more involved in metastases of abdominal and pelvic neoplasms 3. The reason for this phenomenon is first of all an anatomical one. The father of modern pathology, Rudolf Virchow, described in 1848 that left SC lymph node metastases could be frequently originated in gastric carcinomas 4. This study led to the eponym of Virchow’s node to describe the left SC lymph node involved by adenocarcinoma metastases, and is still mentioned in most pathology textbooks 5. Some years later, the French author Charles-Emile Troisier observed that some other abdominal tumours could also spread to left SC lymph node: following this observation, the SC lymph node started to be called “Virchow-Troisier node” 6. This pattern of metastatic spread is logical from an anatomical point of view, since common iliac and para-aortic lymph nodes drain into the thoracic duct. The thoracic duct arises as a continuation of the cisterna chyli at level L1 just below the diaphragm. It enters the thoracic cavity through the aortic hiatus of the diaphragm and passes in the posterior mediastinum between the aorta and the azygos vein, finally ending in the left supraclavicular fossa by joining the superior venous system at the junction of the subclavian and the internal jugular vein. As preliminary described in the article of Stevens in 1907 7, the gradual flow towards the left neck begins in the superior mediastinum, so the lymph nodes in the left base of the neck will have afferent drainage that includes the thorax, abdomen and pelvis. This anatomo-biological behaviour explains why most diseases from the foresaid areas occur in the left side of the neck. On the other hand, it must be recalled that a stop in the lymphatic flow from the left SC site could favour the retrograde lymphatic spread and the involvement of superior or contralateral nodes 8, occasionally producing nodal metastases from a remote primary tumour at an higher neck level or in contralateral nodes.
7.1. Diagnosis
When considering diagnostic workup in patients with a neck mass, first of all comprehensive history is essential and must include not only any existing symptoms related to a possible carcinoma of the head and neck, but also previous malignancy, since it is well known that a late metastasis can appear even many years after the primary tumour. Furthermore, especially if the mass is located in the lower one-third of the neck or in the SC fossa, the suspicion of a metastatic disease for a primary tumour located below the clavicles makes it mandatory to look for palpable masses in other sites outside the neck (the first row of the breast) and other symptoms such as coughing, haematuria, haemoptysis, gynaecological bleeding and weight loss, which should be attentively investigated. However, it is not rare that the cervical lymph node is the only manifestation of a cancer located under the clavicles in completely asymptomatic patients 9.
The coupling of US with FNAB of the cervical mass is the first and most commonly used diagnostic procedure, since it is a minimally-invasive and inexpensive, and is associated with high diagnostic accuracy. Gupta et al. evaluated the diagnostic value of FNAB in supraclavicular masses in 218 patients, showing an overall sensitivity of 92.7% and a specificity of 98,5%, even if in 46 cases (21,1%) an open biopsy resulted necessary in order to confirm the diagnosis 10. Morphological findings can be integrated by immunochemistry and molecular tests, which can be carried out on cytologic samples or on tissues obtained by an open biopsy. An example of this statement is reported in the study of Kuemper et al. showing the usefulness of Polymerase Chain Reaction (PCR) detection of HPV to find out oropharyngeal primary as well as gynecological (utero-cervical) origin in case of a SC metastasis 11. When FNAB fails in producing enough diagnostic information, an open incisional or excisional biopsy of the lymph node should be performed, in order to add more information useful to a more complete diagnosis. In the recent report by Ismi et al. excisional biopsy of SC lymphadenopathy was carried out in 18 patients, since FNABs have been previously proven non-diagnostic. In all the 18 cases the histopathological examination of the lymph nodes allowed the topodiagnosis of the primary tumor; the most frequent histological findings were adenocarcinomas, followed by squamous cell carcinomas and neuroendocrine tumors 12. The Authors points out that the cases of adenocarcinoma are particularly challenging since different anatomic sites can show this primary tumor. In this study adenocarcinomas were mostly demostrated from primaries of the breast, followed by the lung, the prostate and the stomach 12.
There are many relatively specific tumoral markers that can be studied in order to identify the primary site of cancers. In adenocarcinomas the profiles of cytokeratin CK7 and CK20 are the most frequently used to locate the primary site of tumour, since CK7 is present in tumours of the lung, the breast, the ovary and the endometrium. On the contrary, CK20 is more indicative of a tumour of the gastrointestinal tract. The most useful markers for identification of metastases from lung adenocarcinomas are Thyroid Transcriptor Factor-1 (TTF-1) and Napsin-A, while for breast cancers the more commonly used immunohistochemical markers are Estrogen Receptor (ER), Progesterone Receptor (PR), Epidermal Receptor 2 (HER2)/neu (Receptor Thyrosine–Protein Kinase Erb B-2), gross cystic disease fluid protein, mammaglobina and GATA binding protein 3 (GATA-3). ER and PR in SC metastases could sometimes differ from the same markers in the primary tumour, so suggesting de-differentiation of the tumour during the metastatic process 8.
In addition to cytological/histological examination, contrast-enhanced CT of the neck, thorax and abdomen and/or MRI should be performed to locate the possible primary tumour.
FDG PET and FDG PET/CT are now recommended as additional diagnostic tools in conventional workup in patients affected by carcinoma of an unknown primary with cervical lymph node metastases, since they can provide important additional information compared with traditional imaging (CT/MRI) 13.
7.2. Lung cancer
Tumours of the lung are classified in two categories: non-small cell carcinomas (70% of lung tumours) and small cell carcinomas (30% of lung tumours). Non-small cell tumours are divided in SCC (25-30%), adenocarcinoma (40%), large cell carcinoma (10-15%) and alveolar cell carcinoma (1-2%). The risk of metastatic dissemination varies according to the histological type: it is highest for small cell carcinomas (74-96%) and lowest for SCCs (25-54%). Indeed, enlarged nodes of the supraclavicular fossa are found in 16% of non-small cell cancers and in 35% of small cell cancers 14. The presence of metastases in supraclavicular lymph nodes in lung cancer is classified as N3, thus defining stage IIIB. Since the management plan and prognosis of patients affected by lung cancer depends on histological type and stage of disease, it is very important to evaluate the presence of supraclavicular metastases. As they are often impalpable, SC metastases are primarily detected with imaging modalities such as US or neck CT, keeping in mind that the nodes in supraclavicular region might not be seen in chest CT. High resolution US evaluation is extremely useful for good imaging in these patients and to perform FNAB or tissue core biopsy 15. This latter exam has been demonstrated to be a safe procedure with high diagnostic accuracy to determine the tumour subtype and in molecular analysis, avoiding more invasive diagnostic investigations such as bronchoscopy with endoscopic biopsy or CT guided transthoracic biopsy in many patients 16.
The prognosis of patients affected by lung cancer with cervical metastases varies according to histological type, but in general it is poor in advanced stages of disease (stage IIIB or IV): for small cell carcinoma, median survival is 8 months with 5-year survival < 10%. Thus, in the majority of cases surgery for cervical metastases is not indicated, since it does not modify prognosis; only in a few cases with a single, ipsilateral to primary tumour SC lymph node metastasis can surgical excision of the metastatic lymph node be proposed with curative intent associated with adjuvant chemoradiotherapy.
In mesothelioma, the presence of SC metastases is a very rare event: only a few cases have been reported, and in these cases there is no role for neck dissection because of the poor prognosis of the disease 17.
7.3. Breast cancer
Cervical metastases from breast cancer are rare, and the incidence of ipsilateral SC node metastases without distant metastasis is as low as 1-4%. The finding of SC node metastases is still possible even many years after initial diagnosis.
Until 2002, SC lymph node metastases from breast cancer were considered as DM and conferred stage IV to the disease. This classification of stage was justified by the evidence suggesting that prognosis in patients with neck disease was poor, with 5-year survival rates ranging from 5% to 34%. The demonstration that patients with regional stage IV disease had better outcomes than visceral stage IV disease led to a revision of classification in 2003. This revision classifies metastases to the ipsilateral SC lymph node as N3c if no DM are diagnosed, and considers stage IIIC any T stage with N3 disease and M0 18.
As patients with DM were considered incurable, many cases with neck disease received only palliative care. This approach became progressively controversial, since a number of reports showed that patients with SC lymph node metastases managed with aggressive treatment (induction CHT, surgery, adjuvant CHT-RT) had an equivalent prognosis compared with patients classified as stage IIIB without DM and a better prognosis than patients classified as IV stage 19. Nowadays, there is still a widespread inconsistency in the management of breast cancer cervical metastases, even if the trend is towards more aggressive surgical treatment in case of SC metastases and absence of DM 20.
Finally, it must be pointed out that an overlap can exist in the histological and immunohistochemical (same overexpression of HER2/neu) appearances of breast and salivary gland carcinoma, making it sometimes difficult to distinguish between metastases from a breast or a salivary tumour 8.
7.4. Gastrointestinal tract cancer
Oesophageal cancer (EC) is a common upper gastrointestinal tumour with a particularly high incidence in Eastern Asia and Eastern and Southern Africa. SCC represents 95% of cases, even if in Western patients an important increase in adenocarcinoma of the inferior third of oesophagus has been observed in the last decades. Despite improvements in the diagnosis and treatment of EC, overall 5-year survival rates are still very low (< 40% of cases). The lymphatics of the oesophagus are located in the submucosal plexus and run the entire length of the organ with the upper two thirds draining superiorly and the lower third inferiorly; furthermore, there is lateral lymphatic spread draining to the thoracic duct. Because of this complex lymphatic supply, the lymph node metastases rate of EC is very high, even for submucosal EC (about 20-40%), and nodal skip metastases are a common pattern of metastatic lymph node involvement in thoracic EC 21.
Oesophagectomy with two-field lymphadenectomy, including abdomen and mediastinum, or three-field lymphadenectomy, also including SC lymph node dissection, is the therapeutic strategy of choice for resectable EC. However, the extent of lymph node dissection is still controversial, since the 7th American Joint Committee On Cancer (AJCC) Staging Manual 22 includes celiac axis and para-oesophageal nodes as regional lymph nodes, whereas it considers SC lymph nodes as distant metastases. Thus, patients with SC lymph node metastases should be classified as having stage IV disease and consequently excluded from indications for curative surgery. However, nowadays the therapeutic value of dissection of metastases to the SC lymph nodes in patients with thoracic EC is supported by a number of studies that showed a survival benefit of this therapeutic choice, demonstrating that SC lymph nodes have to be considered as regional nodes instead of DM 23.
Perhaps the most well-known of the SC node presenting in tumours not originating in the head and neck is Virchow’s node, which is affected in abdominal cancer, especially gastric cancer. Lymphatic spread from the stomach arises from nodes in the left gastric, hepatic and splenic chains, and reaches left SC nodes through the lymphatic duct. However, metastases to SC lymph nodes are not frequent; their presence indicates stage IV disease with a 5-year survival of 4%, so a role for neck dissection in these cases is not considered 24.
Metastases from hepatocellular carcinoma to the cervical and SC lymph nodes are rarely reported and very few case reports are published in the literature.
Other abdominal cancers such as cholangiocarcinoma or pancreatic adenocarcinoma have such a poor prognosis that, in the very rare cases of presence of cervical nodes metastases, neck dissection is not taken into account.
7.5. Genitourinary tract cancer
Renal cell carcinoma (RCC) is well known for its unpredictable clinical behaviour and is considered to be the third most frequent infraclavicular tumour able to metastasise to the head and neck region. However, SC metastases are rare and are found in about 3% of cases, but this rate increases significantly in advanced metastatic disease up to 13%. RCC metastasising into the head and neck area primarily do so in the cervical lymph nodes. In some cases, a cervical metastasis may represent the first manifestation of disease, while in other cases cervical metastases may occur months or even years after apparently successful treatment of the primary tumour. Since head and neck metastases of RCC may occur at any time during the course of the illness, any head and neck-related symptoms, such as enlarging neck mass, should promptly be submitted to an clinical examination by an otolaryngologist and an ultrasound examination of the neck and the thyroid. The management of such metastases must be tailored to the clinical presentation of the individual patient, especially considering the presence or absence of metastases in other sites and their locations. Surgery should be taken into account in all patients fit for surgery, for both curative treatment and palliative intent, since it may improve the quality of life and provide good local control of the disease in the neck 25.
Cervical lymph nodes metastases from bladder or urothelial carcinomas are very uncommon and usually are associated with advanced disease and very poor prognosis. Thus, at present, there is no evidence supporting therapeutic cervical node dissection for treatment of urothelial or bladder metastases.
Prostate cancer is a common cause of morbidity among elderly men and has a wide spectrum of presentations. It can present with lower urinary tract symptoms or asymptomatically with elevated prostatic-specific antigen (PSA) levels, and usually spreads locally to adjacent pelvic lymph nodes and through direct invasion to nearby organs such as the bladder, rectum or spine. The incidence of metastatic prostate adenocarcinoma to the SC lymph nodes is quite low, with a reported rate of approximately 0.28%. Cervical or SC lymphadenopathy has been very rarely reported as the first presentation of metastatic prostate cancer, even if prostate cancer is the most common genitourinary cause of this presentation. The presence of SC or cervical lymph nodes metastases indicate stage IV disease with a 5-year survival rate of 30%. However, on occasion the prognosis of metastatic prostate cancer to the head and neck is relatively good, since it can show a good response to androgen deprivation therapy, thus attaining long-lasting remission. Surgical excision can be taken considered in case of an isolated resectable neck mass to prevent development of symptoms in selected patients 26.
Although SC lymph nodes metastases from prostate adenocarcinoma are rare, PSA must be used as a diagnostic tool in any male patient aged more than 50 years affected by neck metastases from unknown primary, in order to exclude the presence of prostate cancer.
Testicular tumours are divided in non-seminomatous and seminomatous germ cell tumours; the latter is the most common cancer in patients aged 15-35 years. Cervical lymph node metastases originating from testicular cancer are rare, but represent a well established phenomenon, more commonly observed in patients with advanced stage disease. Neck metastases are almost invariably left-sided, reflecting the anatomy of the lymphatic system and the characteristic route of metastases.
Since metastatic testicular carcinoma can be detected firstly as a cervical mass, testicular cancer must be considered as a differential diagnosis in a young man with neck adenopathy, especially if the nodes are located in the left SC fossa. The treatment of choice of advanced testicular cancer (stage II-IV) is platinum-based CHT with a reported high overall rate of cure. However, approximately 70% of patients will have residual masses in the retroperitoneum or other sites post-chemotherapy, with viable tumour present in 10-15% of these masses. In these patients, surgery often is the only treatment with a potential for cure, because these lesions are often refractory to CHT, especially in patients who have already received CHT.
Surgical resection by selective neck dissection is indicated in both the case of a residual post-CHT mass and in the case of late distant recurrences in the neck, since it has been shown that excision of the residual neck mass allows good local control and can contribute to increasing long-term survival 27.
Literature review has shown that various primary ovarian tumours metastasise to cervical lymph nodes: most are epithelial malignancies. However, SC lymph node metastases from ovarian tumours are unusual. Cervical lymph nodes can be reached by metastatic cells from ovarian cancers through the retroperitoneal and para-aortic lymph nodes. Sometimes metastases in the neck are found before the diagnosis of ovarian carcinoma; in these cases, the presence of circulating tumour cells can be very useful in identifying the primary tumour. In other cases, the time interval between diagnosis of ovarian cancer and appearance of neck metastases can be very long, up to 10 years. Nonetheless, lymphadenopathies in the neck is considered as DM and classified as stage IV. Surgical treatment of cervical lymph nodes metastases can be warranted as a salvage treatment or in order to control local disease in only a small number of cases.
Metastases to the lymph nodes of the neck are extremely rare in uterine cervix cancer as well as in endometrial cancer, while their incidence ranges from the 0.1 to 1.5% of all cases. Recently, with the improvement in the treatment of these cancers, SC adenopathy can be seen more frequently as a sign of recurrent disease; in any case there is no role for curative neck dissection in these patients.
Conclusions
Although most metastatic lymph nodes in the neck arise from a head and neck tumour, a cervical lymphadenopathy, especially if isolated and located in the left SC fossa, should alert the clinician to think about a subclavicular origin of the disease. Indeed, it is not uncommon to refer a neck adenopathy to a first manifestation of a primary unknown subclavicular tumour, mainly in otherwise asymptomatic patients. In the presence of a neck mass, when the primary tumour is not found in the head and neck region, a primary tumour below the clavicle should be therefore considered and the appropriate staging investigations initiated. Complete examination is mandatory, including panendoscopy, fine needle aspiration cytology, imaging and, if the primary remains occult, excisional biopsy of the lymph node, inclusive of immunohistochemical and molecular studies in the search for specific tumour markers. The introduction of PET CT has significantly improved the ability to identify the site of an unknown primary tumour, especially if onset in a distant location, as well as to detect the presence of DM elsewhere in the body. Once the primary tumour has been located, complete staging of the disease should be carried out.
Cervical lymph node metastases of a primary carcinoma below the clavicle is considered in most cases as a distant metastasis, representing an advanced stage of disease often associated with poor prognosis. In view of the choice of individual treatment strategies, close interdisciplinary consultation and cooperation are necessary and all factors involved in the management of the disease have to be taken into account: histology of the tumour, extent of the disease, associated comorbidities and functional status, as well as the treatment preferences of the patient.
Curative neck surgery seems to play no role in most metastatic cancers of the lungs, gastrointestinal tract and prostate.
In breast cancers, the indications for surgical therapy of SC metastases mainly depend on the histological type of the tumour, even if in these cases there is no evidence to support an indication for therapeutic neck dissection. Nevertheless, surgical therapy is warranted in selected cases of distant primaries, such as renal cell carcinomas, oesophageal cancers and testicular cancers.
The control of local symptoms to improve the quality of life can be a motivation for surgery in some cases in which it is not otherwise possible to increase survival, such as in cases of bulky tumours causing functional impairment.
8. Parenchymal metastases to the head and neck
DM in the head and neck occur very rarely and represent only about 1% of all cancers in this region. Hence, most publications in the literature are case reports and only a few papers have analysed larger cohorts.
The most common distant primary tumours with metastases in the head and neck are tumours of the lung, breast and kidney, and those of the gastrointestinal tract, liver and prostate are less common.
Oral cavity, parotid gland, orbit, thyroid and parathyroid glands, sinonasal region, larynx and temporal bone are the most frequently parenchymal structures involved.
In the recent literature, about 1,500 cases of parenchymal metastases to head and neck have been reported (Tab. 8.I).
Table 8.I.
| Lung | Breast | Kidney | Colon-rectum | Prostate | Other | Total | |
|---|---|---|---|---|---|---|---|
| Oral cavity | 118 | 129 | 79 | 53 | 29 | 110 | 518 |
| Parotid gland | 49 | 32 | 40 | 6 | 8 | 6 | 141 |
| Orbit | 6 | 57 | 2 | 1 | 4 | 7 | 77 |
| Thyroid | 110 | 64 | 127 | 63 | 9 | 60 | 433 |
| Nose and sinuses | 18 | 15 | 50 | 11 | 12 | 5 | 111 |
| Parathyroid | 7 | 85 | 4 | 3 | 1 | 6 | 106 |
| Larynx | 14 | 1 | 8 | 2 | 25 | ||
| Temporal bone | 15 | 18 | 5 | 2 | 6 | 15 | 61 |
| Other | 7 | 3 | 1 | 1 | 1 | 9 | 22 |
| Total | 344 | 404 | 308 | 148 | 70 | 220 | 1,494 |
Metastases to the head and neck region from any organ below the clavicle are not frequent and are generally associated with progressive primary disease. Occasionally, a head and neck metastasis from infraclavear tumour may be present at an early stage without showing any other signs or symptoms of the primary disease or even be the first presentation of an occult cancer.
According to Meyer and Shklar 1, in the diagnostic framework of distant metastases, four topics are fundamental:
the primary tumour must be known and histologically verified;
the metastasis must be demonstrated histologically;
both histologies must be identical;
tumour-free tissues must be located between the primary tumour and the metastasis.
Metastatic spread of malignant tumours is a biologically-complex process that occurs through embolic spread over lymph and blood vessels called “metastatic cascade”.
As metastases in the head and neck region are rare and usually occur only when multiple metastases are already present, a different pathway has been postulated.
When only hematogenous metastases are taken into account, the most common way is the portal venous system. As the incidence of accompanying lung metastases is lower than this pathway would lead to, different metastasising mechanisms have been speculated. In 1940, Batson hypothesised the role of the valve-less plexus vertebralis, which extends from the skull base to the os sacrum. An increase in intrathoracic pressure directing blood flow into this system from the caval and azygous venous system, bypassing filtration through the lungs, may account for the increased distribution of axial skeleton and head and neck metastases 2.
More recently, the detection of tumour cells from lung carcinoma in sputum has been described, so that such a pathway, expressly to the oral cavity, might also be possible 3.
8.1. Lung cancer
Lung cancer is the leading cause of all cancer-related deaths worldwide and the second most common cancer in both males and females, with a 5-year survival rate of < 15%. The disease can be broadly divided into non-small cell lung cancer (NSCLC), which account for approximately 80% of cases, and small cell lung cancer (SCLC) which represents the remaining 20% of cases.
Large cell carcinoma, lung squamous cell carcinoma and adenocarcinoma are the most common NSCLC subtypes.
Lung cancer most frequently metastasises lymphogenous to regional lymph nodes and haematogenous to parenchymal tissues.
Approximately half of patients with NSCLC present with metastatic disease at the time of diagnosis, and the predominant pattern of failure in these patients is distant metastatic spread.
The primary treatment for most patients with diffuse metastatic NSCLC is palliative chemotherapy, which results in median survival of 8-11 months and provides a minimal chance of long-term survival.
Up from 1995, Hellman and Weichselbaum proposed the existence of a state of limited systemic metastatic burden, in which eradication of OM could be curative in selected patients 4.
This state identifies patients with a controlled NSCLC primary tumour and 1 to 5 synchronous or metachronous metastases, and eligible for local ablative treatment 5.
In OM-NSCLC, curative treatment of the primary lung cancer, combined with surgical metastasectomy, radical external-beam RT or stereotactic RT/radiosurgery, represent an accepted strategy worldwide.
In a recent meta-analysis on 757 NSCLC oligometastatic patients, median OS was 26 months and OS at 1, 2 and 5 years was 70.2%, 51.1% and 29.4% respectively 6.
Surgery was the most commonly used treatment for metastases (62.3%).
Three risk groups were identified: low risk (metachronous metastases - 5-year OS 47.8%), intermediate risk (synchronous metastases and N0 disease - 5-year OS 36.2%) and high risk (synchronous metastases and N1/N2 disease - 5-year OS 13.8%).
For patients with metastatic disease, NCCN Guidelines recommend that the histologic subtype should be determined before therapy in order to select the best treatment 7.
Biomarker testing for genetic alterations (such as ALK, ROS1, PD-L1, MET) is recommended in patients with NSCLC, since targeted therapy (such as pembrolizumab, crizotinib, ceritinib, alectinib, brigatinib and osimertinib) has been shown to decrease tumour burden, decrease symptoms, and dramatically improve the quality of life for patients with specific genetic alterations (e.g. ceritinib and crizotinib for ALK or ROS1 rearrangements, anti-EGFR agents for EGFR mutations and pembrolizumab for high expression of PD-L1) 8.
CHT-IT regimens (such as pembrolizumab-pemetrexed; cisplatin-gemcitabine-necitumumab; pemetrexed-bevacizumab) are recommended for patients without genetic alterations and low expression of PD-L1 9.
8.2. Breast cancer
Breast cancer is the most common malignancy in women and accounts for a large proportion of cancer deaths.
Although the prognosis of breast cancer is generally favourable, 20-30% of patients will still develop DM with a median time between initial diagnosis and the development of the first metastasis of about 29.0 months (3-176 months) and a post-metastasis OS of about 31.0 months (0-173 months).
Histology, age and pTNM status are well known prognostic factors for metastatic spread in breast cancer; recently, according to St. Gallen recommendations 10, molecular subtypes have been identified as closely related to the different risks of early recurrence and metastasis, preferential site of distant metastases, response to treatment and OS.
Molecular subtypes of breast cancer are divided into four subtypes based on hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) status: HR+/HER2-, HR+/HER2+, HR-/HER2+ and triple negative (TN).
Bone, liver, lung and brain metastases are frequent in breast cancer. In a series of 243,896 patients, including 17,445 cases with distant metastasis, bone metastasis was found in 8,848 cases, lung metastasis in 4,167, liver metastasis in 3,434 and brain metastasis in 1,000 11.
In this large population-based cohort, breast cancer subtypes showed a strong correlation to patterns of site-specific metastasis: patients with all subtypes were most prone to bone metastases, mostly HR+ and TN subtypes; HR-/HER2+ subtype patients had a higher probability of brain metastasis; liver metastasis was more frequently observed in HER2 positive subtypes compared with HER2 negative lesions.
As suggested in other works, breast cancer molecular subtypes may be related to difference in the time of distant recurrence and in prognosis. ER- tumours are associated with early recurrence whereas ER+ are associated with a more than 5-year sustained late risk while HR+/HER2+ being the best prognostic factor and TN being the worst. Similar observation suggest that patients with bone metastases may have better survival outcomes, showing that these patients are more likely to benefit from surgery of the primary tumour 12.
Despite the relatively high prevalence of this disease, breast cancer manifestations in the head and neck are rare. Supraclavicular lymphadenopathy and bony metastases to the mandible and maxilla are the most common manifestation; secondary involvement of the oral cavity, orbital soft tissue, tonsils and larynx have been occasionally described. For patients who develop metastases after initial diagnosis of breast carcinoma, the time from primary diagnosis to head and neck metastases ranges from 1 to 33 years (mean 10.9 years) 13.
According to NCCN guidelines 14, women with recurrent or metastatic HR+ positive disease are appropriate candidates for initial endocrine therapy that includes: nonsteroidal aromatase inhibitors (anastrozole and letrozole); steroidal aromatase inhibitors (exemestane); serum ER modulators (tamoxifen or toremifene); ER down-regulators (fulvestrant); progestin; androgens (fluoxymesterone); high-dose oestrogen (ethinyl oestradiol). Recently, several new combination therapies with novel agents have become available such as exemestane with everolimus, palbociclib in combination with fulvestrant, and palbociclib with letrozole.
Women with metastatic HR- tumours or with HR+ tumours that are refractory to endocrine therapy should receive chemotherapy: a variety of chemotherapy regimens are appropriate, with single agents or combination CHT. The agents used mostly are: anthracyclines (doxorubicin, epirubicin), taxanes (paclitaxel, docetaxel and albumin-bound paclitaxel) and anti-metabolites (capecitabine and gemcitabine).
Patients with metastatic tumours that are HER2-positive may benefit from treatment withHER2-targeted therapy (pertuzumab and trastuzumab).
In addition to systemic therapies, patients with metastatic breast cancer may also benefit from local irradiation, surgery with metastasectomy, or regional chemotherapy (such as intrathecal methotrexate for brain metastasis).
8.3. Renal cell carcinoma
RCC is slowly growing, capsule-forming tumour with different histological types: clear cell renal carcinoma, poorly differentiated or undifferentiated carcinoma, nephroblastoma and small cell renal carcinoma.
Most frequently, RCC metastasise into the lung, lymph nodes, skeletal system and liver; in the majority of the cases, several sites are affected simultaneously.
Historically, the risk of metastatic RCC at presentation and during surveillance has been directly related to primary tumour size, suggesting a high risk of metastatic disease for tumours > 3 cm.
Most commonly, metastases occur in the lung, bone, or liver, and often in multiple sites. Head and neck metastases are rare, but numerous case reports and small series of metastasis of RCC into the head and neck region are available in the literature.
Metastases of RCC in the head and neck are detected in about 3% to 15% of patients; neck nodes are involved in about 60%, while parenchymal metastases affect the remaining 40%. In about 8% of patients with RCC, the head and neck metastasis is the presenting complaint, but only 1% of patients with RCC have metastasis confined only to the head and neck 15,16.
RCC is usually noted to invade the local vascular network by direct extension. If there is no evidence of lung or liver metastasis, it has been postulated that the disease can spread through Batson’s venous plexus or lymphatic spread through the thoracic duct 17.
Head and neck metastases appear simultaneously to the primary tumour or are the first manifestation of RCC in about 45% of cases, while late metastases are detected at follow-up after 24 months on average. Longer periods of detection have been occasionally described up to 90 months.
The therapy of DM of RCC to the head and neck requires close interdisciplinary cooperation. In principle, multimodal surgical, radiotherapeutic, chemotherapeutic and immunotherapeutic procedures are available.
Even if RCC is traditionally described as a radioresistant tumour, many authors have reported the effectiveness of RT in treatment of metastatic disease.
Surgery has therapeutic significance in case of a single metastasis in the head and neck region, when metastasis is the first sign of the disease or when it occurs more than two years after treatment of the primary RCC. In addition, surgical management of RCC metastases to the head and neck can also be appropriate with symptomatic intent. Review of the literature has found that excision of solitary metastatic lesions of RCC following nephrectomy results in 41% survival at 2 years and 13% survival at 5 years, regardless of the time interval between nephrectomy and diagnosis of the metastatic lesion. Depending on the site of presentation, local resection may improve the quality of life and can provide an excellent chance for cure in the head and neck 15.
Regarding systemic therapy, targeted therapy with tyrosine kinase inhibitors (sunitinib, pazopanib) and/or anti-VEGF antibodies (sorafenib, axitinib, bevacizumab) is now widely used in first- and second-line treatment of patients with metastatic disease. Agents targeting the mammalian target of rapamycin (mTOR) are also used in this setting (i.e. temsirolimus, everolimus). Immune checkpoint inhibitors are the new revolution in treatment options: recent studies have shown the efficacy of nivolumab checkpoint monotherapy in the second-line setting for patients with advanced RCC and the combination of nivolumab and ipilimumab in the first-line setting.
IFN-α and high-dose IL-2 as therapies for RCC are now used only in selected patients 18.
8.4. Oral cavity
Metastatic solid tumours to the oral cavity are rare. Metastases to the oral cavity arise from any part of the body, more frequently from tumours of epithelial origin and are frequently a secondary spread from other metastatic lesions. Nevertheless, about 25% of oral metastases have been found to be the first sign of a metastatic process 19.
Metastatic dissemination to the oral cavity is highly indicative of end-stage disease, with reported survival time after diagnosis of an oral metastasis of 3.7-8.25 months 20.
The most common primary sources of metastatic tumours to the oral region are breast in females and lung in males. Kidney, prostate, colon and stomach are other potential primary sites.
In the paediatric age, the most common primary is the adrenal gland.
Involvement of the jawbones can be considered more common than involvement of oral soft tissue.
The most common location for metastases is the mandible, with the molar and premolar regions being the most frequent involved sites. This is perhaps due to the large amount of red bone marrow and peculiar vascularisation of these sites. The post-extraction site has been described as a peculiar site for metastasis. Other secondary localisations, like the maxilla, condyle, or multiple mandibular metastases, are exceptional.
For what concerns oral soft tissue, gingiva is the most frequent involved site, followed by buccal mucosa, tongue and palatal mucosa 21.
Clinical presentation is ambiguous with symptoms like swelling, loosening of affected teeth, hypo-aesthesia or anaesthesia of the lower lip and pain.
The treatment in strictly related to the site of the primary lesion and to the degree of metastatic spread. In selected cases of jaw-only metastasis, surgical resection can be performed with palliative intent.
Prognosis is poor with important differences linked to age and metastatic locations: paediatric patients have a better prognosis compared to adults; in the literature, mean survival after metastases to the oral soft tissue is worse compared to metastases to the jaw (3.7 months vs 7 months).
8.5. Salivary glands
Salivary glands are potential sites of metastatic spread. The majority of metastases in the parotid gland arise from primary tumours of the head and neck. In 10-15% of metastases, the primary tumour is located below the clavicle. Distant primaries are, in descending order of frequency, located in the lung, kidney and breast; only rarely does the primary arise in the gastrointestinal tract or prostate 22,23.
Parotid metastasis may be the first manifestation of an unknown infraclavicular primary or, more often, expression of disseminated disease.
When parotid metastasis from RCC occurs, in the majority of the cases, metastases are the first evidence of the primary tumour, though parotid metastasis may become apparent even more than 10 years after nephrectomy.
Parotid metastasis from an infraclavicular primary are more common in older patients with a peak incidence in the 7th decade, even if there is a wide age range between 23 years and 93 years.
Clinical symptoms are usually non-specific. In most cases, a parotid swelling is present as a slowly growing painless mass; pain and cutaneous involvement may be present in late stages. Bruit and pulsation may occur in cases of highly vascular metastatic masses known to occur in RCC 24.
Facial nerve palsies in conjunction with parotid metastasis of RCC are rare.
In case of disseminated diseases with multi-organ and parotid involvement, combination strategy based on chemotherapy is recommended; parotidectomy is rarely considered with curative intent, but is potentially appropriate for symptom control in patients who are fit for surgery.
When parotid metastasis is the solitary expression of an infraclavear metastatic cancer, mostly from RCC or breast cancer, parotidectomy is indicated, both with curative and palliative intent 25.
Few cases of metastatic involvement of the submandibular gland are reported. In a recent review, Higuera et al. analysed a series of 8 cases of RCC metastatic to the submandibular gland 26. Gastrointestinal tract, breast and lung are others occasionally described primaries.
No reports of secondary localisations to the sublingual gland are present in the recent literature.
8.6. Orbital metastases
Orbital metastases of solid infraclavicular tumours are rarely diagnosed, even though pathological reports suggest an incidence of up to 25-30% in cancer patients.
The breast, lung and prostate are the most common metastatic primary tumours 1.
Ocular metastases are predominantly located in the highly vascular choroids, followed by the anterior segment, orbital structures and the optic nerve.
Orbit metastases most frequently develop in a clinical condition of disseminated disease and in only about 25% of cases are the first sign of metastatic spread.
Symptoms vary due to the affected site in the orbital region. When metastasis infiltrates the choroids, blurred vision is the predominant affection; if the anterior eye is involved, glaucoma might be present. Lid swelling and diplopia are common presentations, while exophthalmos and bulb divergence occur when large lesions are present. Loss of vision can be due to direct infiltration to the optic nerve or subsequent to a mass effect. Local pain resulting from perineural invasion has been described in patients with metastases in all orbital and ocular regions 27.
Therapy of ocular metastases is mainly local. In most patients, chemo-radiotherapy is safe and effective with objective response rates up to 80%.
Surgery is indicated in patients with intractable pain or visual loss secondary to optic nerve compression, but offers no advantage for disease control or survival.
Prognosis is currently poor.
8.7. Thyroid gland
Metastasis to the thyroid gland from distant sites is an uncommon clinical presentation, though autopsy examination suggests that as many as 24% of patients who die of non-thyroid malignancies have metastases to this gland. This is due to the rapid arterial blood flow of the thyroid, which is the second most richly arterialised organ in the body 28.
In autopsy series, the overall incidence of thyroid metastases is about 2%. The majority of metastases are clinically occult and are mostly due to lung or breast disseminated cancers.
When one considers clinically-significant thyroid metastases, RCC is the most common primary tumour 29.
In the majority of the cases, thyroid metastases are diagnosed in the setting of a known previous malignancy, and in 25% thyroid lesions is the first sign of disease.
Management of thyroid metastases depends on the individual situation.
When thyroid metastases is due to multiorgan distant spread from an aggressive tumour, radiotherapy and chemotherapy may be considered and surgery is only indicated with palliative intent.
In the case of a relatively indolent primary (such as RCC) or isolated metastasis, surgery can be curative and radical treatment has been recommended by many authors.
Mean survival after surgery for thyroid metastasis is closely linked to the features of the primary tumour. In RCC, thyroid metastasectomy for selected patients may offer good survival rates (30-50%), and long disease-free intervals.
