Abstract
Background:
Primary shoulder stabilization is successful, but there continues to be a risk of recurrence after operative repair, particularly in the young athlete. It is important for surgeons to understand the outcomes after various revision stabilization techniques to best counsel patients and manage expectations.
Purpose:
To analyze recurrent instability and revision surgery rates in patients who underwent revision anterior glenohumeral stabilization procedures with either arthroscopic repair, open repair, coracoid transfer, free bone block, or capsular reconstruction.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
We performed a systematic review of level 2 to 4 evidence studies using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Clinical studies of revision anterior glenohumeral stabilization (arthroscopic repair, open repair, coracoid transfer, free bone block, or capsular reconstruction) with a minimum 2-year follow-up were analyzed. The rate of recurrent instability, rate of revision surgery, patient-reported outcomes, and range of motion were extracted and reported. Study methodological quality was evaluated using the Downs and Black quality assessment score.
Results:
A total of 37 studies met inclusion criteria and were available for analysis: 20 studies evaluated arthroscopic repair, 8 evaluated open repair, 5 evaluated Latarjet procedure, 3 evaluated bone block, and 2 evaluated capsular reconstruction. There was 1 study included in both arthroscopic and Latarjet procedures, for a total of 1110 revision cases. There was 1 level 2 study, and the remainder were level 3 or 4 with poor Downs and Black scores. Participants analyzed were most commonly young (weighted mean age, 26.1 years) and male (78.4%). The weighted mean clinical follow-up after revision surgery was 47.8 months. The weighted mean rate of recurrent instability was 3.8% (n = 245) after the Latarjet procedure, 13.4% (n = 260) after open repair, 16.0% (n = 531) after arthroscopic repair, 20.8% (n = 72) after bone block, and 31.0% (n = 35) after capsular reconstruction. The weighted mean rate of additional revision surgery was 0.0% after bone block, 0.02% after the Latarjet procedure, 9.0% after arthroscopic repair, 9.3% after open repair, and 22.8% after capsular reconstruction. Patient-reported outcomes and objective measures of range of motion and strength improved with all revision techniques.
Conclusion:
The current review identifies a deficiency in the literature pertaining to consistent meaningful outcomes and the effect of bone loss after revision shoulder stabilization. Published studies demonstrate, however, that revision shoulder stabilization using arthroscopic, open, coracoid transfer, or bone block techniques yielded satisfactory objective and patient-reported outcomes. The Latarjet procedure exhibited the lowest recurrent instability rate. This study confirms that recurrent instability remains a common problem, despite revision shoulder stabilization. The quality of research in revision shoulder stabilization remains poor, and higher quality studies are needed to establish best practices for treatment of this complex problem.
Keywords: shoulder instability, revision, outcomes, recurrent instability
Shoulder instability is a common diagnosis, occurring at an approximate rate of 1.7% in the general population and as high as 14.8% in young athletic cohorts.22,24 Military personnel are also at a particularly high risk, with rates as high as 3% per year and an estimated incidence of 1.69 per 1000 person-years.38,49
Despite success with primary stabilization techniques, there continues to be a risk of recurrence after operative repair, particularly in the young athlete.52 Recurrent instability after an index surgical intervention varies depending on the technique, but reports range from 0% to 60%.9 Not surprisingly, as the incidence of surgical procedures for anterior shoulder instability continues to increase, so too has the need for revision stabilization.8
Which revision technique offers the lowest recurrence rates and most consistent improvements in objective and patient-reported outcomes remains unclear. This uncertainty is in part because of inconsistency in the literature in reporting failures. Some authors consider revision surgery or redislocation as failures, while others designate continued microinstability, inability to return to prior sporting levels, or poor patient-reported outcomes as failures as well. The multitude of surgical techniques reported in the literature additionally confounds the picture, as they are often described in small isolated case series from single institutions. Furthermore, glenoid and/or humeral bone loss play central roles in treatment decisions but are inconsistently reported and quantified in the literature.
Despite incomplete and heterogeneous data, it is valuable to compile available primary evidence such that surgeons may better understand the clinical outcomes of the various surgical options for revision surgical stabilization when counseling their patients and choosing the optimal treatment. The purpose of this systematic review was to review outcomes after revision anterior shoulder stabilization. The goals of this study were to analyze (1) functional and subjective outcomes and (2) failure rates in patients who have undergone revision glenohumeral stabilization with arthroscopic repair, open repair, coracoid transfer, bone block, or capsular reconstruction.
Methods
Study Design
A systematic review was performed on outcomes after revision shoulder stabilization. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed to evaluate and assess study methodology.34 This review was prospectively registered with Prospero (CRD42018109043) before data extraction.
Search Strategy
A systematic computerized search of the literature in the PubMed, Embase, and Scopus databases was conducted by a medical research librarian (L.L.) with controlled vocabulary and keywords related to shoulder joint instability and revision surgery. This coauthor did not participate in aspects of screening, full-text review, or data abstraction. The search time frame was restricted from inception of the database to November 6, 2018. The search included not only peer-reviewed articles. The reference lists of all selected articles were checked to retrieve relevant publications that were not identified in the primary database search.
Eligibility Criteria
Original articles were included if they met all of the following criteria: (1) revision shoulder stabilization outcomes were reported, regardless of whether concomitant procedures were performed and regardless of the study level of evidence; (2) the full text was available in English; and (3) the study was published in a peer-reviewed journal. Excluded were case reports, systematic reviews, imaging reviews, animal studies, anatomic or histological studies, surgical technical reports, studies with fewer than 5 participants, and studies using thermal shrinkage as an exclusive method of shoulder stabilization. Studies that presented outcomes of only primary shoulder stabilization were excluded. Studies were included if they presented outcomes from both primary and revision cases. Series including adhesive capsulitis, shoulder arthroplasty, and rotator cuff surgery were excluded.
Study Selection
Two authors (B.C.L. and L.B.P.) independently assessed eligible studies identified by the search strategy. Titles and abstracts were screened by applying eligibility criteria, and full texts of potentially relevant studies were subsequently obtained. If the title and abstract did not provide adequate information to determine whether eligibility criteria were met, the study was included for a full-text review. Then, 2 authors (B.C.L. and M.W.) independently assessed full-text relevancy according to inclusion and exclusion criteria. If no consensus was reached, the senior author (J.C.R.) was available to make the final decision regarding eligibility. The authors performed additional citation tracking by screening the reference lists within eligible studies.
