Abstract
Background:
The majority of previous investigations on operative fixation of clavicle fractures have been related to the adult population, with occasional assessments of the younger, more commonly affected adolescent population. Despite limited prospective data for adolescents, the incidence of operative fixation of adolescent diaphyseal clavicle fractures has increased.
Purpose:
To detail the demographic features and descriptive epidemiology of a large pooled cohort of adolescent patients with diaphyseal clavicle fractures presenting to pediatric tertiary care centers in the United States through an observational, prospective, multicenter cohort study (Function after Adolescent Clavicle Trauma and Surgery [FACTS]).
Study Design:
Cross-sectional study; Level of evidence, 4.
Methods:
Patients aged 10 to 18 years who were treated for a diaphyseal clavicle fracture between August 2013 and February 2016 at 1 of 8 geographically diverse, high-volume, tertiary care pediatric centers were screened. Treatment was rendered by any of the pediatric orthopaedic providers at each of the 8 institutions, which totaled more than 50 different providers. Age, sex, race, ethnicity, fracture laterality, hand dominance, mechanism of injury, injury activity, athletic participation, fracture characteristics, and treatment decisions were prospectively recorded in those who were eligible and consented to enroll.
Results:
A total of 545 patients were included in the cohort. The mean age of the study population was 14.1 ± 2.1 years, and 79% were male. Fractures occurred on the nondominant side (56%) more frequently than the dominant side (44%). Sport was the predominant activity during which the injury occurred (66%), followed by horseplay (12%) and biking (6%). The primary mechanism of injury was a direct blow/hit to the shoulder (60%). Overall, 54% were completely displaced fractures, defined as fractures with no anatomic cortical contact between fragments. Mean shortening within the completely displaced group was 21.9 mm when measuring the distance between fragment ends (end to end) and 12.4 mm when measuring the distance between the fragment end to the corresponding cortical defect (cortex to corresponding cortex) on the other fragment (ie, true shortening). Comminution was present in 18% of all fractures. While 83% of all clavicle fractures were treated nonoperatively, 32% of completely displaced fractures underwent open reduction and internal fixation.
Conclusion:
Adolescent clavicle fractures occurred more commonly in male patients during sports, secondary to a direct blow to the shoulder, and on the nondominant side. Slightly more than half of these fractures were completely displaced, and approximately one-fifth were comminuted. Within this large cohort, approximately one-third of patients with completely displaced fractures underwent surgery, allowing for future prospective comparative analyses of radiographic, clinical, and functional outcomes.
Keywords: clavicle fracture, adolescent, pediatric, clavicle fixation
The treatment of pediatric and adolescent clavicle fractures has evolved during the past 15 years, with a trend toward operative fixation.26,29 Before the turn of the last century, the rate of surgical treatment of clavicle fractures in children was approximately 1.6%.8 Today, the rate of surgical treatment of clavicle fractures has been reported to be somewhere between 21.9% and 25.9%, even though no high-level evidence has supported this trend in this younger age group.29 Several randomized high-level studies in adults have suggested that operative fixation of displaced clavicle fractures may decrease complications such as nonunion and symptomatic malunion, but there remains controversy regarding the degree to which surgery improves functional outcomes, particularly beyond 6 months after treatment.2,3,13,21,25 Despite this controversy, many utilize fracture shortening ≥20 mm as an indication for performing surgery.5,9,28
This trend toward increased rates of surgical treatment for managing pediatric and adolescent clavicle fractures has been shown to be influenced largely by the adult literature,3 but no comparative investigations have explored the inherent anatomic, physiological, and biological differences between the pediatric and adult clavicles as they relate to injury and surgery.
A vast array of orthopaedic conditions have undergone improved understanding based on large, descriptive epidemiological reports.4,11,18,20 Interestingly, a report of 1000 clavicle fractures across multiple pediatric and adult age groups from a single geographic area estimated the incidence to be 29.14 per 100,000 per year, with the 13- to 20-year-old age group having at least twice the incidence of any other age group.20 Thus, it appears that our understanding of clavicle fracture treatments and their associated outcomes is poorest in the subpopulation most affected by the condition. In a small, single-institution descriptive study of 72 adolescent clavicles, 92% had diaphyseal fractures.18 Replicating such an epidemiological assessment in a much larger cohort of diaphyseal clavicle fractures in the pediatric and adolescent age group is warranted but only if performed across a geographically diverse population. The purpose of the current study was therefore to provide a more detailed description of the epidemiology of adolescent diaphyseal clavicle fractures derived from the first 3 years of patient enrollment in a large, multicenter, prospective cohort study.