Evidence related to surgical management of thyroid metastases from lung, breast and colorectal cancer is limited, though outcomes appear generally poor.
8.8. Parathyroid glands
Parathyroid glands are seldom site of distant metastases. In a large literature review, only 127 cases have been described from 1950 to 2017.
In about 70% of cases, breast is the primary tumour site; parathyroid gland metastases are nearly always identified as part of a widely metastatic disease with only 3% of cases reported as isolated metastases. When metastasis to parathyroid gland occurs, the most significant clinical finding is represented by deranged calcium homeostasis, probably as a result of parenchymal destruction 30.
8.9. Paranasal sinuses and nasal cavity
Paranasal sinuses and nasal cavity are rare locations for metastases. The maxillary sinus is the most frequently involved site, followed by the sphenoid, ethmoid, frontal sinus and nasal cavity.
RCC accounts for about 60% of cases, but metastases from breast, prostate and colon have been occasionally reported 31.
Metastases to the paranasal sinuses are known to be highly vascular lesions, and the most common presenting sign is epistaxis. Nasal obstruction, facial pain and orbital involvement may also be presenting symptoms.
Prognosis is usually poor because of the fact that sinonasal metastasis is usually associated with widespread disseminated disease.
The objective of treatment is to improve or maintain the quality of life.
Surgery is probably the treatment of choice for patients with single resectable sinonasal metastases. In RCC metastases, excision of a solitary metastatic lesion after nephrectomy results in 41% survival at 2 years and 13% at 5 years, regardless of the interval between nephrectomy and diagnosis of metastases. RT is considered the optimal treatment for local symptomatic control. For unresectable lesions, therapeutic strategies include CHT, IT, and RT 32.
8.10. Larynx
DM to the larynx are unusual, accounting for 0.09% to 0.40% of all laryngeal tumours. In the literature, less than 200 cases have been reported 33,34.
The supraglottis and subglottis are the most frequently involved subsites, probably because of the well-developed lymphatic and blood circulation in these sites.
Metastases may occur primarily in the mucosa or in the cartilage. Cartilage ossification is commonly considered as a prerequisite for invasion.
When mucosa is involved, RCC and colorectal carcinoma are the most probable primaries; lung, breast and prostate cancer are mostly responsible for cartilage invasion.
Prognosis for patients with a laryngeal metastasis is generally poor, since involvement of the larynx is usually observed in the terminal stage of the disease, when multiple metastases are present.
Curative treatment of secondary laryngeal tumours should be considered when no other metastases are clinically evident. When laryngeal metastasis presents in a condition of disseminated disease, palliation is indicated.
8.11. Temporal bones metastases
Temporal bone metastases (TBM) are very rare and in most cases occur late in the disease process after the primary malignancy has already metastasised to other organs 35.
The median duration from diagnosis of the primary tumour to TBM is 22.5 months with a range from 0 to 127.0 months. The median time to death after diagnosis is 3.0 months. Breast, lung and prostate are the most common infraclavear primaries involved; TBM from haematologic malignancies are seldom reported 36.
In solid tumours, TMB involves more frequently the temporal squama (23%), facial nerve (20%) and the internal auditory canal (18%); the most common otologic signs and symptoms are facial palsy and hearing loss.
Haematologic malignancies metastasise more frequently to the external auditory canal, mastoid and middle ear compared to solid cancers.
The true incidence of TMB seems to be gradually increasing because of increased cancer survival rates and development of better diagnostic techniques. In autopsy records of patients with primary non-disseminated malignant neoplasms, the prevalence of TBM is about 20%.
9. Role of radiotherapy in the treatment of metastases from head and neck cancer
HNC has a typical locoregional pattern of recurrence, with rates of 45-50%, and a lower incidence of DM, with rates less than 20%. However, in specific primary tumour sites (hypopharynx and supraglottic larynx), in advanced lymphatic cervical disease (N3) or when lower cervical nodes are involved, the incidence of DM may rise to approximately 30% 1.
A relatively favourable prognosis is related to HPV positive tumours which are characterized by high radio- and chemo-sensitivity, resulting in long-term locoregional control for > 75% of cases, but in locally advanced tumours, the survival rate is still suboptimal mainly due to distant spread.
The role of RT in managing metastatic HNC has substantially changed during the last years. In the past, RT was mostly considered as palliative treatment, because of poor prognosis, in order to palliate symptoms and improve quality of life (QoL). The introduction of the concept of OM suggested to use high dose radiation in this tumour setting, thanks to technological and clinical advances in balancing tumour control and toxicity 1. From the recent literature, besides surgical metastasectomy, local ablative treatment, such as stereotactic body radiotherapy (SBRT), may appear to be a promising alternative, obtaining comparable outcomes in terms of local control and OS 2,3.
The newly discovered synergism of high dose/fraction radiation with IT has more recently led to potentially increase the therapeutic ability to control metastatic cancer 4.
The role of RT in metastatic HNC, with special focus on settings, techniques and combination treatments, allows to achieve a potentially radical therapeutic intent.
We reviewed the PubMed and Scopus databases using the following keywords: “head and neck cancer”, “head and neck neoplasm”, “head and neck tumour”, and “metastases”, “oligometastases”, and “radiotherapy”, “stereotactic radiotherapy”, “radiosurgery”. The period of inclusion was from January 1999 to May 2019. We included reviews, retrospective and prospective observational studies, clinical trials and case reports published in English or French, expressively referring to HNC alone or together with other malignancies. Admitted articles also had to provide data on OS, local control (LoC), PFS or QoL of treated metastases. We excluded studies which did not take in account RT as a choice of treatment. We also excluded studies in which primary histology was not reported or not clearly defined.
We found a total of 152 studies referring to metastatic disease from various primaries including the head and neck. A total of 28 papers were analysed and included in the present review, specifically referring to metastatic HNC patients in different proportions (ranging from 1.7% to 100%). All metastatic sites were included, but we reported data for lung, liver, bone and brain due to their higher frequency. At least a group of patients per study underwent RT, using different techniques and schedules, alone or in combination with surgery and/or chemo-immunotherapy.
Fourteen retrospective studies and 11 reviews were included. Six of the 11 reviews reported data only from HNC treated metastases, while 5 collected data from different primaries, including HNC.
A case report showed results of brain metastases from nasopharyngeal carcinoma treated with radiosurgery.
The only article on a prospective study included in the present review reports on the trial design of a phase I/II single arm trial design planned on 35 patients with extracranial metastases from HNC 4. Patients should receive IT with durvalumab and tremelimumab until progression of disease or unacceptable toxicity, with SBRT administered between the second and the third cycle of IT. PFS is the primary endpoint evaluated, using radiological exams every 8 weeks.
Table 9.I summarises results of OS, LC, PFS and QoL of metastatic HNC treated with radiotherapy from the 14 retrospective studies 5-11.
Table 9.I.
The role of radiotherapy in metastases from head and neck malignancies: results of OS, LC, PFS and QoL.
| Author | % of HNC patients | Total of patients per study | Site of metastasis
(number of patients) |
Treatment | Results |
|---|---|---|---|---|---|
| Bates, 2018 5 | 100% | 27 | Lung (16)
Other (11) |
SABR
IMRT 50 Gy 10 Gy/fr VMAT 35 Gy 7 Gy/fr 24 CHT 2 surgery + adjuvant RT 1 surgery |
Median OS 1,9 years
OS 78% at 1 year OS 43% at 2 years DFS 27% at 1 year DFS 14% at 2 years TM-LC 75% at 1 year TM-LC 57% at 2 years |
| Bonomo, 2019 6 | 100% | 27 | Lung (27) | SBRT
Total doses ranging from 26 Gy in single fraction to 54 Gy 18 Gy/fr |
Median PFS 16 months
PFS 1 year 66,6% PFS 2 years 21,6% |
| Duprez, 2017 7 | 100% | 1022 | Lung (110)
Bone (42) Liver (24) |
IMRT 70 Gy 2 Gy/fr (T, N+) or
IMRT 69 Gy 2,16 Gy/fr (T, N+) IMRT 56 Gy 1,75 Gy/fr (neck) IMRT 66 Gy 2 Gy/fr (adjuvant setting)CHT |
Distant control rates:
88% at 1 year 84% at 2 years 80% at 5 years 79% at 10 years |
| Hauswald, 2011 8 | 100% | 127 | Lung (17)
Multiple locations (16) Bone (5) Liver (4) Brain (2) |
RT median dose 66,4 Gy (59,4-70,3)
+ CHT (5-FU or carboplatinum) |
Mean follow up time 34 months
OS 39% at 3 years OS 28% at 5 years OS 14% at 10 years Median LPFS 17 months LPFS 41% at 3 years LPFS 33% at 5 years LPFS 30% at 10 years Median DFS 11 months DFS 30% at 3 years DFS 24% at 5 years DFS 22% at 10 years |
| Park, 2019 9 | 100% | 3 | Brain (3) | SRS
12 Gy in single fraction 16 Gy in single fraction 30 Gy 10 Gy/fr |
1 case volumetric reduction
1 case virtual disappearance |
| Patel, 2017 10 | 100% | 19 | Brain (19) | Stereotactic radiosurgery:
median dose 18 Gy WBRT |
Median survival 15,8 months
LC 77.3% OS 52.9% at 1 year OS 31.7% at 2 years |
| Rambeau, 2019 11 | 100% | 65 | Lung (53)
Bone (12) Extra-cervical lymphnodes (10) Visceral (13) |
IMRT and Conformal
> 60 Gy (radical group) < 60 Gy (palliative group) |
OS:
15.5 months (radical) 22.1 months (consolidation) 13.2 (salvage) 7.5 (not performed) |
9.1. Intrathoracic metastases
Lung is the most frequent site of DM for HNC and is also the most favourable site in terms of prognosis, compared to other locations 12. Pulmonary metastases treated with SBRT showed a median PFS of about 16 months, with 1- and 2-year PFS rates of 66.6% and 21.6%, respectively 6. Furthermore, in Bonomo’s study, 23 lesions were treated only with RT, without administration of further systemic treatment: a median PFS of 10 months was reported for these patients, with 1- and 2- year PFS of 55.6% and 33.3%, respectively. In terms of local control, SBRT and surgical metastasectomy showed similar results with rates of about 85%. OS, local relapse-free and PFS at 2 years after SBRT reached 84.3%, 90% and 34.8% respectively 13.
In Norihisa’s study, 15 patients with head and neck lung metastases were treated with 4 or 5 fractions of 12 Gy. After a median follow-up of 27 months, 2-year OS and PFS were 84% and 35%, respectively 14.
According to Bates’ results, local control of metastases treated with RT was maintained at 1 year in 75% of patients and at 2 years in 57% of patients 9.
Large doses per fraction were used, depending on the position of the metastasis: usually 20 Gy for peripheral lesions and 15 Gy for central lesions with biologically effective doses (BED) > 100 Gy 15. The data show that lung metastases treated with SBRT, with delivered BED 99% > 85 Gy and BED 50% > 100 Gy, present better local control rates than those treated with lower BED values 2.
Salama et al. demonstrated a control rate of 100% in treated metastases in a cohort of patients treated with 48 Gy in three fractions, although 5 and 7 fraction schedules were also reported in the same paper (Fig. 9.1) 16.
Figure 9.1.
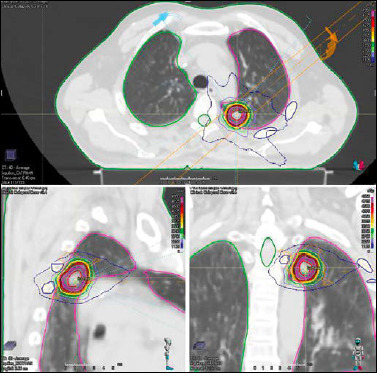
Stereotactic radiotherapy for pulmonary metastasis from oropharynx cancer (stage T4 N2c M1): total dose 45 Gy, 15 Gy/fr.
Chest pain, rib fractures, radiation-induced pneumonitis are the most frequent grade 3 toxicities occurring in less than 5% treated patients, especially those affected by central lesions 17.
The incidence of lymph node recurrence of HNC is relatively high: it can occur in 11% patients at diagnosis and in 12% after first-line chemo-radiation treatment 18. However, there are very few reports on radiotherapy for lymph node OM in HNC outside the neck. Wang et al. recently reported the results of 85 patients with 98 mediastinal lymph node OM or oligorecurrences treated with SBRT. The 1-year and 5-year LC rates were 97% and 77%, respectively. SBRT can be used in these cases with various fractionated schemes, from single doses of 24 Gy to 10 fractions of 5 Gy 19.
9.2. Liver metastases
Liver accounts for about 4% of DM from HNC (20). Despite little specific data on liver metastases from HNC treated with radiotherapy, what emerges from studies of hepatic lesions from heterogeneous origins is a median OS rate of 17-20 months and rates of local disease control ranging from 75% up to 100% and OS of 48-100% 17.
The SBRT dose is adapted to the site and volume of liver metastases, delivered in three to five sessions of 15 to 20 Gy, one session every 48 hours (Fig. 9.2) 3.
Figure 9.2.
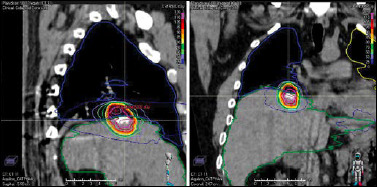
SBRT on liver metastasis: total dose 45 Gy, 15 Gy/fr.
9.3. Bone metastases
HNC has a relatively low risk of bone dissemination: the incidence varies with tumour site, ranging up to 50-80% for NPC, compared to 2-22% for other primaries 21. A Cochrane systematic review of 20 trials on 43 different radiotherapy fractionation schedules reported complete pain relief at 1 month in 395 of 1,580 (25%) patients, and at least 50% relief in 788 of 1,933 (41%). There were no differences in the proportions of patients achieving these outcomes between single or multiple fraction schedules. No difference in the dose response effect among different schedules was demonstrated: a single 8 Gy dose provided equivalent pain control to more fractionated regimens of 20-30 Gy 22 (Fig. 9.3). Stereotactic RT might improve pain and local control in patients with bone metastases compared to conventional RT with rates ranging from 80% to 90% at one year 3. A recent systematic review reported higher rates of pain response following SBRT than had previously been reported following conventional radiotherapy. Local control is excellent (80% versus 75%) with limited low-grade toxicity 23.
Figure 9.3.
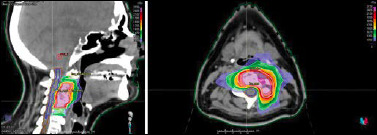
Patient affected by bone metastasis of the cervical spine (C1-C2-C4) from sinonasal cancer (stage T3 N2 M1) treated with SBRT: total dose 21 Gy, 7 Gy/fr.
SBRT might be also useful to treat spinal metastases or solitary metastatic lesions in immediate proximity to the paraspinal area. In most studies, SBRT doses were delivered in 1 to 5 fractions, often 16-20 Gy in 1 fraction, or 27 Gy in 3 fractions and the reported in-field control rate was 84-100% 24.
SBRT can also be a recommended treatment option for re-irradiation of spinal metastases. In fact, a recent systematic literature review showed a median 1-year local control rate of 76% (range 66%-90%) and improvement in pain scores ranging from 65 to 81%. Treatment delivery was safe, with vertebral body fracture rates of 12% (range 0%-22%) and radiation-induced myelopathy rates of 1.2% 25.
9.4. Brain metastases
Data from studies that take in account only brain metastases from the head and neck is limited, but the evidence is clear. Rates of LoC and 1 year-OS of 77.3% and 52.9%, respectively, were obtained after SBRT. A median OS of 15.8 months was achieved after SBRT, only 3-6 months after Whole Brain Radiation Therapy (WBRT) 10. Furthermore, as it emerges from studies comparing SBRT alone versus SBRT after WBRT, improved quality of life at 3 months and decreased neurologic damage at 3 and 12 months were observed.
Park et al. reported on brain metastases from nasopharyngeal carcinoma in 3 patients treated with stereotactic radiosurgery using different schedules (12 Gy or 16 Gy in single fractions and 30 Gy 10 Gy/fr) (Fig. 9.4). Time of appearance of metastasis from diagnosis varied from 14 to 53 months. In one case, brain-MRI performed three months after treatment showed a decrease in tumour size, and in one case complete regression of the lesion 9.
Figure 9.4.
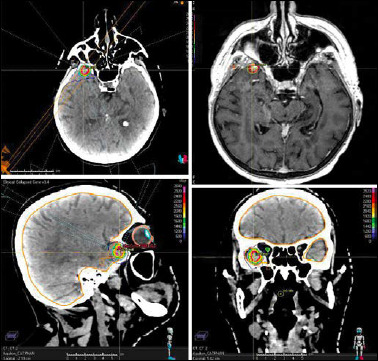
Brain metastasis in the anterior-right portion of temporal lobe treated with stereotactic radiotherapy: total dose prescription 24 Gy in a single fraction.
Discussion
Historically, the management of patients with HNC that have metastasised beyond the primary lesion has been with palliative intent. CHT based on cisplatin-5FU-cetuximab and maintenance with cetuximab until progression has been proposed as standard first-line treatment for metastatic HNC for about 30 years. This regime improves OS, but has many toxicities, such as renal failure (mostly due to cisplatin), fatigue, malnutrition, neutropenia and anaemia 26.
In addition to systemic therapy, RT has been used to reach different goals: improving locoregional control and increasing PFS in the event of stabilised metastases under CHT, or palliating locoregional symptoms.
More recently, an increase in our understanding behind the biological processes driving development of metastases has given weight to the oligometastatic theory. The term “oligometastatic” was introduced by Hellman and Weichselman in 1995 and describes a kind of distinct clinical entity, characterised by the presence of a limited number of metastatic sites (usually < 5) of disease over a long period of time 27. The concept of “oligometastatic disease” has changed over time, including biological aspects related to the disease, but also related to the choice of treatment. In this scenario, curative intent can still be considered in patients with specific features (performance status, histology, HPV status, location, primary tumour control), focusing treatment on eradication of metastases, usually by surgery or RT.
Recent technological advancements allowed for the delivery of ablative doses of radiotherapy of equivalent or higher biological doses instead of many weeks of conventionally fractionated radiotherapy. The use of multiple non-coplanar beam angles and volumetric treatment delivery with intensity modulation allow for highly conformal dose distributions on the tumour, for spare the surrounding normal tissues, minimizing side-effects and toxicities.
Retrospective studies and clinical trials have demonstrated tumour control with SBRT due to different biologic effects than those with conventional fractionation radiotherapy. It seems that high radiation doses in addition to DNA damaging events, can get through hypoxic microenvironment, thanks to apoptosis and necrosis of endothelial cells. Delivering multiple fractions of high-dose radiotherapy allow for re-oxygenation, rendering the metastatic tumour environment more susceptible to subsequent radiation induced cell death. Various dose fractionation schedules have been used in the stereotactic treatment of metastatic HNC disease. The ablative doses need to have a higher BED if compared with conventional treatments with the general consensus that a BED greater than 100 Gy Equivalent Dose in 2 Gy (EQD2) per fraction would be deemed ablative 15.
The studies analyzed in the present review were selected to investigate and summarize current knowledge about potential indications for radiotherapy in this context. What emerges from our research is the difficulty in finding results arising only from HNC primaries: articles more often report very heterogeneous study populations and even when histology of primary neoplasm is known, in some cases they are analyzed without subdivision in specific primary tumour types.
The same issue is encountered in the analysis of metastatic sites, so that unfortunately it was not always possible to calculate their proportion in relation to HNC patients. It becomes mostly noticeable in radiotherapy series on liver metastatic patients, where a mixture of primaries was included, with very limited data for liver metastases from HNC despite others.
More evidences emerge from lung metastases stereotactic treatment, suggesting that they can be treated locally with low toxicity and excellent outcomes. When considering the local treatment of metastases, a good quality of life should be a priority. To that extent, the morbidity of invasive treatments such as surgery is a critical criterion in the decision-making process. Surgical pulmonary metastasectomy can be proposed in fit and young patients with oligometastases, and to define the type of lesion. Nevertheless, surgery cannot always be performed. Hypofractionated stereotactic has the potential to ablate the tumour with control rates similar to surgery, but less invasiveness. As it emerges from Haigentz’ and Bonomo’s studies 6,13, SBRT is a safe and effective therapy to treat lung metastases. It is generally proposed for unfit patients, who cannot undergo surgical treatment because of their medical comorbidities, for the central position of the metastasis, for extensive extra-thoracic disease. The advantages of using this technique include ambulatory setting, good local control and low side effects.
Recently, new systemic therapy for the management of locally advanced/recurrent head and neck carcinomas are improving median survival so there is an increased incidence of uncommon site of metastases, such as bone or brain. The combination of poor patient prognosis and rare metastatic disease has limited identifying the optimal treatment approach for these patients 28.
In the last years, there has been a shift toward stereotactic radiosurgery (SRS) as opposed to WBRT for the treatment of limited brain metastases, reducing neurocognitive toxicity while offering similar survival outcomes. Patel et al. 10 reported that SRS for patients with brain metastases from primary head and neck malignancies, has a comparable OS and LC to previously published literature in other tumour types. Therefore, patients with well-controlled systemic disease and good performance status may benefit the most from SRS while avoiding WBRT.
Usually, bone metastases are not isolated but rather part of systemic progression of disease that includes locoregional recurrence and visceral metastases. In these patients, surgery is reserved to prevent more critical complications, like severe cortical erosion with impending risk of fractures.
EBRT with conventional technique (cEBRT) is the cornerstone of bone metastases management, which are the most frequent cause of cancer-related pain. According to literature, no dose response effect has been demonstrated between a single dose or more fractionated regimens, but studies report higher rates of pain response following SBRT than those reported following cEBRT 23.
Recent studies showed that head and neck cancer, in particular the squamous cell carcinoma histological type, is a strong immunogenic tumor, with high level of PD-L1 expression and elevated levels of intra-tumoral T-cells infiltration. As it is assumed in Bahig’s prospective clinical trial, immunotherapy agents that are able to block the interaction between PD-1 and its ligands, PD-L1 or PD-L2, can block the progression of the cell in cell replicative cycle too 29. Since RT acts by increasing intratumour T cells and by modulating the process of antigen presentation, the effects of these treatment modalities can enhance each other 4. Mediated by the immune system, the abscopal effect occurs when a single lesion treated with a targeted approach, such as radiation, results not only in local tumour regression, but also in regression in non-irradiated areas. High-dose per fraction RT induces antigen presentation within the tumour stroma, which can be used to facilitate cytotoxic T cell therapy. The preferred sequence of radiation and IT remains investigational. Based on current knowledge of cancer immunity and preclinical investigations, radiation prior to IT might be optimal, although certainly the type of immune enhancing agent may dictate the best sequencing.
Conclusions
The role of RT in managing metastases from HNC, as for other tumour types, has evolved over years: if the primary goal in the past was essentially improvement of QoL by palliating symptoms, today achieving locoregional disease control is more often expected. This has been realised thanks to introduction and evolution of the clinical concept of oligometastatic disease and to innovations in techniques, such as SBRT, which allow administration of safer and more effective treatments. One of the most promising perspectives in the treatment of metastatic HNC is related to the immunogenic effects associated with high dose radiation, which contrast the stimulation of antitumor immunity that may be boosted using specific immune therapies.
10. Chemotherapy for recurrent/metastatic head and neck cancer
10.1. Recurrent/metastatic squamous cell head and neck cancer
The prognosis of patients with recurrent/metastatic HNSCC is poor with a median survival of 6-12 months depending upon patient and disease-related factors. Systemic therapy is indicated in conjunction with best supportive care for most patients. The most important unfavourable prognostic characteristics are: poor PS (2 or more), severe weight loss, significant comorbidity, brief disease-free interval (< 3-6 months), previous no response to CHT, previous RT of the lesion, active smoking, hypercalcaemia and HPV negative disease 1.
Healthy old patients have survival comparable to younger patients, but they may experience increased toxicity. In patients with poor PS and very bulky disease best supportive care should be indicated.
The choice of systemic therapy should be individualised based on patient performance, concomitant diseases and previous systemic therapy. Treatment options include single-agent therapy and combination regimens using conventional CHT and/or target agents and/or IT.
The most widely used chemotherapeutic agents are platinoids (cisplatin-CDDP or carboplatin-CBDCA), taxanes (taxol-TAX or docetaxel-DTX or albumin-bound TAX), fluorouracil (5-FU), methotrexate (MTX); response rates to single-agent therapies range from 15% to 35%. Other chemotherapeutic agents that may possess activity but have been less extensively evaluated include etoposide, vinorelbine (VNB), gemcitabine (GEM), capecitabine and pemetrexed. The most widely used target therapy is cetuximab (CET); other less extensive evaluated target agents are: panitumumab, gefitinib, afatinib. IT with nivolumab (NIVO) or pambrolizumab (PEMBRO) has been recently introduced for treatment of recurrent HNSCC.
Combination regimens, on average, result in doubling of response rates compared with single agents. Randomised trials assessing a CDDP-based combination regimen (such as CDDP+5-FU) versus single agent chemotherapy have shown significantly higher response rates and more complete responses, but no difference in OS.
A randomised phase III trial in patients with metastatic or recurrent HNSCC found no significant difference in survival when comparing CDDP+5-FU with CDDP+TAX 2.
A phase III randomised trial (EXTREME) of 442 patients found that CET plus CDDP+5-FU or CBDCA+5-FU improved median survival compared to the standard doublet (CDDP or CBDCA+5-FU) (10.1 months vs 7.4; p = 0.04); the response rate was also improved with CET 36% vs 20% (p < 0.001) 3.
A phase II trial, conducted by GORTEC (Groupe d’Oncologie Radiothérapie Tête Et Cou), with DTX+CDDP+CET (TPEx) has shown promising results with a median OS of 14 months 4.
A phase III trial has compared 6 cycles of the EXTREME regimen versus 4 cycles of TPEx 5; 539 patients (6% HPV DNA positive patients) were randomised and after a median follow-up of 32 months no difference in median OS was observed (13.4 months vs 14.5); PFS was superimposable (6 months) as well as overall response rates (46% vs 40%). Grade 4-5 toxicity was lower in the TPEx arm (36% vs 51%; p < 0.001); Grade 3-4 neutropenia, anaemia, thrombocytopenia, magnesium disorder, oral mucositis and nausea/vomiting were significantly lower with the TPEx regimen probably for less CDDP dose intensity and for the systematic use of Granulocyte Colony-Stimulating Factor (G-CSF) in TPEx regimen (98% of patients). Patients treated with TPEx had better treatment compliance, longer CET maintenance and lower rates of switch to CBDCA. The good survival performance of EXTREME scheme is probably related to better supportive care, IT use in second-third line (20% of patients) and the high percentage (44%) of metastatic alone disease. TPEx requires fewer CHT cycles and is less toxic than the EXTREME regimen and is a new option for patients with first line recurrent HNSCC.
Other CET + CDDP regimen have shown good activity with good tolerance. In a phase II trial 6, 201 patients were randomised to first line CDDP+CET vs CDDP+TAX+CET; PFS was not statistically significant (6 vs 7 months), nor was OS (13 months vs 11) or response rate (41% vs 50.6%), while Grade 4 toxicity was lower in the two-drug versus three-drug arm (14% vs 33%; p = 0.015). CDDP+CET has very good performance and can also be proposed in patients with non-optimal performance status.
Recently, a phase III trial (Keynote 048) 7 compared the EXTREME scheme with PEMBRO alone or CDDP+FU or CBDCA+FU plus PEMBRO that was administered up to 35 total cycles. There was no difference between EXTREME regimen and the CHT+IT scheme in overall response rate (36%), median PFS (5 months) and Grade 3-5 toxicity (84%); duration of response was greater in CHT+IT respect EXTREME scheme (7 months vs 4.3 months); median OS was superior in CHT+IT in the total population (13 months vs 10,7; p = 0.004), in Combined Positive Score (CPS) > 1 (13.6 months vs 10.4; p < 0.0001) and CPS > 20% (14.7 months vs 11; p = 0.0004). PEMBRO alone obtained a lower PFS (2.3 months vs 5.2) and response rates (16% vs 36%) vs the EXTREME regimen, but the duration of the PEMBRO response was significantly longer (22.6 months vs 4.5). OS was significantly higher in the PEMBRO arm in the total population (11.5 months vs 10.7; p = 0.0199) in CPS > 1 (12.3 months vs 10.3; p = 0.086) and in CPS > 20% (14.8 months vs 10.7; p = 0.0007). Grade 3-5 toxicity was significantly lower with PEMBRO vs the EXTREME regimen (55% vs 83%). The study met most of the primary endpoints; PEMBRO alone prolonged survival over EXTREME in patients with CPS > 1 and CPS >20 and was not inferior to EXTREME in the total population. PEMBRO+CHT prolonged OS compared to EXTREME in all patients. PEMBRO alone has the concern of a lower response rate and minimal impact on PFS. PEMBRO alone is safe and in combination with CHT does not cause a major increase in toxicity. Quality of life data have not been reported.
Better biomarkers are needed to predict which patients will benefit. Keynote 048 is a practice changing study even there are many unanswered questions: which patients should get IT alone and which patients should get CHT+IT upfront?; is there a differential effect of IT based on PDL1 by CPS?; why was the response and PFS not improved?; what are predictive biomarkers for response?; is sequential treatment CHT+IT equally effective?; is there a role for targeted therapy?; what is the status of second line therapies? Based on the reported results PEMBRO for PDL1, positive tumours and combined with CDDP and FU are recommended as a first-line option; the combination regimen is a preferred option.
In second-line therapy after CDDP-based CHT, NIVO and PEMBRO have been recently approved after the evidence of improved survival compared to treatment with MTX or DTX or CET.
In the DDP-refractory setting, the single agent response rate of CET is about 12% to 14%, even if the results seem inferior in p16+ positive patients 8; mono-chemotherapy obtains a response rate of 6% with 45% showing stable disease as best response 9.
CCND1 amplification is observed in 30% of recurrent HNSCC and frequent CDNK2A mutations/deletions result in cell cycle dysregulation in HPV- cancers; in a phase II trial in CDDP pre-treated patients, the response rate was 39% with a median PFS of 5.4 months and a median OS of 9.4 months. A randomised phase 2 trial comparing CET vs CET + palbociclib failed to show a difference, probably due to the lack of selection for CDK4/CDK6 amplification 10.
Photo-immunotherapy with EGFR targeting antibody (CET) conjugated with a light (red light, 690 nm) excitable dye in 30 heavily pre-treated patients with loco-regional recurrent HNSCC obtained a 43% response rate with a PFS of 5.2 months and a median OS of 9.3 months 11.
10.2. Recurrent/metastatic nasopharyngeal cancer
NPC is a chemo-sensitive tumour and palliative CHT plays an important role in disease control and prolonging survival in the metastatic setting. Standard treatment comprises CHT with platinum doublets of drugs such as GEM, TAX and 5-FU together with CDDP/CBDCA. In first-line CDDP-based CHT, response rates are as high as 80% and a median survival of 12 to 18 months may be achieved 12. A Chinese phase III trial 13 compared the efficacy and safety of GEM plus CDDP versus 5-FU plus CDDP; the median PFS was 7.0 months in the GEM group an 5.6 months in 5-FU group (p < 0.0001). Significantly different treatment-related grade 3 or 4 adverse events between the GEM and 5-FU groups were leukopenia (29% vs 9%), neutropenia (23% vs 13%), thrombocytopenia (13% vs 2%) and mucositis (0% vs 14%). However, it should be noted that the patients were from endemic areas, where the primary NPC histological classifications are non-keratinising undifferentiated (type III) and non-keratinising differentiated (type II) diseases. For keratinising subtype (type I), which is more prevalent in Western countries, whether GEM is superior to 5-FU needs more investigation. Triplets (CBDCA+TAX+GEM) have the same outcomes of two-drug regimens.
In patients progressing after first line CDDP-based CHT, second line with 5-FU, TAX, DTX, Irinotecan Hydrochloride (CPT11), GEM, and VNB obtain response rates ranging 14% to 48% and there is no standard of care. CHT beyond 2nd and 3rd line therapy may not yield significant and meaningful prolongation of survival in the majority of patients.
PEMBRO and NIVO have been evaluated in previously treated recurrent/metastatic NPC; response rates were between 20% and 26% with 60% OS at one year.
10.3. Recurrent/metastatic malignant salivary gland tumours
Chemotherapy is employed almost exclusively with a palliative aim. Combination CHT such as CDDP+VNB or CDDP+adriamycin (ADR)+cyclophosphamide (CYC) produces response rates in the range of 40-50% and hence is worth trying in patients with aggressive or high symptom disease for early and effective palliation 14,15.
CDDP+CPT11 combination produced overall response rate of 30%. Mono-CHT (CDDP, TAX, ADR, 5-FU, CYC,VNB, mitoxantrone) produces response rates in the range of 15-20%.
ACC seems to be more chemo-resistant, with response rates of 10-15% 14. Patients with adenocarcinoma, ACC, acinic cell carcinoma (AiCC) and malignant mixed tumours are reported to be sensitive to the CDDP+ADR+CYC or 5-FU or CDDP+VNB 14,15. In patients with mucoepidermoid carcinoma (MEC) and undifferentiated tumours, however, a better response seems to be obtained with drugs that are active against HNSCC (CDDP, 5-FU, MTX). TAX is not effective in ACC; some responses have been observed in MEC and adenocarcinoma.
Gene mutations and translocations can help to select the available targeted agents for symptomatic palliation.
Larotrectinib, a specific inhibitor of the neurotrophic tropomyosin receptor kinase (NTRK) gene, commonly seen in secretory carcinoma variants, produces an overall response rate of 25% with 86% of responders continuing to benefit after a median follow-up of 9 months 16.
ACC express c-kit in 90% of cases; however, neither imatinib nor dasatinib has led to significant responses.
Her2 expression is present in 8-17% of MSGT; the frequency is as follows: salivary duct carcinoma (83%), MEC (21%), adenocarcinoma (14%), ACC (4%). In 5 patients with salivary duct carcinoma, 1 complete remission and 4 partial remissions were observed with trastuzumab+CBDCA+TAX; in 57 patients with SGM Her2 Fish positiveness 2-3+, a trastuzumab+ DTX combination obtained an overall response rate of 70.2% with a median DFS of 8.9 months and a median OS of 39.7 months. Ado-trastuzumab emtansine (TDM1) in 10 patients with HER2 overexpression obtained an overall response rate of 90% with a 50% of complete responses; survival data are immature.
Salivary duct carcinoma exclusively express androgen receptor; leuprolide plus bicalutamide obtained a response rate of 41% with a median PFS of 9 months and a median OS of 30 months 16.
11. Present and future of immunotherapy in head and neck cancer
11.1. The development of head and neck cancer (HNC) is under the control of immune system
Immune surveillance is effective in head and neck cancer. Indeed, pharmacologically induced immune suppression in patients undergoing renal transplant favours the occurrence of leukoplakia in up to 13% of patients, compared to 0.6% observed in not transplanted. The malignant transformation occurs in 10% of them 1.
Similarly, patients undergoing bone marrow transplantation show a 17.4-fold increased risk of oral cancer 2 and these tumours appear in younger people, without any known risk factor associated to HNC 3.
Therefore, the role of the immune system is indirectly confirmed by epidemiologic studies performed in specific subpopulations with weak immune reactivity.
These observations support the use of immune therapy in HNC.
11.2. Immunotherapy in HNC
Today, the only class of IT agents available in daily clinical practice are the immunocheckpoint inhibitors (ICIs).
Treatment of HNC with ICIs offers important clinical benefits leading to unexpected improvements in survival of patients with relapsed or metastatic disease (R/M-HNC).
