Abstract
Objective
Post-extubation stridor and hoarseness are important clinical manifestations that indicate laryngeal edema due to intubation. In previous studies the incidence of post-extubation stridor and hoarseness ranged from 1.5% to 26.3% in postoperative patients and patients in the intensive care unit. Female sex and prolonged intubation are reportedly risk factors for post-extubation stridor. However, the risk factors for post-extubation stridor and the appropriate endotracheal tube size in emergency settings remain unknown. This study was performed to identify the risk factors for post-extubation laryngeal edema after emergency intubation.
Methods
A prospective observational study was conducted in a tertiary emergency medical center/trauma center. The primary outcome was post-extubation stridor and hoarseness.
Results
During the study period, 482 emergency intubations and 227 extubations were performed in adult patients. In total, 29% of the patients presented symptoms of stridor and/or hoarseness. Female sex (odds ratio, 2.65; 95% confidence interval, 1.21–5.81) and the duration of intubation (odds ratio, 1.18; 95% confidence interval, 1.05–1.32) were associated with stridor and/or hoarseness.
Conclusions
Patients who undergo emergency intubation have a higher risk of post-extubation upper airway obstruction symptoms than postoperative patients and patients in the intensive care unit, and female sex is associated with these symptoms.
Keywords: Post-extubation stridor, laryngeal edema, emergency intubation, stridor, hoarseness, female
Introduction
Post-extubation stridor and hoarseness are clinical manifestations that indicate laryngeal edema or vocal cord injury due to intubation. Most cases of stridor do not require medical intervention, but stridor can sometimes lead to reintubation because of upper airway obstruction, which is a risk factor for patient mortality and morbidity.1–4 The incidence of post-extubation stridor and hoarseness ranges from 1.5% to 26.3%.5 In general, the extubation failure rate reportedly ranges from 4.6% to 15.6%,1,2,4,6–8 whereas the reintubation rate in patients with post-extubation stridor ranges from 35% to 69%.7,9–11
Patients who are intubated on an emergency basis may have a high risk of post-extubation laryngeal edema for several reasons. First, a lack of patient information at the time of intubation can cause post-extubation laryngeal edema. In clinical emergency settings, physicians rarely obtain the patient’s medical history, including information on previous intubation and tracheostomy, or the physical characteristics of the patient such as body weight and height. Lack of such information may cause a size mismatch between the patient and the endotracheal tube. Second, some patients cannot receive sedative drugs because they are in shock or have hypotension; importantly, the lack of sedative drugs has been associated with a risk of post-extubation stridor.11 Third, a massive transfusion or fluid therapy can also result in laryngeal edema, which might lead to post-extubation stridor.
Previous studies have shown that female sex, prolonged intubation, an increased number of intubation attempts, young age, and trauma are risk factors for post-extubation stridor and laryngeal edema in postoperative patients or patients in the intensive care unit (ICU).10–17 The use of endotracheal tubes of ≥7.0 mm in women is also reportedly a risk factor for post-extubation upper airway obstruction in postoperative patients.18–20 However, the risk factors for post-extubation stridor and the appropriate endotracheal tube size in the emergency setting remain unknown.
The purpose of this study was to identify the risk factors for post-extubation laryngeal edema in the emergency setting.
Methods
We conducted a prospective observational single-center study at a tertiary emergency medical center/severe trauma center with a 12-bed ICU in Yokohama, Japan. Yokohama city is the second largest city in Japan, with an area of 435 km2 and a population of approximately 3.75 million. Nine emergency medical centers and two severe trauma centers are present in Yokohama.
Adult patients (age of ≥20 years) who were intubated in the emergency room from January 2016 to December 2017 and extubated in the emergency ICU were included in this study. Patients who underwent tracheostomy, were transferred, or died before the first attempt to extubate were excluded.