Methods
Study Design
A multicenter study group was formed in 2013 to investigate adolescent clavicle fracture treatments (Function after Adolescent Clavicle Trauma and Surgery [FACTS]). The resulting prospective cohort study drew patients from 8 geographically diverse, tertiary pediatric hospitals of different sizes and payer mixes. The primary purpose of this cohort study was to investigate the safety, cost, and outcomes of the operative and nonoperative treatment of adolescent clavicle fractures in a comparative fashion. Each participating institution obtained institutional review board approval and entered into a data-sharing agreement with the host institution. Institutions were recruited based on their geographic location, research infrastructure, and relatively high-volume pediatric trauma program.
The design of this prospective cohort study involved screening potential clavicle fractures and then enrolling all middiaphyseal fractures in patients aged 10 to 18 years who presented to each institution, regardless of the diagnosing or treating provider at each institution. This included clavicle fractures that presented to nurse practitioners, nonoperative sports medicine providers, and other orthopaedic surgeons not directly involved with the study group. Follow-up regimens and treatments were at the discretion of the provider, in keeping with prudent clinical and cost considerations, but with recommended consideration toward 2-week, 6-week, and 3-month postinjury or postsurgical follow-up clinic visits with radiographs at each visit. Each surgeon from each study institution confirmed the adequacy/appropriateness of enrollment and reviewed all radiographs (see Radiographic Evaluation section). During enrollment, each participant’s parent or guardian was required to provide written and verbal consent according to local institutional review board requirements.
Participants
Inclusion criteria consisted of traumatic diaphyseal clavicle fractures (as diagnosed on radiographs) and patient age 10 to 18 years. Exclusion criteria consisted of pathological (nontraumatic) fractures, underlying metabolic or congenital disorders that systemically affected bone quality (eg, osteogenesis imperfecta) or bone healing, or an inability to complete forms or attend follow-up visits.
Data Collection
HIPAA (Health Insurance Portability and Accountability Act)–compliant web-based data management software (StudyTRAX; ScienceTRAX) was utilized to maintain patient enrollment, capture data elements through a secure portal, and facilitate the transfer of data. Tablets were utilized at each institution for data entry and for participants and their guardians to complete forms at the time of each visit. Paper versions were available and used on an as-needed basis. Confidential health information was able to be viewed by only representatives of the host institution.
Demographic data, including birth year, sex, ethnicity and race, and patient’s range of athletic participation, were collected upon screening. If the patient described himself or herself as an athlete, the athlete was asked to list his or her primary sport. Any prior treatment or previous clavicle fracture (either ipsilateral or contralateral) was recorded. If the patient had a previous clavicle fracture(s), any previous treatment was noted. Injury mechanism, side of injury, and hand dominance were entered by the participants and their guardians but confirmed by the treating provider. Baseline physical examination findings were also noted, including visual appearance of the deformity and a neurovascular assessment.
The disposition of the patient (including treatment) was at the discretion of the treating physician. Management of the patient was noted. If surgery was performed, surgical data, including operative time, approach, implant selection, and intraoperative complications, were collected by the principal investigator at the site based on operative reports and/or direct communication with the operative surgeon.
Radiographic Evaluation
There were 2 upright views of the clavicle obtained for clinical decision making and classification, which included an anteroposterior view and a 15° to 45° anteroposterior cephalad tilt view. Clavicle fractures were classified using the following 2 ways: (1) the AO classification12 for diaphyseal fractures and (2) a descriptive classification emphasizing displacement, consisting of either (a) nondisplaced/minimally displaced, (b) partially displaced or angulated (in which at least 1 cortex was disrupted but at least 1 corresponding cortex remained in contact), or (c) completely displaced (in which there was no anatomic cortical contact between fragments).