Data Abstraction
Reviewers (T.R.J., B.P.G., L.B.P., M.W., A.N.F., and J.H.H.) collected data in duplicate and recorded them in a customized database using an Excel spreadsheet (Version 2007; Microsoft). If a disagreement in data extraction was present, it was resolved by the senior author (J.C.R.). Data regarding study design, sample size, age, sex, follow-up, timing of surgery, indications, surgical methods, concomitant procedures, outcomes, and complications were recorded. Whenever outcomes were reported for more than 1 time point during follow-up, values from the last recorded follow-up were used.
Quality Assessment
The level of evidence (levels 2-4) of the included studies was assessed by the reviewers independently using the American Academy of Orthopaedic Surgeons classification system for orthopaedic literature.23 The Downs and Black score (maximum possible score, 31) was also used to assess the methodological quality of the included studies.16 The reviewers thoroughly reviewed the guidelines for grading studies, and discrepancies in scoring were discussed among them. A minimum follow-up of 2 years was deemed an appropriate interval to accurately assess outcomes.
Statistical Analysis
Given the nonuniform nature of the studies included in this systematic review with respect to techniques and outcome reporting, the results are presented as a narrative summary. The weighted mean was used because of the varying number of participants between studies. This was calculated by summing the total number of participants undergoing each procedure type. The number of participants in each individual study was then divided by the total number of participants. This created a weight, which was than multiplied by the rate of instability and repeat revision surgery in the study. The results for the studies for each procedure type were then summed to create a weighted mean.
Results
Search Strategy Findings
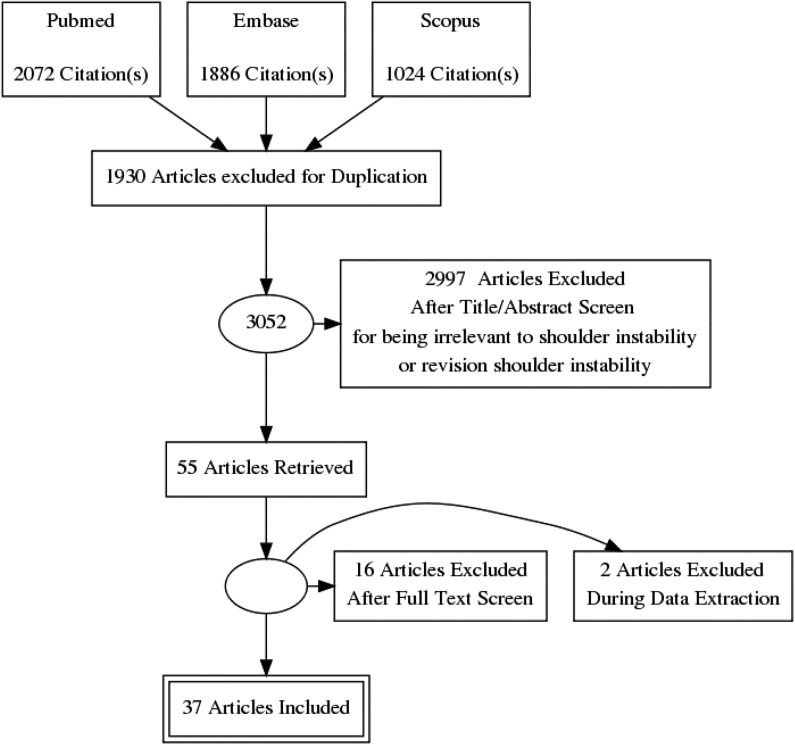
A total of 4982 studies were identified in an initial round of database and reference searches. After duplicates were removed, 3052 titles and abstracts were screened. After a review of titles and abstracts, 55 studies were deemed eligible for inclusion. After a full-text review, 18 studies were excluded. There were 37 remaining studies included in the final quality assessment and analysis (Figure 1).
Figure 1.
Preferred Reporting items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram demonstrating systematic review of literature for revision shoulder stabilization.
The study quality of the 37 nonrandomized studies was assessed using the Downs and Black criteria.16 Of these, 1 study was scored as level 2, three were scored as level 3, and 33 were scored as level 4. The median Downs and Black score for the studies was 6.42 of 31. All studies met appropriate follow-up criteria (minimum 2 years). There were no randomized controlled studies (Table 1). Table 2 presents the weighted mean for the rate of recurrent instability and the rate of repeat revision surgery for each procedure type.
Table 1.
Outcomes of Revision Anterior Shoulder Stabilizationa
| First Author (Year) | Level of Evidence | No. of Patients | No. of Revision Procedures | Mean Age, y | Mean Follow-up, mo | Rate of Recurrent Instability,b % | Rate of Repeat Revision Surgery, % |
|---|---|---|---|---|---|---|---|
| Arthroscopic repair | |||||||
| Arce3 (2012) | 4 | 16 | 16 | 26.8 | 30.9 | 19.0 | 1.0 |
| Barnes4 (2009) | 4 | 15 | 16 | 30 | 38 | 6.0 | 6.0 |
| Bartl5 (2011) | 4 | 56 | 56 | 29.4 | 37 | 13.0 | 7.0 |
| Boileau7 (2009) | 4 | 22 | 22 | 25 | 43 | 14.0 | 0.0 |
| Castagna10 (2010) | 4 | 18 | 18 | 33.4 | 69 | 16.7 | 0.0 |
| Cuellar13 (2017) | 4 | 12 | 12 | 32.2 | 36 | 0.0 | 0.0 |
| Creighton12 (2007) | 4 | 18 | 18 | 28.6 | 29.7 | 17.0 | 6.0 |
| De Giorgi14 (2014) | 4 | 22 | 22 | 27 | 56 | 36.4 | NR |
| Franceschi18 (2008) | 4 | 10 | 10 | 25.6 | 68 | 10.0 | 0.0 |
| Frank19 (2015) | 4 | 90 | 63 | 23.2 | 46.9 | 19.0 | NR |
| Kim25 (2002) | 2 | 23 | 23 | 24 | 36 | 21.7 | NR |
| Neri35 (2007) | 4 | 11 | 11 | 28 | 34.5 | 27.2 | NR |
| Patel39 (2008) | 4 | 40 | 40 | 33.1 | 36 | 10.0 | 5.0 |
| Ryu42 (2011) | 4 | 12 | 12 | 27.5 | 22 | 26.7 | 13.3 |
| Shin45 (2015) | 4 | 62 | 63 | 23.2 | 46.4 | 10.4 | 12.7 |
| Su48 (2018) | 4 | 65 | 65 | 26.1 | 56.4 | 41.5 | 27.7 |
| Krueger26 (2011) | 3 | 75 | 20 | 29 | 25 | 10.0 | 0.0 |
| Millar33 (2008) | 3 | 25 | 10 | 31 | 37 | 20.0 | 10.0 |
| McCabe31 (2014) | 4 | 31 | 11 | 24.6 | 41 | 36.4 | 0.0 |
| Stein47 (2014) | 3 | 46 | 23 | 32 | 28 | 20.0 | 0.0 |