We used oral tracheal tubes with a subglottic drainage lumen (TaperGuard Evac; Medtronic, Minneapolis, MN, USA) or standard oral tracheal tubes with a stylet (TaperGuard with stylet; Medtronic) depending on device availability. The ICU nurses checked the endotracheal cuff at least once every 8-hour shift, and the cuff pressure was maintained at 20 to 24 cm H2O. Extubation was considered if the following six criteria were met. (1) The disease causing the need for intubation was controlled and had not worsened. (2) No shock or circulatory failure was present. (3) The patient’s level of consciousness was clear or the same as the previous state. (4) The ventilator support had been adequately weaned (positive end-expiratory pressure of approximately ≤5, pressure support of ≤5). (5) Oxygenation was maintained (P/F ratio of ≥200). (6) The tidal volume was high enough for the patient’s body size, and there was no retention of carbon dioxide. We routinely checked for cuff leakage before extubation. The doctor who performed the extubation assessed the patient for symptoms of stridor and hoarseness and indicated on the patients’ sheet whether the patient had these symptoms with a “yes” or “no.”
The following demographic and clinical information was obtained: age, sex, reason for intubation, height, endotracheal tube size and type, use of a sedative drug at intubation, use of a muscle relaxant at intubation, number of intubation attempts, intubation doctor’s years of experience (junior resident: 1–2 years, senior resident: 3–5 years, post-resident: ≥6 years), use of a video laryngoscope or bougie to guide intubation, history of tracheostomy or prolonged (>2 weeks) intubation, duration of intubation before extubation (days), use of steroids before extubation, presence of cuff leakage before extubation, increase in body weight from admission date to extubation date (kg), hospital length of stay, and hospital mortality. The primary outcome was post-extubation stridor and/or hoarseness. The secondary outcome was unplanned reintubation within 48 hours.
For the statistical analysis, we first divided the patients into two groups: those who had post-extubation stridor or hoarseness and those who had no such symptoms. Quantitative variables are expressed as mean ± standard deviation and were compared using an unpaired t-test as appropriate. Categorical variables were compared using the chi-squared test or Fisher’s exact test as appropriate. The multivariate analysis was performed using a logistic regression model for the primary and secondary outcomes. We excluded patients with missing data from the analysis. We also performed a subgroup analysis based on factors that remained significant after the multivariate analysis. In the subgroup analysis, quantitative variables are expressed as median (interquartile range, 25th–75th percentile) and were compared using the Mann–Whitney U test. A p value of <0.05 was considered statistically significant. All statistical analyses were performed using STATA software (Stata/SE 13.0; StataCorp LLC, College Station, TX, USA). We also performed a power analysis using a type I error of 0.05 for the three independent variables in a regression model, which provided a power of 0.81 (PASS 14 Power Analysis and Sample Size Software (2015); NCSS, LLC, Kaysville, UT, USA).
This study was approved by the Institutional Review Board of the Yokohama City University Medical Center (D1506007). We obtained informed consent in the form of an opt-out choice on the website. Those who rejected participation were excluded. We used only routine procedures, and no interventions or invasive treatments were performed in this study.