Unfortunately, these results are less significant than in other solid tumours, such as melanoma or lung cancer.
Actually, there are major advantages in favour of IT with ICIs, but also some disadvantages.
In summary, in favour of IT there is unexpected long-term survival in a small proportion of patients with heavily pre-treated R/M-HNC and a very favourable toxicity profile compared to standard chemotherapy. It must be considered that OS in patients with R/M-HNC at second line treatment rarely exceeds 1-year 4.
On the contrary, the update of Check-Mate 141, at 2 year median follow-up 5 shows that patients treated with the anti PD-1 nivolumab in second or more advanced lines of therapy have a median OS almost twice of that of patients treated with chemotherapy or cetuximab: 8.2 months vs 4.7 months.
The two-year survival rates are 20% and 3%, respectively.
Moreover, severe adverse events have been recorded in 15% of patients treated with nivolumab, which compares favourably to 36% of patients treated with CHT.
A little known effect of IT is the high proportion of response (> 30%) to palliative CHT observed after IT failure 6.
Even if median PFS is relatively low (3-4 months), it must be considered that patients at immunotherapy failure have already received at least two lines of therapy and in many case three or more. Classically, in this population responses to further treatment are anecdotic.
However, long term survivors are rare: less than 15% of patients are still alive at 36 months 5 and more than two-thirds of the patient population dies within 1 year.
Recently, the study KEYNOTE 048 was presented both at the European Society of Medical Oncology (ESMO) 2018 annual meeting 7 and at the American Society of Clinical Oncology (ASCO) 2019 annual meeting 8.
The KEYNOTE 048 study accrued patients with R/M-HNC drug-naïve.
This is a “practice changing” study designed to compare both pembrolizumab (an anti-PD-1 monoclonal antibody) alone to the standard of care (the combination of CDDP, 5-FU and CET – EXTREME regimen), and the combination of CDDP, 5-FU and pembrolizumab to the EXTREME regimen. Pembrolizumab alone or the combination of pembrolizumab with CHT both showed highly significant improvement in OS compared to the standard of care. The magnitude of benefit was directly proportional to the level of expression of PD-L1 in tumour specimens.
Based on these positive results, the Food and Drug Administration (FDA) has recently approved pembrolizumab, either alone or in combination with cisplatin and fluorouracil for use in clinical practice. Approval from the EMA is expected soon.
Notwithstanding these excellent results, it must be taken in mind that even in the best subset of patients, those with the highest PD-L1 expression (combined positive score/CPS higher than 20), more than 60% of the population dies within 2 years.
It is underlined that it is still necessary to improve the results to achieve fully satisfactory outcomes in R/M-HNC patients.
The most important results of immunotherapy are summarised in Table 11.I.
Table 11.I.
Immunotherapy in R/M-HNC.
| Second or more line of treatment 5 | First line of treatment 7 | |||
|---|---|---|---|---|
| Nivolumab | Investigator choice therapy | Pembrolizumab | Extreme (cisplatin, fluorouracil and cetuximab) | |
| ORR | 13,3% | 5.8% | 19.1% | 34.9% |
| Median duration of response | 9.7 months | 4.0 months | 20.9 months | 4.5 months |
| Median OS (months) | 7.7
(5.7-8.8) |
5.1
(4.0-6.2) |
12.3
(10.8-14.9) |
10.3
(9.0-11.5) |
| OS at 12 months | 33.6% | 19.8% | 51% | 43.6% |
| OS at 24 months | 16.9% | 6% | 30.2% | 18.6% |
11.3. Limits of the available immunotherapies
As stated above, at present the only class of IT agents available in daily clinical practice is the ICIs, namely, monoclonal antibodies targeting the suppressive receptor CTLA-4 or the PD-1/PD-L1 axis.
CTLA-4 physiologically serves mainly as an inhibitor of the activating signalling triggered by the link of CD28 expressed by naïve T cells, with CD80 or CD86 expressed by the antigen presenting cells.
The PD-1/PD-L1 axis is an inhibitor mechanism operating mainly in the tumour microenvironment whose physiological effect is to reduce immune response to prevent tissue damage.
Tumours use this effect to escape immune attack.
Therefore, both anti-CTLA-4 and anti-PD-(L)1 represent major escape mechanisms that can be reverted by the available ICIs.
However, these mechanisms are of utmost importance only in inflamed tumours.
There are two other main categories of tumours from an immune point of view: excluded tumours and immune desert tumours 9.
Tumour “excluded” are characterised by a high density of immune cells at the margin of the tumour nests, which are not infiltrated. These tumours have a low chance to benefit from ICIs.
Immune desert tumours are characterised by the lack of immune cells infiltrating the tumour, and cannot benefit from ICIs.
Considering that expression of PD-L1 is a marker, albeit not completely reliable, of inflammation (i.e. of inflamed tumours) it explains why in most tumours, including head and neck cancer, there is a direct relationship between PD-L1 expression and response to ICIs.
To recapitulate, ICIs are not effective in all tumours: their activity depends on the microenvironment or, in other words, from the escape mechanisms predominant in each individual tumour.
11.4. Future directions of immunotherapy in head and neck cancer
Three major evasion mechanisms have been observed in HNC 10: disruption (or down-regulation) of antigen presenting machinery; development of a cancer-permissive tumour microenvironment promoting the production of immunosuppressive cytokines and exploiting immune checkpoints such as PD-L1; induction of T cell anergy through, for example, reduced response to IL-2 or down-regulation of the CD3 complex. It must be considered that many different pathways can trigger each one of these mechanisms and that these pathways may represent targets for future IT.
On the other hand, some receptors can act as stimulators of immune response such as GITR, CD40, toll-like receptors (TLRs) and many others. Even these activating or co-activating mechanisms may represent targets for IT.
In reality, many immune-compounds are under evaluation in head and neck cancer, but it is intuitive that better results will be obtained by the combination of drugs targeting different pathways and able to induce a synergic effect.
Below some examples of combination IT already in clinical trials are given.
Targeting STAT 3
STAT 3 is an important transcription factor that under chronic inflammation can trigger many mechanisms of immune suppression. The use of antisense oligonucleotides is under clinical evaluation. One oligonucleotide (AZD9150) showed positive preliminary results in combination with ICIs in R/M-HNC. The data have been presented at major oncology meetings 11.
Targeting TLR
TLRs can be target with an agonist. SD101 is an oligonucleotide targeting TLR9, and is under investigation with pembrolizumab with positive results. Motolimod is a small molecule targeting TLR8 that is under clinical investigation with CET and NIVO.
A previous randomised study comparing CDDP, 5-FU and CET plus or minus motolimod was negative 12.
This may depend on the different companion drugs used, but also by the scheduling of motolimod. Indeed, the drug was administered systemically, while SD101 and other TLRs agonists showing promising in vivo preclinical and clinical results were administered directly in the tumour.
Targeting NKG2A
NKG2A is an inhibitor receptor expressed on NK cells and by subsets of CD8+ T cells.
NKG2A links to HLA-E, a non-classical HLA class I protein highly expressed in HNC. Moreover, endothelial cells and immune cells such as M2 type tumour associated macrophages also express HLA-E.
NKG2A activation results in a strong inhibition of the antitumor activities of NK cells and CD8+ T cells.
Monalizumab is a monoclonal antibody targeting NKG2A, thus preventing its activation by HLA-E. In a phase II study in R/M-HNC presented at ESMO 2018, the combination of CET and monalizumab offered excellent response rates and good OS 13. It must be stressed that most patients treated had already failed previous CHT and CET and a previous line of treatment including ICIs.
Targeting GITR
GITR is a receptor that belongs to the TNF receptor superfamily. Its stimulation increases the CD8+/Treg ratio while improving the effector function of the former cells and dampening the inhibitory effect of the latter 14.
There are numerous compounds targeting GITR in clinical development. Among these, BMS-986156 in combination with nivolumab has shown promising clinical activity and a good toxicity profile in advanced solid tumours 15. Other clinical trials are in progress.
Targeting CD40
CD40 is a costimulatory molecule member of the TNF superfamily. It is expressed on antigen presenting cells, and non-immune cells such as epithelial, endothelial and mesenchymal cells, platelets and tumours. The link of CD40 with its ligand (CD40L) stimulates antigen presenting cells to upregulation of other costimulatory molecules such as CD80 and CD86 resulting in a more efficient priming of effector T cells.
Many agonist monoclonal antibodies are under development in combination with either pembrolizumab or NIVO in clinical trials (NCT02376699; NCT02988960). However, CD40 agonists have shown activity also as single agents 16.
Targeting the cancer permissive tumour microenvironment
Modification of the TME may also promote antitumor immune response. For example, indoleamine 2-3-dyoxigenase (IDO), an important enzyme able to catalyse the tryptophan necessary for lymphocyte activity and survival, can be targeted using small molecules such as epacadostat. Preliminary results in patients with advanced solid tumours including HNC were positive 17. Studies of epacadostat in combination with ICIs are in progress in the neoadjuvant setting (NCT03325465) and in locally advanced HNC (NCT02327078).
11.5. Immunotherapy combined with chemotherapy and/or radiotherapy
Both CHT and RT cause immune effects. Therefore, the combination with IT may benefit from this property to exploit synergistic effects. However, many immune effects of CHT and RT are linked to non-conventional dose/scheduling and require extensive studies to understand how to best combine treatments 18.
Most studies combining chemotherapy and immunotherapy to date simply add ICIs to conventional CHT regimens. This is the case in KEYNOTE 048 8 which combined pembrolizumab plus CDDP and f5-FU in R/M-HNC. Similarly, many trials are in progress adding IT to RTR in different settings (adjuvant, concurrent or adjuvant), but most just add ICIs to standard RT 19.
Conclusions
IT is changing the natural history of many solid tumours. In HNC, even if the number of patients benefiting from treatment is not as high as in other tumours, the consolidated data show the possibility of obtaining long-term disease-free survival even in heavily pretreated cases. Furthermore, the only use of IT in patients with R/M-HNC in first line of treatment offers better results of CHT and with a better toxicity profile.
Further development of IT will arise from the identification of new targets and, more importantly, from the insights on the combination of different IT agents and/or by exploiting the immune effects of CHT and RT.
Researches in the forthcoming years will further improve the benefits of IT in the management of head and neck cancer.
12. Role of surgery in oligometastatic disease
About 15% of patients affected by HNC develop distant metastases. Metastases are more frequent in advanced stages and in HPV related OPSCC 1.
Head and neck carcinoma metastases are diagnosed most frequently in the lung, with an incidence of about 65%. Other sites of DM are bone in 22%, liver in 10%, skin in 1%-2%, and brain in 0.4% 1.
After diagnosis of a primary head and neck neoplasm, there is a rapid increase of incidence of DM between months 0 and 8, and a slow increase between months 8 and 24, except cases of ACC, in which the clinical course is characterised by very late recurrences, so that follow-up should extend at least > 15 years 2.
DM to HPV-related OPSCC may occur in unexpected sites and after long intervals 3. In metastatic HPV-positive OPSCC, OM is linked with better prognosis compared to polymetastasis 4.
Aggressive interventions may be indicated for patients with limited metastatic disease with the aim to extend remission. Ablative techniques, such as surgery, RT or, radiofrequency are used to improve local control rates, survival and morbidity 5,6. As stated by Albergotti et al. 4, in oligometastatic HPV-positive OPSCC, control of metastasis with metastasectomy or SBRT should be pursued whenever feasible.
12.1. Lung metastases
Lung is by far the most frequent site of metastatic spread in HNSCC, representing about 65% of DM.
As stated by international guidelines, the treatment of DM is dependent on performance score, which can determine if systemic therapy or best supportive care is in the patients’ best interest. Currently, systemic CHT with or without molecular targeted therapy represents the standard treatment of distant metastatic disease whenever possible; in selected patients, surgery, RT, or other SABR treatments can be considered 5,6.
At present, the treatment of pulmonary metastases is linked to the concept of metastasectomy, and surgical therapy, in the absence of major contraindications, is the best therapeutic option.
Metastasectomy is the surgical procedure for secondary neoplastic disease.
In 1786, John Hunter reported the first historical case of pulmonary metastasis 7.
In 1934, Tudor Edwards described wedge resections and lobectomies for pulmonary metastases performed at the Royal Brompton Hospital in London, with excellent results in terms of survival 8. A scientific debate began on the usefulness of pulmonary metastasectomy.
In 1947, Alexander and Haight published the first case series of pulmonary metastasectomies, identifying inclusion criteria that, although modified, still remain valid today 9.
In 1991, the International Registry of Lung Metastasis (IRLM) was created, which has collected more than 5,000 cases of metastasectomies from 18 centres in North America and Europe 10.
The theoretical basis that supports surgery in pulmonary metastasis is oligometastatic disease status proposed in 1995 by Hellman and Weichselbaum 11.
This oligometastatic status makes it possible to think that local treatments, such as metastasectomy, are curative in a selected group of patients 10.
In HNC, lung is the most common metastatic site; the most frequent histotype is SCC, followed by ACC. Diagnosis of pulmonary metastasis usually occurs in oncological follow-up of patients with HNSCC 12.
The incidence of DM in patients with HNSCC varies from 4% to 26% depending on clinical stage.
In HNSCC metastases, excisional surgery is feasible according to the following criteria:
primary cancer is under control;
lung as the exclusive metastatic site;
patient in good clinical condition such to tolerate the surgical procedure;
HNSCC can be distinguished in two groups, on the basis of HPV-status.
HPV-related SCC distant metastasis does not vary significantly. Survival curve analysis demonstrate that patients undergoing lung metastasis excision of HPV-related squamous neoplasms has a 5-year OS greater than patients with non-HPV-related malignancies (11% vs 4%).
However, there is no evidence to suggest that the two groups should be treated differently. The data regarding pulmonary metastasectomy in HNSCC are extremely limited.
Pulmonary metastasectomy case series show an advantage in terms of OS at 1 and 5 years.
Depending on the cases, 5-year OS varies from 45.7% to 67% 14,15.
Young et al, in a recent systematic review, provide level IIA evidence for the effectiveness in pulmonary metastasectomy for metachronous pulmonary metastases from HNSCC, reporting an overall absolute 5-year survival rate of 29.1% in a series of 387 patients. Poor prognostic factors in this cohort include the presence of lymph node metastasis at diagnosis of original tumour, SCC of the oral cavity, incomplete pulmonary resection and the presence of multiple pulmonary nodules 16.
In a series of 77 consecutive patients who underwent metastasectomy for pulmonary metastases, Oki et al. demonstrate a 5-year OS of 54% with median OS of 66 months. In the same series, the authors identified the main poor prognostic factors in SCC, disease-free interval (DFI) < 18 months, history of recurrence before pulmonary metastases and size of pulmonary metastases > 2.5 cm 12.
In a similar retrospective study relative to 34 patients with lung metastases from primary HNC and a median DFI between primary diagnosis and metastasectomy of 40 months, Yotsukura et al. reported an overall 5-years survival rate of 57.9%, focusing on main survival predictors. In their multiple variable analysis, age > 60 years and DFI < 26 months were predictors of adverse long-term outcomes following resection of HNC lung metastases. A long DFI combined with young age suggests that pulmonary metastasectomy is a worthwhile therapeutic endeavour regardless of the primary site or number of metastatic lesions 14.
Favourable outcomes are expected for patients who have:
DFI > 18/26 months;
no other disease relapses before pulmonary metastasectomy;
age < 60 years;
lesion size < 2.5 cm.
Negative prognostic factors include:
advanced age;
male sex;
squamous histotype;
recurrent disease before pulmonary metastases;
positive lymph node status at the diagnosis of the primary;
oral cavity cancer;
multiple pulmonary nodes.
In patients with one or more negative prognostic factors, adjuvant systemic CHT should be considered 17.
Platinum-based CHT associated with an anti-EGFR monoclonal antibody, usually CET, represents the gold standard in systemic therapy.
Recent studies have demonstrated the efficacy of salvage treatments in patients who are refractory to CET with pembrolizumab and NIVO.
As with other pulmonary lesions, CT with and without contrast is the main diagnostic tool. Recent evidence has demonstrated the utility of metabolic evaluation with CT-PET in suspected metastatic lesions. According to these authors, the evaluation by CT-PET often determines a delay in the therapeutic pathway 18.
Lung metastases surgical procedures
Surgical procedures for pulmonary metastases resection include: unilateral thoracotomy, bilateral thoracotomy, axillary thoracotomy, median sternotomy, clamshell incision and video-thoracoscopy.
Patients with bilateral metastases are effectively treated with either median sternotomy or bilateral thoracotomy 10.
In fact, one specific access is not better than another: the surgeon’s experience and radicality (removing all metastases) throughout the chosen access are also determining criteria.
Median sternotomy represents a correct approach in bilateral localisations, and compared with bilateral thoracotomy has some advantages: both lungs can be examined at the same time, and iatrogenic damage to the muscles of the chest wall, nerves and parietal pleura is avoided. Furthermore, median sternotomy grants a lower number of pleural adhesions and significant advantage in case of second-look surgery.
Transverse thoracosternotomy, or clamshell incision, is mainly used for bilateral lung transplants. However, it can be a valid alternative to median sternotomy to guarantee a synchronous access, in the case of bilateral metastases.
This access route, while guaranteeing excellent exposure of the left hilum and the left lower lobe, is burdened by important postoperative thoracalgia and by difficulty in sternal reconstruction.
Posterolateral thoracotomy has the undeniable advantage of a broad view of the operative field. However, this advantage is obviously associated with the possible complications related to the size of the incision and the number of muscles and soft tissues sectioned 10.
Axillary thoracotomy was originally designed for operations on the superior sympathetic nerve. This access route is extremely rapid and has a very limited impact on the muscles of the chest wall; nevertheless, it does not guarantee the same surgical view as posterolateral thoracotomy.
Anterior thoracotomy has the advantage of being able to leave the patient supine, with a consequent minor obstacle to cardiopulmonary function compared to a lateralised position. The real indication for this access is for open lung biopsies 10.
Choice of the access route is conditioned by obtaining complete resection in surgical procedure, even in case of synchronous or delayed bilateral procedures.
Thoracoscopy or thoracotomy approach depends on the lesion distance from lung surface: specifically, lesions located in the external third of the lung are candidates for thoracoscopic resection.
Nevertheless, thoracoscopy is indicated in performing lobectomies, segmentectomies, atypical resections. Thoracoscopy must be converted into a thoracotomy when exploration fails to identify metastatic lesion visually or with mono or bidigital palpation.
Unidentified metastases can lead to the risk of metastasis to regional lymph nodes taking in account that 20% of patients with lung metastases have lymph node involvement.
Excisional thoracoscopy is indicated in lesions < 3 cm, mostly unique, unilateral, located on the surface of the lung.
VATS-friendly surgeons propose a repetition of endoscopic metastasectomy if new nodes become visible at subsequent CT and conclude that VATS is not inferior to open surgery.
Pulmonary metastasectomy takes place in a logic of parenchyma-sparing surgery.
Nevertheless, segmentectomies and lobectomies with the intent of removing a lung metastasis have been described in literature.
No data in the literature has established the efficacy of repeated pulmonary metastasectomy in patients with HNSCC lung metastasis 16.
In the presence of synchronous pulmonary and hepatic metastases, surgery is not contraindicated.
Locoregional treatments as an alternative to surgery
Few data are present in the literature about locoregional treatments as an alternative to surgery for HNSCC lung metastases.
The role of RT, and in particular of SBRT, is not yet defined.
In Bates’ experience, treatment with SBRT is effective, even with limited DFS 19.
Toxicity risks, especially in patients with central or bilateral lesions, must be carefully evaluated.
Radiofrequency ablation is an effective treatment with results comparable to surgery. This treatment can be repeated with efficacy in case of recurrent pulmonary disease 20.
Cryoablation, based on the Joule-Thomson principle can be considered a well-performing alternative. In fact, cryoablation is effective in metastatic nodule treatment using high pressure gases to freeze (argon) or vaporise (helium) lesions.
Cryoablation gives rise to ice balls, easily detected by CT as a glass opacity.
The air in the lung can interfere with the formation of these ice balls: when a cryoablation probe is inserted into a normal lung parenchyma, the onset of freezing causes the formation of a small ice ball with a diameter of only one cm because the air prevents conduction.
However, after vaporisation, the massive interalveolar haemorrhage excludes the air and allows the formation of large ice ball in the subsequent freezing phase 21.
12.2. Pulmonary metastases from thyroid cancer
Lung metastasis from thyroid cancer is related to a significant reduction in life expectancy. Pulmonary metastasectomy, in patients who are not responsive to radiometabolic therapy, is associated with an increase in 5-year survival, especially if radical resection is achieved.
A further indication for surgical resection of thyroid lung metastases is represented by the attempt in reducing overall tumour volume, in order to make radiometabolic therapy more effective.
In this case, treatment efficacy is demonstrated by a reduction in serum thyroglobulin levels 22.
12.3. Pulmonary metastases or non-small cell lung carcinoma: an upstanding question
The identification of one or more pulmonary nodules in patients with HNSCC represents a challenge in differential diagnosis between secondary and primary pulmonary neoplasia.
Both neoplasms share some risk factors, first of all, smoking status.
Imaging represents the first level of diagnostic approach 23. The number, dimensions, densitometric and volumetric characteristics, type of lesion margin, proximity to the visceral pleura, presence of satellite nodes and dimensional change at follow-up are all criteria that can support differential diagnosis, but no one is pathognomonic.
According to Ichinose and colleagues, analysis of the immunohistochemical pattern (CK19, MMP3, and PI3) of SCC can lead to the correct diagnostic definition 24.
Other authors suggest the analysis of miRNA expression to obtain a discriminating gene pattern between NSCLC and HNC 25.
Taking into account these data, preoperative histological diagnostic attempts based on these acquisitions using molecular biology is fundamental and allows to plan lung-sparing surgery in case of a metastatic lesion or an anatomical resection for a primary NSCLC.
12.4. Bone metastases
Bone metastases are not frequent in head and neck malignancies, except for nasopharyngeal undifferentiated primaries.
The standard first line treatment for bone metastases consists in stereotactic radiosurgery. Only in very selected patients may surgery be indicated 6.
Since bony lesions mostly occur at advanced stages, palliation alone is often the treatment of choice.
12.5. Liver metastases
Lung, breast and gastrointestinal cancers frequently give rise to liver metastases. In selected oligometastatic patients with limited involvement of the liver, surgical resection may be performed.
Liver is the third most common site of metastasis from head and neck cancer, with a median survival of about 4 months 5,6.
In literature reports, hepatic resection of metastatic SCC from colorectal, head and neck and oesophagus primaries is associated with overall 5-year survival rates ranging from 19% to 24% and a median time to recurrence of 9.8 to 18 months. Overall median survival after hepatic resection is 22.3 months.
Synchronous primary and metastatic disease, hepatic metastases > 5 cm and positive resection margins represent the main risk factors associated with treatment failure. Width of the surgical margin does not affect the outcome 26.
Stereotactic irradiation is increasingly used and should be considered if surgical resection appears contraindicated 27,28. Patients eligible for liver stereotactic irradiation include those with:
good liver function;
no extra-hepatic disease;
focally distributed metastases (< 5 lesions).
Higher doses of irradiation are safer for tumours < 6 cm, although larger metastases can be treated if distant from gastrointestinal structures.
12.6. Brain metastases
Brain metastases are rarely observed in HNSCC, occurring in less than 1% of all reported cases. In these cases, central nervous system (CNS) involvement is usually seen via direct invasion of the skull base or through perineural invasion 29.
The combination of poor prognosis and low incidence of brain metastases from HNSCC are the factors limiting the identification of a suitable treatment approach in these patients.
Patients treated by radiation and/or surgical resection have a median survival that is three times higher than those that who do not receive local therapy 5.
Traditionally, in cases of single limited brain metastases, in establishing a diagnosis and improving OS, surgery may be the treatment of choice. In patients with multiple brain metastases, WBRT is often utilized with the intent to improve neurologic symptoms and increase intracranial disease control.
In patients with solitary brain metastases that are surgically accessible and who have good performance status, surgery with postoperative WBRT is more effective than WBRT alone in improving survival.
Recent studies suggest that SRS can extend survival in patients with metastatic brain disease. This technique focuses high doses of radiation without exposing the remaining brain parenchyma and has been shown to be like surgery combined with WBRT in terms of survival 30.
13. Emerging strategies for treatment of metastatic disease
Cancer remains a leading cause of death worldwide. Cancer metastases are associated with poor prognosis and are responsible approximately for 90% of cancer-related deaths. For this reason, addressing metastases is nowadays one of the greatest challenges in cancer treatment. Among the various treatment options, the rapid advancement and the application of nanotechnology for biomedical field has brought many exciting and novel opportunities in the development of new anti-metastatic treatments and diagnostic strategies.
In the first part of this chapter, we briefly explain the process involved in formation of tumour metastases and list some new FDA-approved anti-metastatic drugs for clinical use, but which show some adverse reactions. Next, we focus on innovative biomimetic three-dimensional tumour/metastasis models developed for personalised pre-clinical research and helping to accelerate clinical translation of therapeutic drugs. The last part of the chapter is focused on innovative strategies in pharmaceutical products and, in particular, summarises existing nanotechnology-based approaches in clinical trials for the treatment of tumour metastases, which mainly include nanomedicine-based therapies, diagnostic solutions and their synergic theranostic potential.
All these aspects presented aim to the better understanding of metastatic pathways and spread in order to quickly achieve advanced treatments that are useful to eradicate the disease.
13.1. Metastatic spread and current treatments
The metastatic spread from the primary tumour site to distant organs is a complex and multifaceted process that involves cancer cells. Moreover, due to the complexity of the biological processes in each individual cancer patient, it is hard to predict the exact location for formation of a neo-metastasis.
The main steps implicated in malignant cell dissemination and growth are invasion, extravasation, escape from the host immune response system and angiogenesis 1. Cancer cells are able to travel from the primary site to different regions of the body through the circulatory system, to then extravasate through tissue into the extra cellular matrix (ECM). Cells are helped by MMPs and integrin expression to translocate into the final site where they metastasise. Cancer cells that arrive in the blood circulation system are defined as circulating tumour cells (CTCs); these cells are carried throughout the body, evade recognition by the cells of the immune system and can extravasate in different organs to colonise tissue and form a metastasis (second tumour site). Metastatic growth needs to be supported by nutrients and oxygen, and neo-angiogenic processes are activated through synthesis and secretion of pro-angiogenic molecules that are able to induce capillary network formation by host endothelial cells and bring nourishment to the new tumour 2.
Metastatic cancers are currently treated in the clinic by surgery, RT, IT and CHT. The pharmaceutical industry in the last few years has developed new anti-metastatic drugs that are able to selectively block and target signalling pathways involved in formation and growth of metastases. Table 13.I shows some examples and mechanisms of action (MOA) of the most recent drugs approved by FDA for treatment of cancer metastases.
Table 13.I.
FDA-approved anti-metastatic drugs reported with own mechanism of action and specific anti- metastasis application.
| Commercial name | Drug | Mechanism of action (MOA) | Application | FDA-approval year |
|---|---|---|---|---|
| Lonsurf
(Taiho Pharmaceutical Co., Ltd) |
Trifluridine/Tipiracil | Inhibits DNA synthesis and further cellular proliferation | Metastatic gastric or gastro-oesophageal junction (GEJ) adenocarcinoma | 2019 |
| Keytruda (Merck) | Pembrolizumab | Binds to the PD-1 receptor, blocking both immune-suppressing ligands, PDL1 and PDL2, from interacting with PD-1 to help restore T-cell response and immune response | Previously treated metastatic small cell lung cancer and recurrent oesophageal cancer with PD-L1 expressing tumours; metastatic or unresectable recurrent HNSCC | 2019 |
| Rozlytrek (Roche) | Entrectinib | Block ROS-1 and NTRK kinase activity inducing death of cancer cell | ROS1-positive, metastatic NSCLC | 2019 |
| Lorbrena (Pfizer) | Lorlatinib | ALK-tyrosine kinase inhibitor (TKI) | ALK-positive metastatic non-small cell lung cancer | 2018 |
| Vizimpro (Pfizer) | Dacomtinib | EGFR kinase inhibitor | Metastatic NSCLC | 2018 |
| Alunbrig
(Ariad Pharmaceuticals) |
Brigatinib | ALK/IGF-1R/FLT-3 TKI | Advanced ALK-positive metastatic non-small cell lung cancer | 2017 |
| Opdivo
(Bristol-Myers Squibb) |
Nivolumab | Binds to the PD-1 receptor, blocking both immune-suppressing ligands, PDL1 and PDL2, from interacting with PD-1 to help restore T-cell response and immune response | Recurrent or metastatic HNSCC | 2017 |
In parallel, there are already some FDA-approved anticancer drugs currently under testing in clinical trials to verify their additional activity in treatment of metastases; the most used classes of drugs belong to small-molecule receptor tyrosine kinase inhibitors (RTKIs) and small-molecule nonreceptor tyrosine kinase inhibitors (NRTKIs). Insight on these latter two MOA are summarised below:
RTKIs: these molecules lock receptor tyrosine kinases (RTKs) with a competitive mechanism. The most important RTKs are vascular endothelial growth factor receptor (VEGFR), EGFR and platelet-derived growth factor receptor (PDGFR), which are unregulated in cancer cells and are involved in angiogenesis, proliferation, migration and cells survival 3.
Cetuximab (Erbitux®): is a chimeric monoclonal antibody used in clinical application for metastatic or recurrent HNC and currently also in clinical trials for the treatment of recurrent/metastatic SCC of the head and neck (Phase II, EMR200068-006) and metastatic skin SCC (Phase II, NCT03944941) 4.
Erlotinib (Tarceva®): approved in 2005 by FDA for the treatment of metastatic pancreatic cancer is also used for locally advanced or metastatic NSCLC and is under clinical trials for metastatic HNSCC (Phase III, NCT01856478) 5.
Sorafenib (Phase II, NCT00390325) and Vandetanib (Phase III, NCT00410761): are under investigation for their activity against metastatic medullary thyroid cancer.
NRTKIs: cytoplasmic non-receptor protein tyrosine kinases (NRTKs) are enzymes involved in fundamental cellular functions, but are upregulated during carcinogenesis 6.
Cabozantinib (Cabometyx®) and Alectinib (Alecensa®): are in clinical trials for the treatment of metastatic, radioactive iodine-resistant thyroid cancer (Phase III, NCT03690388) and advanced or metastatic NSCLC ALK positive (Phase II, NCT01801111), respectively.
Unfortunately, patients with cancer recurrence and/or metastatic spread do not usually respond well to currently-approved treatments due to cancer severity or therapy resistance.
Moreover, anti-metastatic drugs used in the clinic are correlated with serious and severe side effects (nausea, vomiting, alopecia, anaemia, lowering immune defences, etc.) that negatively affect the patient’s quality of life. These adverse reactions can be associated with the drug’s formulation (poor water solubility, non-specific distribution, severe toxicity to normal cells, inadequate drug concentrations at tumours or cancerous cells) 7.
Regarding the poor effectiveness of chemotherapeutic drugs, the main reason why metastases are invulnerable and resistant to common anti-cancer drugs is largely due to mutation of a subpopulation of metastatic cells in which gene expression, growth properties, surface and protein functions have been modified compared to cells of the primary tumour. These unpredictable mutations make metastases more difficult to treat and completely different from the original tumour, and for these reasons they cannot be treated in the same way. This provided insight on three types of chemotherapy resistance: kinetic, biochemical and pharmacologic.
Kinetic resistance is correlated with tumour growth factors and the plateau growth phase; metastatic growth rate is specific and variable depending on the type of metastasis. Biochemical resistance derives from tumour inability to convert the drug to its active form due to a decrease drug uptake, increase efflux, change the levels or structure of the intracellular target, reduce intracellular activation, increase inactivation of the drug, or increase the rate of DNA repair damage. Pharmacologic resistance is related to poor tumour blood supply, poor or erratic drug absorption, increased excretion or catabolism, and poor transport of agents into diseased tissues and tumour cells 8. Taking in consideration all the limitations mentioned above, the discovery, optimisation and validation of new anti-metastatic drugs has been slow due to several challenging factors that can be summarised as follow:
adoption of validated preclinical models that reflect the pathogenesis of metastatic disease in patients;
identification of end points that reflect the prevention of metastatic disease;
costs of trials with large cohorts and long follow-up durations are prohibitive;
consider that active drugs are likely to be required by the patient years in advance of the appearance of the metastatic event 9.
13.2. Innovative strategies: from pre-clinical to translation in the clinic
The pharmaceutical industry and research are cooperating to develop novel therapeutic strategies and agents that are able to prevent the establishment of tissue colonisation by metastases and overcome drug resistance and adverse effects. The two main challenges to face are: 1) development of more predictive pre-clinical models to replicate pathological conditions in vitro and accelerate drug screening; 2) production of targeted-drugs that are able to selectively attack malignant cells and avoid adverse reactions.
A concrete help has been given by Cancer Research UK (CRUK), Cancer Research Technology (CRT) and Cancer Therapeutics CRC Australia (CTx) which formed a Metastasis Working Group with representatives from academia, industry, government and regulatory bodies to assist cancer drug discovery and development of models to facilitate clinical testing of therapeutic agents for treatment of metastatic disease 9.
Regarding the first topic, novel three-dimensional models able to mimic diseased environment are under investigation in research projects. Due to the complexity of the process for anti-metastasis drug development and consequently translation in clinical trials, some general considerations have to take into account: starting from target identification, a model able to reflect human metastatic disease and mimic clinical conditions is important in preclinical research. The output of preclinical development must provide information on drug activity, risk-benefit relationship, pharmacokinetic (PK) profile and define pharmacodynamic (PD) markers that are suitable for translation into the clinic.
For the second point, one strategy adopted to reduce toxic side effects, overcome the problem of drug resistance and improve selective treatment efficacy against neoplastic cells is the application of nanomedicine(s) in the oncology field. Nanomedicine development takes advantages of innovative nanotechnology systems to detect, prevent and treat diseases with the goal to optimise drug distribution, obtain specific activity at the target site, remotely deliver agents under imaging guidance and locally release drugs on demand 1.
The final goal is to get innovative solutions focused on personalised medicine as an “emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, lifestyle and the response to a specific treatment for each person.” This approach put the basis for an improvement in the therapeutic result and at the same time brings benefits into clinical use for patients (improved treatment efficacy, survival and reduced adverse events, and thus improved safety), but also for healthcare systems and society (prevention and prediction of disease, improvement in patient management, reduced hospitalisation and costs of care) 10,11.
13.3. 3D-Metastasis models in the pre-clinical phase
Due to the increasing number of patients suffering from cancers and correlated metastasis disease worldwide and the ever-greater variability of neoplastic cells profiles, it is extremely necessary to develop active drugs in a timely and economic manner. Drug discovery is an extremely complex process. One of the main challenges to face is to predict the effect of the drug before it is tested in a clinical study. Current preclinical models for drug screening are largely based on animal models or simple 2D cell cultures. However, these methods often prove to be limiting or unable to simulate the microenvironment of the original tumours and metastatic spread, so that the model does not reproduce many of the key parameters involved in metastasis formation, with high costs, slow timing and ethical issues. Some of the effects of medicines are indeed difficult to predict on animal models, and cell cultures are limited by the lack of biological functionality. Scientists and the pharmaceutical industry therefore felt the need to resort to innovative strategies that could overcome these limitations 12.
Innovation in manufacturing technologies on micro- and nanoscales allows to develop three-dimensional devices with the purpose to mimic in vitro the characteristics of human organs. These devices have the ability to: 1) avoid certain drawbacks of 2D-cultures; 2) closely mimic the physiologic pathways of the tumour and cancer metastases; 3) replicate the key parameters that affect tumour progression (e.g., oxygen tension, nutrient gradients, and tissue stiffness); 4) provide the flexibility to decouple these parameters in experimental settings; 5) allow a clear understanding of the results; 6) provide a validated and fast drug screening platform 13.