| Open repair | |||||||
| Cho11 (2009) | 4 | 25 (1 bilateral) | 26 | 24 | 42 | 11.5 | 11.5 |
| Levine27 (2000) | 4 | 50 | 50 | 27 | 56.4 | 22.0 | 10.0 |
| Marquardt30 (2007) | 4 | 24 | 16 | 24.3 | 68 | 50.0 | 38.0 |
| Meehan32 (2005) | 4 | 28 | 28 | 31.7 | 60 | 14.3 | 14.2 |
| Neviaser36 (2015) | 4 | 30 | 30 | 31 | 122.4 | 0.0 | 0.0 |
| Rowe41 (1984) | 4 | 24 | 24 | 25 | 48 | 8.3 | 4.2 |
| Sisto46 (2007) | 4 | 30 | 30 | 24 | 46 | 0.0 | 0.0 |
| Zabinski51 (1999) | 4 | 23 | 23 | 77.3 | 17.4 | 13.0 | |
| Latarjet procedure | |||||||
| Flinkkila17 (2015) | 4 | 52 | 52 | 28.4 | 38 | 16.7 | 3.3 |
| Frank19 (2015) | 4 | 90 | 28 | 27.5 | 46.9 | 7.1 | 1.4 |
| Nicholson37 (2014) | 4 | 51 | 51 | 32.6 | 48 | 0.0 | 0.0 |
| Ranalletta40 (2018) | 4 | 65 | 65 | 26.8 | 44 | 0.0 | 0.0 |
| Schmid43 (2012) | 4 | 49 | 49 | 29 | 38 | 14.3 | 2.9 |
| Free bone block | |||||||
| Giannakos21 (2017) | 4 | 12 | 12 | 37.5 | 28.8 | 58.3 | 0.0 |
| Lunn28 (2008) | 4 | 34 | 34 | 30 | 81.6 | 17.6 | 0.0 |
| Willemot50 (2019) | 4 | 26 | 26 | 29.4 | 43.7 | 11.5 | 0.0 |
| Capsular reconstruction | |||||||
| Alcid2 (2007) | 4 | 15 | 15 | 30.9 | 36 | 33.0 | 13.3 |
| Dewing15 (2012) | 4 | 15 (5 bilateral) | 20 | 26 | 38.4 | 30.0 | 30.0 |
aFrank et al19 included both arthroscopic repair and Latarjet procedures. NR, not reported.
bRate of recurrent instability included apprehension, subluxations, and frank dislocations.
Table 2.
Weighted Mean Rates of Recurrent Instability and Repeat Revision Surgery
| Revision Procedure | Recurrent Instability,a % | Repeat Revision Surgery, % |
|---|---|---|
| Arthroscopic repair | 16.0 | 9.0 |
| Open repair | 13.4 | 9.3 |
| Latarjet procedure | 3.8 | 0.02 |
| Free bone block | 20.8 | 0.0 |
| Capsular reconstruction | 31.0 | 22.8 |
aRate of recurrent instability included apprehension, subluxations, and frank dislocations.
Outcomes of Revision Arthroscopic Anterior Capsulolabral Repair
There were 20 studies from 2002 to 2018 that reported the outcomes of revision arthroscopic labral repair in a total of 531 revision cases. There was 1 level 2 study, 3 level 3 studies, and the remainder were level 4. The mean follow-up was 39.5 months. The range of reported recurrent instability after revision was 0% to 41.5%. The weighted mean recurrent instability rate was 16.0%, and the weighted mean repeat revision rate was 9.0% (Table 2). The rate of recurrent instability included apprehension, subluxations, and frank dislocations.
Outcomes Comparing Revision With Primary Arthroscopic Repair
There were 4 included studies that compared revision arthroscopic stabilization with primary arthroscopic stabilization, with variable reported outcomes.26,31,33,47 Krueger et al26 compared 20 revision with 20 primary arthroscopic shoulder stabilization cases and reported no significant difference in the number of recurrent postoperative dislocations, although the apprehension sign was positive in 2 of the patients in the revision group. Of note, however, the number of preoperative dislocations for the primary arthroscopic stabilization group was 8.7 versus 9.8 for the revision arthroscopic stabilization group. The study also excluded any patient with a bony glenoid defect >25%. Importantly, revision cases exhibited significantly lower scores on the Walch-Duplay score, Melbourne Instability Shoulder Scale, Western Ontario Shoulder Instability Index (WOSI), and subjective shoulder value (SSV) but no difference in the Rowe score.26 The study also showed significantly poorer forward flexion and abduction in the revision group compared with the primary group.
Millar and Murrell33 similarly compared 10 revision with 15 primary shoulder stabilization cases and found no significant difference in outcome scores (University of California Los Angeles [UCLA]) or rates of recurrent instability. However, a finding of no statistically significant differences in Rowe scores was contingent on the exclusion of 4 early failures in the revision group. When these were included, the primary group’s postoperative Rowe scores were significantly higher versus the revision group. In this case series, only 1 patient in the primary group exhibited a bony Bankart lesion (<10% inferior glenoid), while none of the patients in the revision group demonstrated inferior glenoid bone loss, but 5 had evidence of Hill-Sachs lesions, which were not quantified. Interestingly, in this study, all revision procedures were performed after prior initial open procedures (5 Putti-Platt, 3 Bankart, and 2 open capsular shift).