A single surgeon from each institution reviewed every radiograph from his or her respective institution to minimize variability. Uniform methods for additional clavicle measurements were used at each institution by a single reader including degrees of shortening, displacement, and angulation. Because some literature-based variation in the measurement techniques for shortening of clavicle fractures exists,17,23 2 different methods were utilized for study purposes. An end-to-end technique was performed by measuring the distance between the most lateral tip of the major medial fragment and the most medial tip of the major lateral fragment23 (Figure 1A). A second cortex-to– corresponding cortex measurement was also made from the fracture tip of the major medial fragment to the corresponding defect, or lucency, on the major lateral fragment, or vice versa, depending on what provided the closest approximation of “true” shortening24 (Figure 1B).
Figure 1.

Anteroposterior radiograph of a diaphyseal fracture of the left clavicle. There were 2 methods to measure fracture shortening: (A) end-to-end (long arrow) and (B) cortex-to–corresponding cortex (short arrow).
Radiographic data were entered into the web-based data management software. Interobserver reliability between surgeons and radiographic data were assessed in a separate methodological study10 in which either good or excellent kappa values were demonstrated for all measurements, other than the AO classification designations and direction of angulation, both of which yielded fair kappa values.7,10,23
Statistical Analysis
Statistical analysis was descriptive, using means, standard deviations, and percentages. Each percentage was calculated using the number with nonmissing data for that characteristic as the denominator.
Results
During the recruitment period, August 2013 to February 2016, a total of 853 clavicle fractures were screened and 550 (65%) enrolled, of which 5 were later found to be ineligible and were excluded, resulting in 545 being analyzed. Exclusions were primarily because of inability to complete forms/refusal to participate (65%), nondiaphyseal fractures (24%), distal clavicle or acromioclavicular injuries (11%), or presentation >90 days from injury or inadequate initial imaging and delayed presentation (7%). Some were excluded for more than 1 reason.
Patient Characteristics
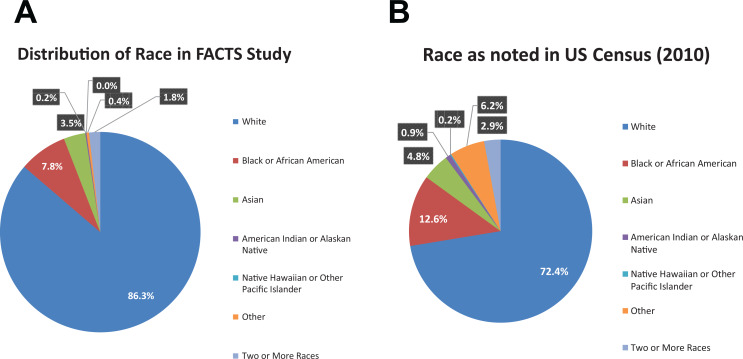
The cohort of 545 patients (79% male) with diaphyseal clavicle fractures had a mean age of 14.1 ± 2.1 years, with 82% of fractures presenting in patients between the ages of 11 and 16 years (Figure 2). The racial distribution of the study cohort is shown in Figure 3. A majority of the enrolled patients were athletes (88%), of whom 68% were competitive athletes. Football, rugby, and soccer were the most common sports played by those who sustained a clavicle fracture (Table 1).
Figure 2.
Histogram of the age at enrollment of patients with diaphyseal clavicle fractures.
Figure 3.
Graphical representation of race in the current study compared with demographics of the overall United States (US) population according to the most recent US Census data (2010). (A) Distribution of race in the FACTS (Function after Adolescent Clavicle Trauma and Surgery) cohort. (B) Distribution of race in the overall US population.
Table 1.
Primary Sport at the Time of Clavicle Fracturea
| Sport | n (%) |
|---|---|
| Football or rugby | 137 (29) |
| Soccer | 104 (22) |
| Baseball | 40 (8) |
| Ice hockey | 38 (8) |
| Basketball | 31 (7) |
| Lacrosse | 24 (5) |
| Skateboarding | 11 (2) |
| Other (<10 each) | 87 (18) |
aPercentage is of 472 athletes who reported their primary sport.