At the moment these 3D-models are only used in pre-clinical research and need to be optimized and validated for approval by institutions for use as in vivo comparative models.
One representative example of a biomimetic 3D model is represented by miniaturised organs also called “organoids”. Organoids are 3D multicellular clusters of living cells cultured in non-adherent conditions recapitulating the architectures and distinctive functions of a specific organ (Fig. 13.1A) 14.
Figure 13.1.
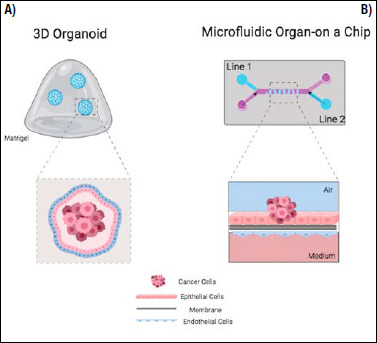
(A) 3D cancer organoid model; (B) microfluidic organ-on-a-chip cancer model (created with biorender.com).
Organoid structure is obtained using multiple cell types such as embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), fibroblasts, endothelial cells and cancer cells (they may obtained directly from patients), assembled in order to give a 3D culture system with specifically selected functions. The cellular complex is then embedded in Matrigel, a gelatinous protein mixture able to mimic extracellular matrix (ECM) and maintain non-adherent organoids in a 3D environment 15.
Promising organoid models are under investigation for drug screening, translational and clinical cancer research and personalised medicine to better predict drug responses and guide optimised treatment strategies for the individual patient 16. Some examples reported in literature show the promising properties of organoids for the study of metastasis formation, spread and pharmacologic treatment.
Vlachogiannis et al. developed patient-derived organoids (PDOs) from 110 metastatic tumour samples from 71 patients with colorectal or gastro-oesophageal cancer enrolled in phase I/II clinical trials. The PDOs showed phenotypic and genotypic profiling similar to that of the original tumours and same gene-mutation spectrum 17.
Ramamoorthy et al. developed a functional multi-cellular lung organoid lung-in-a-dish (PLiD), to recreate metastatic disease using primary and established cancer cells. This metastatic tumour-in-a-dish” (mTiD) platform was used to test the therapeutic efficacy of several standard chemotherapeutic agents and an anti-VEGF antibody 18. Other examples of organoids mimicking metastatic disease, used for drug screening and genetic pathway identification, are reported (Tab. 13.II).
Table 13.II.
Examples of 3D organoids and microfluidic organ-on a chip models reported in literature.
| 3D Organoids | |||
| Biomimetic model | Application | Target | Ref. |
| CRC organoids | Markers and genes identification. Response to drug therapy quantification |
Colorectal cancer (CRC) liver metastasis | 25 |
| Patient-derived organoids | Comparison of the genomic profiles | Metastatic breast cancer | 26 |
| Patient-derived organoids | Predict in vivo drug sensitivity | Head and neck squamous cell carcinoma (HNSCC) | 27 |
| Organoids from primary tumor tissue | Metabolic imaging | Recurrent/metastatic head and neck cancer | 28 |
| Microfluidic “organs-on-a-chip” | |||
| Biomimetic model | Application | Target | Ref. |
| 4 layers microfluidic model | Organ-specific metastasis of circulating tumour cells (CTC) | Breast and salivary gland cancer cells driving lung metastasis | 29 |
| 3 PDMS layer + 2 microporous membranes | Mimics the in vivo microenvironment of cancer metastasis and investigates cell-cell interactions during metastasis | Lung cancer metastasis | 19 |
| 2 interconnected microfluidic channels assay | Evaluates mechanisms and microenvironment factors promoting tumour high invasive potential | HT1080 fibrosarcoma cells and Human microvascolature endothelial cells treated with Tumour necrosis factor (TNF) | 30 |
| Vascular channel microfluidic devices | Transendothelial migration of highly metastatic breast cancer cells and to monitor their behaviour within the bone-like matrix | Human breast cancer metastases to bone | 31 |
| Perfusable 3D microvascular network | Influence of microenviromental factors (integrins, ECM components, cytokines) on cell extravasation across endothelium vessels | Bone-mimicking and muscle-mimicking environments perfused with media containing metastatic breast cancer | 22 |
| 2 layer PDMS microfluidic device | Trans-endothelial invasion of tumour aggregates in real time | Salivary gland adenoid cystic carcinoma (ACC) cell aggregates | 32 |
Another representative example of a biomimetic 3D model is the engineered “organs-on-a-chip” (OOC) that is able to recapitulate single organ function and tumour aetiology, as well as tissue-tissue interfaces and complex function between organ and distant organs in metastasis dissemination 19. OOCs are microfluidic cell culture devices that are able to replicate miniature tissues and organs grown in vitro that enable modelling of human physiology and disease. OOCs are composed of optically clear plastic, glass or flexible polymers, such as the biocompatible polydimethylsiloxane (PDMS). Microfluidic technology allows manipulation of small volumes of fluids (10−9 to 10−18 L) using interconnected channels with dimensions ranging from tens to hundreds of micrometres; these reduced dimensions permit a laminar flow that cannot be reached in macroscale devices 20.
OOCs perfused hollow microchannels are populated by living cells that recapitulate in vivo organ-level physiology and pathophysiology by recreating tissue-level and organ-level structures and functions (Fig. 13.1B) 21.
Microfluidic models allow the study of cancer metastatic processes under biochemically and biophysically controlled 3D microenvironments coupled with high-resolution real-time imaging 22. Some microfluidic models have been realised by focusing on specific steps in the metastatic cascade, including tumour intravasation, extravasation and neovascularisation 13.
Liu et al. developed a MNO2 nanofiber-integrated microfluidic microchip for capture and release of circulating cancer cells under controlled dynamic conditions. Other examples reported the fabrication of HA-functionalised PLGA nanofibrous mat embedded within a microfluidic chamber for CD44 receptor positive cancer cell capture and culture. These examples of combined hybrid systems for cancer cell capture show promising results for future use in early and efficient diagnosis and detection of metastatic dissemination 23.
Table 13.II reports some examples of microfluidic models used to study metastasis progression and spread in distant organs. These models could be useful in the pre-clinical phase as well as in in vitro pre-metastatic organ platforms to validate and screen the PK-PD of anti-metastatic drugs and speed-up their study in clinical trials 24.
13.4. Nanomedicine for metastasis treatment in clinical trials
Nanotechnology-development of medicinal products into nanomedicines, takes advantage of the use of nanomaterials (NMs), defined by the EU commission as: “A natural, incidental or manufactured material containing particles, in an unbound state or as an aggregate or as an agglomerate and where, for 50% or more of the particles in the number size distribution, one or more external dimensions is in the size range 1 nm - 100 nm” 33.
Nanomaterials, which can be manipulated to obtain different nanostructures such as nanoparticles (NPs), nanofibers and nanogels, have several advantages like a high surface area-to-volume ratio, adjustable porosity rate and completely different physiochemical properties (degradation rate, stiffness, reactive group, toxicity, and others) than the same bulk materials. Moreover, these nanostructures can be prepared using different kinds of organic/inorganic or naturals/synthetic materials taking advantage of the main properties of each category.
In particular, nanomaterials have been used to design and develop targeted drug delivery system (TDDS), which might safely deliver therapeutic drugs to diseased sites or specific selected cells.
TDDS offers many potential benefits such as:
avoiding the unwanted side effects of traditional clinical formulations thanks to improved drug solubility;
protecting the entrapped therapeutic drug from degradation and prolonging the circulating time;
modifying the PK and tissue distribution profile to increase drug distribution in selective tissue/organ;
reducing distribution, uptake and toxicity to off-target tissues;
increasing cellular uptake and internalisation in cells.
In the anti-neoplastic field, compared to conventional chemotherapeutics drugs, nanomedicines exhibit several outstanding advantages: 1) the enhanced permeability and retention (EPR) effect in promoting passive tumour targeting due to increased vascular permeability at the tumour site 34; 2) the easy surface modification for active tumour targeting taking advantage of ligand-receptor affinity mechanism by conjugating selective targeting molecules; 3) the controllable and responsive drug release at the target site by coating sensitive molecules on the nano-carrier surface; 4) the morphological and structural tuneable properties at a nanoscale to improve endocytosis mechanism and controlled drug-release kinetics; 5) the integration of nano-carriers with various drug molecules and imaging agents for multi-drug therapy and nano-theranostics purposes 35.
In addition to all these advantages, novel nanomedicine-based medicinal solutions, by offering flexible and fast drug design and production based on genetic profiles of the tumour and metastasis, allow the development of new nano-carried drug therapies for the construction of personalised treatments that are much more rational and effective than those used currently.
A correct nanostructure design is necessary for their efficient targeting and to achieve suitable and simultaneous activity against malignant cells; by optimising nanostructure parameters such as size, shape, surface charge, architecture and surface functionalisation, it is possible to drive and control the accumulation, uptake, pharmacokinetic, biodistribution and degradation rate of the nanomaterial in question with the final goal to destroy malignant cells 36.
Figure 13.2 summarises the features of nanostructures that can be adapt and result in biological activity.
Figure 13.2.
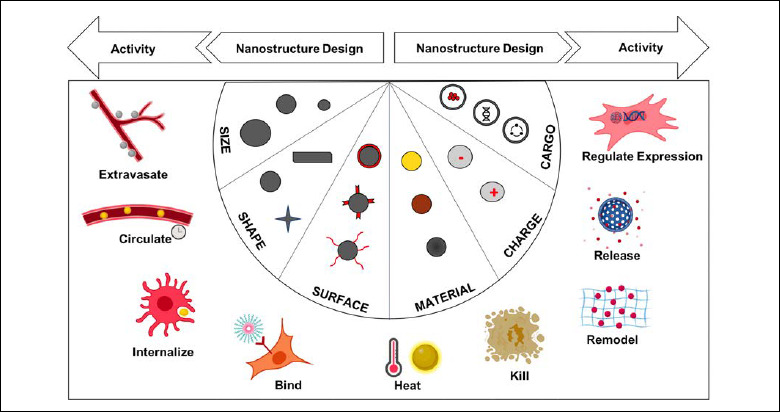
Nanostrucuture classification depending on material composition with specific description and, respectively, pros and cons in the nanomedicine field.
As some practical examples, for instance on the importance of nanostructure dimensions, it was established that the uptake of spherical gold nanoparticles with diameters of about 50 nm was higher than that of particles whose diameter was lower (14 nm) or higher (74 nm). Regarding the shape, comparing different shapes of gold nanoparticles (spherical, rod, wire, hollow) different cellular up-take by endothelial cells was observed and uptake of spherical NPs was preferred 37. A poly(ethylene glycol) (PEG) nanostructure surface is usually preferred in order to prolong circulating time, minimise incorrect adsorption by opsonin and decrease immunogenicity 38.
Electrospun nanofibres, due to their characteristic architecture that can mimic natural ECM and have extremely large specific area, are used as an ideal filter platform for applications involving capture of circulating tumour cells (CTCs). Accurate detection of these cells in peripheral blood has a large impact on early diagnosis, the prediction of cancer development, and the evaluation of efficacy, prognosis and individualised treatment of tumours. Inorganic and organic nanofibers functionalised with different molecules have been developed for cancer cell capture in static and dynamic conditions 23.
Furthermore, selection of the administration route (IV or intratumor) can influence the biodistribution and toxicity of nano-structures; Xie et al. reported that intratumoural administration is preferred over systemic administration due to a higher intratumoural retention effect and low concentration in other tissues. Moreover, the study showed that 10 min after systemic injection approximately 50% of nanoparticles are accumulated outside the site of interest, especially in reticuloendothelial system (RES) or mononuclear phagocytic system (MPS); for this reason, in the case of superficial tumours, intra-tumour administration is preferred 39.
Another large potential for the use of nanotechnology in anti-neoplastic treatment is the possibility to combine both diagnostic and treatment into a multifunctional approach, also called theranostics. This new field of research attempts not only to improve the detection and increase the efficacy of cancer treatment by reducing systemic toxicity, but also provide a rapid review of the outcome and immediate feedback of the treatment applied.
Studies on the theranostic activity of nanostructures are currently in preclinical evaluation for treatment of metastases. Chen et al. demonstrated that multimodal imaging guided photothermal therapy can inhibit tumour metastasis after surgery by burning the sentinel lymph nodes (SLNs) with metastatic tumour cells. They used IR825 dye and formed a HSA-Gd-IR825 nanocomplex exhibiting strong fluorescence together with high near-infrared (NIR) absorbance. After NIR laser exposure, metastatic cancer cell photothermal ablation was obtained and detected at the same time by MRI 40.
An innovative theranostic nanoparticle platform composed of a near-infrared (NIR) fluorescent polymer loaded with siRNA was developed for imaging-guided siRNA delivery to metastatic anaplastic thyroid cancer. Polymeric nanoparticles with a dimension of 50 nm showed long blood circulation time and high tumour accumulation, allowing for non-invasive NIR-diagnosis. Preliminary results showed that they efficiently silenced the expression of V-Raf murine sarcoma viral oncogene homolog B (BRAF) in tumour tissues and significantly suppressed tumour growth and metastasis in an orthotopic mouse model of ATC (metastatic anaplastic thyroid cancer) 41.
The advantages of theranostic products (saving time, reduction of treatment cost, targeted bifunctional action, less invasive procedures) are promising for their future translation into routine clinical use.
Table 13.III reports specific case studies that used nanotechnology strategies for the diagnosis and treatment of metastases. Currently, these nano-drugs are in clinical trials and PK, PD and toxicity results obtained from in vivo studies will be needful for future validation and approval for clinical use.
Table 13.III.
NPs in clinical trials for applications in metastasis diagnosis, therapy and theranostics.
| Nano-system | Active compound | Administration route | Application in clinical trials | Activity time | Primary purpose |
|---|---|---|---|---|---|
| CNPs | - | Injection | Predicting lymph node metastasis (phase I, NCT03632746) | 2018 | Diagnosis |
| PEG-Si-Cornell dots | cRGDY | IV | Mapping of nodal metastases;
intraoperative sentinel lymph node mapping (phase II, NCT02106598) |
2014-2019 | Diagnosis |
| Combidex® | - | MRI | Lymph node imaging (phase II, NCT00416455);
approved in some European countries - application withdrawn from EMA (Sinerem 2007)/ application withdrawn from FDA (2005) |
2015-2018 | Diagnosis |
| NAB | PTX/GCT | - | Circulating tumor cells as a potential biomarker for metastatic pancreatic cancer;
treatment monitoring (phase II, NCT02707159) |
2016 | Diagnosis |
| USPIO | Ferumoxytol | MRI | Metastatic medullary thyroid cancer follicular thyroid cancer lymph node metastasis (NCT01927887) | 2013-2017 | Diagnosis |
| ABI-007 | PTX | Infusion | Metastasis (phase II, NCT00046514) | 2002-2016 | Therapy |
| Alu gel | 3H1 | Colorectal cancer metastatic to the liver (phase II, NCT00033748) | 2016 | Therapy | |
| Abraxane albumin-stabilized nanoparticle formulation | PTX | Topical | Recurrent breast cancer;
skin metastases (phase II, NCT00821964) |
2009-2018 | Therapy |
| AuroLase® | - | - | Refractory and/or recurrent tumors for head and neck cancer (NCT00848042);
treatment of primary and/or metastatic lung tumours (NCT01679470) |
2009-2017;
2012-2016 |
Therapy |
| BIND-014 | DTX | Injectable Suspension | Advanced solid tumour cancers and metastatic cancer (phase I, NCT01300533) | 2011-2016 | Therapy |
| CriPec® | DTX | IV | Metastatic cancer (phase I, NCT02442531) | 2015-2018 | Therapy |
| LCP-AA | HIF1α siRNA | PDT | SCC4 and SAS cell lines (derived from a squamous carcinoma of human tongue with expression of sigma receptors) | - | Therapy |
| LEP-ETU | PTX | Injection | Metastatic breast cancer (phase IV, NCT02996214) | 2016 | Therapy |
| NAB (nanoparticle albumin-bound) | PTX | IV | Metastatic pancreatic cancer (phase II, NCT03697239);
metastatic thyroid gland carcinoma (phase II, NCT03181100); head and neck squamous cell carcinoma (phase I, NCT02495896) |
2018-2019;
2017-2019; 2015-2018 |
Therapy |
| NBTXR3 | Hafnium oxide | Radiotherapy | Recurrent Head and neck cancer (phase II, NCT03589339) | 2018 | Therapy |
| NC-6004 | CDDP | IV | Recurrent and/or metastatic squamous cell carcinoma of the head and neck (phase I, NCT02817113) | 2016 | Therapy |
| Polymeric Micelles (PM) | Docetaxel | IV | Oesophageal squamous cell carcinoma (SCC) metastatic (phase II, NCT03585673) | 2018 | Therapy |
| Promitil | Mytomycin-C | IV with EBR | Metastatic disease (phase I, NCT03823989) | 2019 | Therapy |
| SGT-53 | p53 | IV | Metastatic pancreatic cancer and recurrent glioblastoma (phase II, NCT02340156) | 2015-2017 | Therapy |
| SOR007 | PTX | Topical ointment | Non-melanoma cutaneous metastases (phase II, NCT03101358) | 2017-2019 | Therapy |
| ThermoDox | DOX | Injection with RFA | Metastatic tumour of liver (phase I, NCT00441376) | 2007-2019 | Therapy |
| TKM-080301 | siRNA directed against human PLK1 mRNA | Injection | Colorectal cancer with hepatic metastases (phase I, NCT01437007) | 2011-2018 | Therapy |
| CALAA-01 | siRNA | IV | Inhibit tumour/metastasis growth and/or reduce tumour size (phase I, NCT00689065) | 2008-2013 | Therapy |
| 177Lu-PSMA617 | Lu177 | Radionuclide therapy | Progressive metastatic castration resistant prostate cancer (phase II, NCT03392428) | 2018 | Theranostic |
177Lu-PSMA617: prostate-specific membrane antigen (PSMA)-targeted radioligand therapy (PRLT) using 177Lu (isotopos of lutetium); 3H1: monoclonal antibody anti-idiotype vaccine; ABI-007: albumin-stabilised nanoparticle formulation of paclitaxel; ALU: specific DNA sequence; AuroLase®: silica-gold nanoshells coated with (poly) ethylene glycol (PEG); BIND-014: PSMA-targeted polymeric nanoparticles; CALAA-01: targeted nanocomplex that contains anti-R2 siRNA; Cis-Pt: cisplatin; CNPs: carbon nanoparticles; Combidex®: ferumoxtran-10; cRGDY: cyclo-[Arg-Gly-Asp-Tyr] peptides; DOX: doxorubicin; DTX: docetaxel; EBR: external beam radiotherapy; LCP-AA: anisamide-targeted lipid-calcium-phosphate; LEP-ETU: liposomal encapsulated paclitaxel; MRI: magnetic resonance imaging; NAB: nanoparticle albumin-bound; NBTXR3: first-in-class of radioenhancer hafnium oxide nanoparticle; NC-6004: nanocarrier has prepared micellar nanoparticles containing cisplatin derivatives; PDT: photosan-based photodynamic therapy; PEG-Si-Cornell dots: silica nanoparticles with a NIR fluorophore, PEG coating, and a 124I radiolabeled; PMSA: prostate specific membrane antigen; PTT: photothermal therapy; PTX/GCT: paclitaxel/gemcitabine; RFA: radiofrequency ablation; SGT-53: liposomal nanocomplex designed for systemic, tumor-targeting delivery of the wt p53 gene; SOR007: topical nanoparticle paclitaxel ointment; TKM-080301: lipid nanoparticle formulation of a siRNA against PLK1 (polo-like kinase 1); USPIO: ultra-small superparamagnetic iron oxide.
Conclusions
Many strategies are under investigation in order to improve treatment of cancer metastases. Surgery and chemotherapy are the still the first line approaches used to obtain reduction or disappearance of a cancer mass. Unfortunately, in most cases these common strategies are not sufficient to achieve remission or full clearance from cancer recurrence, cell mutation and drug resistance. Moreover, when the metastatic process is advanced (clinical stage 3 or upwards) or when the mass is unresectable or highly vascularised, alternative approaches must be developed to provide an alternative treatment.
For these reasons, new approaches are needed to achieve more effective, selective and targeted responses. Nanotechnology carriers, thanks to their suitable and multiple properties, are under investigation to exploit anti-metastatic activity in preclinical and clinical trials. Moreover, nanosystems have several advantages such as reduction of systemic adverse effects and improvement of efficacy and safety of chemotherapeutics. Nanotechnology-based pharmacological strategies have shown many encouraging results for treatment of metastases as demonstrated by nano-formulation testing, which is in advanced phases of clinical testing. Nevertheless, at the moment, anti-metastasis nanomedicines have not yet been approved for clinical use.
New 3D in vitro models are under development to achieve more detailed information about cancer aetiology and metastasis dissemination. These advanced biomimetic systems reproduce in vitro the pathologic microenvironment and are emerging, valuable tools that can accelerate the discovery of factors and genetic process responsible for carcinogenic diseases. The possibility to use realistic models for the study of pathways implicated in cancer and metastasis as well as discovery of new and sensitive markers can allow establishing personalised treatments and speed up screening of new therapeutic drugs for subsequent clinical trials.
In the near future, thanks to these innovative technologies, metastasis prevention, localisation and treatment might be performed using synergic nano-systems that can selectively destroy the diseased cells and inform about the efficacy of treatment in real time. In addition, the few side effects and less invasive administration make nanocarriers preferable to traditional surgery.
Realisation of 3D models that can replicate the metastatic condition and reveal information about gene modification and aggressiveness to aid physicians in promptly fighting metastatic lesions with specific tools.
14. Head and neck metastatic disease and frailty: clinical and ethical approaches
Most patients with HNC have metastatic disease at diagnosis: nodal involvement is present in 43% and distant metastasis in 10%. Nearly 60% of patients with HNSCC report an advanced stage of disease 1.
Although locoregional control has improved, failure rate at distant organs remains relevant. The rate of DM in patients with HNSCC ranges from 4% to 26% 2.
DM from metastatic SCC have unfavourable prognosis: even with the best systemic therapy, median OS is about 10 months 3. Around 15-20% of patients with HNSCC will die from DM. Observations from autopsy series indicate that the rate of DM is 3 to 4 times higher than that reported in clinical series 4,5.
At diagnosis of DM, median time to death is about 4 months. As already stated, DM from HNSCC appear shortly after primary treatment 6. Typical curves of DM show a rapid increase between months 0 and 8, a slow increase between months 8 and 24, and a plateau between months 24 and 84.5 indicating the absence of late metastasis. In head and neck cancers with other histological origins, with primary tumours located in different regions, DM can still appear even 20 years after diagnosis 7,8.
The chance of cure for patients with HNC developing DM have a low possibility of curative treatment. Palliative chemotherapy is the most frequently used treatment, although response rates are not satisfying and treatment modalities remain controversial. Moreover, patients must be fit enough at diagnosis of DM to receive chemotherapy and/or radiotherapy.
Resection of solitary metastases in patients with HNC is controversial 9.
Treatments, if necessary, can be implemented by pain management and other holistic interventions (psychological and/or nutritional support). Counselling with patient at diagnosis about treatment options and prognosis is strongly recommended 10.
The patient’s clinical condition at diagnosis of DM is inevitably compromised. In the presence of economical and/or social problems, DM leads to worsening of the condition for both the patient and his/her family.
Progressive deterioration of the patient’s general condition takes place in this phase, leading to a consequent state of frailty. Thus, adequate evaluation of the patient’s status cannot be ignored.
Cancer features, such as site, stage and histological aggressiveness are the main aspects to be evaluated. It is also essential to evaluate comorbidities, social conditions, cognitive state and psychological conditions.
In other words, the concept of frailty can be defined as lack in what can guarantee an adequate quality of life.
Frailty in subjects over 65 years is present in at least 10%; for those aged up to 85, the value range from 25-50%. One must take note that a cancer diagnosis can give rise to frailty condition in 42% of sick subjects.
Moreover, with progressive aging of the population and its obvious effects on health warrant consideration. In 2016, in the EU, those over 65 years will represent almost 17%; by 2040, those in their 80s will be about 10% of the population 11,12.
What does frailty mean? It is a phenotype characterised by the decreased ability to re-establish homeostasis after exposure to stress with an increased risk of a negative result.
Frailty, in a biomedical context, can be defined as follows:
biomedical type: physiological syndrome characterised by reduction in functional reserves and by weak resistance to “stressors”; resulting from the cumulative decline of different physiological systems that cause vulnerability and adverse consequences 13;
bio-psycho-social type: dynamic state characterised by loss in one or more functional domains (social, psychological, corporeal) caused by the influence of multiple variables that increase the risk of adverse health outcomes 14.
We can hypothesise two different types of outcomes:
frail phenotype theory: explains that age-related cellular physiological changes lead to processes of system compromise and loss of homeostatic capacity 14;
frail accumulation theory: deficit determines the loss of more functions in various domains – medical, social and functional – involving increased vulnerability 15,16.
There are five measures that define the frail phenotype are 14:
involuntary weight loss;
self-reported exhaustion;
weakness in grip;
slow walking speed;
low physical activity.
In frailty, we have to consider that the remaining 30% of multi-organ function can represent the minimum threshold for functionality of the system itself.
It is therefore possible to lose 70% of function without any symptomatic manifestations, especially if this reduction takes place over a long period of time and this happens in patients with cancer that was just treated, and now with metastatic disease 17.
Sarcopenia is a cofactor for frailty: loss of muscle mass/strength, associated with progressive age increase comorbidities, while metastatic disease decreases patient reserves 18.
Further causes are acute and chronic stress, depression, low activity levels, decreased protein intake, social isolation, alcohol abuse, smoking, chronic diseases and multiple intake of drugs 19.
In preoperative frailty evaluation, the goal is:
statement of perioperative risk predictive value;
identification of patient risk, proposing a personalised therapeutic approach.
In a recent meta-analysis, frailty was associated with an increased incidence of postoperative complications, although there was no association between complications and factors commonly considered as age 20.
Reviews have stated that in patients over 75, frailty is associated with an increase in:
mortality;
post-operative complications;
prolonged hospital stay 20.
Comorbidity and frailty must be differentiated as 21:
comorbidities: presence of 2 or more chronic conditions or diseases;
-
frailty: physiological state of vulnerability characterised by:
weight loss,
tiredness,
decreased muscle mass,
changes in gait,
decrease in psychological activity.
Comorbidities are significantly more common in frail patients (52.8%) than in non-frail patients (37.1%; p < 0.001). Frailty is an independent predictor of in-hospital mortality, postoperative surgical complications and increased costs. It has synergic interaction with comorbidity associated with the increasing of likelihood of medical complications. Moreover, greater LOS (length of standing) is present in patients with comorbidity who are also frail 22. In metastatic disease, patients obviously become increasingly vulnerable with the combination of frailty and comorbidities.
In frailty, age is not a discriminating factor. In fact, even young subjects can be considered frail. In those over 65 years, chronicity, comorbidity, functional impairment, polypharmacy and socio-medical problems play a decisive role.
Homeostenosis, which is related to frailty, consists in the constant decline of homeostatic mechanisms that begins around the age of 30 and is established with a gradual decline in functional reserves and a diminished capacity for biological response to stress and changes.
Aging can therefore take a main role in the process of individual decreases and functional capabilities.
Vulnerable in elderly patients means a wide range of conditions that precede frailty. We can consider “vulnerable elder” a patient at high risk of pathologies and an ideal candidate for preventive interventions 23.
The not fit-elderly are 15/18% of the population between 65-84 years old. It’s a status of extreme vulnerability and predisposition to negative events in stress conditions with high risk of adverse events and rapid aging process complicated by disability 24.
Frailty assessment can contribute to individualising pre-operative risk counselling, personalised treatment plans, justify allocation of hospital resources (length of stay, costs) and improve planning and management of discharge for the most frail patients (rehabilitation, protected structures, integrated home assistance…).
Moreover, frailty assessment involves different tools that vary following the examined domains.
Careful attention is reserved to frailty in the oncological patient, with special attention to the elderly. Many guidelines have been proposed 25-27.
Some of these focus on physical aspects, while others include cognitive, psychological and/or social elements. The most relevant are:
Charlson Comorbidity Index (CCI);
Edmonton Frailty Scale (EFS);
Comprehensive Geriatric Assessment (CGA);
Groningen Frailty Index (GFI);
modified Frailty Index (mFI).
Although the CGA remains the standard test for diagnosis of frailty, the G8 (screening tool) provides practical and objective tools that can be efficiently implemented in daily practice, providing prognostic ability to guide individualisation of treatment regimens in this heterogeneous population 28. All this considering the time needed to define the patient’s frailty and that only 4% of care structures have a geriatric specialist available.
Moreover, a further problem is the impact of the possible evolution of metastatic disease on friends and relatives.
The daily activities of cohabitants are estimated to be influenced by illness in 71.5% of cases. All aspects of sociability are affected by the illness in at least one-quarter of cases.
The quality of life of the HNC patient’s cohabitants is demonstrated to be deteriorated at diagnosis.
It is significantly deteriorated when tumour is at an advanced stage (OR = 1.88 [1.13-3.13], p < 0.05), when patient has relevant aesthetic sequelae (OR = 1.75 [1.07-2.85], p < 0.05) and when patient has been treated with RT (OR = 2.46 [1.31-4.60] p < 0.01).
If the couple’s income is more than 1099 euro/month, the friendly environment is significantly deteriorated (OR = 2.34 [1.26-4.35] p < 0.01). It is the same if the partner is male (p < 0.05) 29.
In addition, one must take in account psychological problems that impact the life of patient and which become more acute and take gloomy contours in case of diagnosis of metastatic disease. HNC treatment can be intrusive, resulting in permanent functional and disfiguring changes, thereby increasing the likelihood of a post-traumatic stress reaction. At least 13% of patients meet diagnostic criteria for post-traumatic stress disorder (PTSD), with an additional 33% experiencing some post-traumatic stress symptoms (PTSS); 12.8% of partners report PTSD and 25.7% of partners are indicative of PTSS 30.
Post-treatment, patients describe greater difficulties in coping with the side effects of treatment and accessing supportive care when away from the hospital setting. The first 6 to 12 months post-treatment are a critical time in providing supportive care, and this time is the time in which metastatic disease arises, a period of particular vulnerability for the patient.
Nowadays, cost-effectiveness and the balance between unreasonable obstinacy and the principle of beneficence are crucial in treatment of metastatic disease 31,32.
“Patients with advanced incurable cancer face complex physical, psychological, social, and spiritual consequences of disease and its treatment. Care for these patients should include an individualized assessment of the patient’s needs, goals, and preferences throughout the course of illness. Consideration of disease-directed therapy, symptom management, and attention to quality of life are important aspects of quality cancer care. However, emerging evidence suggests that, too often, realistic conversations about prognosis, the potential benefits and limitations of disease-directed therapy, and the potential role of palliative care, either in conjunction with or as an alternative to disease-directed therapy, occur late in the course of illness or not at all.
Personalized cancer care describes our aspiration to base treatment on the unique biologic features of a patient’s disease. However, in the context of advanced cancer, defined as incurable disease, there is a need to more broadly consider how we can best “personalize” or tailor care to the diverse physical, psychological, social, and spiritual consequences of cancer for the individual patient. Such an approach requires stepping back from the paradigm of applying one line of therapy after the other and focusing primarily on disease-directed interventions. Instead, we need to move toward developing a treatment plan that is consistent with evidence-based options (including disease-directed and palliative care) and the patient’s informed preferences for how we pursue and balance these options throughout the course of illness” 33.
15. Observations on the socio-economic impact of metastatic disease in head and neck oncology
The data referring to the incidence of tumours in Italy in 2018 1 indicate 373,000 newly diagnosed cases (52% men and 48% women), 4300 more compared to 2017, with approximately 1000 new diagnoses each day. The regions with the greatest number of estimated cancer diagnoses in 2018 are Lombardy, Lazio and Veneto: currently 6% of the Italian population (3.4 million people) live with a tumour diagnosis, but for 2020 it is expected to rise to 4.5 million people. The death toll in 2015 was 169,726 (Tab. 15.I); about 9000 new cases of head and neck tumours, 7400 men and 2300 women, are expected in 2020.
Table 15.I.
Number of deaths from malignant tumors by site and gender registered in Italy - 2015 1.
| Site | Males | Females | Total |
|---|---|---|---|
| Malignant tumours | 94,498 | 75,228 | 169,726 |
| Lips, oral cavity and pharynx MTs | 1,889 | 986 | 2,975 |
| Larynx MTs | 1,315 | 161 | 1,476 |
| Thyroid MTs | 218 | 331 | 549 |
| Trachea, bronchi and lung MTs | 24,305 | 9,531 | 33,836 |
| Colon, rectum and anus MTs | 10,084 | 8,851 | 18,935 |
In Italy the deaths for head and neck in 2015 1 were 2875, 1898 men and 986 women, with 57% of survivability up to 5 years and 48% survivability up to 10 years; the probability of survival up to 5 years following diagnosis, having lived the first year, is 68% in men and 74% in women. There are no data specifically referring to the incidence of metastasis in head and neck tumour.
The upcoming observations will thus concern general aspects of neoplastic pathology 2-10.
General data highlight that cancer is a “mass pathology” with an increasing trend worldwide (Tab. 15.II) and has significant socio-economic impact 2.
Table 15.II.
Estimate of the 2009-2020 incidence trend in the world of some tumors. Censis processing of data from the Economist Intelligence Unit, 2010 2.
| Trend (%) | |
|---|---|
| Larynx | 32.0 |
| Other parts of the pharynx | 30.0 |
| Oral cavity | 29.6 |
| Nasopharynx | 23.6 |
| Thyroid | 22.7 |
| Lung | 33.9 |
| Colonrectum | 33.5 |
It is, therefore, important to consider the health aspects and socio-economic costs of the pathology, since the effects have multidimensional traits and require elaboration of data and indicators from different sources and which must be made homogeneous in order to define a value that represents the total cost of the pathology and, consequently, invest in appropriate prevention and treatment strategies 3-6.
Cancer is increasingly assuming the characteristics of a pathology with the outlines of a medical-social issue: this means we are facing new needs that require adequate and effective solutions for:
sustaining personal and work autonomy during treatment;
encouraging appropriate presentation to socio-sanitary structures;
improving the quality of the relationship with caregivers;
obtaining the best results from therapy;
allowing an equal source distribution on both social and health levels.
In Italy, in 2013, there were 2.8 million estimated prevailing cases with an oncological health care expense of 7.5 billion euros, or 6.7% of the total healthcare expense (Tab. 15.III) 1,2.
Table 15.III.
Index of average costs per case and loss of productivity by type of tumor in the world, 2009 (index numbers) 2.
| Index of average expenses for case and loss of productivity for tumour type in the world 2009
(index numbers) |
Relative medical costs: costs for medical procedures-services, treatment and cure with hospitalization costs, ambulatory medical examinations, medication prescriptions | Relative extramedical costs: transportation costs to execute the cure, complementary and alternative costs, assistance costs | Relative loss of productivity (includes the economic value of lost time and results) |
|---|---|---|---|
| Larynx | 64 | 93 | 61 |
| Nasopharynx | 94 | 107 | 67 |
| Oral cavity | 81 | 99 | 57 |
| Other parts of the pharynx | 120 | 122 | 42 |
| Thyroid | 23 | 64 | 150 |
| Lung | 141 | 121 | 132 |
| Colon rectum | 94 | 84 | 87 |
Neoplastic pathologies are multifaceted and involve a plurality of life dimensions for individuals and their community, the costs they produce are also multifaceted and articulated, ranging from strictly healthcare costs to socio-economic costs, and is linked to the impact on work, the ability to produce income, psychological issues which concern and involve not only patients but also their relatives, caregivers and friends.