Results
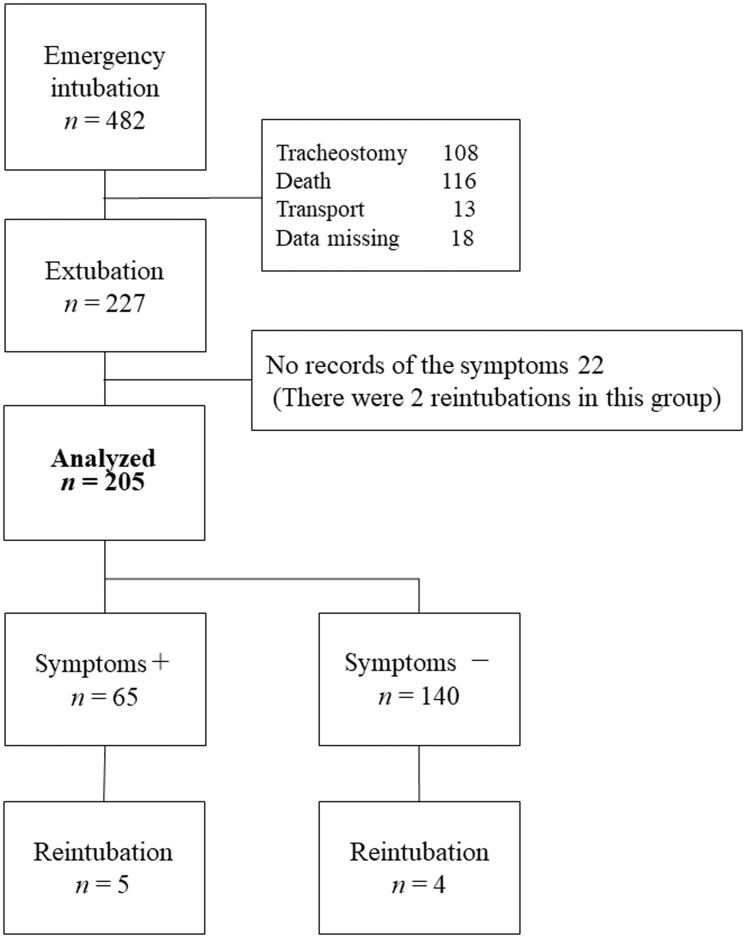
The flow diagram for the study is shown in Figure 1. During the 2-year time period, we performed 482 emergency intubations of adult patients in the emergency department, and 227 patients were included in the study. Twenty-two patients whose records of post-extubation airway obstruction symptoms were lost; therefore, 205 patients were finally analyzed. The patients’ mean height was 163.6 ± 9.58 cm. We used a sedative drug in 189 (83%) patients and a muscle relaxant in 177 (78%) to assist with intubation. We intubated 216 patients with a normal laryngoscope, 10 patients with a video laryngoscope, and 1 patient with a bougie. Of the 205 patients, 172 were intubated with oral tracheal tubes with a subglottic drainage lumen, and only 3 patients were intubated with tracheal tubes without a subglottic drainage lumen; the data regarding the tracheal tube type were missing for 30 patients. The proportion of patients intubated on the first attempt was 85%, and the proportion of those intubated on the second or later attempts was 13%. After extubation, 65 patients (29%) presented stridor and/or hoarseness. Among the 65 patients, 5 (7.7%) required unplanned reintubation within 48 hours because of upper airway obstruction. In addition, six other patients required unplanned reintubation because of respiratory failure or deterioration of consciousness and not because of upper airway obstruction.
Figure 1.
Patient flow diagram. Symptoms included stridor and/or hoarseness.
A comparison of patients with and without symptoms of post-extubation upper airway obstruction is shown in Table 1. Female sex (p < 0.001) and two or more intubation attempts (p = 0.029) were related to stridor and hoarseness. Trauma was the most common reason for intubation, although there was no significant difference between the two groups. Furthermore, the reasons for intubation and the hospital mortality rate were not significantly different between the two groups. The length of hospital stay in patients with symptoms was significantly longer than that in patients without symptoms (29.72 ± 38.81 vs. 18.22 ± 18.24 days, respectively; p = 0.012). The multivariable analysis showed that female sex (odds ratio, 2.65; 95% confidence interval, 1.21–5.81; p = 0.002) and the duration of intubation (OR, 1.18; 95% CI, 1.05–1.32; p = 0.005) were related to stridor and hoarseness (Table 2).
Table 1.