McCabe et al31 evaluated 11 revision and 20 primary arthroscopic stabilization cases in patients with moderate glenoid bone loss (<25%) and Hill-Sachs lesions measuring 10% to 50% of the humeral articular surface. Arthroscopic labral repair with remplissage was performed in all patients. They identified clinical improvement in American Shoulder and Elbow Surgeons (ASES) and Rowe scores in all patients, with no significant differences between groups. However, 13% of revision cases demonstrated recurrent instability versus 0% of primary stabilization cases. The findings suggested that arthroscopic repair in the setting of even moderate bone loss led to higher recurrent instability rates than primary stabilization, despite improved clinical outcome scores.31
Stein et al47 retrospectively evaluated 25 revision arthroscopic Bankart repair cases and compared 23 of these with matched primary Bankart repair cases (based on sex, age, and follow-up time). The study reported a 20% failure rate for the revision cases (4% redislocation and 16% positive apprehension), with 1 patient requiring subsequent glenoid augmentation and another requiring arthroscopic osteosynthesis for a traumatic glenoid fracture. Failure and revision rates for primary cases were not explicitly reported. The study, however, demonstrated that revision arthroscopic repair could restore anterior and inferior labral congruency similar to primary arthroscopic repair based on magnetic resonance imaging follow-up at an average of 28 and 32 months, respectively. This study also found that patients undergoing revision arthroscopic repair had statistically poorer Rowe, Walch-Duplay, Constant, and pain scores than patients undergoing primary arthroscopic stabilization. Furthermore, postoperative external rotation deficits at 0° and 90° of abduction were identified in revision cases compared with primary arthroscopic repair cases.47
Outcomes of Revision Arthroscopic Bankart Repair After Primary Latarjet Procedure
In 2 retrospective case series of 30 total patients, the outcomes of revision arthroscopic surgery after a primary open Latarjet procedure were reported, with a mean follow-up of 52.5 months.10,13 The weighted mean recurrent instability rate for this cohort was 10.0%. No subsequent revision procedures were performed in either of the studies.
Before the primary Latarjet procedure, each patient had sustained an average of 6.9 shoulder dislocations, and capsular laxity was noted in 73.3% (22/30) of all patients at the time of revision arthroscopic surgery.10,13 Both studies demonstrated improvements in patient-reported outcome scores after revision surgery, with a mean Constant score of 83.9, mean Rowe score of 78.0, and mean visual analog scale (VAS) score of 2.1 (30 total patients). A mean postoperative ASES score of 99.6 was reported by Castagna et al,10 while Cuellar et al13 also noted a significant improvement in external rotation after revision arthroscopic surgery from 16.8° preoperatively to 33.5° postoperatively (P < .0001).
Outcomes of Revision Open Bankart Repair
Between 1984 and 2015, there were 8 studies that described the outcomes of revision open Bankart repair in a total of 237 revision cases. All studies were level 4. The mean follow-up was 65.0 months. The range of reported recurrent instability was 0.0% to 50.0%. The weighted mean recurrent instability rate was 13.4%, and the weighted mean revision rate was 9.3%.
There were 3 studies that focused solely on revision open Bankart repair, while the remainder included heterogeneous results.11,36,46 In the homogeneous studies reporting on revision open Bankart repair alone, the average loss of external rotation after revision was 10°11 and 8°.46 While Neviaser et al36 did not report preoperative versus postoperative range of motion, they noted only a 3° “loss” of external rotation in the operative versus contralateral shoulder. Additionally, they found no statistically significant motion loss in any measured plane, and no patient considered any motion loss functionally significant.36 There was an improvement in Rowe scores in all patients postoperatively. The results were excellent or good in 87% to 93% of patients.11,36,46
Outcomes of Revision Open Latarjet Procedure After Failed Primary Arthroscopic or Open Repair
Overall, 5 studies, from 2012 to 2018, reported the results of revision Latarjet procedures in a total of 245 revision cases. All studies were level 4. The mean follow-up was 42.98 months. The range of reported recurrent instability was 0.0% to 16.7%. The weighted mean recurrent instability rate was 3.8%, and the weighted mean revision rate was 0.02%.
All studies involved patients who had recurrent instability after a prior soft tissue stabilization procedure, and all reported clinical improvement in patient-reported outcome scores after revision (SSV, VAS, Constant, Rowe, WOSI, Oxford, ASES, SST, Athletic Shoulder Outcome Scoring System).
There were 2 studies (114 patients) that included only patients with >20% anterior glenoid bone loss.40,43 The weighted mean recurrent instability rate for this population was 6.14%, with subluxations but no frank dislocations, and the weighted mean revision rate was 1.25%. Ranalletta et al40 also performed computed tomography at 3 to 5 months postoperatively (average, 3.3 months), which demonstrated 92% bone block healing.
The average complication rate for revision Latarjet procedures was 12.3% and included delayed wound healing, infections, frozen shoulder, coracoid malunion and nonunion, and graft fragmentation.40,43 There were a total of 3 reoperations: irrigation and debridement of septic arthritis, an intra-articular screw requiring removal, and recurrent instability treated with open capsular shift.40,43
Outcomes Comparing Revision Arthroscopic Repair With Revision Latarjet Procedure
Frank et al19 reported clinical outcomes after revision arthroscopic stabilization compared with a revision Latarjet procedure. A total of 90 patients (91 shoulders) who had failed prior soft tissue stabilization were included. Those with >25% glenoid bone loss (n = 28) underwent a revision Latarjet procedure, while those with <25% bone loss underwent revision arthroscopic repair (n = 63). The mean follow-up for the revision arthroscopic repair group was 46.9 months, with a significant improvement in mean ASES (63.7 to 85.1), VAS (2.89 to 0.81), and Simple Shoulder Test (SST) scores (6.2 to 9.1) (P < .001). Similarly, the revision Latarjet procedure group had a significant improvement in mean ASES (65.7 to 87.0), VAS (3.1 to 1.1), and SST scores (7.2 to 10.3) (P < .001). The revision arthroscopic repair group exhibited a recurrent instability rate of 19.0% (12/63), while the revision Latarjet procedure group had a lower recurrence rate of 7.1% (2/28). However, the study did not explicitly report a statistical comparison, as these represented clinically different cohorts based on their degree of glenoid bone loss.
Outcomes After Glenoid Free Bone Block
A total of 3 studies that were published between 2008 and 2019, with a total of 72 participants, reported on the outcomes of revision procedures with free bone block of the anterior glenoid (iliac crest or distal tibia). All studies were level 4, and the mean follow-up was 51.37 months.21,28,50 The range of reported recurrent postoperative instability was 11.5% to 58.3%. The weighted mean recurrent instability rate was 20.8%, and the weighted mean revision rate was 0.0%. Many of the participants in these studies represented difficult salvage scenarios with recurrent instability or multiple prior revision procedures, making an interpretation of results and direct comparison with other cohorts difficult.