The most recent data quantify the impact of oncology on the National Health System in terms of healthcare expenses with growth rates included between + 5 and + 10% per year; the expense of the National Health System for diagnosis, cures, rehabilitation etc. covers 20% of the entire hospital expense with very high per-capita costs, being 5 times higher than most other pathologies: these numbers are sufficient to cause a crisis in the sustainability of the Italian healthcare system 2,7-9.
The tariff value of the last year of life in subjects affected by tumour is roughly twice the value of subjects deceased for another pathology, and the tariff value of the year of life preceding the decease of subjects with tumour is roughly 5 times superior to that of male subjects without neoplasia and almost four times that of female subjects.
A very recent study by the Imperial College of London has reconfirmed the link between economic and public finance crisis and the death toll from tumours, showing how, in a significantly relevant way, a greater death toll for the majority of neoplastic pathologies is associated with the growth of unemployment and a reduction in public sanitary expenses (260,000 more deaths than in Organization for Economic Cooperation and Development (OECD) countries; furthermore, this study has highlighted how this association reduces or disappears in countries with universal healthcare systems 10.
The socio-economic impact of oncological pathologies is constantly growing in our health system: it is, therefore, fundamental to develop a reliable system for estimating healthcare expenses needed for the treatment of these patients in the initial stage (no later than one year since the diagnosis), the medium term (the time between the initial and the final phase) and the final stage of the disease (no later than one year before the decease) 2.
We must also consider the costs when the neoplastic disease cannot be cured, in the majority of the cases of metastatic tumours: survivability of patients in these cases has noticeably increased in the last few years, so much that it is now possible to talk about “chronicisation” of a cancer, with an often acceptable quality of life and a sensitive economic implication with regards to the assistance required 5.
The “U-shaped” trend of costs in the three phases of the disease, growth of costs for advanced stages and decrease of costs with the growth of age have determined the necessity of developing standardised techniques for the collection and analysis of cost data attributed to tumours, but only for certain cases of neoplasia 6.
The scientific and research experience in analysing clinical and assistive costs starts to become broad in economically advanced countries and with the initiation of collaborative projects to conduct comparative analyses of the results obtained. Italy, from this point of view, has done less compared with other countries in Northern Europe or America 5,7.
Notwithstanding, direct healthcare costs are the clearest economic expression, even in the presence of so-called “submerged costs” (Tab. 15.IV) 8,9:
Table 15.IV.
| Direct costs | Indirect costs | ||
|---|---|---|---|
|
Medical expenses:
specialist exams |
Radiological and nuclear medicine exams, blood sampling, and other tests
Physiotherapy/rehabilitation service Reconstructive surgery procedures Healthcare facilities (prostheses…) Dressing, drugs Private nurses |
Missed salaries from the patients’ job | Monetisation of working hours lost during the year
Missing income due to retirement Monetisation of working hours lost during the year |
| Missed salaries from the caregivers’job | Missing income due to retirement
Further reduction of annual income of caregivers following the disease Monetisation of assistance/surveillance provided by caregivers Monetary help by caregivers |
||
| Non-medical expenses | Domestic helper/caretaker
Transport Hotel costs (including caregivers) Special diets Other non-medical costs sustained by caregivers |
direct social costs, including costs which are chargeable to social security, national health system, in the forms of “relocation” of the citizen who is unable to work;
indirect costs, i.e. those connected to care and provided by relatives/caregivers or linked to obtaining care (relocations in other centres);
indirect social costs linked to the loss of human capital.
The yearly social per-capita cost for patients with or without a caregiver is17,483 euros, of which roughly 6,500 are direct and 10,500 are indirect, with a per-capita reduction with the passing of time since initial diagnosis. The sole social cost referring to all patients, with or without a caregiver, amounts to roughly 36.4 billion euros: 5.8 billion in direct costs and more than 30 billion in indirect costs 9.
Moreover, we have to consider that even in Italy the problem of “financial toxicity” exists. Economic suffering negatively affects the chance for the patient to appreciate the therapeutic benefits expressed in quality of live. This occurs in 1 of 5 patients, and is often associated with worsening prognosis.
Many of these patients experience worsening of their economic hardships during therapy, and this worsening is a predictive signal of a higher risk for death in the following months/years, although in Italy the estimation of an increasing death risk is definitely lower compared to that published in the United States (20% vs 70%) 4,5.
All these factors lead to the necessity of an active engagement of the oncological patient, in the management of their healthcare pathway and their disease. Recent studies have shown how engaged patients maintain good working performance and better psychological wellbeing in their daily life with a subsequent reduction of healthcare expenses 7,8.
The Italian healthcare context is demonstrating, in the medium term, to be suffering and increasingly less able to be adequate and satisfactory in its social mission. This situation is due to emerging needs which go beyond the administration of strictly understood therapeutic procedures and which may influence outcomes and evolution in pathologies (Tab. 15.V) 9.
Table 15.V.
Areas where the greatest problems following the diagnosis emergerd 7.
| Psychological level | 57.1% |
| Processing of day-to-day practises | 49.8% |
| Family | 45.5% |
| Work | 33.9% |
| Social relationships | 33.7% |
| Economic availability | 32.2% |
It will be challenging for our healthcare system to restore itself. Taking into account the above observations, these efforts could be focused on: Reorganisation of surrounding patient system; Systemic measurements of health and health and cost outcomes; Reformulation of funding procedures; Comparison of results and systemic diffusion of best managerial practices; Full implementation of computerised platforms.
Figures and tables
Acknowledgements
The Authors thank Andrea Colombo, MD and Maria Luisa Invernizzi, PhD for their editorial support.
References
1. Introduction
- 1.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 2.Takes RP, Rinaldo A, Silver CE, et al. Distant metastases from head and neck squamous cell carcinoma. Part I. Basic aspects. Oral Oncol 2012;48:775-9. https://doi.org/10.1016/j.oraloncology.2012.03.013 10.1016/j.oraloncology.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 3.Wiegand S, Zimmermann A, Wilhelm T, et al. Survival after distant metastasis in head and neck cancer. Anticancer Res 2015;35:5499-502. [PubMed] [Google Scholar]
2. Epidemiology and natural history
- 1.Teymoortash A, Werner JA. Current advances in diagnosis and surgical treatment of lymph node metastasis in head and neck cancer. GMS Curr Top Otorhinolaryngol Head Neck Surg 2012;11:Doc04 https://doi.org/10.3205/cto000086 10.3205/cto000086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melchardt T, Magnes T, Hufnagl C, et al. Clonal evolution and heterogeneity in metastatic head and neck cancer - an analysis of the Austrian Study Group of Medical Tumour Therapy study group. Eur J Cancer 2018;93:69-78. https://doi.org/10.1016/j.ejca.2018.01.064 10.1016/j.ejca.2018.01.064 [DOI] [PubMed] [Google Scholar]
- 3.Crile G. Landmark article Dec 1, 1906: excision of cancer of the head and neck. With special reference to the plan of dissection based on one hundred and thirty-two operations. By George Crile. JAMA 1987;258:3286-93. [DOI] [PubMed] [Google Scholar]
- 4.Tai SK, Li WY, Yang MH, et al. Perineural invasion in T1 oral squamous cell carcinoma indicates the need for aggressive elective neck dissection. Am J Surg Pathol 2013;37:1164-72. https://doi.org/10.1097/PAS.0b013e318285f684 10.1097/PAS.0b013e318285f684 [DOI] [PubMed] [Google Scholar]
- 5.Audet N, Beasley NJ, MacMillan C, et al. Lymphatic vessel density, nodal metastases, and prognosis in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 2005;131:1065-70. https://doi.org/10.1001/archotol.131.12.1065 10.1001/archotol.131.12.1065 [DOI] [PubMed] [Google Scholar]
- 6.Stoeckli SJ. Sentinel node biopsy for oral and oropharyngeal squamous cell carcinoma of the head and neck. Laryngoscope 2007;117:1539-51. https://doi.org/10.1097/MLG.0b013e318093ee67 10.1097/MLG.0b013e318093ee67 [DOI] [PubMed] [Google Scholar]
- 7.Dwivedi RC, Kazi R, Agrawal N, et al. Comprehensive review of small bowel metastasis from head and neck squamous cell carcinoma. Oral Oncol 2010;46:330-5. https://doi.org/10.1016/j.oraloncology.2010.01.013 10.1016/j.oraloncology.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 8.Spector JG, Sessions DG, Haughey BH, et al. Delayed regional metastases, distant metastases, and second primary malignancies in squamous cell carcinomas of the larynx and hypopharynx. Laryngoscope 2001;111:1079-87. https://doi.org/10.1097/00005537-200106000-00028 10.1097/00005537-200106000-00028 [DOI] [PubMed] [Google Scholar]
- 9.Kuperman DI, Auethavekiat V, Adkins DR, et al. Squamous cell cancer of the head and neck with distant metastasis at presentation. Head Neck 2011;33:714-8. https://doi.org/10.1002/hed.21529 10.1002/hed.21529 [DOI] [PubMed] [Google Scholar]
- 10.Ferlito A, Shaha AR, Silver CE, et al. Incidence and sites of metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec 2001;63:202-7. https://doi.org/10.1159/000055740 10.1159/000055740 [DOI] [PubMed] [Google Scholar]
- 11.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 12.Liu JC, Bhayani M, Kuchta K, et al. Patterns of distant metastasis in head and neck cancer at presentation: implications for initial evaluation. Oral Oncol 2019;88:131-6. https://doi.org/10.1016/j.oraloncology.2018.11.023 10.1016/j.oraloncology.2018.11.023 [DOI] [PubMed] [Google Scholar]
- 13.Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. https://doi.org/10.1200/JCO.1995.13.1.8 10.1200/JCO.1995.13.1.8 [DOI] [PubMed] [Google Scholar]
- 14.Florescu C, Thariat J. Local ablative treatments of oligometastases from head and neck carcinomas. Crit Rev Oncol Hematol 2014;91:47-63. https://doi.org/10.1016/j.critrevonc.2014.01.004 10.1016/j.critrevonc.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 15.Albergotti WG, Abberbock S, Mathews F, et al. Oligometastatic status as predictor of survival in metastatic human papillomavirus-positive oropharyngeal carcinoma. Head Neck 2018;40:1685-90. https://doi.org/10.1002/hed.25171 10.1002/hed.25171 [DOI] [PubMed] [Google Scholar]
- 16.Bates JE, De Leo AN, Morris CG, et al. Oligometastatic squamous cell carcinoma of the head and neck treated with stereotactic body ablative radiotherapy: single-institution outcomes. Head Neck 2019;41:2309-14. https://doi.org/10.1002/hed.25695 10.1002/hed.25695 [DOI] [PubMed] [Google Scholar]
- 17.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. https://doi.org/10.1002/ijc.29210 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- 18.Choussy O, Ferron C, Védrine P-O, et al. Adenocarcinoma of ethmoid: a GETTEC retrospective multicenter study of 418 cases. Laryngoscope 2008;118:437-43. https://doi.org/10.1097/MLG.0b013e31815b48e3 10.1097/MLG.0b013e31815b48e3 [DOI] [PubMed] [Google Scholar]
- 19.Peyraga G, Lafond C, Pointreau Y, et al. Nasal cavity and paranasal sinus cancer. Cancer Radiother 2016;20(Suppl):S99-S103. https://doi.org/10.1016/j.canrad.2016.07.035 10.1016/j.canrad.2016.07.035 [DOI] [PubMed] [Google Scholar]
- 20.Ahn PH, Mitra N, Alonso-Basanta M, et al. Nodal metastasis and elective nodal level treatment in sinonasal small-cell and sinonasal undifferentiated carcinoma: a surveillance, epidemiology and end results analysis. Br J Radiol 2016;89:20150488 https://doi.org/10.1259/bjr.20150488 10.1259/bjr.20150488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahn PH, Mitra N, Alonso-Basanta M, et al. Risk of lymph node metastasis and recommendations for elective nodal treatment in squamous cell carcinoma of the nasal cavity and maxillary sinus: a SEER analysis. Acta Oncol 2016;55:1107-14. https://doi.org/10.1080/0284186X.2016.1216656 10.1080/0284186X.2016.1216656 [DOI] [PubMed] [Google Scholar]
- 22.Dubal PM, Bhojwani A, Patel TD, et al. Squamous cell carcinoma of the maxillary sinus: a population-based analysis. Laryngoscope 2016;126:399-404. https://doi.org/10.1002/lary.25601 10.1002/lary.25601 [DOI] [PubMed] [Google Scholar]
- 23.Unsal AA, Dubal PM, Patel TD, et al. Squamous cell carcinoma of the nasal cavity: a population-based analysis. Laryngoscope 2016;126:560-5. https://doi.org/10.1002/lary.25531 10.1002/lary.25531 [DOI] [PubMed] [Google Scholar]
- 24.Ant A, Kilic C, Baltu Y, et al. Lip cancer: reconsidering the at-risk patients with pathological assessment. Oral Dis 2019;25:742-9. https://doi.org/10.1111/odi.13017 10.1111/odi.13017 [DOI] [PubMed] [Google Scholar]
- 25.Byers RM, Weber RS, Andrews T, et al. Frequency and therapeutic implications of “skip metastases” in the neck from squamous carcinoma of the oral tongue. Head Neck 1997;19:14-9. https://doi.org/10.1002/(sici)1097-0347(199701)19:1<14::aid-hed3>3.0.co;2-y [DOI] [PubMed] [Google Scholar]
- 26.Asakage T, Yokose T, Mukai K, et al. Tumor thickness predicts cervical metastasis in patients with stage I/II carcinoma of the tongue. Cancer 1998;82:1443-8. https://doi.org/10.1002/(sici)1097-0142(19980415)82:8<1443::aid-cncr2>3.0.co;2-a [DOI] [PubMed] [Google Scholar]
- 27.D’Cruz AK, Vaish R, Kapre N, et al. Elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med 2015;373: 521-9. https://doi.org/10.1056/NEJMoa1506007 10.1056/NEJMoa1506007 [DOI] [PubMed] [Google Scholar]
- 28.Huang SH, Hwang D, Lockwood G, et al. Predictive value of tumor thickness for cervical lymph-node involvement in squamous cell carcinoma of the oral cavity: a meta-analysis of reported studies. Cancer 2009;115:1489-97. https://doi.org/10.1002/cncr.24161 10.1002/cncr.24161 [DOI] [PubMed] [Google Scholar]
- 29.Sakamoto Y, Matsushita Y, Yamada S, et al. Risk factors of distant metastasis in patients with squamous cell carcinoma of the oral cavity. Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:474-80. https://doi.org/10.1016/j.oooo.2015.11.022 10.1016/j.oooo.2015.11.022 [DOI] [PubMed] [Google Scholar]
- 30.Kang CJ, Lin CY, Wang HM, et al. The number of pathologically positive lymph nodes and pathological tumor depth predicts prognosis in patients with poorly differentiated squamous cell carcinoma of the oral cavity. Int J Radiat Oncol Biol Phys 2011;81:e223-30. https://doi.org/10.1016/j.ijrobp.2011.03.060 10.1016/j.ijrobp.2011.03.060 [DOI] [PubMed] [Google Scholar]
- 31.Chen TC, Hsu CW, Lou PJ, et al. The clinical predictive factors for subsequent distant metastasis in patients with locoregionally advanced oral squamous cell carcinoma. Oral Oncol 2013;49:367-73. https://doi.org/10.1016/j.oraloncology.2012.10.006 10.1016/j.oraloncology.2012.10.006 [DOI] [PubMed] [Google Scholar]
- 32.Chiesa F, De Paoli F. Distant metastases from nasopharyngeal cancer. ORL J Otorhinolaryngol Relat Spec 2001;63:214-6. https://doi.org/10.1159/000055743 10.1159/000055743 [DOI] [PubMed] [Google Scholar]
- 33.King AD, Ahuja AT, Leung SF, et al. Neck node metastases from nasopharyngeal carcinoma: MR imaging of patterns of disease. Head Neck 2000;22:275-81. https://doi.org/10.1002/(sici)1097-0347(200005)22:3<275::aid-hed10>3.0.co;2-n [DOI] [PubMed] [Google Scholar]
- 34.Cocuzza S, Di Mauro P, Maiolino L, et al. Segni clinici e sintomi iniziali di insorgenza nei tumori del rinofaringe e valutazioni prognostiche. Serra A. (ed.). Relazione ufficiale “Tumori del rinofaringe: Attualità diagnostiche e terapeutiche”. Lecce: Torgraf; 2015. p. 117. [Google Scholar]
- 35.Wu MY, He XY, Hu CS. Tumor regression and patterns of distant metastasis of T1-T2 nasopharyngeal carcinoma with intensity-modulated radiotherapy. PLoS One 2016;11:e0154501 https://doi.org/10.1371/journal.pone.0154501 10.1371/journal.pone.0154501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gross BC, Olsen SM, Lewis JE, et al. Level IIB lymph node metastasis in oropharyngeal squamous cell carcinoma. Laryngoscope 2013;123:2700-5. https://doi.org/10.1002/lary.24129 10.1002/lary.24129 [DOI] [PubMed] [Google Scholar]
- 37.Youssef E, Chuba P, Salib N, et al. Pathological distribution of positive lymph nodes in patients with clinically and radiologically N0 oropharyngeal carcinoma: implications for IMRT treatment planning. Cancer J 2005;11:412-6. https://doi.org/10.1097/00130404-200509000-00009 10.1097/00130404-200509000-00009 [DOI] [PubMed] [Google Scholar]
- 38.Sood AJ, McIlwain W, O’Connell B, et al. The association between T stage and clinical nodal metastasis in HPV-positive oropharyngeal cancer. Am J Otolaryngol 2014;35:463-8. https://doi.org/10.1016/j.amjoto.2013.12.008 10.1016/j.amjoto.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 39.Lim YC, Lee SY, Lim JY, et al. Management of contralateral N0 neck in tonsillar squamous cell carcinoma. Laryngoscope 2005;115:1672-5. https://doi.org/10.1001/archotol.128.3.229 10.1001/archotol.128.3.229 [DOI] [PubMed] [Google Scholar]
- 40.Wei WI. The dilemma of treating hypopharyngeal carcinoma: more or less: Hayes Martin Lecture. Arch Otolaryngol Head Neck Surg 2002;128:229-32. https://doi.org/10.1001/archotol.128.3.229 10.1001/archotol.128.3.229 [DOI] [PubMed] [Google Scholar]
- 41.Spector GJ. Distant metastases from laryngeal and hypopharyngeal cancer. ORL J Otorhinolaryngol Relat Spec 2001;63:224-8. https://doi.org/10.1159/000055746 10.1159/000055746 [DOI] [PubMed] [Google Scholar]
- 42.Villaret AB, Piazza C, Peretti G, et al. Multicentric prospective study on the prevalence of sublevel IIb metastases in head and neck cancer. Arch Otolaryngol Head Neck Surg 2007;133:897-903. https://doi.org/10.1001/archotol.133.9.897 10.1001/archotol.133.9.897 [DOI] [PubMed] [Google Scholar]
- 43.Lucioni M, D’Ascanio L, De Nardi E, et al. Management of paratracheal lymph nodes in laryngeal cancer with subglottic involvement. Head Neck 2018;40:24-33. https://doi.org/10.1002/hed.24905 10.1002/hed.24905 [DOI] [PubMed] [Google Scholar]
- 44.Amar A, Chedid HM, Franzi SA, et al. Neck dissection in squamous cell carcinoma of the larynx: indication of elective contralateral neck dissection. Braz J Otorhinolaryngol 2012;78:7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Werner JA, Dünne AA, Myers JN. Functional anatomy of the lymphatic drainage system of the upper aerodigestive tract and its role in metastasis of squamous cell carcinoma. Head Neck 2003;25:322-32. https://doi.org/10.1002/hed.10257 10.1002/hed.10257 [DOI] [PubMed] [Google Scholar]
- 46.Garavello W, Ciardo A, Spreafico R, et al. Risk factors for distant metastases in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 2006;132:762-6. [DOI] [PubMed] [Google Scholar]
3. Biological factors in metastatic dissemination of head and neck squamous cell carcinomas
- 1.Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium: clinical implications of multicentric origin. Cancer 1953;6:963-8. https://doi.org/10.1002/1097-0142(195309)6:5<963::aid-cncr2820060515>3.0.co;2-q [DOI] [PubMed] [Google Scholar]
- 2.Curry JM, Sprandio J, Cognetti D. Tumor microenvironment in head and neck squamous cell carcinoma. Semin Oncol 2014;41:217-34. https://doi.org/10.1053/j.seminoncol.2014.03.003 10.1053/j.seminoncol.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 3.Bànkfalvi A, Krassort M, Vègh A, et al. Deranged expression of the E-cadherin/beta-catenin complex and the epidermal growth factor receptor in the clinical evolution and progression of oral squamous cell carcinomas. J Oral Pathol Med 2002;31:450-7. https://doi.org/10.1034/j.1600-0714.2002.00147.x 10.1034/j.1600-0714.2002.00147.x [DOI] [PubMed] [Google Scholar]
- 4.Andrews NA, Jones AS, Helliwell TR, et al. Expression of the E-cadherin-catenin cell adhesion complex in primary squamous cell carcinomas of the head and neck and their nodal metastases. Br J Cancer 1997;75:1474-80. https://doi.org/10.1038/bjc.1997.252 10.1038/bjc.1997.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramos DM, But M, Regezi J, et al. Expression of integrin beta 6 enhances invasive behavior in oral squamous cell carcinoma. Matrix Biol 2002;21:297-307. https://doi.org/10.1016/s0945-053x(02)00002-1 10.1016/s0945-053x(02)00002-1 [DOI] [PubMed] [Google Scholar]
- 6.Kunishi M, Kayada Y, Yoshiga K. Down-regulated expression of CD44 variant 6 in oral squamous cell carcinomas and its relationship to regional lymph node metastasis. Int J Oral Maxillofac Surg 1997;26:280-3. https://doi.org/10.1016/s0901-5027(97)80869-7 10.1016/s0901-5027(97)80869-7 [DOI] [PubMed] [Google Scholar]
- 7.Oliveira DT, Sherriff M, Odell EW. Expression of CD44 variant exons by primary and metastatic oral squamous carcinomas. J Oral Pathol Med 1998;27:303-7. https://doi.org/10.1111/j.1600-0714.1998.tb01961.x 10.1111/j.1600-0714.1998.tb01961.x [DOI] [PubMed] [Google Scholar]
- 8.O-Charoenrat P, Rhys-Evans P, Court WJ, et al. Differential modulation of proliferation, matrix metalloproteinase expression and invasion of human head and neck squamous carcinoma cells by c-erbB ligands. Clin Exp Metastasis 1999;17:631-9. https://doi.org/10.1023/a:1006751016860 10.1023/a:1006751016860 [DOI] [PubMed] [Google Scholar]
- 9.O-Charoenrat P, Rhys-Evans P, Modjtahedi H, et al. Overexpression of epidermal growth factor receptor in human head and neck squamous carcinoma cell lines correlates with matrix metalloproteinase-9 expression and in vitro invasion. Int J Cancer 2000;86:307-17. https://doi.org/10.1002/(sici)1097-0215(20000501)86:3<307::aid-ijc2>3.0.co;2-i [DOI] [PubMed] [Google Scholar]
- 10.Vigneswaran N, Zhao W, Dassanayake A, et al. Variable expression of cathepsin B and D correlates with highly invasive and metastatic phenotype of oral cancer. Hum Pathol 2000;31:931-7. https://doi.org/10.1053/hupa.2000.9035 10.1053/hupa.2000.9035 [DOI] [PubMed] [Google Scholar]
- 11.Gandour-Edwards R, Trock B, Donald PJ. Predictive value of cathepsin-D for cervical lymph node metastasis in head and neck squamous cell carcinoma. Head Neck 1999;21:718-22. https://doi.org/10.1002/(sici)1097-0347(199912)21:8<718::aid-hed6>3.0.co;2-w [DOI] [PubMed] [Google Scholar]
- 12.Di Renzo MF, Olivero M, Martone T, et al. Somatic mutations of the MET oncogene are selected during metastatic spread of human HNSC carcinomas. Oncogene 2000;19:1547-55. https://doi.org/10.1038/sj.onc.1203455 10.1038/sj.onc.1203455 [DOI] [PubMed] [Google Scholar]
- 13.O-Charoenrat P, Rhys-Evans PH, Modjtahedi H, et al. The role of c-erbB receptors and ligands in head and neck squamous cell carcinoma. Oral Oncol 2002;38:627-40. https://doi.org/10.1016/s1368-8375(02)00029-5 10.1016/s1368-8375(02)00029-5 [DOI] [PubMed] [Google Scholar]
- 14.Lin SY, Dolfi SC, Amiri S, et al. TP53 regulates the migration of mesenchymal stromal cells in response to the tumor microenvironment through both CXCL12 -dependent and independent mechanism. Int J Oncol 2013;43:1817-23. https://doi.org/10.3892/ijo.2013.2109 10.3892/ijo.2013.2109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshida R, Nagata M, Nakayama H, et al. The pathological significance of NOTCH 1 in oral squamous cell carcinoma. Lab Invest 2013;93:1068-81. https://doi.org/10.1038/labinvest.2013.95 10.1038/labinvest.2013.95 [DOI] [PubMed] [Google Scholar]
- 16.Sheu JJ, Hua Ch, Wan L, et al. Functional genomic analysis identified epidermial growth factor receptor activation as the most common genetic event in oral squamous cell carcinoma. Cancer Res 2009; 69:2568-76. https://doi.org/10.1158/0008-5472.CAN-08-3199 10.1158/0008-5472.CAN-08-3199 [DOI] [PubMed] [Google Scholar]
- 17.Geiger J, Grandis J, Bauman J. The STAT3 pathway as a therapeutic target in head and neck cancer: Barriers and innovations. Oral Oncol 2016;56:84-92. https://doi.org/10.1016/j.oraloncology.2015.11.022 10.1016/j.oraloncology.2015.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Squarize CH, Castilho RM, Sriuranpong V, et al. Molecular cross-talk between NFkB and STAT3 pathways in head and neck squamous cell carcinoma. Neoplasia 2006;8:733-46. https://doi.org/10.1593/neo.06274 10.1593/neo.06274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wheeler SE, Shi H, Lin F, et al. Enhancement of head and neck squamous cell carcinoma proliferation, invasion and metastasis by tumor-associated fibroblasts in preclinical models. Head Neck 2014;36:385-92. https://doi.org/10.1002/hed.23312 10.1002/hed.23312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franco OE, Shaw AK, Strand DW, et al. Cancer associated fibroblasts in cancer pathogenesis. Semin Cell Dev Biol 2010; 21:33-9. https://doi.org/10.1016/j.semcdb.2009.10.010 10.1016/j.semcdb.2009.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lim KP, Cirillo N, Hessona Y, et al. Fibroblasts gene expression profile reflects the stage of tumor progression in oral squamous cell carcinoma. J Pathol 2011;223:459-69. https://doi.org/10.1002/path.2841 10.1002/path.2841 [DOI] [PubMed] [Google Scholar]
- 22.Leef G, Thomas SM. Molecular communication between tumor-associated fibroblasts and head and neck squamous cell carcinoma. Oral Oncol 2013;49:381-6. https://doi.org/10.1016/j.oraloncology.2012.12.014 10.1016/j.oraloncology.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knowles LM, Stabile LP, Egloff AM, et al. HGF and c-MET participate in paracrine tumorigenic pathways in head and neck squamous cell cancer. Clin Cancer Res 2009;15:3740-50. https://doi.org/10.1158/1078-0432.CCR-08-3252 10.1158/1078-0432.CCR-08-3252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishikawa T, Nakashiro K, Klosek SK, et al. Hypoxia enhances CXCR4 expression by activating HIF1 in oral squamous cell carcinoma. Oncol Rep 2009;21:707-12. [PubMed] [Google Scholar]
- 25.Duray A, Demoulin S, Houvert P, et al. Immune suppression in head and neck cancers: a review. Clin Dev Immunol 2010:701657 https://doi.org/10.1155/2010/701657 10.1155/2010/701657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogino T, Shigyo H, Ishii H, et al. HLA class I antigen down-regulation in primary laryngeal squamous cell carcinoma lesions as a poor prognostic marker. Cancer Res 2006;66:9281-9. [DOI] [PubMed] [Google Scholar]
- 27.Yilmaz T, Gedikoglu G, Celik A, et al. Prognostic significance of Langerhans cell infiltration in cancer of the larynx. Otolaryngol Head Neck Surg 2005;139:309-16. https://doi.org/10.1016/j.otohns.2004.04.018 10.1016/j.otohns.2004.04.018 [DOI] [PubMed] [Google Scholar]
- 28.Hartmann E, Wollenberg B, Rothenfusser S, et al. Identification and functional analysis of tumor-infiltrating plasmacytoid dendritic cells in head and neck cancer. Cancer Res 2003;63: 6478-87. [PubMed] [Google Scholar]
- 29.Bekeredjian-Ding I, Schafer M, Hartmann E, et al. Tumour-derived prostaglandin E and transforming growth factor-beta synergize to inhibit plasmacytoid dendritic cell derived interferon-alpha. Immunology 2009;128:439-50. https://doi.org/10.1111/j.1365-2567.2009.03134.x 10.1111/j.1365-2567.2009.03134.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li C, Shintani S, Terakado N, et al. Infiltration of tumor-associated macrophages in human oral squamous cell carcinoma. Oncol Rep 2002; 9:1219-23. [PubMed] [Google Scholar]
- 31.Ritt M, De Andrea M, Mondini M, et al. Cell cycle and viral and immunologic profiles of head and neck squamous cell carcinoma as predictable variables of tumor progression. Head Neck 2009;31:318-27. https://doi.org/10.1002/hed.20977 10.1002/hed.20977 [DOI] [PubMed] [Google Scholar]
- 32.Bardos H, Juhasz A, Repassy G, et al. Fibrin deposition in squamous cell carcinomas of the larynx and hypopharynx. Thromb Haemost 1998;80:767-72. [PubMed] [Google Scholar]
- 33.Marcus B, Arenberg D, Lee J, et al. Prognostic factors in oral cavity and oropharyngeal squamous cell carcinoma. Cancer 2004;101:2779-87. https://doi.org/10.1002/cncr.20701 10.1002/cncr.20701 [DOI] [PubMed] [Google Scholar]
- 34.Whiteside TL. Immunobiology in head and neck cancer. Cancer Metastasis Rev 2005;24:95-105. https://doi.org/10.1007/s10555-005-5050-6 10.1007/s10555-005-5050-6 [DOI] [PubMed] [Google Scholar]
- 35.Gastman BR, Atarashi Y, Reichert TE, et al. Fas ligand is expressed on human squamous cell carcinomas of the head and neck, and it promotes apoptosis of T lymphocytes. Cancer Res 1999;59:5356-64. [PubMed] [Google Scholar]
- 36.Kassouf N, Thornhill MH. Oral cancer cell lines can use multiple ligands, including Fas-L, TRAIL and TNF-α, to induce apoptosis in Jurkat T cells: possible mechanisms for immune escape by head and neck cancers. Oral Oncol 2008;44:672-82. https://doi.org/10.1016/j.oraloncology.2007.08.013 10.1016/j.oraloncology.2007.08.013 [DOI] [PubMed] [Google Scholar]
- 37.Cho YA, Yoon HJ, Lee JI, et al. Relationship between the expression of PDL-1 and tumor infiltrating lymphocytes in oral squamous cell carcinoma. Oral Oncol 2011;47:1148-53. https://doi.org/10.1016/j.oraloncology.2011.08.007 10.1016/j.oraloncology.2011.08.007 [DOI] [PubMed] [Google Scholar]
- 38.Valente G, De Stefani A, Jemma C, et al. Infiltrating leukocyte populations and T-lymphocyte subsets in head and neck squamous cell carcinomas from patients receiving perilymphatic injections of recombinant Interleukin 2. A pathologic and immunophenotypic study. Mod Pathol 1990;3:702-8. [PubMed] [Google Scholar]
- 39.De Ruiter EJ, Ooft ML, Devriese LA, et al. The prognostic role of tumor infiltrating T-lymphocytes in squamous cell carcinoma of the head and neck: a systematic review and meta-analysis. Oncoimmunology 2017;6:e1356148 https://doi.org/10.1080/2162402X.2017.1356148 10.1080/2162402X.2017.1356148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li JZ, Gao W, Chan JY, et al. Hypoxia in head and neck squamous cell carcinoma. ISRN Otolaryngol 2012;2012:708974 https://doi.org/10.5402/2012/708974 10.5402/2012/708974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liang X, Yang D, Hu J, et al. Hypoxia inducible factor alfa expression correlates with vascular endothelial growth factor-C expression and lympahngiogenesis/angiogenesis in oral squamous cell carcinoma. Anticancer Res 2008;28:1659-66. [PubMed] [Google Scholar]
- 42.Karl E, Zhang Z, Dong Z, et al. Unidirectional cross talk between Bcl2-xL and Bcl2 enhances the angiogenic phenotype of endothelial cells. Cell Death Differ 2007;14:1657-66. https://doi.org/10.1038/sj.cdd.4402174 10.1038/sj.cdd.4402174 [DOI] [PubMed] [Google Scholar]
- 43.Huang L, David O, Cabay RJ, et al. Molecular classification of lymph node metastases subtypes predict for survival in head and neck cancer. Clin Cancer Res 2019;25:1795:808. https://doi.org/10.1158/1078-0432.CCR-18-1884 10.1158/1078-0432.CCR-18-1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brierley J D, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours, Eigth Edition Hoboken:Wiley Blackwell; 2017. [Google Scholar]
4. Diagnostic imaging of metastatic disease in head and neck malignancies
- 1.Patkar D, Yanamandala R, Lawande M. Imaging in head and neck cancers. Otorhinolaryngol Clin 2010;2:15-23. https://doi.org/10.5005/jp-journals-10003-1013 10.5005/jp-journals-10003-1013 [DOI] [Google Scholar]
- 2.Singh FM, Mak SY, Bonington SC. Patterns of spread of head and neck adenoid cystic carcinoma. Clin Radiol 2015;70:644-53. https://doi.org/10.1016/j.crad.2015.01.013 10.1016/j.crad.2015.01.013 [DOI] [PubMed] [Google Scholar]