Comparison of patients with and without symptoms of post-extubation upper airway obstruction.
| Characteristics | Symptoms present(n = 65) | Symptoms absent(n = 140) | p value |
|---|---|---|---|
| Age, years | 50.8 ± 19.47 | 54.8 ± 20.39 | 0.185 |
| Female sex | 36 (55%) | 43 (31%) | <0.001 |
| Reason for intubation | 0.409 | ||
| Trauma | 23 (35%) | 47 (34%) | |
| Pneumonia | 1 (2%) | 6 (4%) | |
| Sepsis | 3 (5%) | 8 (6%) | |
| Cardiac arrest | 6 (9%) | 6 (4%) | |
| Overdose | 11 (17%) | 13 (9%) | |
| Brain Stroke | 6 (9%) | 9 (6%) | |
| Seizure | 2 (3%) | 13 (9%) | |
| Burn | 3 (5%) | 6 (4%) | |
| Gastrointestinal bleeding | 3 (5%) | 8 (6%) | |
| Other | 7 (11%) | 24 (17%) | |
| History of tracheostomy or prolonged intubation (>2 weeks) | 0 (0%) | 5 (4%) | 0.113 |
| Two or more intubation attempts | 13 (20%) | 13 (9%) | 0.029 |
| Use of sedative drug at intubation | 58 (89%) | 119 (85%) | 0.412 |
| Use of steroid before extubation | 10 (15%) | 12 (9%) | 0.131 |
| Absence of cuff leakage before extubation | 0 (0%) | 7 (5%) | 0.055 |
| Increase in body weight, kg | 0.11 ± 2.03 | 0.88 ± 3.03 | 0.084 |
| Duration of intubation, days | 5.13 ± 4.28 | 3.94 ± 4.43 | 0.077 |
| Unplanned reintubation within 48 hours | 5 (8%) | 4 (3%) | 0.146 |
| Hospital mortality | 3 (6%) | 6 (5%) | 0.072 |
| Hospital length of stay, days | 29.72 ± 38.81 | 18.22 ± 18.24 | 0.012 |
Data are presented as mean ± standard deviation or n (%).
Table 2.
Multivariate logistic regression of factors associated with symptoms of upper airway obstruction.
| Variables | Odds ratio | 95% Confidence interval | p value |
|---|---|---|---|
| Female sex | 2.65 | 1.21–5.81 | 0.002 |
| Two or more intubation attempts | 2.27 | 0.76–6.80 | 0.144 |
| Duration of intubation | 1.18 | 1.05–1.32 | 0.005 |
Other than the above-listed variables, the regression model was controlled for “absence of cuff leakage” and “use of steroid before extubation.”
We performed a subgroup analysis according to sex because of significance in the multivariable analysis. Among the 89 female patients, 67 (75.3%) patients used endotracheal tubes with a subglottic drainage lumen, 1 patient used an endotracheal tube without a subglottic drainage lumen (inner diameter of 7.0 mm), and the data regarding the tube type were missing for 16 patients. In 11 female patients, 6.5-mm tubes were used; in 62 patients (70%), 7.0-mm tubes were used; and in 13 patients, 7.5-mm tubes were used. The median height of the female patients with symptoms was 157.5 cm (interquartile range, 155–163.3 cm). Interestingly, no variables including height, tube size, intubation attempts, and duration of intubation were significantly associated with symptoms of post-extubation upper airway obstruction in female patients. Among the 138 male patients, 118 (85.5%) received endotracheal tubes with a subglottic drainage lumen, 2 patients received endotracheal tubes without a subglottic drainage lumen (diameter of 7.5 mm for both), and the data regarding the tube type were missing for 14 patients. Overall, 71% of the male patients were intubated with 7.5-mm endotracheal tubes and only 11 were intubated with ≤7.0-mm tubes. For men, more than two intubation attempts were related to stridor and hoarseness (p = 0.006). The median [interquartile range] number of intubation days was significantly higher in those with than without symptoms (5 [3–9] vs. 3 [2–6] days, respectively; p = 0.014), and the median [interquartile range] length of hospital stay was significantly longer in those with than without symptoms (26.5 [12.25–36.75] vs. 12 [8.25–21.25] days, respectively; p = 0.006) (Table 3).
Table 3.