In a small case series, Giannakos et al21 reported outcomes after a revision all-arthroscopic Eden-Hybinette procedure for 12 patients. A total of 10 of these patients had previously undergone the Latarjet procedure, and 2 had previously undergone arthroscopic labral repair. All patients demonstrated improvement in mean patient-reported outcome scores after revision (Rowe, Walch-Duplay, WOSI), and 8 patients reported excellent to good outcomes. Overall, 5 had persistent positive apprehension postoperatively, and 2 patients had recurrent subluxations. The average postoperative anterior flexion was 176°, with 66° of external rotation. The rate of complication was 50%, with 2 patients with progressive glenohumeral osteoarthritic changes and 4 patients with nonunion identified on postoperative computed tomography.21
Lunn et al28 reported the results of 34 patients who underwent a revision Eden-Hybinette procedure after a previous Latarjet procedure. There was an improvement in Walch-Duplay scores, with 79% reporting good to excellent outcomes. A recurrent instability rate of 17.6% was described, with 4 patients with a single postoperative dislocation and 2 with recurrent dislocations. The average postoperative forward flexion was 170°, and the average external rotation was 70°. A total of 16 patients developed progressive glenohumeral arthritis graded as moderate or severe at an average follow-up of 6.8 years. There was 1 patient who developed a superficial wound infection, which resolved without surgery or sequelae, while 5 patients (14.7%) had complaints related to the iliac crest donor site (discomfort and hypesthesia).28
Willemot et al50 evaluated patients who underwent revision stabilization after initial Bristow (5 patients) and Latarjet (21 patients) procedures with either a structural iliac crest bone graft (20 cases; 76.9%), reimplantation of the original coracoid graft with an iliac crest bone graft or autologous cancellous bone graft (3 cases; 11.5%), or repositioning of the original graft (3 cases; 11.5%). At a mean follow-up of 43.7 months, the average shoulder subjective score was 60.2%, and the average WOSI score was 709.3. There were 3 patients (11.5%) who reported persistent feelings of instability or reported subluxations, but none reported recurrent dislocations. At follow-up (mean, 43.7 months), 34.6% demonstrated progressive degenerative radiographic changes versus before revision imaging.50
Outcomes After Capsular Reconstruction
Overall, 2 studies from 2007 to 2012 characterized the outcomes of revision stabilization with capsular reconstruction in a total of 35 shoulders (30 participants).2,15 Both studies were level 4. The mean follow-up was 37.2 months, and the range of reported recurrent postoperative instability was 30.0% to 33.0%. The weighted mean recurrent instability rate was 31.0%, and the weighted mean revision rate was 22.8%.
Alcid et al2 reported the outcomes of capsular reconstruction using a hamstring tendon autograft (9 patients) or tibialis anterior tendon allograft (6 patients) at a minimum 2-year follow-up. These patients had undergone an average of 2.1 prior surgical procedures (range, 1-4), and 7 patients had capsular deficiency related to previous thermal capsular shrinkage. The amount of glenoid bone loss was not reported. There were no postoperative dislocations, but one-third of patients reported subluxations postoperatively. Postoperative motion of the operative shoulder was significantly reduced versus the contralateral side by 21° of external rotation at the side and 24° with the arm in abduction and 4 spinal levels of internal rotation. An improvement in ASES scores was noted, reaching a postoperative mean of 73. There were no significant differences between the hamstring tendon autograft and tibialis anterior tendon allograft groups when comparing patient satisfaction, difference in postoperative pain, function, ASES score, forward elevation, or external or internal rotation range of motion. There were no complaints of functional deficits at the operative donor knee in the autograft group. Overall, 2 patients (13.3%) subsequently went on to undergo total shoulder arthroplasty because of the progression of degenerative arthritis at 42 and 62 months after revision capsular reconstruction. Of note, both had undergone 3 prior surgical procedures on the operative shoulder.3
Dewing et al15 also used a hamstring tendon autograft (2 shoulders) and tibialis anterior tendon allograft (18 shoulders) to perform anterior capsulolabral reconstruction, re-creating the anterior labrum, the middle glenohumeral ligament, and the anterior band of the inferior glenohumeral ligament in patients who had previously failed multiple stabilization procedures (mean, 4.6 prior surgical procedures). Notably, the series included 5 patients (10 shoulders) who had a pre-existing diagnosis of Ehlers-Danlos type III hypermobility, while patients with pre-existing bony deficiencies or arthritis were excluded . With the described tendon-based technique, 45% of shoulders remained completely stable at a mean of 3.8 years, while 25% reported instability but elected to undergo nonoperative management, and 30% had continued instability and underwent subsequent revision surgery (3 revision reconstruction with a tibialis anterior tendon allograft, 1 glenohumeral fusion, and 2 Latarjet procedures) at a mean 11.2 months after initial capsular reconstruction. In the 14 of 20 shoulders that did not progress to follow-up instability procedures, the mean ASES score improved from 43 preoperatively to 84 postoperatively, with 64% highly satisfied with their outcomes. On the other hand, 21% did require additional follow-up procedures for pain.15
Discussion
Recurrent shoulder instability after primary surgical stabilization continues to present a challenging treatment dilemma for orthopaedic surgeons. Improved primary arthroscopic techniques and a trend to intervene early before significant bone loss occurs have prompted an increase in the rate of surgical shoulder stabilization procedures.8 Unfortunately, as the rate of surgical stabilization increases, so too has the need for revision stabilization. Recurrent instability and the need for revision stabilization continue to pose a challenge, with a variety of treatment techniques described. Whether open repair, arthroscopic repair, coracoid transfer, bone block, or capsular reconstruction, most published research has taken the form of small, heterogeneous, and retrospective case series, making an interpretation difficult and limiting generalizability. The findings in the current study, however, do suggest that in the revision setting, Latarjet coracoid transfer offers the lowest combination in terms of the recurrent instability rate (3.8%) and revision rate (0.02%).
This is in contrast to a prior systematic review that concluded that revision with open Bankart repair produced the lowest recurrent instability rate.20 Importantly, the current study included 4 series of revision Latarjet procedures that were published after Friedman et al’s20 work as well as 5 additional studies on the outcomes of open Bankart repair. Similarly, with the additional data from 5 interim studies, we calculated a recurrent instability rate of 16.0% after revision arthroscopic stabilization versus 12.7% previously reported by Abouali et al1 in 2013. These updated conclusions point to the fact that our understanding of best practices must continue to evolve as more outcome data become available with greater consistency in reporting and more detailed accounting of contributing variables such as bone loss.
To this end, similar to prior studies, the current study found many inconsistencies in reporting, including the way that “failure” was defined and reported in publications. Despite this, every attempt was made in this review to define recurrent instability as any sense of instability, including positive apprehension and subjective subluxations in addition to frank dislocations.