- 3.Allen CT, Law JH, Dunn GP, et al. Emerging insights into head and neck cancer metastasis: metastasis of head and neck cancer. Head Neck 2013;35:1669-78. https://doi.org/10.1002/hed.23202 10.1002/hed.23202 [DOI] [PubMed] [Google Scholar]
- 4.Takes RP, Rinaldo A, Silver CE, et al. Distant metastases from head and neck squamous cell carcinoma. Part I. Basic aspects. Oral Oncol 2012;48:775-9. https://doi.org/10.1016/j.oraloncology.2012.03.013 10.1016/j.oraloncology.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 5.Lewis-Jones H, Colley S, Gibson D. Imaging in head and neck cancer: United Kingdom national multidisciplinary guidelines. J Laryngol Otol 2016;130:S28-31. https://doi.org/10.1017/S0022215116000396 10.1017/S0022215116000396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker M, Zaidi H. Imaging in head and neck squamous cell carcinoma: the potential role of PET/MRI. Br J Radiol 2014;87:20130677 https://doi.org/10.1259/bjr.20130677 10.1259/bjr.20130677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Bree R, Senft A, Coca-Pelaz A, et al. Detection of distant metastases in head and neck cancer: changing landscape. Adv Ther 2018;35:161-72. https://doi.org/10.1007/s12325-018-0662-8 10.1007/s12325-018-0662-8 [DOI] [PubMed] [Google Scholar]
- 8.Ng S, Chan S, Yen T, et al. Comprehensive imaging of residual/recurrent nasopharyngeal carcinoma using whole-body MRI at 3 T compared with FDG-PET-CT. Eur Radiol 2010;20:2229-40. https://doi.org/10.1007/s00330-010-1784-9 10.1007/s00330-010-1784-9 [DOI] [PubMed] [Google Scholar]
- 9.Morsing A, Hildebrandt MG, Vilstrup MH, et al. Hybrid PET/MRI in major cancers: a scoping review. Eur J Nucl Med Mol Imaging 2019;46:2138-51. https://doi.org/10.1007/s00259-019-04402-8 10.1007/s00259-019-04402-8 [DOI] [PubMed] [Google Scholar]
- 10.de Bree R, Deurloo EE, Snow GB, et al. Screening for distant metastases in patients with head and neck cancer. Laryngoscope 2000;110:397-401. https://doi.org/10.1097/00005537-200003000-00012 10.1097/00005537-200003000-00012 [DOI] [PubMed] [Google Scholar]
- 11.Blanchard D, Barry B, De Raucourt D, et al. Guidelines update: post-treatment follow-up of adult head and neck squamous cell carcinoma: screening for metastasis and metachronous esophageal and bronchial locations. Eur Ann Otorhinolaryngol Head Neck Dis 2015;132:217-21. https://doi.org/10.1016/j.anorl.2015.07.001 10.1016/j.anorl.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 12.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 2010;363:24-35. https://doi.org/10.1056/NEJMoa0912217 10.1056/NEJMoa0912217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo Nigro C, Denaro N, Merlotti A, et al. Head and neck cancer: improving outcomes with a multidisciplinary approach. Cancer Manag Res 2017;9:363-71. https://doi.org/10.2147/CMAR.S115761 10.2147/CMAR.S115761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bree RD, Mehta DM, Snow GB, et al. Intracranial metastases in patients with squamous cell carcinoma of the head and neck. Otolaryngol Neck Surg 2001;124:217-21. https://doi.org/10.1067/mhn.2001.112478 10.1067/mhn.2001.112478 [DOI] [PubMed] [Google Scholar]
- 15.Harrison RA, Nam JY, Weathers SP, et al. Intracranial dural, calvarial, and skull base metastases. Handb Clin Neurol 2018;149:205-25. https://doi.org/10.1016/B978-0-12-811161-1.00014-1 10.1016/B978-0-12-811161-1.00014-1 [DOI] [PubMed] [Google Scholar]
- 16.Haughey BH, Arfken CL, Gates GA, et al. Meta-analysis of second malignant tumors in head and neck cancer: the case for an endoscopic screening protocol. Ann Otol Rhinol Laryngol 1992;101:105-12. https://doi.org/10.1177/000348949210100201 10.1177/000348949210100201 [DOI] [PubMed] [Google Scholar]
- 17.Boysen M, Lövdal O, Winther F, et al. The value of follow-up in patients treated for squamous cell carcinoma of the head and neck. Eur J Cancer 1992;28:426-30. https://doi.org/10.1016/S0959-8049(05)80068-1 10.1016/S0959-8049(05)80068-1 [DOI] [PubMed] [Google Scholar]
- 18.de Bree R, Haigentz M, Silver CE, et al. Distant metastases from head and neck squamous cell carcinoma. Part II. Diagnosis. Oral Oncol 2012;48:780-6. https://doi.org/10.1016/j.oraloncology.2012.03.014 10.1016/j.oraloncology.2012.03.014 [DOI] [PubMed] [Google Scholar]
- 19.Ferlito A, Shaha AR, Silver CE, et al. Incidence and sites of distant metastases from head and neck cancer. ORL 2001;63:202-7. https://doi.org/10.1159/000055740 10.1159/000055740 [DOI] [PubMed] [Google Scholar]
- 20.Funk GF. A Head and Neck surgeon’s perspective on best practices for the use of PET/CT scans for the diagnosis and treatment of head and neck cancers. Arch Otolaryngol Neck Surg 2012;138:748-52. https://doi.org/10.1001/archoto.2012.1404 10.1001/archoto.2012.1404 [DOI] [PubMed] [Google Scholar]
- 21.Digonnet A, Hamoir M, Andry G, et al. Post-therapeutic surveillance strategies in head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 2013;270:1569-80. https://doi.org/10.1007/s00405-012-2172-7 10.1007/s00405-012-2172-7 [DOI] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network. NCCN guidelines. Head and neck cancer. http://www.nccn.org/professional/physician_gls/pdf/head-and-neck.pdf. Version 1. 2019
- 23.Digonnet A, Hamoir M, Andry G, et al. Follow-up strategies in head and neck cancer other than upper aerodigestive tract squamous cell carcinoma. Eur Arch Otorhinolaryngol 2013;270:1981-9. https://doi.org/10.1007/s00405-012-2220-3 10.1007/s00405-012-2220-3 [DOI] [PubMed] [Google Scholar]
- 24.Al Tamimi AS, Zaheer S, Ng DC, et al. The incidence and sites of nasopharyngeal carcinoma (NPC) metastases on FDG PET/CT scans. Oral Oncol 2015;51:1047-50. https://doi.org/10.1016/j.oraloncology.2015.08.001 10.1016/j.oraloncology.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 25.Watal P, Bathla G, Thaker S, et al. Multimodality imaging spectrum of the extranodal lymphomas in the head and neck - a pictorial review. Curr Probl Diagn Radiol 2018;47:340-52. https://doi.org/10.1067/j.cpradiol.2017.07.007 10.1067/j.cpradiol.2017.07.007 [DOI] [PubMed] [Google Scholar]
5. Head and neck cancer distant metastases
- 1.Kuperman DI, Auethavekiat V, Adkins DR, et al. Squamous cell cancer of the head and neck with distant metastasis at presentation. Head Neck 2011;33:714-8. https://doi.org/10.1002/hed.21529 10.1002/hed.21529 [DOI] [PubMed] [Google Scholar]
- 2.Deurvorst SE, Hoekstra OS, Castelijns JA, et al. Clinical value of 18FDG PET/CT in screening for distant metastases in head and neck squamous cell carcinoma. Clin Otolaryngol 2018;43:875-81. https://doi.org/10.1111/coa.13074 10.1111/coa.13074 [DOI] [PubMed] [Google Scholar]
- 3.Brouwer J, Bree R, Hoekstra OS, et al. Screening for distant metastases in patients with head and neck cancer: what is the current clinical practice? Clin Otolaryngol 2005;30:438-43. https://doi.org/10.1111/j.1365-2273.2005.01068.x 10.1111/j.1365-2273.2005.01068.x [DOI] [PubMed] [Google Scholar]
- 4.Leon X, Quer M, Orus C, et al. Distant metastases in head and neck cancer patients who achieved loco-regional control. Head Neck 2000;22:680-6. https://doi.org/10.1002/1097-0347(200010)22:7<680::aid-hed7>3.0.co;2-j [DOI] [PubMed] [Google Scholar]
- 5.Li X, Di B, Shang Y, et al. Clinicopathologic risk factors for distant metastases from head and neck squamous cell carcinomas. Eur J Surg Oncol 2009;35:1348-53. https://doi.org/10.1016/j.ejso.2009.06.010 10.1016/j.ejso.2009.06.010 [DOI] [PubMed] [Google Scholar]
- 6.Fortin A, Couture C, Doucet R, et al. Does histologic grade have a role in the management of head and neck cancers? J Clin Oncol 2001;19:4107-16. https://doi.org/10.1200/JCO.2001.19.21.4107 10.1200/JCO.2001.19.21.4107 [DOI] [PubMed] [Google Scholar]
- 7.Spector JG, Sessions DG, Haughey BH, et al. Delayed regional metastases, distant metastases, and second primary malignancies in squamous cell carcinomas of the larynx and hypopharynx. Laryngoscope 2001;111:1079-87. https://doi.org/10.1097/00005537-200106000-00028 10.1097/00005537-200106000-00028 [DOI] [PubMed] [Google Scholar]
- 8.Al-Othman MO, Morris CG, Hinerman RW, et al. Distant metastases after definitive radiotherapy for squamous cell carcinoma of the head and neck. Head Neck 2003;25:629-33. https://doi.org/10.1002/hed.10275 10.1002/hed.10275 [DOI] [PubMed] [Google Scholar]
- 9.Carvalho AL, Magrin J, Kowalski LP. Sites of recurrence in oral and oropharyngeal cancers according to the treatment approach. Oral Dis 2003;9:112-8. https://doi.org/10.1034/j.1601-0825.2003.01750.x 10.1034/j.1601-0825.2003.01750.x [DOI] [PubMed] [Google Scholar]
- 10.Kowalski LP, Carvalho AL, Martins Priante AV, et al. Predictive factors for distant metastasis from oral and oropharyngeal squamous cell carcinoma. Oral Oncol 2005;41:534-41. https://doi.org/10.1016/j.oraloncology.2005.01.012 10.1016/j.oraloncology.2005.01.012 [DOI] [PubMed] [Google Scholar]
- 11.Garavello W, Ciardo A, Spreafic R, et al. Risk factors for distant metastases in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 2006;132:762-6. https://doi.org/10.1001/archotol.132.7.762 10.1001/archotol.132.7.762 [DOI] [PubMed] [Google Scholar]
- 12.Bourhis J, Overgaard J, Audry H, et al. Hyperfractionated or accelerated radiotherapy in head and neck cancer: a meta-analysis. Lancet 2006;368:843-54. https://doi.org/10.1016/S0140-6736(06)69121-6 10.1016/S0140-6736(06)69121-6 [DOI] [PubMed] [Google Scholar]
- 13.Lim JY, Lim YC, Kim SH, et al. Predictive factors of isolated distant metastasis after primary definitive surgery without systemic treatment for head and neck squamous cell carcinoma. Oral Oncol 2010;46:504-8. https://doi.org/10.1016/j.oraloncology.2010.02.005 10.1016/j.oraloncology.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 14.van der Schroeff MP, Steyerberg EW, Wieringa MH, et al. Prognosis: a variable parameter: dynamic prognostic modeling in head and neck squamous cell carcinoma. Head Neck 2012;34:34-41. https://doi.org/10.1002/hed.21693 10.1002/hed.21693 [DOI] [PubMed] [Google Scholar]
- 15.Kjems J, Gothelf AB, Hakansson K, et al. Elective nodal irradiation and patterns of failure in head and neck cancer after primary radiation therapy. Int J Radiat Oncol Biol Phys 2016;94:775-82. https://doi.org/10.1016/j.ijrobp.2015.12.380 10.1016/j.ijrobp.2015.12.380 [DOI] [PubMed] [Google Scholar]
- 16.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 17.Liu JC, Bhayani M, Kuchta K, et al. Patterns of distant metastasis in head and neck cancer at presentation: Implications for initial evaluation. Oral Oncol 2019;88:131-6. https://doi.org/10.1016/j.oraloncology.2018.11.023 10.1016/j.oraloncology.2018.11.023 [DOI] [PubMed] [Google Scholar]
- 18.Black RJ, Gluckman JL, Shumrick DA. Screening for distant metastases in head and neck cancer patients. Aust N Z J Surg 1984;54:527-30. https://doi.org/10.1111/j.1445-2197.1984.tb05440.x 10.1111/j.1445-2197.1984.tb05440.x [DOI] [PubMed] [Google Scholar]
- 19.de Bree R, Deurloo EE, Snow GB. Screening for distant metastasis in patients with head and neck cancer. Laryngoscope 2000;110:397-401. https://doi.org/10.1097/00005537-200003000-00012 10.1097/00005537-200003000-00012 [DOI] [PubMed] [Google Scholar]
- 20.Jackel MC, Rausch H. Distant metastasis of squamous epithelial carcinomas of the upper aerodigestive tract. The effect of clinical tumor parameters and course of illness. HNO 1999;47:38-44. https://doi.org/10.1007/s001060050356 10.1007/s001060050356 [DOI] [PubMed] [Google Scholar]
- 21.Li Y, Ou X, Hu C. Prevalence and prognostic impact of synchronous distant metastases in patients with hypopharynx squamous cell carcinomas: a SEER-based study. J Cancer 2019;10:620-6. https://doi.org/10.7150/jca.28554 10.7150/jca.28554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haerle SK, Schmid DT, Ahmad N, et al. The value of (18) F-FDG PET/CT for the detection of distant metastases in high-risk patients with head and neck squamous cell carcinoma. Oral Oncol 2011;47:653-9. https://doi.org/10.1016/j.oraloncology.2011.05.011 10.1016/j.oraloncology.2011.05.011 [DOI] [PubMed] [Google Scholar]
- 23.Fogh SE, Kubicek GJ, Champ C, et al. Value of fluoro-2-deoxy-D-glucose-positron emission tomography for detecting metastatic lesions in head and neck cancer. Am J Clin Oncol 2012;35:311-5. https://doi.org/10.1097/COC.0b013e3181ec5f2e 10.1097/COC.0b013e3181ec5f2e [DOI] [PubMed] [Google Scholar]
- 24.Grisanti S, Bianchi S, Locati LD, et al. Bone metastases from head and neck malignancies: prognostic factors and skeletal-related events. PLoS One 2019;14:e0213934 https://doi.org/10.1371/journal.pone.0213934 10.1371/journal.pone.0213934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhatia R, Bahadur S. Distant metastasis in malignancies of head and neck. J Laryngol Otol 1987;101:925-8. https://doi.org/10.1017/s0022215100102993 10.1017/s0022215100102993 [DOI] [PubMed] [Google Scholar]
- 26.Wiegand S, Zimmermann A, Wilhelm T, et al. Survival after distant metastasis in head and neck cancer. Anticancer Res 2015;35:5499-502. [PubMed] [Google Scholar]
- 27.Alvi A, Johnson JT. Development of distant metastasis after treatment of advanced-stage head and neck cancer. Head Neck 1997;19:500-5. https://doi.org/10.1002/(sici)1097-0347(199709)19:6<500::aid-hed7>3.0.co;2-2 [DOI] [PubMed] [Google Scholar]
- 28.Ferlito A, Shaha AR, Silver CE, et al. Incidence and sites of distant metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec 2001;63:202-7. https://doi.org/10.1159/000055740 10.1159/000055740 [DOI] [PubMed] [Google Scholar]
- 29.Kim Y, Roh JL, Kim JS, et al. Chest radiography or chest CT plus head and neck CT versus 18F-FDG PET/CT for detection of distant metastasis and synchronous cancer in patients with head and neck cancer. Oral Oncol 2019;88:109-14. https://doi.org/10.1016/j.oraloncology.2018.11.026 10.1016/j.oraloncology.2018.11.026 [DOI] [PubMed] [Google Scholar]
- 30.Senft A, Hoekstra OS, Castelijns JA, et al. Pretreatment screening for distant metastases in the Dutch head and neck centers: 10 years later. Eur Arch Otorhinolaryngol 2016;273:3287-91. https://doi.org/10.1007/s00405-016-3897-5 10.1007/s00405-016-3897-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grégoire V, Lefebvre JL, Licitra L, et al. Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010;21(Suppl 5):v184-6. https://doi.org/10.1093/annonc/mdq185 10.1093/annonc/mdq185 [DOI] [PubMed] [Google Scholar]
- 32.NCCN clinical practice guidelines in oncology (NCCN Guidelines). Head and neck cancers, version 1.2016. NCCN website. http://oralcancerfoundation.org/wpcontent/uploads/2016/09/head-and-neck.pdf. Accessed August 31, 2017.
- 33.Rohde M, Nielsen AL, Johansen J, et al. Head-to-head comparison of chest X-ray/head and neck MRI, chest CT/head and neck MRI, and 18F-FDG PET/CT for detection of distant metastases and synchronous cancer in oral, pharyngeal, and laryngeal cancer. J Nucl Med 2017;58:1919-24. https://doi.org/10.2967/jnumed.117.189704 10.2967/jnumed.117.189704 [DOI] [PubMed] [Google Scholar]
6. Distant metastases in EBV- and HPV-related squamous cell carcinomas
- 1.Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma. Lancet 2019;394:64-80. https://doi.org/10.1016/S0140-6736(19)30956-0 10.1016/S0140-6736(19)30956-0 [DOI] [PubMed] [Google Scholar]
- 2.Yeo ELL, Li YQ, Soo KC, et al. Combinatorial strategies of radiotherapy and immunotherapy in nasopharyngeal carcinoma. Chin Clin Oncol 2018;7:15 https://doi.org/10.21037/cco.2018.04.05 10.21037/cco.2018.04.05 [DOI] [PubMed] [Google Scholar]
- 3.Brierley J D, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours, Eigth Edition Hoboken: Wiley Blackwell; 2017. [Google Scholar]
- 4.Ferrari D, Codecà C, Bertuzzi C, et al. Role of plasma EBV DNA levels in predicting recurrence of nasopharyngeal carcinoma in a Western population. BMC Cancer 2012;12:208 https://doi.org/10.1186/1471-2407-12-208 10.1186/1471-2407-12-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakanishi Y, Wakisaka N, Kondo S, et al. Progression of understanding for the role of Epstein-Barr virus and management of nasopharyngeal carcinoma. Cancer Metastasis Rev 2017;36:435-47. https://doi.org/10.1007/s10555-017-9693-x 10.1007/s10555-017-9693-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J, Shu C, Song Y, et al. Epstein-Barr virus DNA level as a novel prognostic factor in nasopharyngeal carcinoma. Medicine (Baltimore) 2016;95:e5130 https://doi.org/10.1097/MD.0000000000005130 10.1097/MD.0000000000005130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lertbutsayanukul C, Kannarunimit D, Prayongrat A, et al. Prognostic value of plasma EBV DNA for nasopharyngeal cancer patients during treatment with intensity-modulated radiation therapy and concurrent chemotherapy. Radiol Oncol 2018;52:195-203. https://doi.org/10.2478/raon-2018-0016 10.2478/raon-2018-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li SW, Wang H, Xiang YQ, et al. Prospective study of prognostic value of Raf kinase inhibitory protein and pretreatment plasma Epstein-Barr virus DNA for distant metastasis in locoregionally advanced nasopharyngeal carcinoma. Head Neck 2013;35:579-81. https://doi.org/10.1002/hed.23009 10.1002/hed.23009 [DOI] [PubMed] [Google Scholar]
- 9.Liu TB, Zheng ZH, Pan J, et al. Prognostic role of plasma Epstein-Barr virus DNA load for nasopharyngeal carcinoma: a meta-analysis. Clin Invest Med 2017;40:E1-E12. https://doi.org/10.25011/cim.v40i1.28049 10.25011/cim.v40i1.28049 [DOI] [PubMed] [Google Scholar]
- 10.Zhou X, Yang Y, Ou X, et al. Interplay of tumor spread, volume and Epstein-Barr virus DNA in nasopharyngeal carcinoma: feasibility of an integrative risk stratification scheme. J Cancer 2018;9:4271-8. https://doi.org/10.7150/jca.26777 10.7150/jca.26777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen QY, Guo SY, Tang LQ, et al. Combination of tumor volume and Epstein-Barr virus DNA improved prognostic stratification of stage II nasopharyngeal carcinoma in the intensity-modulated radiotherapy era: a large-scale cohort study. Cancer Res Treat 2018;50:861-71. https://doi.org/10.4143/crt.2017.237 10.4143/crt.2017.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alfieri S, Iacovelli NA, Marceglia S, et al. Circulating pre-treatment Epstein-Barr virus DNA as prognostic factor in locally-advanced nasopharyngeal carcinoma in a non-endemic area. Oncotarget 2017;8:47780-9. https://doi.org/10.18632/oncotarget.17822 10.18632/oncotarget.17822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang W, Chen Y, Chen L, et al. The clinical utility of plasma Epstein-Barr DNA assays in nasopharyngeal carcinoma: the dawn of a new era? Medicine (/Baltimore) 2015;94:e845 https://doi.org/10.1097/MD.0000000000000845 10.1097/MD.0000000000000845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin J, Xie G, Liao G, et al. Prognostic value of 18F-FDG-PET/CT in patients with nasopharyngeal carcinoma: a systematic review and meta-analysis. Oncotarget 2017;8:33884-96. https://doi.org/10.18632/oncotarget.13934 10.18632/oncotarget.13934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AJCC (American Joint Committee on Cancer) Cancer Staging Manual - Seventh Edition - New York, NY: Springer; 2010. [Google Scholar]
- 16.Jin YN, Yao JJ, Wang SY, et al. Prognostic value of primary gross tumor volume and standardized uptake value of 18F-FDG in PET/TC for distant metastases in locoregionally advanced nasopharyngeal carcinoma. Tumor Biol 2017;39:1010428317717843 https://doi.org/10.1177/1010428317717843 10.1177/1010428317717843 [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Huang Y, Hong S, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomized, open-label phase 3 trial. Lancet 2016;388;1883-92. https://doi.org/10.1016/S0140-6736(16)31388-5 (erratum in: Lancet 2016;388:1882) 10.1016/S0140-6736(16)31388-5 [DOI] [PubMed] [Google Scholar]
- 18.Liu LT, Chen QY, Tang LQ, et al. Neoadjuvant or adjuvant chemotherapy plus concurrent CRT versus concurrent CRT alone in the treatment of nasopharyngeal carcinoma: a study based on EBV-DNA. J Natl Compr Canc Netw 2019;17:703-10. https://doi.org/10.6004/jnccn.2018.7270 10.6004/jnccn.2018.7270 [DOI] [PubMed] [Google Scholar]
- 19.Sun XS, Liang YJ, Liu SL, et al. Subdivision of nasopharyngeal carcinoma patients with bone-only metastasis at diagnosis for prediction of survival and treatment guidance. Cancer Res Treat 2019;51:1259-68. https://doi.org/10.4143/crt.2018.652 10.4143/crt.2018.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lv JW, Li JY, Luo LN, et al. Comparative safety and efficacy of anti-PD-1 monotherapy, chemotherapy alone, and their combination therapy in advanced nasopharyngeal carcinoma: findings from recent advances in landmarks trials. J Immunother Cancer 2019;7:159 https://doi.org/10.1186/s40425-019-0636-7 10.1186/s40425-019-0636-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Resteghini C, Alfieri S, Quattrone P, et al. RANK expression in EBV positive nasopharyngeal carcinoma metastasis: a read- to-treat target? Oncotarget 2017;8:96184-9. https://doi.org/10.18632/oncotarget.21856 10.18632/oncotarget.21856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Martel C, Plummer M, Vignat J, et al. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer 2017;141:664-70. https://doi.org/10.1002/ijc.30716 10.1002/ijc.30716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larsen CG, Jensen DH, Carlander AF, et al. Novel nomograms for survival and progression in HPV+ HPV- oropharyngeal cancer: a population-based study of 1,542 consecutive patients. Oncotarget 2016;7:71761-72. https://doi.org/10.18632/oncotarget.12335 10.18632/oncotarget.12335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tiedemann D, Jakobsen KK, Von Buchwald C, et al. Systematic review on location and timing of distant progression in human papillomavirus-positive and human papillomavirus-negative oropharyngeal squamous cell carcinomas. Head Neck 2019;41:793-8. https://doi.org/10.1002/hed.25458 10.1002/hed.25458 [DOI] [PubMed] [Google Scholar]
- 25.O’Sullivan B, Huang SH, Siu LL, et al. Deintensification candidate subgroups in human papillomavirus-related oropharyngeal cancer according to minimal risk of distant metastases. J Clin Oncol 2013;31:543-50. https://doi.org/10.1200/JCO.2012.44.0164 10.1200/JCO.2012.44.0164 [DOI] [PubMed] [Google Scholar]
- 26.Huang SH, Perez-Ordonez B, Weinreb I, et al. Natural course of distant metastases following radiotherapy or chemoradiotherapy in HPV-related oropharyngeal cancer. Oral Oncol 2013;49:79-85. https://doi.org/10.1016/j.oraloncology.2012.07.015 10.1016/j.oraloncology.2012.07.015 [DOI] [PubMed] [Google Scholar]
- 27.Sinha P, Thorstad WT, Nussenbaum B, et al. Distant metastasis in p16-positive oropharyngeal squamous cell carcinoma: a critical analysis of patterns and outcomes. Oral Oncol 2014;50:45-51. https://doi.org/10.1016/j.oraloncology.2013.10.007 10.1016/j.oraloncology.2013.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trosman SJ, Koyfman SA, Ward MC, et al. Effect of human papillomavirus on patterns of distant metastatic failure in oropharyngeal squamous cell carcinoma treated with chemoradiotherapy. JAMA Otolaryngol Head Neck Surg 2015;141:457-62. https://doi.org/10.1001/jamaoto.2015.136 10.1001/jamaoto.2015.136 [DOI] [PubMed] [Google Scholar]
- 29.Dok R, Glorieux M, Holacka K, et al. Dual role for p16 in the metastasis process of HPV positive head and neck cancers. Mol Cancer 2017;16:113 https://doi.org/10.1186/s12943-017-0678-8 10.1186/s12943-017-0678-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Urban D, Corry J, Rischin D. What is the best treatment for patients with human papillomavirus-positive and -negative oropharyngeal cancer? Cancer 2014;120:1462-70. https://doi.org/10.1002/cncr.28595 10.1002/cncr.28595 [DOI] [PubMed] [Google Scholar]
- 31.Bourhis J, Overgaard J, Audry H, et al. Hyperfractionated or accelerated radiotherapy in head and neck cancer: a meta-analysis. Lancet 2006;368:843-54. https://doi.org/10.1016/S0140-6736(06)69121-6 10.1016/S0140-6736(06)69121-6 [DOI] [PubMed] [Google Scholar]
- 32.Lacab B, Bourhis J, Overgaard J, et al. Role of radiotherapy fractionation in head and neck cancers (MARCH): an updated meta-analysis. Lancet Oncol 2017;18:1221-37. https://doi.org/10.1016/S1470-2045(17)30458-8 10.1016/S1470-2045(17)30458-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lassen P, Lacas B, Pignon JP, et al. Prognostic impact of HPV-associated p16-expression and smoking status on outcomes following radiotherapy for oropharyngeal cancer: The MARCH- HPV project. Radiother Oncol 2018;126:107-15. https://doi.org/10.1016/j.radonc.2017.10.018 10.1016/j.radonc.2017.10.018 [DOI] [PubMed] [Google Scholar]
- 34.Weller MA, Ward MC, Berriochoa C, et al. Predictors of distant metastasis in human papillomavirus-associated oropharyngeal cancer. Head Neck 2017;39:940-6. https://doi.org/10.1002/hed.24711 10.1002/hed.24711 [DOI] [PubMed] [Google Scholar]
- 35.Spector ME, Chinn SB, Bellile E, et al. Matted nodes as a predictor of distant metastasis in advanced-stage III/IV oropharyngeal squamous cell carcinoma. Head Neck 2016;38:184-90. https://doi.org/10.1002/hed.23882 10.1002/hed.23882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vainshtein JM, Spector ME, Ibrahim M, et al. Matted nodes: high distant-metastasis risk and a potential indication for intensification of systemic therapy in human papillomavirus-related oropharyngeal cancer. Head Neck 2016;38(Suppl 1):E805-14. https://doi.org/10.1002/hed.24105 10.1002/hed.24105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rasmussen JH, Grønhøj C, Hakansson K, et al. Risk profiling based on p16 and HPV DNA more accurately predicts location of disease relapse in patients with oropharyngeal squamous cell carcinoma. Ann Oncol 2019;30:629-36. https://doi.org/10.1093/annonc/mdz010 10.1093/annonc/mdz010 [DOI] [PubMed] [Google Scholar]
- 38.Rieckmann T, Kriegs M. The failure of cetuximab-based de-intensified regimes for HPV-positive OPSCC: a radiobiologists perspective. Clin Transl Radiat Oncol 2019;17:47-50. https://doi.org/10.1016/j.ctro.2019.05.003 10.1016/j.ctro.2019.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhattasali O, Ryoo JJ, Thompson LDR, et al. Impact of chemotherapy regimen on treatment outcomes in patients with HPV-associated oropharyngeal cancer with T4 disease treated with definitive concurrent chemoradiation. Oral Oncol 2019;95:74-8. https://doi.org/10.1016/j.oraloncology.2019.06.007 10.1016/j.oraloncology.2019.06.007 [DOI] [PubMed] [Google Scholar]
- 40.Shibata T, Lieblong BJ, Sasagawa T, et al. The promise of combining cancer vaccine and checkpoint blockade for treating HPV-related cancer. Cancer Treat Rev 2019;78:8-16. https://doi.org/10.1016/j.ctrv.2019.07.001 10.1016/j.ctrv.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frazer IH, Chandra J. Immunotherapy for HPV associated cancer. Papillomavirus Res 2019;8:100176 https://doi.org/10.1016/j.pvr.2019.100176 10.1016/j.pvr.2019.100176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen EEW, Soulières D, Le Tourneau C, et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head and neck squamous cell carcinoma (KEYNOTE-040): a randomized, open-label, phase 3 study. Lancet 2019;393:156-67. https://doi.org/10.1016/S0140-6736(18)31999-8 10.1016/S0140-6736(18)31999-8 [DOI] [PubMed] [Google Scholar]
- 43.Mehra R, Seiwert TY, Gupta S, et al. Efficacy and safety of pembrolizumab in recurrent/metastatic head and neck squamous cell carcinoma: pooled analyses after long term follow-up in KEYNOTE-012. Br J Cancer 2018;119:153-9. https://doi.org/10.1038/s41416-018-0131-9 10.1038/s41416-018-0131-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bauml J, Seiwert TY, Pfister DG, et al. Pembrolizumab for platinum- and cetuximab- refractory head and neck cancer: results from a single arm, phase II study. J Clin Oncol 2017;35:1542-9. https://doi.org/10.1200/JCO.2016.70.1524 10.1200/JCO.2016.70.1524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gillison ML, Blumenschein G, Jr, Fayette J, et al. Check-Mate 141: 1-year update and subgroup analysis of nivolumab as first line therapy in patients with recurrent/metastatic head and neck cancer. Oncologist 2018;23:1079-82. https://doi.org/10.1634/theoncologist.2017-0674 10.1634/theoncologist.2017-0674 [DOI] [PMC free article] [PubMed] [Google Scholar]
7. Cervical lymph nodes metastases from distant infraclavicular tumors
- 1.Sagheb K, Manz A, Albrich SB, et al. Supraclavicular metastases from distant primary solid tumours: a retrospective study of 41 years. J Maxillofac Oral Surg 2017;16:152-7. https://doi.org/10.1007/s12663-016-0910-x 10.1007/s12663-016-0910-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rusthoven KE, Koshy M, Paulino AC. The role of fluorodeoxyglucose positron emission tomography in cervical lymph node metastases from an unknown primary tumor. Cancer 2004;101:2641-9. https://doi.org/10.1002/cncr.20687 10.1002/cncr.20687 [DOI] [PubMed] [Google Scholar]
- 3.Franzen A, Günzel T, Buchali A, et al. Etiologic and differential diagnostic significance of tumor location in the supraclavicular fossa. Laryngoscope 2018;128:646-50. https://doi.org/10.1002/lary.26775 10.1002/lary.26775 [DOI] [PubMed] [Google Scholar]
- 4.Virchow RLK. Zur diagnose der krebse im unterleibe. Med Reform 1848;45:248. [Google Scholar]
- 5.Fernàndez Aceñero MJ, Caso Viesca A, Diaz del Arco C. Role of fine needle aspiration citology in the management of supraclavicular lymph node metastasis: review of our experience. Diagn Cytopathol 2019;47:181-6. https://doi.org/10.1002/dc.24064 10.1002/dc.24064 [DOI] [PubMed] [Google Scholar]
- 6.Troisier CE. L’adenopathie sus-claviculaire dans les cancers de l’abdomen. Arch Gén Méd 1889;1:129-38, 297-309. [Google Scholar]
- 7.Stevens WM. The dissemination of intra-abdominal malignant disease by means of the lymphatics and thoracic duct. Br Med J 1907;1:306-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lopez F, Rodrigo JP, Silver CE, et al. Cervical lymph node metastases from remote primary tumor sites. Head Neck 2016;38(Suppl 1):E2374-85. https://doi.org/10.1002/hed.24344 10.1002/hed.24344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakurai N, Tateoka K, Fukaya K, et al. Supraclavicular lymph node metastasis as the initial presentation of primary fallopian tube carcinoma. Int J Clin Oncol 2010;15:301-4. https://doi.org/10.1007/s10147-010-0030-4 10.1007/s10147-010-0030-4 [DOI] [PubMed] [Google Scholar]
- 10.Gupta RK, Naran S, Lallu S, et al. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology 2003;14:201-7. https://doi.org/10.1046/j.1365-2303.2003.00057.x 10.1046/j.1365-2303.2003.00057.x [DOI] [PubMed] [Google Scholar]
- 11.Kuemper C, Burges A, Hillemanns P, et al. Supraclavicular lymph node metastases of unknown origin: HPV-typing identifies the primary tumour. Eur J Cancer Care 2009;18:606-11. https://doi.org/10.1111/j.1365-2354.2008.00937.x 10.1111/j.1365-2354.2008.00937.x [DOI] [PubMed] [Google Scholar]
- 12.Ismi O, Vasyisoglu Y, Ozcan C, et al. Supraclavicular metastasis from infraclavicular organs: retrospective analysis of 18 patients. Int J Cancer Manag 2017;10:e4720 https://doi.org/10.5812/ijcm.4720 10.5812/ijcm.4720 [DOI] [Google Scholar]
- 13.Lee JR, Kim JS, Roh JL, et al. Detection of occult primary tumors in patients with cervical metastases of unknown primary tumors: comparison of (18)F FDG PET/CT with contrast-enhanced CT or CT/MR imaging-prospective study. Radiology 2015;274:764-71. https://doi.org/10.1148/radiol.14141073 10.1148/radiol.14141073 [DOI] [PubMed] [Google Scholar]
- 14.Feng ZX, Zhao LJ, Guan Y, et al. Identification of risk factors and characteristics of supraclavicular lymph node metastasis in patients with small cell lung cancer. Med Oncol 2013;30:493 https://doi.org/10.1007/s12032-013-0493-z 10.1007/s12032-013-0493-z [DOI] [PubMed] [Google Scholar]
- 15.Sihoe AD, Lee TW, Ahuja AT, et al. Should cervical ultrasonography be a routine staging investigation for lung cancer patients with impalpable cervical lymph nodes? Eur J Cardiothorac Surg 2004;25:486-91. https://doi.org/10.1016/j.ejcts.2003.12.026 10.1016/j.ejcts.2003.12.026 [DOI] [PubMed] [Google Scholar]
- 16.Stigt JA, Boers JE, Boomsma MF. Ultrasound-guided tissue core biopsies in supraclavicular lymph nodes in patients with suspected thoracic malignancies. Respiration 2015;90:412-5. https://doi.org/10.1159/000441301 10.1159/000441301 [DOI] [PubMed] [Google Scholar]