Characteristics and proportions of patients of each sex with symptoms of post-extubation upper airway obstruction.
| Characteristics | Female (n = 36) | Male (n = 29) |
|---|---|---|
| Age, years | 47.5 (31.75–66) | 55 (37–66) |
| Height, cm | 157.5 (155–163.3) | 170 (165–173.2) |
| Inner diameter of endotracheal tube, mm | 7.0 (7.0–7.0) | 7.5 (7.5–7.5) |
| Outer diameter of endotracheal tube, mm | 10.4 (10.4–10.4) | 11.2 (11.2–11.2) |
| History of tracheostomy or prolonged intubation (>2 weeks) | 0 (0%) | 0 (0%) |
| Two or more intubation attempts | 4 (11%) | 9 (31%)* |
| Use of steroid before extubation | 6 (17%) | 4 (14%) |
| Absence of cuff leakage before extubation | 0 (0%) | 0 (0%) |
| Duration of intubation, days | 2 (1.75–5) | 5 (3–9)* |
| Hospital mortality | 2 (7%) | 1 (5%) |
| Hospital length of stay, days | 10 (4.5–38) | 26.5 (12.75–36.75)* |
Data are presented as median (interquartile range) or n (%).
*Significant difference between patients with and without symptoms (p < 0.05).
We analyzed the factors associated with unplanned reintubation within 48 hours. Eleven patients required reintubation, and five of them were reintubated because of upper airway obstruction. There were no significant variables. A total of 7.7% of the patients with symptoms required reintubation, and 4.3% of the patients without symptoms required reintubation; therefore, there was no significant difference in the reintubation rate.
Discussion
In the present study, 29% of patients treated on an emergency basis in the ICU exhibited stridor and/or hoarseness after extubation. Notably, 5 (45%) of the 11 patients who required reintubation had symptoms of post-extubation upper airway obstruction and required reintubation because of airway problems. Female sex and the duration of intubation were significantly associated with stridor and hoarseness.
In previous studies, the incidence of post-extubation stridor ranged from 1.5% to 26.3%,5 and 15% to 45% of reintubations were attributable to upper airway obstruction.6,12,21 Our results suggest that patients who undergo emergency intubation might have a higher risk of post-extubation upper airway obstruction. This risk of post-extubation upper airway obstruction may be increased for multiple reasons. First, in emergency settings, emergency physicians must perform intubation without adequate preparation or information such as the patient’s body weight, history of tracheostomy, and difficulty of intubation. Critically ill patients sometimes have hemodynamic instability. Thus, intubation of critically ill patients in emergency settings has a lower rate of success for the first attempt and is associated with more complications than intubation in the operating room.22,23 Emergency physicians select the endotracheal tube size based mainly on the patient’s physical body size and the clinical experience gained from treating postoperative patients. Lack of information may be the cause of a size mismatch between the patient and the endotracheal tube. Second, intubation without sedative drugs is reportedly a risk factor for post-extubation stridor.11 We intubated 17% of the patients in the present study without the use of sedative drugs, and this might have affected the results.
In our study, female sex was associated with stridor and hoarseness. In previous studies, female sex was found to be a risk factor for post-extubation stridor and laryngeal edema.6,10,11,18–20 The reason for the greater risk of post-extubation laryngeal edema in women has been discussed. One reason is the anatomical feature of airway size; namely, women have smaller airways than men.24–26 In addition, the mucous membrane in women is thought to be more vulnerable than that in men.26 Using endotracheal tubes of ≥7.0 mm in women was reported to be a risk factor for post-extubation upper airway obstruction in postoperative patients.18–20 In these studies, endotracheal tubes without subglottic drainage lumens were used.18,19 Endotracheal tubes with and without subglottic drainage lumens have different outer diameters even if they have the same inner diameter. In this study, the size of the tracheal tubes with respect to both the inner and outer diameters was not different between patients with and without symptoms of post-extubation upper airway obstruction. Only three patients used tubes without subglottic drainage lumens, and most women used 7-mm tubes with subglottic drainage lumens. This might indicate that tracheal tubes with 7-mm inner diameters with subglottic drainage lumens might be relatively large for female patients.