Recurrence can occur for various reasons, but one of the most important contributing factors is bone loss. However, in the current review of the literature, there was inconsistent reporting in the degree of bone loss in revision cases, and in some series, these patients were explicitly excluded. The majority of studies included did not report bone loss as a metric in individual participants or specifically quantify the relation of humeral and glenoid bone loss (on-track vs off-track). Accordingly, conclusions are limited beyond the observation that revision arthroscopic repair tended to be employed when the bony glenoid deficit was <10%. Nonetheless, 1 study utilized arthroscopic repair in “moderate” glenoid/humeral bone loss and found a comparable recurrent instability rate independent of the degree of bone loss.31 On the other hand, 2 studies of the revision Latarjet procedure reported on patients with >20% glenoid bone loss and found that in this population, 6.14% suffered recurrent instability, double the overall weighted mean of revision Latarjet procedures.40,43 However, in these cases, recurrent instability was defined as subluxations rather than frank dislocations and may be less clinically significant. Thus, while bone loss certainly influences the decision making of most shoulder surgeons, the fidelity of data in the revision shoulder stabilization setting is still significantly limited by inconsistent and incomplete reporting in case series.
Beyond individual patient factors and recurrence metrics, researchers have also begun to explore higher level decision-making tools, such as cost-effectiveness. To this end, Makhni et al29 compared the cost-effectiveness of revision arthroscopic repair with a revision Latarjet procedure after failed arthroscopic repair using an expected value decision analysis model. Inputs for this model, including procedure costs and clinical outcomes, were obtained from a review of the literature. Interestingly, the authors reported that the revision Latarjet procedure was more cost-effective (US$13,672 vs US$15,287) than revision arthroscopic repair or nonoperative management because of the decreased cost of the procedure and improved functional outcomes (WOSI).
However, when choosing a revision surgical approach, there are a multitude of factors that surgeons must consider beyond the aforementioned. Specifically, the Latarjet procedure is a technically challenging procedure with complication rates as high as 12.3% to 25%, including delayed wound healing, infections, or coracoid fractures/malunion/nonunion.40,43,44 Additionally, some surgeons perform subscapularis tenotomy for the Latarjet procedure, which can serve as a source of instability recurrence, stiffness, or weakness, even after it is repaired anatomically. Thus, despite an advancing body of research and our findings of reduced instability recurrence after revision Latarjet procedures, a revision surgical technique offering clearly superior objective and subjective outcomes remains elusive.
In light of the high recurrent instability rates after primary arthroscopic stabilization, we reviewed findings at revision in the articles to identify potential risk factors or technical errors in arthroscopic shoulder stabilization that resulted in failure of the initial arthroscopic Bankart repair. This is particularly poignant, as arthroscopic stabilization has become the first-line procedure for instability treatment for an increasing number of orthopaedic surgeons. Particularly, Sisto46 noted inadequate postoperative immobilization, large rotator intervals, and technical errors such as improper anchor placement as risk factors that may increase the incidence of failure of arthroscopic Bankart repair. Similarly, Cho et al11 identified multiple patients with retears of the repaired Bankart lesion, nonanatomic reconstruction of the glenoid labrum, failure of repair at the anteroinferior labrum because of improper fixation of suture anchors, and failure to achieve concentric restoration of the capsulolabral bump. Neviaser et al36 also identified anchor placement too medial and too superior as a cause for failure and recurrent instability. These findings at revision surgery highlight the importance of meticulous anatomic repair during arthroscopic Bankart procedures to avoid the recurrence of instability and the need for revision surgery.
Open Bankart repair was traditionally considered the procedure of choice in the revision setting; however, this systematic review revealed similar recurrence and revision rates to revision arthroscopic repair. Several of the reviewed studies of revision open Bankart repair sought to identify the risk factors and contraindications for revision open repair. The identified risk factors included patients with an engaging Hill-Sachs lesion, bony Bankart lesion, atraumatic cause of failure, voluntary dislocations, multiple prior stabilization procedures, multidirectional instability and hyperlaxity, glenohumeral arthritis, and age older than 30 years.11,27,32,52 A careful approach should be considered when treating such abnormalities. These patients should be counseled appropriately if revision open Bankart repair is being considered, to ensure appropriate expectations for functional outcomes including the possibility of recurrent instability and/or loss of range of motion, particularly external rotation.
With respect to capsular reconstruction techniques using a hamstring tendon autograft or tibialis anterior tendon allograft, our review of available case series categorizes these techniques as experimental, to be considered only in salvage scenarios after multiple failed revision procedures. Given the salvage setting of these procedures, interpreting published results is difficult, and outcomes are modest. The available literature reported a high recurrent instability rate, although nearly 70% of patients did not require conversion to arthroplasty or fusion. Clearly, additional work with careful quantification and reporting of comorbid variables (bone loss, age, prior surgical interventions, etc) is required to understand and further develop best practices in this complex patient population.
Other important considerations are patient age and activity levels. Younger patients participating in contact/collision activities have well-documented greater risks of recurrent shoulder instability.49 The current study focused on the adult population, as the majority of the patients in the literature on revision shoulder stabilization were in this population. However, as younger athletes are training more frequently and subspecializing in specific sports earlier, there may be a greater risk of earlier traumatic dislocations leading to earlier surgery and the possibility of revision surgery at younger ages. A study by Blackman et al6 specifically evaluated the outcomes of revision shoulder stabilization in the adolescent population (aged <18 years). The findings are limited because of a small sample size of only 15 patients (14 male, 1 female) in which 13 underwent primary arthroscopic repair and 2 underwent open repair. Nonetheless, in this series, all activity (mean Marx activity score, 14.8) and functional outcomes (mean ASES score, 82.1; mean UCLA score, 30.8) improved at 2 years postoperatively, with an 86% failure-free rate. However, by 5.5-year follow-up, the reoperation rate jumped to 33%.6 Interestingly, there was no difference in outcomes or failure rates when analyzed by type of primary or revision surgery (arthroscopic vs open repair), number of anchors, amount of glenoid bone loss, or presence or depth of Hill-Sachs lesions.6 Of note, all patients were identified as on-track at the time of revision surgery, and the primary mode of failure of revision surgery was a retear at the previous repair site.6 Once again, more focused, higher fidelity work is needed in this specific demographic of young athletes to develop better evidence-based approaches to revision shoulder stabilization.
Limitations
This study has several limitations. The body of evidence included in the systematic review is entirely composed of observational studies. Most of the data reported came from studies of modest methodological quality with level 3 and 4 evidence, which were characterized by consistently low Downs and Black scores. Furthermore, there was significant heterogeneity in techniques (eg, operative positioning, number of anchors, treatment of the subscapularis in open repair) and abnormalities (bone loss, previous thermal capsulorrhaphy), with few studies describing specific postoperative rehabilitation protocols. The large variety of reported outcome tools and measurements further confounds conclusions and generalizability. Finally, the paucity of comparative studies precluded definitive conclusions on the efficacy of revision shoulder stabilization and how best to counsel patients.