- 17.Ansari NA, Derias NW. Diagnosis of malignant mesothelioma by fine needle aspiration of a cervical lymph node. A case report. Acta Cytol 2000;44:70-4. https://doi.org/10.1159/000326229 10.1159/000326229 [DOI] [PubMed] [Google Scholar]
- 18.Olivotto IA, Chua B, Allan SJ, et al. Long-term survival of patients with supraclavicular metastases at diagnosis of breast cancer. J Clin Oncol 2003;21:851-4. https://doi.org/10.1200/JCO.2003.11.105 10.1200/JCO.2003.11.105 [DOI] [PubMed] [Google Scholar]
- 19.Liu XH, Zhang L, Chen B. A meta-analysis of the prognosis in patients with breast cancer with ipsilateral supraclavicular lymph node metastasis versus patients with stage IIIb/c or IV breast cancer. Chronic Dis Transl Med 2016;19:236-42. https://doi.org/10.1016/j.cdtm.2016.01.002 10.1016/j.cdtm.2016.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bisase B, Kerawala C. Survey of UK practice for management of breast cancer metastases to the neck. Ann R Coll Surg Engl 2012;94:484-9. https://doi.org/10.1308/003588412X13171221591736 10.1308/003588412X13171221591736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Y, Zhu L, Xia W, et al. Anatomy of lymphatic drainage of the esophagus and lymph node metastasis of thoracic esophageal cancer. Cancer Manag Res 2018;10:6295-03. https://doi.org/10.2147/CMAR.S182436 10.2147/CMAR.S182436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.AJCC (American Joint Committee on Cancer). Cancer Staging Manual - Seventh Edition New York, NY: Springer; 2010. [Google Scholar]
- 23.Tachimori Y, Ozawa S, Numasaki H, et al. Supraclavicular node metastasis from thoracic esophageal carcinoma: a surgical series from a Japanese multi-institutional nationwide registry of esophageal cancer. J Thorac Cardiovasc Surg 2014;148:1224-9. https://doi.org/10.1016/j.jtcvs.2014.02.008 10.1016/j.jtcvs.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 24.Takashima T, Nakata B, Hatama M, et al. Gastric cancer with cervical lymph node metastasis as first presentation: report of a case. Int Surg 2008;93:295-9. [PubMed] [Google Scholar]
- 25.Lieder A, Guenzel T, Lebentrau S, et al. Diagnostic relevance of metastatic renal cell carcinoma in the head and neck: an evaluation of 22 cases in 671 patients. Int Braz J Urol 2017;43:202-8. https://doi.org/10.1590/S1677-5538.IBJU.2015.0665 10.1590/S1677-5538.IBJU.2015.0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hematpour K, Bennett CJ, Rogers D, et al. Supraclavicular lymph node: incidence of unsuspected metastatic prostate cancer. Eur Arch Otorhinolaryngol 2006;263:872-4. https://doi.org/10.1007/s00405-006-0066-2 10.1007/s00405-006-0066-2 [DOI] [PubMed] [Google Scholar]
- 27.Baum SH, Mohr C. Metastases from distant primary tumours on the head and neck: clinical manifestation and diagnostics of 91 cases. Oral Maxillofac Surg 2018;22:119-28. https://doi.org/10.1007/s10006-018-0677-y 10.1007/s10006-018-0677-y [DOI] [PubMed] [Google Scholar]
8. Parenchymal metastases to the head and neck
- 1.Meyer I, Shklar G. Malignant tumors metastatic to mouth and jaws. Oral Surg Oral Med Oral Pathol 1965;20:350-62. [DOI] [PubMed] [Google Scholar]
- 2.Batson OV. The function of the vertebral veins and their role in the spread of metastases. Ann Surg 1940;112:138-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baum SH, Mohr C. Metastases from distant primary tumours on the head and neck: clinical manifestation and diagnostic of 91 cases. Oral Maxillofac Surg 2018;22:119-28. https://doi.org/10.1007/s10006-018-0677-y 10.1007/s10006-018-0677-y [DOI] [PubMed] [Google Scholar]
- 4.Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. https://doi.org/10.1200/JCO.1995.13.1.8 10.1200/JCO.1995.13.1.8 [DOI] [PubMed] [Google Scholar]
- 5.Ashworth A, Rodrigues G, Boldt G, et al. Is there an oligometastatic state in non-small cell lung cancer? A systematic review of the literature. Lung Cancer 2013;82:197-203. https://doi.org/10.1016/j.lungcan.2013.07.026 10.1016/j.lungcan.2013.07.026 [DOI] [PubMed] [Google Scholar]
- 6.Ashworth AB, Senan S, Palma DA, et al. An individual patient data metaanalysis of outcomes and prognostic factors after treatment of oligometastatic non-small-cell lung cancer. Clin Lung Cancer 2014;15:346-55. https://doi.org/10.1016/j.cllc.2014.04.003 10.1016/j.cllc.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 7.Gubens MA, Davies M. NCCN guidelines updates: new immunotherapy strategies for improving outcomes in non-small cell lung cancer. J Natl Compr Netw 2019;17:574-8. https://doi.org/10.6004/jnccn.2019.5005 10.6004/jnccn.2019.5005 [DOI] [PubMed] [Google Scholar]
- 8.Pacheco JM, Camidge DR, Doebele RC, et al. A changing of the guard: immune checkpoint inhibitors with and without chemotherapy as first line treatment for metastatic non-small cell lung cancer. Front Oncol 2019;9:195 https://doi.org/10.3389/fonc.2019.00195 10.3389/fonc.2019.00195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frederickson AM, Arndorfer S, Zhang I, et al. Pembrolizumab plus chemotherapy for first-line treatment of metastatic non squamous non-small-cell lung cancer: a network meta-analysis. Immunotherapy 2019;11:407-28. https://doi.org/10.2217/imt-2018-0193 10.2217/imt-2018-0193 [DOI] [PubMed] [Google Scholar]
- 10.Goldhirsch A, Ingle JN, Gelber RD, et al. Thresholds for therapies: highlights of the St Gallen International Consensus on the primary therapy of early breast cancer 2009. Annal Oncol 2009;20:1319-29. https://doi.org/10.1093/annonc/mdp322 10.1093/annonc/mdp322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Q, Li J, Zhu S, et al. Breast cancer subtypes predict the preferential site of distant metastases: a SEER based study. Oncotarget 2017;8:27990-6. https://doi.org/10.18632/oncotarget.15856 10.18632/oncotarget.15856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiao W, Zheng S, Yang A, et al. Breast cancer subtypes and the risk of distant metastasis at initial diagnosis: a population-based study. Cancer Manag Res 2018;10:5329-38. https://doi.org/10.2147/CMAR.S176763 10.2147/CMAR.S176763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gondim DD, Chernock R, El-Mofty S, et al. The great mimicker: metastatic breast carcinoma to the head and neck with emphasis on unusual clinical and pathologic features. Head Neck Pathol 2017;11:306-13. https://doi.org/10.1007/s12105-016-0768-8 10.1007/s12105-016-0768-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Telli ML, Gradishar WJ, Ward JH. NCCN guidelines updates: breast cancer. J Natl Compr Canc Netw 2019;17:552-5. https://doi.org/10.6004/jnccn.2019.5006 10.6004/jnccn.2019.5006 [DOI] [PubMed] [Google Scholar]
- 15.Pritchyk KM, Schiff BA, Newkirk KA, et al. Metastatic renal cell carcinoma to the head and neck. Laryngoscope 2002;112:1598-602. https://doi.org/10.1097/00005537-200209000-00012 10.1097/00005537-200209000-00012 [DOI] [PubMed] [Google Scholar]
- 16.Lieder A, Guenzel T, Lebentrau S, et al. Diagnostic relevance of metastatic renal cell carcinoma in the head and neck: an evaluation of 22 cases in 671 patients. Int Braz J Urol 2017;43:202-8. https://doi.org/10.1590/S1677-5538.IBJU.2015.0665 10.1590/S1677-5538.IBJU.2015.0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyamoto R, Helmus C. Hypernephroma metastatic to the head and neck. Laryngoscope 1973;83:898-905. [DOI] [PubMed] [Google Scholar]
- 18.Jonasch E. NCCN Guidelines updates: management of metastatic kidney cancer. J Natl Compr Canc Netw 2019;17:587-9. https://doi.org/10.6004/jnccn.2019.5008 10.6004/jnccn.2019.5008 [DOI] [PubMed] [Google Scholar]
- 19.Shen ML, Kang J, Wen YL, et al. Metastatic tumors to the oral and maxillofacial region: a retrospective study of 19 cases in West China and review of the Chinese and English literature. J Oral Maxillofac Surg 2009;67:718-37. https://doi.org/10.1016/j.joms.2008.06.032 10.1016/j.joms.2008.06.032 [DOI] [PubMed] [Google Scholar]
- 20.Owosho AA, Xu B, Kadempour A, et al. Metastatic solid tumors to the jaw and oral soft tissue: a retrospective clinical analysis of 44 patients from a single institution. J Craniomaxillofac Surg 2016;44:1047-53. https://doi.org/10.1016/j.jcms.2016.05.013 10.1016/j.jcms.2016.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hirsberg A, Buchner A. Metastatic tumours to the oral region. An overview. Eur J Cancer B Oral Oncol 1995;31:355-60. https://doi.org/10.1016/0964-1955(95)00031-3 10.1016/0964-1955(95)00031-3 [DOI] [PubMed] [Google Scholar]
- 22.Pisani P, Angeli G, Krengli M, et al. Renal carcinoma metastasis to the parotid gland. J Laryngol Otol 1990;104:352-4. https://doi.org/10.1017/s0022215100112691 10.1017/s0022215100112691 [DOI] [PubMed] [Google Scholar]
- 23.Pisani P, Krengli M, Ramponi A, et al. Metastases to parotid gland from cancers of the upper airway and digestive tract. BrJ Oral Maxillofac Surg 1998;36:54-7. https://doi.org/10.1016/s0266-4356(98)90750-1 10.1016/s0266-4356(98)90750-1 [DOI] [PubMed] [Google Scholar]
- 24.Mrena R, Leivo I, Passador-Santos F, et al. Histopathological findings in parotid gland metastases from renal cell carcinoma. Eur Arch Otorhinolaryngol 2008;265:1005-9. https://doi.org/10.1007/s00405-008-0679-8 10.1007/s00405-008-0679-8 [DOI] [PubMed] [Google Scholar]
- 25.Franzen A, Buchali A, Lieder A. The rising incidence of parotid metastases: our experience from four decades of parotid gland surgery. Acta Otorhinolaryngol Ital 2017;37:264-9. https://doi.org/10.14639/0392-100X-1095 10.14639/0392-100X-1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higuera F, Boccalatte LA, Labanca MJ, et al. Renal clear cell carcinoma metastasis to submandibular gland: case report and review of the literature. J Surg Case Rep 2018;10:1-4. https://doi.org/10.1093/jscr/rjy261 10.1093/jscr/rjy261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dieing A, Schulz CO, Schmid P, et al. Orbital metastases in breast cancer: report of two cases and review of the literature. J Cancer Res Clin Oncol 2004;130:745-8. https://doi.org/10.1007/s00432-004-0606-3 10.1007/s00432-004-0606-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wood K, Vini L, Harmer C. Metastases to the thyroid gland: the Royal Marsden experience. Eur J Surg Oncol 2004;30:583-8. https://doi.org/10.1016/j.ejso.2004.03.012 10.1016/j.ejso.2004.03.012 [DOI] [PubMed] [Google Scholar]
- 29.Nixon IJ, Coca-Pelaz A, Kaleva AI, et al. Metastasis to the thyroid gland: a critical review. Ann Surg Oncol 2017;24:1533-9. https://doi.org/10.1245/s10434-016-5683-4 10.1245/s10434-016-5683-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bauer JL, Toluie S, Thompson LDR. Metastases to the parathyroid glands: a comprehensive literature review of 127 reported cases. Head Neck Pathol 2018;12:534-41. https://doi.org/10.1007/s12105-017-0850-x 10.1007/s12105-017-0850-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prescher A, Brors D. Metastases to the paranasal sinuses: case report and review of the literature. Laryngorhinootologie 2001;80:583-94. https://doi.org/10.1055/s-2001-17835 10.1055/s-2001-17835 [DOI] [PubMed] [Google Scholar]
- 32.Lòpez F, Devaney KO, Hanna EY, et al. Metastases to nasal cavity and paranasal sinuses. Head Neck 2016;38:1847-54. https://doi.org/10.1002/hed.24502 10.1002/hed.24502 [DOI] [PubMed] [Google Scholar]
- 33.Nicolai P, Puxeddu R, Cappiello J, et al. Metastatic neoplasms to the larynx: report of three cases. Laryngoscope 1996;106:851-5. https://doi.org/10.1097/00005537-199607000-00013 10.1097/00005537-199607000-00013 [DOI] [PubMed] [Google Scholar]
- 34.Ferlito A, Caruso G, Recher G. Secondary laryngeal tumors. Report of seven cases with review of the literature. Arch Otolaryngol Head Neck Surg 1988;114:635-9. https://doi.org/10.1001/archotol.1988.01860180049028 10.1001/archotol.1988.01860180049028 [DOI] [PubMed] [Google Scholar]
- 35.Gloria-Cruz TI, Schachern PA, Paparella MM, et al. Metastases to temporal bones from primary nonsystemic malignant neoplasms. Arch Otolaryngol Head Neck Surg 2000;126:209-14. https://doi.org/10.1001/archotol.126.2.209 10.1001/archotol.126.2.209 [DOI] [PubMed] [Google Scholar]
- 36.Song K, Park KW, Heo JH, et al. Clinical characteristics of temporal bone metastases. Clin Exp Otorhinolaryngol 2019;12:27-32. https://doi.org/10.21053/ceo.2018.00171 10.21053/ceo.2018.00171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanchez Aniceto G, Garcia Penin A, de la Mata Pages R, et al. Tumors metastatic to the mandible: analysis of nine cases and review of the literature. J Oral Maxillofac Surg 1990;48:246-51. [DOI] [PubMed] [Google Scholar]
- 38.Wanamaker JR, Kraus DH, Eliachar I, et al. Manifestations of metastatic breast carcinoma to the head and neck. Head Neck 1993;15:257-62. [DOI] [PubMed] [Google Scholar]
- 39.Kaminski B, Kobiorska-Nowak J, Bien S. Distant metastases to nasal cavities and paranasal sinuses, from the organs outside the head and neck. Otolaryngol Pol 2008;62:422-5. https://doi.org/10.1016/S0030-6657(08)70284-1 10.1016/S0030-6657(08)70284-1 [DOI] [PubMed] [Google Scholar]
- 40.Kobiorska-Nowak J, Bien S. The metastases to the head and neck region from distant primary localization. Otolaryngol Pol 2009;63:353-7 https://doi.org/10.1016/S0030-6657(09)70140-4 10.1016/S0030-6657(09)70140-4 [DOI] [PubMed] [Google Scholar]
- 41.Thiele OC, Freier K, Bacon C. Craniofacial metastases: a 20-year survey. J Cranio-Maxillo-Facial Surg 2011;39:135-7 [DOI] [PubMed] [Google Scholar]
- 42.Kumar Parida P. Renal cell carcinoma metastatic to the sinonasal region: three case reports with a review of the literature. Ear Nose Throat J 2012;91:E11. [DOI] [PubMed] [Google Scholar]
- 43.Wang H, Chen P. Palatine tonsillar metastasis of rectal adenocarcinoma: a case report and literature review. World J Surg Oncol 2013;11:114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang L, Yang H, Zhang X. Metastatic renal cell carcinoma to the jaws: report of cases. World J Surg Oncol 2014;12:204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raap M, Antonopoulos W, Dammrich M, et al. High frequency of lobular breast cancer in distant metastases to orbit. Cancer Medicine 2015;4:104-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pittoni P, Di Lascio S, Conti-Beltraminelli M, et al. Paranasal sinus metastasis of breast cancer. BMJ Case Rep 2014. https://doi.org/10.1136/bcr-2014-205171 10.1136/bcr-2014-205171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olsen JB, Sim F, Chandu A. Non-small cell lung cancer metastasis to the oral cavity: a case report. Aust Dent J 2014;59:520-4. https://doi.org/10.1111/adj.12215 10.1111/adj.12215 [DOI] [PubMed] [Google Scholar]
- 48.Zenga J, Mehrad M, Bradley JP. Metastatic cancer to the larynx: a case report and update. J Voice 2016;30:774.e9-774.e12. https://doi.org/10.1016/j.voice.2015.11.017 10.1016/j.voice.2015.11.017 [DOI] [PubMed] [Google Scholar]
- 49.Lenouvel D, Bhagwat P, Warnakulasurija S. Metastases from the lung presenting as a parotid lump. Br J Oral Maxillofac Surg 2016;54:e10-e12. [DOI] [PubMed] [Google Scholar]
- 50.Rusha AEA, Kamal EHM. Metastatic clear cell renal cell carcinoma presenting with a gingival metastasis. Clinics and Practice 2016;6:847-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Russel JO, Yan K, Burkey B, et al. Nonthyroid metastasis to the thyroid gland: case series and review with observations by primary pathology. Otolaryngol Head Neck Surg 2016;155:961-8. [DOI] [PubMed] [Google Scholar]
- 52.Arthur A, Horo S, Balasubramanian DA, et al. Orbital metastasis of cervical carcinoma - case report and review of literature. J Clin Diagn Res 2016;10:ND01-ND02. https://doi.org/10.7860/JCDR/2016/14400.7085 10.7860/JCDR/2016/14400.7085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Franzen AM, Gunzel T, Lieder A. Parotid gland metastases of distant primary tumours: a diagnostic challenge. Auris Nasus Larynx 2016;43:187-91. https://doi.org/10.1016/j.anl.2015.09.010 10.1016/j.anl.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 54.Tracy JC, Mildenhall NR, Wein RO, et al. Breast cancer metastases to the head and neck: Case series and literature review. Ear Nose Throat J 2017;96:E21-E24. [DOI] [PubMed] [Google Scholar]
- 55.Munakomi S, Chaudhary S, Chaudhary P, et al. Case report: orbital metastasis as the presenting feature of lung cancer. F1000Res 2017;6:430 https://doi.org/10.12688/f1000research.11247.1 10.12688/f1000research.11247.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cao XS, Cong BB, Yu ZY. Parotid gland metastasis from carcinoma of the breast detected by PET/TC. Medicine 2018;97:21(e10616) https://doi.org/10.1097/MD.0000000000010616 10.1097/MD.0000000000010616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sklar BA, Gervasio KA, Karmazin K, et al. Orbital metastasis from urothelial carcinoma: a comprehensive literature review. Ophtalmic Plast Reconstr Surg 2018;21 https://doi.org/10.1097/IOP.0000000000001256 10.1097/IOP.0000000000001256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Forner D, Cho P, Bullock M, et al. Report of metastatic ileal neuroendocrine tumor to the submandibular gland. Int J Surg Case Reports 2018;53:1-4. https://doi.org/10.1016/j.ijscr.2018.10.028 10.1016/j.ijscr.2018.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sahin B, Doruk C, Celik M, et al. Atypical metastasis to the head and neck region: an analysis of 11 patients. Turk Arch Otorhinolaryngol 2018;56:210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manafi-Farid R, Ayati N, Eftekhari M, et al. A rare presentation of colorectal cancer with unusual progressive intramuscular and subcutaneous metastatic spread. Asia Ocean J Nucl Med Biol 2019;7:89-94. https://doi.org/10.22038/AOJNMB.2018.11934 10.22038/AOJNMB.2018.11934 [DOI] [PMC free article] [PubMed] [Google Scholar]
9. Role of radiotherapy in the treatment of metastases from head and neck cancer
- 1.Ordoňez R, Otero A, Jerez I, et al. Role of radiotherapy in the treatment of metastatic head and neck cancer. Onco Targets Ther 2019;12:677-83. https://doi.org/10.2147/OTT.S181697 10.2147/OTT.S181697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aparicio DZ, Requejo OH, de Julián MAC, et al. Local control rates in stereotactic body radiotherapy (SBRT) of lung metastases associated with the biologically effective dose. Rep Pract Oncol Radiother 2019;24:142-50. https://doi.org/10.1016/j.rpor.2019.01.001 10.1016/j.rpor.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barillot I, Antoni D, Bellec J, et al. Bases référentielles de la radiothérapie en conditions steréotaxiques pour les tumeurs ou métastases bonchopulmonaires, hépatiques, prostatiques, des voies aérodigestives supérieures, cérébrales et osseuses. Cancer Radiother 2018;22:660-81. https://doi.org/10.1016/j.canrad.2018.08.001 10.1016/j.canrad.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 4.Bahig H, Aubin F, Stagg J, et al. Phase I/II trial of Durvalumab plus Tremelimumab and stereotactic body radiotherapy for metastatic head and neck carcinoma. BMC Cancer 2019;19:68 https://doi.org/10.1186/s12885-019-5266-4 10.1186/s12885-019-5266-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bates JE, De Leo AN, Morris CG, et al. Oligometastatic squamous cell carcinoma of the head and neck treated with stereotactic body ablative radiotherapy: Single-institution outcome. Head Neck 2019;41:2309-14. https://doi.org/10.1002/hed.25695 10.1002/hed.25695 [DOI] [PubMed] [Google Scholar]
- 6.Bonomo P, Greto D, Desideri I, et al. Clinical outcome of stereotactic body radiotherapy for lung-only oligometastatic head and neck squamous cell carcinoma: is the deferral of systemic therapy a potential goal? Oral Oncology 2019;93:1-7. https://doi.org/10.1016/j.oraloncology.2019.04.006 10.1016/j.oraloncology.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 7.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 8.Hauswald H, Simon C, Hecht S, et al. Long-term outcome and patterns of failure in patients with advanced head and neck cancer. Radiat Oncol 2011;6:70 https://doi.org/10.1186/1748-717X-6-70 10.1186/1748-717X-6-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park SH, Yoon SY, Park KS, et al. Brain metastasis from nasopharyngeal carcinoma treated with stereotactic radiosurgery. World Neurosurg 2019;126:160-3. https://doi.org/10.1016/j.wneu.2019.03.029 10.1016/j.wneu.2019.03.029 [DOI] [PubMed] [Google Scholar]
- 10.Patel RA, Bell JB, Kim T, et al. Stereotactic radiosurgery for brain metastases from primary head and neck carcinomas: a retrospective analysis. J. Neurooncol 2017;134:197-203. https://doi.org/10.1007/s11060-017-2509-6 10.1007/s11060-017-2509-6 [DOI] [PubMed] [Google Scholar]
- 11.Rambeau A, Bastit V, Thureau S, et al. Impact of locoregional irradiation in patients with upfront metastatic head and neck squamous cell carcinoma. Oral Oncol 2019;93:46-51. https://doi.org/10.1016/j.oraloncology.2019.04.005 10.1016/j.oraloncology.2019.04.005 [DOI] [PubMed] [Google Scholar]
- 12.Widder J, Klinkenberg TJ, Ubbels JF, et al. Pulmonary oligometastases: metastasectomy or stereotactic ablative radiotherapy? Radiother Oncol 2013;107:409-13. https://doi.org/10.1016/j.radonc.2013.05.024 10.1016/j.radonc.2013.05.024 [DOI] [PubMed] [Google Scholar]
- 13.Haigentz M, Jr, Hartl DM, Silver CE, et al. Distant metastases from head and neck squamous cell carcinoma. Part III. Treatment. Oral Oncol 2012;48:787-93. https://doi.org/10.1016/j.oraloncology.2012.03.019 10.1016/j.oraloncology.2012.03.019 [DOI] [PubMed] [Google Scholar]
- 14.Norihisa Y, Nagata Y, Takayama K, et al. Stereotactic body radiotherapy for oligometastatic lung tumors. Int J Radiat Oncol Biol Phys 2008;72:398-403. https://doi.org/10.1016/j.ijrobp.2008.01.002 10.1016/j.ijrobp.2008.01.002 [DOI] [PubMed] [Google Scholar]
- 15.Timmerman RD, Bizekis CS, Pass HI, et al. Local surgical, ablative, and radiation treatment of metastases. CA Cancer J Clin 2009;59:145-70. https://doi.org/10.3322/caac.20013 10.3322/caac.20013 [DOI] [PubMed] [Google Scholar]
- 16.Salama JK, Hasselle MD, Chmura SJ, et al. Stereotactic body radiotherapy for multisite extracranial oligometastases: final report of a dose escalation trial in patients with 1 to 5 sites of metastatic disease. Cancer 2012;118:2962-70. https://doi.org/10.1002/cncr.26611 10.1002/cncr.26611 [DOI] [PubMed] [Google Scholar]
- 17.Florescu C, Thariat J. Local ablative treatments of oligometastases from head and neck carcinoma. Crit Rev Oncol Ematol 2014;91:47-63. https://doi.org/10.1016/j.critrevonc.2014.01.004 10.1016/j.critrevonc.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 18.Matsushita H, Jingu K, Umezawa R, et al. Stereotactic radiotherapy for oligometastases in lymph nodes - a review. Tecnol Cancer Res Treat 2018;17:1533033818803597 https://doi.org/10.1177/1533033818803597 10.1177/1533033818803597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang HH, Zaorsky NG, Meng MB, et al. Stereotactic radiation therapy for oligometastases or oligorecurrence within mediastinal lymph nodes. Oncotarget 2016;7:18135-45. https://doi.org/10.18632/oncotarget.7636 10.18632/oncotarget.7636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcy PY, Magné N, Bailet C, et al. Liver metastases from head and neck squamous cell carcinomas: radiological and biological features. Onkologie 2004;27:157-60. https://doi.org/10.1159/000076905 10.1159/000076905 [DOI] [PubMed] [Google Scholar]
- 21.Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 2011;79:965-76. https://doi.org/10.1016/j.ijrobp.2010.11.026 10.1016/j.ijrobp.2010.11.026 [DOI] [PubMed] [Google Scholar]
- 22.McQuay HJ, Collins SL, Carroll D, et al. WITHDRAWN: radiotherapy for the palliation of painful bone metastases. Cochrane Database Syst Rev 2013;(11):CD001793 https://doi.org/10.1002/14651858.CD001793 10.1002/14651858.CD001793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spencer K, van der Velden JM, Wong E, et al. Systematic review of the role of stereotactic radiotherapy for bone metastases. J Natl Cancer Inst 2019;111:1023-32. https://doi.org/10.1093/jnci/djz101 10.1093/jnci/djz101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerszten PC, Burton SA, Ozhasoglu C, et al. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine (Phila Pa 1976) 2007;32:193-9. https://doi.org/10.1097/01.brs.0000251863.76595.a2 10.1097/01.brs.0000251863.76595.a2 [DOI] [PubMed] [Google Scholar]
- 25.Myrehaug S, Sahgal A, Hayashi M, et al. Reirradiation spine stereotactic body radiation therapy for spinal metastases: systematic review. J Neurosurg Spine 2017;27:428-35. https://doi.org/10.3171/2017.2.SPINE16976 10.3171/2017.2.SPINE16976 [DOI] [PubMed] [Google Scholar]
- 26.Sun XS, Michel C, Babin E, et al. Approach to oligometastatic disease in head and neck cancer, on behalf of the GORTEC. Future Oncol 2018;14:877-89. https://doi.org/10.2217/fon-2017-0468 10.2217/fon-2017-0468 [DOI] [PubMed] [Google Scholar]
- 27.Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. https://doi.org/10.1200/JCO.1995.13.1.8 10.1200/JCO.1995.13.1.8 [DOI] [PubMed] [Google Scholar]
- 28.Maclean J, Fersht N, Singhera M, et al. Multi-disciplinary management for patients with oligometastases to the brain: results of a 5 year cohort study. Radiat Oncol 2013;8:156 https://doi.org/10.1186/1748-717X-8-156 10.1186/1748-717X-8-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bahig H, Aubin F, Stagg J, et al. Phase I/II trial of Durvalumab plus Tremelimumab and stereotactic body radiotherapy for metastatic head and neck carcinoma. BMC Cancer 2019;19:68 https://doi.org/10.1186/s12885-019-5266-4 10.1186/s12885-019-5266-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
10. Chemotherapy for recurrent/metastatic head and neck cancer
- 1.Argiris A, Li Y, Forastiere A. Prognostic factors and long-term survivorship in patients with recurrent or metastatic carcinoma of the head and neck. Cancer 2004;101:2222-9. https://doi.org/10.1002/cncr.20640 10.1002/cncr.20640 [DOI] [PubMed] [Google Scholar]
- 2.Gibson MK, Li Y, Murphy B, et al. Randomized phase III evaluation of cisplatin plus fluorouracil versus cisplatin plus paclitaxel in advanced head and neck cancer (E1395): an intergroup trial of the Eastern Cooperative Oncology Group. J Clin Oncol 2005;23:3562-7. https://doi.org/10.1200/JCO.2005.01.057 10.1200/JCO.2005.01.057 [DOI] [PubMed] [Google Scholar]
- 3.Vermorken JB, Mesia R, Rivera F, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 2008;359:1116-27. https://doi.org/10.1056/NEJMoa0802656 10.1056/NEJMoa0802656 [DOI] [PubMed] [Google Scholar]
- 4.Guigay J, Fayette J, Dillies AF, et al. Cetuximab, docetaxel, and cisplatin as first-line treatment in patients with recurrent or metastatic head and neck squamous cell carcinoma: a multicenter, phase II GORTEC study. Ann Oncol 2015;26:1941-7. https://doi.org/10.1093/annonc/mdv268 10.1093/annonc/mdv268 [DOI] [PubMed] [Google Scholar]
- 5.Guigay J, Fayette J, Mesia R, et al. TPExtreme randomized trial: TPEx versus Extreme regimen in 1st line recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC). J Clin Oncol 2019;37(Suppl 15):6002 https://doi.org/10.1200/JCO.2019.37.15_suppl.6002 10.1200/JCO.2019.37.15_suppl.6002 [DOI] [Google Scholar]
- 6.Bossi P, Miceli R, Locati LD, et al. A randomized, phase 2 study of cetuximab plus cisplatin with or without paclitaxel for the first-line treatment of patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. Ann Oncol 2017;28:2820-6. https://doi.org/10.1093/annonc/mdx439 10.1093/annonc/mdx439 [DOI] [PubMed] [Google Scholar]
- 7.Rischin D, Harrington KJ, Greil R, et al. Protocol-specified final analysis of the phase 3 KEYNOTE-048 trial of pembrolizumab (pembro) as first-line therapy for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC). J Clin Oncol 2019;37(Suppl 15):6000 https://doi.org/10.1200/JCO.2019.37.15_suppl.6000 10.1200/JCO.2019.37.15_suppl.6000 [DOI] [Google Scholar]
- 8.Szturz P, Seiwert TY, Vermorken JB. How standard is the second-line cetuximab in recurrent or metastatic head and neck cancer in 2017?. J Clin Oncol 2017;35:2229-31. https://doi.org/10.1200/JCO.2016.71.8072 10.1200/JCO.2016.71.8072 [DOI] [PubMed] [Google Scholar]
- 9.Siano M, Infante G, Resteghini C, et al. Outcome of recurrent and metastatic head and neck squamous cell cancer patients after first line platinum and cetuximab therapy. Oral Oncol 2017;69:33-7. https://doi.org/10.1016/j.oraloncology.2017.04.002 10.1016/j.oraloncology.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 10.Adkins D, Lin JC, Sacco AG, et al. Palbociclib plus cetuximab versus placebo plus cetuximab in platinum-resistant, cetuximab-naïve, HPV-unrelated head and neck cancer: a double blind randomized phase II trial (PALATINUS). J Clin Oncol 2019;37(Suppl 15):6013 https://doi.org/10.1200/JCO.2019.37.15_suppl.6013 10.1200/JCO.2019.37.15_suppl.6013 [DOI] [Google Scholar]
- 11.Cognetti DM, Johnson JM, Curry JM, et al. Results of a phase 2a, multicenter, open-label, study of RM-1929 photoimmunotherapy (PIT) in patients with locoregional, recurrent head and neck squamous cell carcinoma (rHNSCC). J Clin Oncol 2019;37(Suppl 15):6014 https://doi.org/10.1200/JCO.2019.37.15_suppl.6014 10.1200/JCO.2019.37.15_suppl.6014 [DOI] [Google Scholar]
- 12.Prawira A, Oosting SF, Chen TW, et al. Systemic therapies for recurrent or metastatic nasopharyngeal carcinoma: a systematic review. Br J Cancer 2017;117:1743-52. https://doi.org/10.1038/bjc.2017.357 10.1038/bjc.2017.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L, Huang Y, Hong S, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet 2016;388:1882-92. https://doi.org/10.1016/S0140-6736(16)31388-5 10.1016/S0140-6736(16)31388-5 [DOI] [PubMed] [Google Scholar]
- 14.Rizk S, Robert A, Vandenhooft A, et al. Activity of chemotherapy in the palliative treatment of salivary gland tumors: review of the literature. Eur Arch Otorhinolaryngol 2007;264:587-94. https://doi.org/10.1007/s00405-007-0297-x 10.1007/s00405-007-0297-x [DOI] [PubMed] [Google Scholar]
- 15.Airoldi M, Garzaro M, Pedani F, et al. Cisplatin + Vinorelbine treatment of recurrent or metastatic salivary gland malignancies (RMSGM): a final report on 60 cases. Am J Clin Oncol 2017;40:86-90. https://doi.org/10.1097/COC.0000000000000112 10.1097/COC.0000000000000112 [DOI] [PubMed] [Google Scholar]
- 16.Pandey A, Kumar M, Shahi H, et al. Novel therapeutic options for recurrent metastatic salivary gland tumors: review of the ongoing clinical trials. Cancer Res Stat Treat 2018;110-8. https://doi.org/10.4103/CRST.CRST_1_18 10.4103/CRST.CRST_1_18 [DOI] [Google Scholar]
11. Present and future of immunotherapy in head and neck cancer
- 1.King GN, Healy CM, Glover MT, et al. Increased prevalence of displastic and malignant lip lesions in renal-transplanted recipients. N Engl J Med 1995;332:1052-7. https://doi.org/10.1056/NEJM199504203321602 10.1056/NEJM199504203321602 [DOI] [PubMed] [Google Scholar]
- 2.Bhatia S, Louie AD, Bhatia R, et al. Solid cancers after bone marrow transplantation. J Clin Oncol 2001;19:464-71. https://doi.org/10.1200/JCO.2001.19.2.464 10.1200/JCO.2001.19.2.464 [DOI] [PubMed] [Google Scholar]
- 3.Demarosi F, Lodi G, Carassi A, et al. Oral malignancies following HSCT: graft versus host disease and other risk factors. Oral Oncol 2005;41:865-77. https://doi.org/10.1016/j.oraloncology.2005.02.001 10.1016/j.oraloncology.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 4.Maciels JP, Haddad RI, Fayette J, et al. Afatinib versus methotrexate as second-line treatment in patients with recurrent or metastatic squamous-cell carcinoma of the head and neck progressing on or after platinum-based therapy (LUX-Head & Neck 1): an open-label, randomized phase 3 trial. Lancet Oncol 2015;16:583-94. https://doi.org/10.1016/S1470-2045(15)70124-5 10.1016/S1470-2045(15)70124-5 [DOI] [PubMed] [Google Scholar]
- 5.Ferris RL, Blumenschein GR, Fayette J, et al. Two-year update from Checkmate 141: outcomes with nivolumab (Nivo) vs investigator choice (IC) in recurrent or metastatic (R/M) squamous cell carcinoma of the head and neck (SCCHN) in the overall population and PD-L1 subgroups. Int J Radiat Biol Phys 2018;100:1317 https://doi.org/10.1016/j.ijrobp.2017.12.300 10.1016/j.ijrobp.2017.12.300 [DOI] [Google Scholar]