We used height as an indicator of airway size because we cannot measure airway size directly. We compared the heights of patients with and without symptoms of post-extubation airway obstruction by sex, but there was no significant difference (Table 3). Because height and airway size are not perfectly proportional, the 7-mm tube with a subglottic drainage lumen that was used in most patients was thought to be too large for female airways.
Stridor and hoarseness were related to the number of intubation attempts and the duration of intubation in male patients, but there were no significant relationships in female patients. This suggests that even one intubation event and a short duration of intubation may be risk factors for upper airway obstruction in women.
Our study had several limitations. First, this was a single-center study. The generalizability of the findings might be limited; thus, our results might not apply in other situations, hospitals, or geographical areas. Second, almost all of our patients were Asian, and Asian individuals are known to have a small body size.27 This may have affected the results of the study because the appropriate endotracheal tube size may vary according to the patient’s body size. Third, the number of intubation attempts was associated with stridor and hoarseness in male patients, but this factor might be dependent on the physician’s experience. Although the number of years of the physicians’ experience had no relationship with stridor and hoarseness, physicians’ experience with intubation might have varied and thus affected the patient’s outcome. Fourth, this was an observational study, so causation could not be implied. Fifth, we did not use a scoring system for the symptoms of post-extubation stridor/hoarseness to assist with the physicians’ decisions. This might limit the generalizability of our study findings. Additionally, we did not calculate the sample size because this was an exploratory study to determine the current status. However, our power analysis provided a sufficient level of power. A relatively large interventional study that includes measurement of the laryngeal diameter to determine the most appropriate endotracheal tube size, especially for female patients, in emergency intubations is needed.
Conclusion
Patients who undergo emergency intubation have an increased risk of post-extubation upper airway obstruction symptoms, and female sex is associated with these symptoms.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs
Mafumi Shinohara https://orcid.org/0000-0002-2701-1223
Takeru Abe https://orcid.org/0000-0003-3496-1953
References
- 1.Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest 1997; 112: 186–192. [DOI] [PubMed] [Google Scholar]
- 2.Frutos-Vivar F, Esteban A, Apezteguia C, et al. Outcome of reintubated patients after scheduled extubation. J Crit Care 2011; 26: 502–509. [DOI] [PubMed] [Google Scholar]
- 3.Seymour CW, Martinez A, Christie JD, et al. The outcome of extubation failure in a community hospital intensive care unit: a cohort study. Crit Care 2004; 8: R322–R327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miltiades AN, Gershengorn HB, Hua M, et al. Cumulative probability and time to reintubation in united states intensive care units. Crit Care Med 2017; 45: 835–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pluijms WA, Von Mook WN, Wittekamp BH, et al. Postextubation laryngeal edema and stridor resulting in respiratory failure in critically ill adult patients: updated review. Crit Care 2015; 19: 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaber S, Quintard H, Cinotti R, et al. Risk factors and outcome for airway failure versus non-airway failure in the intensive care unit; a multicenter observational study of 1514 extubation procedures. Crit Care 2018; 22: 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaber S, Chanques G, Matecki S, et al. Post-extubation stridor in intensive care unit patients Risk factors evaluation and importance of the cuff-leak test. Intensive Care Med 2003; 29: 69–74. [DOI] [PubMed] [Google Scholar]