Conclusion
The indications for various revision surgical techniques (arthroscopic repair, open repair, coracoid transfer, bone block, capsular reconstruction) were poorly reported, and surgical techniques were inconsistent. Most studies reported improved patient-reported and objective outcomes after surgery, but these outcomes were typically not as good as in the setting of primary stabilization. Revision with the Latarjet procedure demonstrated the lowest combined recurrent instability and repeat revision rates; however, the choice of an optimal revision shoulder stabilization technique depends on a complete evaluation of patient characteristics, goals, bone loss, and complications as well as surgeon comfort with the technique.
Footnotes
Final revision received January 19, 2020; accepted February 12, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.C.L. has received research support from Arthrex and educational support from Smith & Nephew and SouthTech Orthopedics. T.R.J. has received educational support from Smith & Nephew and SouthTech Orthopedics. B.P.G. has received grant support from DJO, educational support from Smith & Nephew and SouthTech Orthopedics, and hospitality payments from Stryker. J.C.R. has received research support from Arthrex, educational support from SouthTech Orthopedics, consulting fees from Stryker, and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abouali JAK, Hatzantoni K, Holtby R, Veillette C, Theodoropoulos J. Revision arthroscopic Bankart repair. Arthroscopy. 2013;29(9):1572–1578. [DOI] [PubMed] [Google Scholar]
- 2. Alcid JG, Powell SE, Tibone JE. Revision anterior capsular shoulder stabilization using hamstring tendon autograft and tibialis tendon allograft reinforcement: minimum two-year follow-up. J Shoulder Elbow Surg. 2007;16(3):268–272. [DOI] [PubMed] [Google Scholar]
- 3. Arce G, Arcuri F, Ferro D, Pereira E. Is selective arthroscopic revision beneficial for treating recurrent anterior shoulder instability. Clin Orthop Relat Res. 2012;470(4):965–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnes CJ, Getelman MH, Snyder SJ. Results of arthroscopic revision anterior shoulder reconstruction. Am J Sports Med. 2009;37(4):715–719. [DOI] [PubMed] [Google Scholar]
- 5. Bartl C, Schumann K, Paul J, Vogt S, Imhoff AM. Arthroscopic capsulolabral revision repair for recurrent anterior shoulder instability. Am J Sports Med. 2011;39(3):511–518. [DOI] [PubMed] [Google Scholar]
- 6. Blackman AJ, Krych AJ, Kuzma SA, Chow RM, Camp C, Dahm DL. Results of revision anterior shoulder stabilization surgery in adolescent athletes. Arthroscopy. 2014;30(11):1400–1405. [DOI] [PubMed] [Google Scholar]
- 7. Boileau P, Richou J, Lisai A, Chuinard C, Bicknell RT. The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy. 2009;25(10):1075–1084. [DOI] [PubMed] [Google Scholar]
- 8. Bonazza NA, Liu G, Leslie DL, Dhawan A. Trends in surgical management of shoulder instability. Orthop J Sports Med. 2017;5(6):2325967117712476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25(3):298–304. [DOI] [PubMed] [Google Scholar]
- 10. Castagna A, Garofalo R, Melito G, Markopoulos N, De Giorgi S. The role of arthroscopy in the revision of failed Latarjet procedures. Musculoskelet Surg. 2010;94(suppl 1):S47–S55. [DOI] [PubMed] [Google Scholar]
- 11. Cho NS, Yi JW, Lee BG, Rhee YG. Revision open Bankart surgery after arthroscopic repair for traumatic anterior shoulder instability. Am J Sports Med. 2009;37(11):2158–2164. [DOI] [PubMed] [Google Scholar]
- 12. Creighton RA, Romeo AA, Brown FM, Jr, Hayden JK, Verma NN. Revision arthroscopic shoulder instability repair. Arthroscopy. 2007;23(7):703–709. [DOI] [PubMed] [Google Scholar]
- 13. Cuellar A, Cuellar R, de Heredia PB. Arthroscopic revision surgery for failure of open Latarjet technique. Arthroscopy. 2017;33(5):910–917. [DOI] [PubMed] [Google Scholar]
- 14. De Giorgi S, Garofalo R, Tafuri S, Cesari E, Rose GD, Castagna A. Can arthroscopic revision surgery for shoulder instability be a fair option? Muscles Ligaments Tendons J. 2014;4(2):226–231. [PMC free article] [PubMed] [Google Scholar]
- 15. Dewing CB, Horan MP, Millett PJ. Two-year outcomes of open shoulder anterior capsular reconstruction for instability from severe capsular deficiency. Arthroscopy. 2012;28(1):43–51. [DOI] [PubMed] [Google Scholar]
- 16. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Flinkkila T, Sirnio K. Open Latarjet procedure for failed arthroscopic Bankart repair. Orthop Traumatol Surg Res. 2015;101(1):35–38. [DOI] [PubMed] [Google Scholar]
- 18. Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. Arthroscopic salvage of failed arthroscopic Bankart repair: a prospective study with a minimum follow-up of 4 years. Am J Sports Med. 2008;36(7):1330–1336. [DOI] [PubMed] [Google Scholar]
- 19. Frank RM, Mellano C, Shin JJ, et al. Clinical outcomes following revision anterior shoulder stabilization: arthroscopic revision stabilization versus Latarjet. Orthop J Sports Med. 2015;3(7 suppl 2):2325967115S00048. [Google Scholar]
- 20. Friedman LGM, Griesser MJ, Miniaci AA, Jones MH. Recurrent instability after revision anterior shoulder stabilization surgery. Arthroscopy. 2014;30(3):372–381. [DOI] [PubMed] [Google Scholar]
- 21. Giannakos A, Vezeridis PS, Schwartz DG, Jany R, Lafosse L. All-arthroscopic revision 22. Eden-Hybinette procedure for failed instability surgery: technique and preliminary results. Arthroscopy. 2017;33(1):39–48. [DOI] [PubMed] [Google Scholar]
- 22. Gottschalk LJ IV, Walia P, Patel RM, et al. Stability of the glenohumeral joint with combined humeral head and glenoid defects. Am J Sports Med. 2016;44(4):933–940. [DOI] [PubMed] [Google Scholar]
- 23. Guyatt GH, Sackett DL, Sinclair JC, Hayward R, Cook DJ, Cook RJ. Users’ guides to the medical literature, IX: a method for grading health care recommendations. Evidence-Based Medicine Working Group. JAMA. 1995;274:1800–1804. [DOI] [PubMed] [Google Scholar]