- 6.Saleh K, Daste A, Martin N, et al. Response to salvage chemotherapy after progression on immune checkpoint inhibitors in patients with squamous cell carcinoma of the head and neck. J Clin Oncol 2018;36 (Suppl 15):6015 https://doi.org/10.1200/JCO.2018.36.15_suppl.6015 10.1200/JCO.2018.36.15_suppl.6015 [DOI] [PubMed] [Google Scholar]
- 7.Burtness B, Harrington KJ, Greil R, et al. KeyNote 048: phase 3 study of first-line pembrolizumab (P) for recurrent/metastatic head and neck neck squamous cell carcinoma (R/M HNSCC). Ann Oncol 2018;29(Suppl 8):mdy424.045 https://doi.org/10.1093/annonc/mdy424.045 10.1093/annonc/mdy424.045 [DOI] [Google Scholar]
- 8.Rischin D, Harrington KJ, Greil R, et al. Protocol-specified final analysis of the phase 3 KEYNOTE-048 trial of pembrolizumab (pembro) as first-line therapy for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC). J Clin Oncol 2019;37(Suppl 15):6000 https://doi.org/10.1200/JCO.2019.37.15_suppl.6000 10.1200/JCO.2019.37.15_suppl.6000 [DOI] [Google Scholar]
- 9.Chen DS, Mellman I. Elements of cancer immunity and the cancer immune-set point. Nature 2017;541:321-30. https://doi.org/10.1038/nature21349 10.1038/nature21349 [DOI] [PubMed] [Google Scholar]
- 10.Economopoulou P, Agelaki S, Perisanidis C, et al. The promise of immunotherapy in head and neck carcinoma. Ann Oncol 2016;27:1675-85. https://doi.org/10.1093/annonc/mdw226 10.1093/annonc/mdw226 [DOI] [PubMed] [Google Scholar]
- 11.Cohen EE, Harrington KJ, Hong DS, et al. A phase Ib/II study (SCORES) of durvalumab (D) plus Danvatirsen (DAN;AZD9150) or AZD5069 (CX2i) in advanced solid malignancies and recurrent/metastatic head and neck cancer. Ann Oncol 2018;29(Suppl 8):viii372-viii399. https://doi.org/10.1093/annonc/mdy287 10.1093/annonc/mdy287 [DOI] [Google Scholar]
- 12.Ferris RL, Saba NF, Gitlitz BJ, et al. Effect of adding motolimod to standard combination chemotherapy and cetuximab treatment of patients with squamous cell carcinoma of the head and neck. The Active8 randomized clinical trial. Jama Oncol 2018;4:1583-8. https://doi.org/10.1001/jamaoncol.2018.1888 10.1001/jamaoncol.2018.1888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fayette J, Lefebvre G, Posner MR, et al. Results of a phase II study evaluating monalizumab in combination with cetuximab in previously treated recurrent or metastatic squamous cell carcinoma of the head and neck. Ann Oncol 2018;29(Suppl 8):viii372-viii399. https://doi.org/10.1093/annonc/mdy287 10.1093/annonc/mdy287 [DOI] [Google Scholar]
- 14.Knee DA, Hewes B, Brogdon JL. Rationale for anti-GITR cancer immunotherapy. Eur J Cancer 2016;67:1-10. https://doi.org/10.1016/j.ejca.2016.06.028 10.1016/j.ejca.2016.06.028 [DOI] [PubMed] [Google Scholar]
- 15.Siu LL, Burris H, Le DT, et al. Preliminary phase 1 profile of BMS-986179, an anti-CD73 antibody, in combination with nivolumab in patients with advanced solid tumors. Cancer Res 2018;78:CT180 https://doi.org/10.1158/1538-7445.AM2018-CT180 10.1158/1538-7445.AM2018-CT180 [DOI] [Google Scholar]
- 16.Grilley-Olson JE, Curti BD, Smith DC, et al. SEA-CD40, a non-fucosylated CD40 agonist: Interim results from a phase 1 study in advanced solid tumors. J Clin Oncol 2018;36(Suppl 15):3093 https://doi.org/10.1200/JCO.2018.36.15_suppl.3093 10.1200/JCO.2018.36.15_suppl.3093 [DOI] [Google Scholar]
- 17.Mitchell TC, Hamid O, Smith DC, et al. Epacadostat plus pembrolizumab in patients with advanced solid tumors: phase I results from a multicenter, open-label phase I/II trial (ECHO-202/KEYNOTE-037). J Clin Oncol 2018:JCO2018789602 https://doi.org/10.1200/JCO.2018.78.9602 [Epub ahead of print] 10.1200/JCO.2018.78.9602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merlano MC, Abbona A, Denaro N, et al. Knowing the tumor microenvironment to optimize immunotherapy. Acta Othorinolaryngol Ital 2019;39:2-8 https://doi.org/10.14639/0392-100X-2481 10.14639/0392-100X-2481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyauchi S, Kim SS, Pang J, et al. Immune modulation of head and neck squamous cell carcinoma and the tumor microenvironment by conventional therapeutics. Clin Cancer Res 2019:25:4211-23. https://doi.org/10.1158/1078-0432.CCR-180871 10.1158/1078-0432.CCR-180871 [DOI] [PMC free article] [PubMed] [Google Scholar]
12. Role of surgery in oligometastatic disease
- 1.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 2.Coca-Pelaz A, Rodrigo JP, Bradley PJ, et al. Adenoid cystic carcinoma of the head and neck - an update. Oral Oncol 2015;51:652-61. https://doi.org/10.1016/j.oraloncology.2015.04.005 10.1016/j.oraloncology.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 3.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 2010;363:24-35. https://doi.org/10.1056/NEJMoa0912217 10.1056/NEJMoa0912217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albergotti WG, Abberbock S, Mathews F, et al. Oligometastatic status as predictor of survival in metastatic human papillomavirus-positive oropharyngeal carcinoma. Head Neck 2018;40:1685-90. https://doi.org/10.1002/hed.25171 10.1002/hed.25171 [DOI] [PubMed] [Google Scholar]
- 5.Schulz D, Wirth M, Piontek G, et al. Improved overall survival in head and neck cancer patients after specific therapy of distant metatases. Eur Arch Otorhinolaryngol 2018;275:1239-47. https://doi.org/10.1007/s00405-018-4920-9 10.1007/s00405-018-4920-9 [DOI] [PubMed] [Google Scholar]
- 6.Florescu C, Thariat J. Local ablative treatments of oligometastases from head and neck carcinomas. Crit Rev Oncol Hematol 2014;91:47-63. https://doi.org/10.1016/j.critrevonc.2014.01.004 10.1016/j.critrevonc.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 7.Hunter J. Of diseases, supposed to be venereal, produced by transplante teeth. Lond Med J 1786;7:205-16. [PMC free article] [PubMed] [Google Scholar]
- 8.Edwards T. Cirugia del pulmon. Prensa Med Argent 1934;34:732-4. [PubMed] [Google Scholar]
- 9.Alexander J, Haight C. Pulmonary resection for solitary metastatic sarcomas and carcinomas. Surg Gynecol Obstet 1947; 85:129-46. [PubMed] [Google Scholar]
- 10.Deslauriers J, Meyerson SL, Patterson A, et al. Pearson’s thoracic & esophageal surgery. Third Edition Philadelphia: Churchill Livingstone; 2008. [Google Scholar]
- 11.Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. https://doi.org/10.1200/JCO.1995.13.1.8 10.1200/JCO.1995.13.1.8 [DOI] [PubMed] [Google Scholar]
- 12.Oki T, Hishida T, Yoshida J, et al. Survival and prognostic factors after pulmonary metastasectomy of head and neck cancer: what are the clinically informative prognostic factors? Eur J Cardiothorac Surg 2019;55:942-7. https://doi.org/10.1093/ejcts/ezy384 10.1093/ejcts/ezy384 [DOI] [PubMed] [Google Scholar]
- 13.Yamazaki K, Shodo R, Ueki Y, et al. Therapeutic outcome after resection of pulmonary metastasis from head and neck carcinomas. Ind J Otolaryn Head Neck Surg 2015;67:124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yotsukura M, Kinoshita T, Kohno M, et al. Survival predictors after resection of lung metastases of head or neck cancers. Thorac Cancer 2015;6:579-83. https://doi.org/10.1111/1759-7714.12225 10.1111/1759-7714.12225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hosokawa S, Funai K, Sugiyama K, et al. Survival outcomes after surgical resection of pulmonary metastases of head and neck tumours. J Laryngol Otol 2015;130:291-5. https://doi.org/10.1017/S0022215116000050 10.1017/S0022215116000050 [DOI] [PubMed] [Google Scholar]
- 16.Young ER, Diakos E, Khalid-Raja M, et al. Resection of subsequent pulmonary metastases from treated head and neck squamous cell carcinoma: systematic review and meta-analysis. Clin Otolaryngol 2015;40;208-18. https://doi.org/10.1111/coa.12348 10.1111/coa.12348 [DOI] [PubMed] [Google Scholar]
- 17.Adachi H, Yamamoto T, Saito S, et al. Therapeutic outcome after resection of pulmonary metastases from oral and/or head and neck cancers: complete republication of the article published in Jpn J Chest Surg. Gen Thorac Cardiovasc Surg 2015;63:459-64. https://doi.org/10.1007/s11748-015-0554-7 10.1007/s11748-015-0554-7 [DOI] [PubMed] [Google Scholar]
- 18.Leto CJ, Sharbel D, Wang CW, et al. Workup of suspected chest metastases on 18F-FDG-PET/CT in head and neck cancer: worth the wait? Ear Nose Throat J 2019;98:158-64. https://doi.org/10.1177/0145561319828315 10.1177/0145561319828315 [DOI] [PubMed] [Google Scholar]
- 19.Bates JE, De Leo AN, Morris CG, et al. Oligometastatic squamous cell carcinoma of the head and neck treated with stereotactic body ablative radiotherapy: single-institution outcomes. Head Neck 2019;41:2309-14. https://doi.org/10.1002/hed.25695 10.1002/hed.25695 [DOI] [PubMed] [Google Scholar]
- 20.Iguchi T, Hiraki T, Gobara H, et al. Radiofrequency ablation of lung metastases from adenoid cystic carcinoma of the head anf neck: retrospective evaluation in nine patients. J Vasc Interv Radiol 2015;26:703-8. https://doi.org/10.1016/j.jvir.2014 10.1016/j.jvir.2014 [DOI] [PubMed] [Google Scholar]
- 21.Ye X, Fan W, Wang H, et al. Expert consensus workshop report: Guidelines for thermal ablation of primary and metastatic lung tumors (2018 edition). J Cancer Res Ther 2018;14:730-44. https://doi.org/10.4103/jcrt.JCRT_221_18 10.4103/jcrt.JCRT_221_18 [DOI] [PubMed] [Google Scholar]
- 22.Moneke I, Kaifi JT, Kloeser R, et al. Pulmonary metastasectomy for thyroid cancer as salvage therapy for radioactive iodine-refractory metastases. Eur J Cardiothoracic Surg 2018;53:625-30. https://doi.org/10.1093/ejcts/ezx367 10.1093/ejcts/ezx367 [DOI] [PubMed] [Google Scholar]
- 23.Deniffel D, Sauter A, Dangelmaier J, et al. Differentiating intrapulmonary metastases from different primary tumors via quantitative dual-energy CT based iodine concentration and conventional CT attenuation. Eur J Radiol 2019;11:6-13. https://doi.org/10.1016/j.ejrad.2018.12.015 10.1016/j.ejrad.2018.12.015 [DOI] [PubMed] [Google Scholar]
- 24.Ichinose J, Shinozaki-Ushiku A, Nagayama K, et al. Immunohistochemical pattern analysis of squamous cell carcinoma: Lung primary and metastatic tumors of head and neck. Lung Cancer 2016;100:96-101. https://doi.org/10.1016/j.lungcan.2016.08.003 10.1016/j.lungcan.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 25.Muñoz-Largacha JA, Gower AC, Sridhar P, et al. miRNA profiling of primary lung and head and neck squamous cell carcinomas: addressing a diagnostic dilemma. J Thorac Cardiovasc Surg 2017;54:714-27. https://doi.org/10.1016/j.jtcvs.2017.02.071 10.1016/j.jtcvs.2017.02.071 [DOI] [PubMed] [Google Scholar]
- 26.Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol 2011;8:378-82. https://doi.org/10.1038/nrclinonc.2011.44 10.1038/nrclinonc.2011.44 [DOI] [PubMed] [Google Scholar]
- 27.Pawlik TM, Gleisner AL, Bauer TW, et al. Liver-directed surgery for metastatic squamous cell carcinoma to the liver: results of a multi-center analysis. Ann Surg Oncol 2007;14:2807-16. https://doi.org/10.1245/s10434-007-9467-8 10.1245/s10434-007-9467-8 [DOI] [PubMed] [Google Scholar]
- 28.Katz AW, Carey-Sampson M, Muhs AG, et al. Hypofractioned sterotactic body radiation therapy (SBRT) for limited hepatic metastases. Int J Radiat Oncol Biol Phys 2007;67:793-8. https://doi.org/10.1016/j.ijrobp.2006.10.025 10.1016/j.ijrobp.2006.10.025 [DOI] [PubMed] [Google Scholar]
- 29.Djalilian HR, Tekin M, Hall WA, et al. Metastatic head and neck squamous cell carcinoma to the brain. Auris Nasus Larynx 2002;29:47-54. https://doi.org/10.1016/s0385-8146(01)00113-4 10.1016/s0385-8146(01)00113-4 [DOI] [PubMed] [Google Scholar]
- 30.Patel RA, Bell JB, Kim T, et al. Stereotactic radiosurgery for brain metasteses from primary head and neck cacinomas: a retrospective analysis. J Neurooncol 2017;134:197-203. https://doi.org/10.1007/s11060-017-2509-6 10.1007/s11060-017-2509-6 [DOI] [PubMed] [Google Scholar]
13. Emerging strategies for treatment of metastatic disease
- 1.Banerjee D, Cieslar-Pobuda A, Zhu GH, et al. Adding nanotechnology to the metastasis treatment arsenal. Trends Pharmacol Sci 2019;40:403-18. https://doi.org/10.1016/j.tips.2019.04.002 10.1016/j.tips.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 2.Papetti M, Herman IM. Mechanisms of normal and tumor-derived angiogenesis. Am J Physiol Cell Physiol 2002;282:C947-70. https://doi.org/10.1152/ajpcell.00389.2001 10.1152/ajpcell.00389.2001 [DOI] [PubMed] [Google Scholar]
- 3.Gschwind A, Fischer OM, Ullrich A. The discovery of receptor tyrosine kinases: targets for cancer therapy. Nat Rev Cancer 2004;4:361-70. https://doi.org/10.1038/nrc1360 10.1038/nrc1360 [DOI] [PubMed] [Google Scholar]
- 4.Specenier P, Vermorken JB. Cetuximab: its unique place in head and neck cancer treatment. Biologics 2013;7:77-90. https://doi.org/10.2147/BTT.S43628 10.2147/BTT.S43628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cappuzzo F, Ciuleanu T, Stelmakh L, et al. Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: a multicentre, randomised, placebo-controlled phase 3 study. Lancet Oncol 2010;11:521-9. https://doi.org/10.1016/S1470-2045(10)70112-1 10.1016/S1470-2045(10)70112-1 [DOI] [PubMed] [Google Scholar]
- 6.Gocek E, Moulas AN, Studzinski GP. Non-receptor protein tyrosine kinases signaling pathways in normal and cancer cells. Crit Rev Clin Lab Sci 2014;51:125-37. https://doi.org/10.3109/10408363.2013.874403 10.3109/10408363.2013.874403 [DOI] [PubMed] [Google Scholar]
- 7.Schroeder A, Heller DA, Winslow MM, et al. Treating metastatic cancer with nanotechnology. Nat Rev Cancer 2011;12:39-50. https://doi.org/10.1038/nrc3180 10.1038/nrc3180 [DOI] [PubMed] [Google Scholar]
- 8.Markman JL, Rekechenetskiy A, Holler E, et al. Nanomedicine therapeutic approaches to overcome cancer drug resistance. Adv Drug Deliv Rev 2013;65:1866-79. https://doi.org/10.1016/j.addr.2013.09.019 10.1016/j.addr.2013.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson RL, Balasas T, Callaghan J, et al. A framework for the development of effective anti-metastatic agents. Nat Rev Clin Oncol 2019;16:185-204. https://doi.org/10.1038/s41571-018-0134-8 10.1038/s41571-018-0134-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilsdon T, Barron A, Edwards G, et al. The benefits of personalised medicine to patients, society and healthcare systems. European Biopharmaceutical Enterprises (EBE) atEFoPIaAE; 2018. Report No.: CRA Project No. D24332. [Google Scholar]
- 11.Ginsburg GS, Phillips KA. Precision medicine: from science to value. Health Aff (Millwood) 2018;37:694-701. https://doi.org/10.1377/hlthaff.2017.1624 10.1377/hlthaff.2017.1624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imamura Y, Mukohara T, Shimono Y, et al. Comparison of 2D- and 3D-culture models as drug-testing platforms in breast cancer. Oncol Rep 2015;33:1837-43. https://doi.org/10.3892/or.2015.3767 10.3892/or.2015.3767 [DOI] [PubMed] [Google Scholar]
- 13.Lee E, Song HG, Chen CS. Biomimetic on-a-chip platforms for studying cancer metastasis. Curr Opin Chem Eng 2016;11:20-7. https://doi.org/10.1016/j.coche.2015.12.001 10.1016/j.coche.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu H, Lyu X, Yi M, et al. Organoid technology and applications in cancer research. J Hematol Oncol 2018;11:116 https://doi.org/10.1186/s13045-018-0662-9 10.1186/s13045-018-0662-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lancaster MA, Knoblich JA. Organogenesis in a dish: modeling development and disease using organoid technologies. Science 2014;345:1247125 https://doi.org/10.1126/science.1247125 10.1126/science.1247125 [DOI] [PubMed] [Google Scholar]
- 16.Movia D, Prina-Mello A. Nanotoxicity in cancer research: technical protocols and considerations for the use of 3D tumour spheroids. Gomes AC, Sarria MP. (eds.). Unraveling the safety profile of nanoscale particles and materials - from biomedical to environmental applications. London: InterTech Open; 2018. pp. 88-131. https://doi.org/10.5772/intechopen.69447 10.5772/intechopen.69447 [DOI] [Google Scholar]
- 17.Vlachogiannis G, Hedayat S, Vatsiou A, et al. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science 2018;359:920-6. https://doi.org/10.1126/science.aao2774 10.1126/science.aao2774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramamoorthy P, Thomas SM, Kaushik G, et al. Metastatic tumor-in-a-dish, a novel multi-cellular organoid to study lung colonization and predict therapeutic response. Cancer Res 2019;79:1681-95. https://doi.org/10.1158/0008-5472.CAN-18-2602 10.1158/0008-5472.CAN-18-2602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Z, Li E, Guo Z, et al. Design and construction of a multi-organ microfluidic chip mimicking the in vivo microenvironment of lung cancer metastasis. ACS Appl Mater Interfaces 2016;8:25840-7. https://doi.org/10.1021/acsami.6b08746 10.1021/acsami.6b08746 [DOI] [PubMed] [Google Scholar]
- 20.Chiesa E, Dorati R, Pisani S, et al. The microfluidic technique and the manufacturing of polysaccharide nanoparticles. Pharmaceutics 2018;10 Pii:E267 https://doi.org/10.3390/pharmaceutics10040267 10.3390/pharmaceutics10040267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sontheimer-Phelps A, Hassell BA, Ingber DE. Modelling cancer in microfluidic human organs-on-chips. Nat Rev Cancer 2019;19:65-81. https://doi.org/10.1038/s41568-018-0104-6 10.1038/s41568-018-0104-6 [DOI] [PubMed] [Google Scholar]
- 22.Jeon JS, Bersini S, Gilardi M, et al. Human 3D vascularized organotypic microfluidic assays to study breast cancer cell extravasation. Proc Natl Acad Sci USA 2015;112:214-9. https://doi.org/10.1073/pnas.1417115112 10.1073/pnas.1417115112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao Y, Shen M, Shi X. Design of functional electrospun nanofibers for cancer cell capture applications. J Mater Chem B 2018;6:1420-32. https://doi.org/10.1039/C7TB03347H 10.1039/C7TB03347H [DOI] [PubMed] [Google Scholar]
- 24.Jarvis M, Arnold M, Ott J, et al. Microfluidic co-culture devices to assess penetration of nanoparticles into cancer cell mass. Bioeng Transl Med 2017;2:268-77. https://doi.org/10.1002/btm2.10079 10.1002/btm2.10079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buzzelli JN, Ouaret D, Brown G, et al. Colorectal cancer liver metastases organoids retain characteristics of original tumor and acquire chemotherapy resistance. Stem Cell Res 2018;27:109-20. https://doi.org/10.1016/j.scr.2018.01.016 10.1016/j.scr.2018.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu K, Newbury PA, Glicksberg BS, et al. Evaluating cell lines and organoids as models for metastatic cancer through integrative analysis of open genomic data. BioRxiv 2018:337287 https://doi.org/10.1101/337287 10.1101/337287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tanaka N, Osman AA, Takahashi Y, et al. Head and neck cancer organoids established by modification of the CTOS method can be used to predict in vivo drug sensitivity. Oral Oncol 2018;87:49-57. https://doi.org/10.1016/j.oraloncology.2018.10.018 10.1016/j.oraloncology.2018.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah AT, Heaster TM, Skala MC. Metabolic imaging of head and neck cancer organoids. PLoS One 2017;12:e0170415 https://doi.org/10.1371/journal.pone.0170415 10.1371/journal.pone.0170415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kong J, Luo Y, Jin D, et al. A novel microfluidic model can mimic organ-specific metastasis of circulating tumor cells. Oncotarget 2016;7:78421-32. https://doi.org/10.18632/oncotarget.9382 10.18632/oncotarget.9382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zervantonakis IK, Hughes-Alford SK, Charest JL, et al. Three-dimensional microfluidic model for tumor cell intravasation and endothelial barrier function. P Natl Acad Sci USA 2012;109:13515-20. https://doi.org/10.1073/pnas.1210182109 10.1073/pnas.1210182109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bersini S, Jeon JS, Dubini G, et al. A microfluidic 3D in vitro model for specificity of breast cancer metastasis to bone. Biomaterials 2014;35:2454-61. https://doi.org/10.1016/j.biomaterials.2013.11.050 10.1016/j.biomaterials.2013.11.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Q, Liu T, Qin J. A microfluidic-based device for study of transendothelial invasion of tumor aggregates in realtime. Lab Chip 2012;12:2837-42. https://doi.org/10.1039/c2lc00030j 10.1039/c2lc00030j [DOI] [PubMed] [Google Scholar]
- 33.EU Commission. Commission Recommendation of 18 October 2011 on the definition of nanomateria. Official Journal of the European Union 20October2011. [Google Scholar]
- 34.Greish K. Enhanced permeability and retention (EPR) effect for anticancer nanomedicine drug targeting. Methods Mol Biol 2010;624:25-37. https://doi.org/10.1007/978-1-60761-609-2_3 10.1007/978-1-60761-609-2_3 [DOI] [PubMed] [Google Scholar]
- 35.He Q, Guo S, Qian Z, et al. Development of individualized anti-metastasis strategies by engineering nanomedicines. Chem Soc Rev 2015;44:6258-86. https://doi.org/10.1039/c4cs00511b 10.1039/c4cs00511b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang DY, Hou YL, Yang SM, et al. Advances in nanomedicine for head and neck cancer. Front Biosci (Landmark Ed) 2014;19:783-8. https://doi.org/10.2741/4245 10.2741/4245 [DOI] [PubMed] [Google Scholar]
- 37.Bartczak D, Muskens OL, Nitti S, et al. Interactions of human endothelial cells with gold nanoparticles of different morphologies. Small 2012;8:122-30. https://doi.org/10.1002/smll.201101422 10.1002/smll.201101422 [DOI] [PubMed] [Google Scholar]
- 38.Suk JS, Xu Q, Kim N, et al. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev 2016; 99:28-51. https://doi.org/10.1016/j.addr.2015.09.012 10.1016/j.addr.2015.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xie H, Goins B, Bao A, et al. Effect of intratumoral administration on biodistribution of 64Cu-labeled nanoshells. Int J Nanomedicine 2012;7:2227-38. https://doi.org/10.2147/IJN.S30699 10.2147/IJN.S30699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen Q, Liang C, Wang X, et al. An albumin-based theranostic nano-agent for dual-modal imaging guided photothermal therapy to inhibit lymphatic metastasis of cancer post surgery. Biomaterials 2014;35:9355-62. https://doi.org/10.1016/j.biomaterials.2014.07.062 10.1016/j.biomaterials.2014.07.062 [DOI] [PubMed] [Google Scholar]
- 41.Liu Y, Gunda V, Zhu X, et al. Theranostic near-infrared fluorescent nanoplatform for imaging and systemic siRNA delivery to metastatic anaplastic thyroid cancer. Proc Natl Acad Sci USA 2016;113:7750-5. https://doi.org/10.1073/pnas.1605841113 10.1073/pnas.1605841113 [DOI] [PMC free article] [PubMed] [Google Scholar]
14. Head and neck metastatic disease and frailty: clinical and ethical approaches
- 1.Lee JH, Song JH, Lee SN, et al. Adjuvant postoperative radiotherapy with or without chemotherapy for locally advanced squamous cell carcinoma of the head and neck: the importance of patient selection for the postoperative chemoradiotherapy. Cancer Res Treat 2013;45:31-9. https://doi.org/10.4143/crt.2013.45.1.31 10.4143/crt.2013.45.1.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leòn X, Quer M, Orus C, et al. Distant metastases in head and neck cancer patients who achieved locoregional control. Head Neck 2000;22:680-6. https://doi.org/10.1002/1097-0347(200010)22:7<680::aid-hed7>3.0.co;2-j [DOI] [PubMed] [Google Scholar]
- 3.Wiegand S, Zimmermann A, Wilhelm T, et al. Survival after distant metastasis in head and neck cancer. Anticancer Res 2015;35:5499-502. [PubMed] [Google Scholar]
- 4.Kotwall C, Sako K, Razack MS, et al. Metastatic patterns in squamous cell cancer of the head and neck. Am J Surg 1987;154:439-42. https://doi.org/10.1016/0002-9610(89)90020-2 10.1016/0002-9610(89)90020-2 [DOI] [PubMed] [Google Scholar]
- 5.Vermorken JB, Mesia R, Rivera F, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 2008;359:1116–27. https://doi.org/10.1056/NEJMoa0802656 10.1056/NEJMoa0802656 [DOI] [PubMed] [Google Scholar]
- 6.Merino OR, Lindberg RD, Fletcher GH. An analysis of distant metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 1977;40:145-51. https://doi.org/10.1002/1097-0142(197707)40:1<145::aid-cncr2820400124>3.0.co;2-9 [DOI] [PubMed] [Google Scholar]
- 7.McGale P, Taylor C, Correa C, et al. EBCTCG (Early Breast Cancer Trialists’ Collaborative Group) Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 2014;383:2127-35. https://doi.org/10.1016/S0140-6736(14)60488-8 10.1016/S0140-6736(14)60488-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duprez F, Berwouts D, De Neve W, et al. Distant metastases in head and neck cancer. Head Neck 2017;39:1733-43. https://doi.org/10.1002/hed.24687 10.1002/hed.24687 [DOI] [PubMed] [Google Scholar]
- 9.Winter H, Meimarakis G, Hoffmann G, et al. Does surgical resection of pulmonary metastases of head and neck cancer improve survival? Ann Surg Oncol 2008;15:2915-26. https://doi.org/10.1245/s10434-008-0001-4 10.1245/s10434-008-0001-4 [DOI] [PubMed] [Google Scholar]
- 10.Haigentz M, Hartl DM, Silver CE, et al. Distant metastases from head and neck squamous cell carcinoma. Part III. Oral Oncol 2012;48:787-93. https://doi.org/10.1016/j.oraloncology.2012.03.019 10.1016/j.oraloncology.2012.03.019 [DOI] [PubMed] [Google Scholar]
- 11.Handforth C, Clegg A, Young C, et al. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol 2015;26:1091-101. https://doi.org/10.1093/annonc/mdu540 10.1093/annonc/mdu540 [DOI] [PubMed] [Google Scholar]
- 12.Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet 2016;387:2145-54. https://doi.org/10.1016/S0140-6736(15)00516-4 10.1016/S0140-6736(15)00516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004;59:255-63. https://doi.org/10.1093/gerona/59.3.m255 10.1093/gerona/59.3.m255 [DOI] [PubMed] [Google Scholar]
- 14.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:146-56. https://doi.org/10.1093/gerona/56.3.m146 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Mitnitski A, Song X, et al. Long-term risks of death and institutionalization of elderly people in relation to deficit accumulation at age 70. J Am Geriatr Soc 2006;54:975-9. https://doi.org/10.1111/j.1532-5415.2006.00738.x 10.1111/j.1532-5415.2006.00738.x [DOI] [PubMed] [Google Scholar]
- 16.Gobbens RJ, van Assen MA, Luijkx KG, et al. Determinants of frailty. J Am Med Dir Assoc 2010;11:356-64. https://doi.org/10.1016/j.jamda.2009.11.008 10.1016/j.jamda.2009.11.008 [DOI] [PubMed] [Google Scholar]
- 17.Bortz WM. A conceptual framework of frailty: a review. J Gerontol A Biol Sci Med Sci 2002;57:M283-8. https://doi.org/10.1093/gerona/57.5.m283 10.1093/gerona/57.5.m283 [DOI] [PubMed] [Google Scholar]
- 18.Rolland Y, Czerwinski S, Abellan Van Kan G, et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging 2008;12:433-50. https://doi.org/10.1007/bf02982704 10.1007/bf02982704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walston J, Fried LP. Frailty and the older man. Med Clin North Am 1999;83:1173-94. https://doi.org/10.1016/s0025-7125(05)70157-7 10.1016/s0025-7125(05)70157-7 [DOI] [PubMed] [Google Scholar]
- 20.Lin HS, Watts JN, Peel NM, et al. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 2016;16:157 https://doi.org/10.1186/s12877-016-0329-8 10.1186/s12877-016-0329-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Genther DJ, Gourin CG. Effect of comorbidity on short-term outcomes and cost of care after head and neck cancer surgery in the elderly. Head Neck 2015;37:685-93. https://doi.org/10.1002/hed.23651 10.1002/hed.23651 [DOI] [PubMed] [Google Scholar]
- 22.Nieman CL, Pitman KT, Tufaro AP, et al. The effect of frailty on short-term outcomes after head and neck cancer surgery. Laryngoscope 2018;128:102-10. https://doi.org/10.1002/lary.26735 10.1002/lary.26735 [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Pederson JL, Churchill TA, et al. Impact of frailty on outcomes after discharge in older surgical patients: a prospective cohort study. CMAJ 2018;190:E184-E190. https://doi.org/10.1503/cmaj.161403 10.1503/cmaj.161403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrucci L, Guralnik JM, Cavazzini C, et al. The frailty syndrome: a critical issue in geriatric oncology. Crit Rev Oncol Hematol 2003;46:127-37. https://doi.org/10.1016/s1040-8428(02)00177-4 10.1016/s1040-8428(02)00177-4 [DOI] [PubMed] [Google Scholar]
- 25.NCCN Clinical Practice Guidelines in Oncology. Older Adult Oncology v1.2019 - January 8, 2019. [Google Scholar]
- 26.AIOM Linee guida 2017. - Tumori dell’anziano. [Google Scholar]
- 27.SIAARTI. Strategie perioperatorie: presa in carico dell’anziano con gravi comorbilità e fase avanzata di malattia con patologia chirurgica acuta. www.siaarti.it. Accessed Jan 18, 2020. [DOI] [PubMed]
- 28.Noor A, Gibb C, Boase S, et al. Frailty in geriatric head and neck cancer: a contemporary review. Laryngoscope 2018;128:E416-E424. https://doi.org/10.1002/lary.27339 10.1002/lary.27339 [DOI] [PubMed] [Google Scholar]
- 29.Grandazzi G, Roussel LM, Cuny F, et al. Impact of head and neck cancer on partner’s sociability. Eur Ann Otorhinolaryngol Head Neck Dis 2019;136:165-8. https://doi.org/10.1016/j.anorl.2019.02.017 10.1016/j.anorl.2019.02.017 [DOI] [PubMed] [Google Scholar]
- 30.Moschopoulou E, Hutchinson I, Bhui K, et al. Post-traumatic stress in head and neck cancer survivors and their partners. Support Care Cancer 2018;26:3003-11. https://doi.org/10.1007/s00520-018-4146-9 10.1007/s00520-018-4146-9 [DOI] [PubMed] [Google Scholar]
- 31.Moore KA, Ford PJ, Farah CS. “I have quality of life… but…”: exploring support needs important to quality of life in head and neck cancer. Eur J Oncol Nurs 2014;18:192-200. https://doi.org/10.1016/j.ejon.2013.10.010 10.1016/j.ejon.2013.10.010 [DOI] [PubMed] [Google Scholar]
- 32.Boulahssass R, Gonfrier S, Sanchez M, et al. Predicting early death in older adults with cancer. Eur J Cancer 2018;100:65-74. https://doi.org/10.1016/j.ejca.2018.04.013 10.1016/j.ejca.2018.04.013 [DOI] [PubMed] [Google Scholar]
- 33.Peppercorn JM, Smith TJ, Helft PR, et al. American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol 2011;29:755-60. https://doi.org/10.1200/JCO.2010.33.1744 10.1200/JCO.2010.33.1744 [DOI] [PubMed] [Google Scholar]
15. Observations on the socio-economic impact of metastatic disease in head and neck oncology
- 1.AIOM, AIRTUM, Fondazione AIOM, PASSI Istituto superiore di Sanità. I numeri del cancro in Italia - 2018. Brescia: Intermedia; 2018. [Google Scholar]
- 2.FAVO. Secondo rapporto sulla condizione assistenziale dei malati oncologici. Roma 2010. www.favo.it
- 3.Yabroff KR, Francisci S, Mariotto A, et al. Advancing comparative studies of patterns of care and economic outcomes in cancer: challenges and opportunities. J Natl Cancer Inst Monogr 2013;46:1-6. https://doi.org/10.1093/jncimonographs/lgt005 10.1093/jncimonographs/lgt005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipscom J, Ybrahoff KR, Hornbrook MC, et al. Comparing cancer care, outcomes, and costs across health systems: charting the course. J Natl Cancer Inst Monogr 2013;46:124-30. https://doi.org/10.1093/jncimonographs/lgt011 10.1093/jncimonographs/lgt011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Divi V, Tao L, Whittemore A, et al. Geographic variation in Medicare treatment cost and outcomes for advanced head and neck cancer. Oral Oncol 2016;61:83-8. https://doi.org/10.1016/j.oraloncology.2016.08.018 10.1016/j.oraloncology.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 6.Francisci S, Guzzinati S, Mezzetti M, et al. Cost profiles of colorectal cancer patients in Italy based on individual patterns of care. BMC Cancer 2013;13:329 https://doi.org/10.1186/1471-2407-13-329 10.1186/1471-2407-13-329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FAVO. Undicesimo rapporto sulla condizione assistenziale dei malati oncologici. Roma 2019. www.favo.it
- 8.Polesel J, Lupato V, Collarile P, et al. Direct health-care cost of head and neck cancers: a population-based study in north-eastern Italy. Med Oncol 2019;36:31 https://doi.org/10.1007/s12032-019-1256-2 10.1007/s12032-019-1256-2 [DOI] [PubMed] [Google Scholar]
- 9.Progetto EPICOST. L’impatto economico dei tumori sui sistemi sanitari regionali: stime e proiezioni in relazione a diversi scenari di intervento. Coord ISS 2015-2017. [Google Scholar]
- 10.Maruthappu M, Watkins J, Noor AM, et al. Economic downturns, universal health coverage, and cancer mortality in high-income and middle-income countries, 1990-2010: a longitudinal analysis. Lancet 2016;388:684-95. https://doi.org/10.1016/S0140-6736(16)00577-8 10.1016/S0140-6736(16)00577-8 [DOI] [PubMed] [Google Scholar]