- 8.Weinberg JA, Stevens LR, Goslar PW, et al. Risk factors for extubation failure at a level I trauma center: does the specialty of the intensivist matter? Trauma Surg Acute Care Open 2016; 1: e000052. doi: 10.1136/tsaco-2016-000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng KC, Chen CM, Tan CK, et al. Methylprednisolone reduces the rates of postextubation stridor and reintubation associated with attenuated cytokine responses in critically ill patients. Minerva Anestesiol 2011; 77: 503–509. [PMC free article] [PubMed] [Google Scholar]
- 10.Kriner EJ, Shafazand S, Colice GL. The endotracheal tube cuff-leak test as a predictor for postextubation stridor. Respir Care 2005; 50: 1632–1638. [PubMed] [Google Scholar]
- 11.Cheng KC, Hou CC, Huang HC, et al. Intravenous injection of methylprednisolone reduces the incidence of postextubation stridor in intensive care unit patients. Crit Care Med 2006; 34: 1345–1350. [DOI] [PubMed] [Google Scholar]
- 12.Lilienstein JT, Davis JW, Bilello JF, et al. Risk factors associated with post-extubation stridor in the trauma intensive care unit. Am J Surg 2016; 212: 379–383. [DOI] [PubMed] [Google Scholar]
- 13.Lee CH, Peng MJ, Wu CL. Dexamethasone to prevent postextubation airway obstruction in adults: a prospective, randomized, double-blind, placebo-controlled study. Crit Care 2007; 11: R72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maury E, Guglielminotti J, Alzieu M, et al. How to identify patients with no Risk for postextubation stridor? J Crit Care 2004; 19: 23–28. [DOI] [PubMed] [Google Scholar]
- 15.Ding LW, Wang HC, Wu HD, et al. Laryngeal ultrasound: a useful method in predicting post-extubation stridor. A pilot study. Eur Respir J 2006; 27: 384–389. [DOI] [PubMed] [Google Scholar]
- 16.Valles J, Millan S, Diaz E, et al. Incidence of airway complications in patients using endotracheal tubes with continuous aspiration of subglottic secretions. Ann Intensive Care 2017; 7: 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Baradey GF, EL-Shmaa NS, Elsharawy F. Ultrasound-guided laryngeal air column width difference and the cuff leak volume in predicting the effectiveness of steroid therapy on postextubation stridor in adult. Are they useful? J Crit Care 2016; 36: 272–276. [DOI] [PubMed] [Google Scholar]
- 18.Jaensson M, Olowsson LL, Nilsson U. Endotracheal tube size and sore throat following surgery: a randomized-controlled study. Acta Anaesthesiol Scand 2010; 54: 147–153. [DOI] [PubMed] [Google Scholar]
- 19.Jaensson M, Gupta A, Nilsson UG. Risk factors for development of postoperative sore throat and hoarseness after endotracheal intubation in women: a secondary analysis. AANA J 2012; 80: S67–S73. [PubMed] [Google Scholar]
- 20.Hu B, Bao R, Wang X, et al. The size of endotracheal tube and sore throat after surgery: a systematic review and meta-analysis. PLoS One 2013; 8: e74467. doi: 10.1371/journal.pone.0074467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Epstein SK, Ciubotaru RL. Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am J Repir Crit Care Med 1998; 158: 489–493. [DOI] [PubMed] [Google Scholar]
- 22.Ho LI, Harn HJ, Lien TC, et al. Postextubation laryngeal edema in adults risk factor evaluation and prevention by hydrocortisone. Intensive Care Med 1996; 22: 933–936. [DOI] [PubMed] [Google Scholar]
- 23.Griesdale DEG, Bosma TL, Kurth T, et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008; 34: 1835–1842. [DOI] [PubMed] [Google Scholar]
- 24.Alkhouri H, Vassiliadis J, Murray M, et al. Emergency airway management in Australian and New Zealand emergency departments: a multicenter descriptive study of 3710 emergency intubations. Emerg Med Australas 2017; 29: 499–508. [DOI] [PubMed] [Google Scholar]
- 25.Darmon JY, Rauss A, Dreyfuss D, et al. Evaluation of risk factors for laryngeal edema after tracheal extubation in adults and its prevention by dexamethasone. A placebo-controlled, double-blind, multicenter study. Anesthesiology 1992; 77: 245–251. [DOI] [PubMed] [Google Scholar]
- 26.Wittekamp BH, Van Mook WN, Tjan DH, et al. Clinical review: post-extubation laryngeal edema and extubation failure in critical ill adult patients. Crit Care 2009; 13: 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perkins JM, Subramanian SV, Smith GD, et al. Adult height, nutrition, and population health. Nutr Rev 2016; 74: 149–165. [DOI] [PMC free article] [PubMed] [Google Scholar]