- 24. Kawasaki T, Ota C, Urayama S, et al. Incidence of and risk factors for traumatic anterior shoulder dislocation: an epidemiologic study in high-school rugby players. J Shoulder Elbow Surg. 2014;23(11):1624–1630. [DOI] [PubMed] [Google Scholar]
- 25. Kim SH, Ha KI, Kim YM. Arthroscopic revision Bankart repair: a prospective outcome study. Arthroscopy. 2002;18(5):469–482. [DOI] [PubMed] [Google Scholar]
- 26. Krueger D, Kraus N, Pauly S, Chen J, Scheibel M. Subjective and objective outcome after revision arthroscopic stabilization for recurrent anterior instability versus initial shoulder stabilization. Am J Sports Med. 2011;39(1):71–77. [DOI] [PubMed] [Google Scholar]
- 27. Levine WN, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Open revision stabilization surgery for recurrent anterior glenohumeral instability. Am J Sports Med. 2000;28(2):156–160. [DOI] [PubMed] [Google Scholar]
- 28. Lunn JV, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg. 2008;17(5):744–750. [DOI] [PubMed] [Google Scholar]
- 29. Makhni EC, Lamba N, Swart E, et al. Revision arthroscopic repair versus Latarjet procedure in patients with recurrent instability after initial repair attempt: a cost-effectiveness model. Arthroscopy. 2016;32(9):1764–1770. [DOI] [PubMed] [Google Scholar]
- 30. Marquardt B, Garmann S, Schulte T, Witt KA, Steinbeck J, Potzl W. Outcome after failed traumatic anterior shoulder instability repair with and without surgical revision. J Shoulder Elbow Surg. 2007;16(6):742–747. [DOI] [PubMed] [Google Scholar]
- 31. McCabe MP, Weinberg D, Field LD, O’Brien MJ, Hobgood ER, Savoie FH., III Primary versus revision arthroscopic reconstruction with remplissage for shoulder instability with moderate bone loss. Arthroscopy. 2014;20(4):444–450. [DOI] [PubMed] [Google Scholar]
- 32. Meehan RE, Petersen SA. Results and factors affecting outcome of revision surgery for shoulder instability. J Shoulder Elbow Surg. 2005;14(1):31–37. [DOI] [PubMed] [Google Scholar]
- 33. Millar NL, Murrell GA. The effectiveness of arthroscopic stabilization for failed open shoulder instability surgery. J Bone Joint Surg Br. 2008;90(6):745–750. [DOI] [PubMed] [Google Scholar]
- 34. Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Neri BR, Tuckman DV, Bravman JT, Yim D, Sahajpal DT, Rokito AS. Arthroscopic revision of Bankart repair. J Shoulder Elbow Surg. 2007;16(4):419–424. [DOI] [PubMed] [Google Scholar]
- 36. Neviaser AS, Benke MT, Neviaser RJ. Open Bankart repair for revision of failed prior stabilization: outcome analysis at a mean of more than 10 years. J Shoulder Elbow Surg. 2015;24(6):897–901. [DOI] [PubMed] [Google Scholar]
- 37. Nicholson GP, Rahman Z, Verma NN, et al. Results of Latarjet coracoid transfer to revise failed arthroscopic instability repairs. Orthop J Sports Med. 2014;2(suppl 1):2325967114S00014. [Google Scholar]
- 38. Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791–796. [DOI] [PubMed] [Google Scholar]
- 39. Patel RV, Apostel K, Leith JM, Regan WD. Revision arthroscopic capsulolabral reconstruction for recurrent instability of the shoulder. J Bone Joint Surg Br. 2008;90(11):1462–1467. [DOI] [PubMed] [Google Scholar]
- 40. Ranalletta M, Rossi LA, Bertona A, Tanoira I, Maignon GD, Bongiovanni SL. Modified Latarjet procedure without capsulolabral repair for the treatment of failed previous operative stabilizations in athletes. Arthroscopy. 2018;34(5):1421–1427. [DOI] [PubMed] [Google Scholar]
- 41. Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair: apparent causes of failure and treatment. J Bone Joint Surg Am. 1984;66(2):159–168. [PubMed] [Google Scholar]
- 42. Ryu RK, Ryu JH. Arthroscopic revision Bankart repair: a preliminary evaluation. Orthopedics. 2011;34(1):17. [DOI] [PubMed] [Google Scholar]
- 43. Schmid SL, Farshad M, Vatanzaro S, Gerber C. The Lateret procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients. J Bone Joint Surg Am. 2012;94(11):e75. [DOI] [PubMed] [Google Scholar]
- 44. Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94(6):495–501. [DOI] [PubMed] [Google Scholar]
- 45. Shin JJ, Mascarenhas R, Patel AV, et al. Clinical outcomes following revision anterior shoulder arthroscopic capsulolabral stabilization. Arch Orthop Trauma Surg. 2015;135(11):1553–1559. [DOI] [PubMed] [Google Scholar]
- 46. Sisto DJ. Revision of failed arthroscopic Bankart repairs. Am J Sports Med. 2007;35(4):537–541. [DOI] [PubMed] [Google Scholar]
- 47. Stein T, Buckup J, Mehling AP, et al. Restoration of joint congruency and the glenoidal labrum after arthroscopic revision Bankart repair: a MRI match-paired analysis comparing primary Bankart repair and the uninjured labrum. Arch Orthop Trauma Surg. 2014;134:1121–1134. [DOI] [PubMed] [Google Scholar]
- 48. Su F, Kowalczuk M, Ikpe S, Lee H, Sabzevari S, Lin A. Risk factors for failure of arthroscopic revision anterior shoulder stabilization. J Bone Joint Surg Am. 2018;100(15):1319–1325. [DOI] [PubMed] [Google Scholar]
- 49. Waterman B, Owens BD, Tokish JM. Anterior shoulder instability in the military athlete. Sports Health. 2016;8(6):514–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Willemot L, De Boey S, Van Tongel A, Declercq G, De Wilde L, Verborgt O. Analysis of failures after the Bristow-Latarjet procedure for recurrent shoulder instability. Int Orthop. 2019;43(8):1899–1907. [DOI] [PubMed] [Google Scholar]
- 51. Zabinski SJ, Callaway GH, Cohen S, Warren RF. Revision shoulder stabilization: 2- to 10-year results. J Shoulder Elbow Surg. 1999;8(1):58–65. [DOI] [PubMed] [Google Scholar]
- 52. Zaremski JL, Galloza J, Sepulveda F, Vasilopoulos T, Michea W, Herman DC. Recurrence and return to play after shoulder instability events in young and adolescent athletes: a systematic review and meta-analysis. Br J Sports Med. 2017;51(3):177–184. [DOI] [PubMed] [Google Scholar]