Injury Data
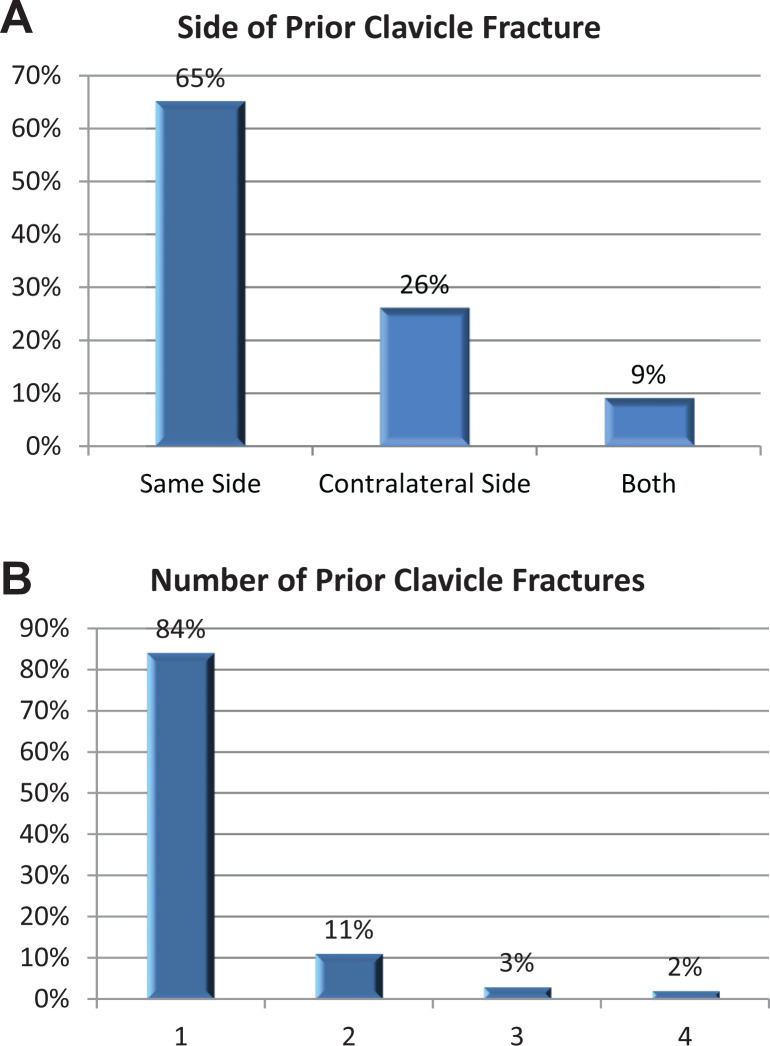
The most commonly described injury activity was sport (66%), with other injury activities including horseplay (12%), biking (6%), a fall or trip (6%), or a motor vehicle accident (3%). The most common mechanism of injury was a direct blow to the shoulder or upper arm (60%). Additional mechanisms included a direct blow to the clavicle or chest (24%) and a fall onto an outstretched hand (11%). The injury was more likely to occur on the left (58%) and nondominant side (56%). A total of 68 patients (13%) reported a previous clavicle fracture (Figure 4).
Figure 4.
Chart demonstrating the (A) location and (B) number of prior clavicle fractures of 68 patients with a prior clavicle fracture.
In this large cohort, there were no cases of an open fracture. While 4% of fractures appeared to be “tenting” the skin, less than 1% were thought to be at risk for skin necrosis at the time of the initial presentation, and none had skin erosion or skin-related complications.
Radiographic Fracture Characteristics
Slightly more than half of fractures were completely displaced (54%). Overall, 33% were partially displaced or angulated, and only 13% were considered nondisplaced or minimally displaced. Approximately 18% of fractures were comminuted. The most common classification according to the AO classification12 was B1.2 (43%) and B1.3 (35%). The most common comminuted fracture pattern was B2.2 or a bending wedge pattern (Figure 5).
Figure 5.
Distribution of fracture patterns according to the AO classification.12
Of the completely displaced fractures, the mean end-to-end measurement was 21.9 mm, while the mean cortex-to–corresponding cortex measurement was 12.4 mm. The mean end-to-end shortening of the operative group was 25.3 mm compared with 20.0 mm for the nonoperative group. Among completely displaced fractures, the mean superior-inferior distance of fracture displacement was 14.5 ± 6.2 mm.
Treatment
Overall, 451 (83%) clavicle fractures were treated nonoperatively, while 32% of completely displaced fractures underwent surgical management (ie, open reduction and internal fixation).
Discussion
The current descriptive epidemiological study provides a more comprehensive assessment than previously provided in the literature of the salient demographic and clinical features of a large cohort of adolescent patients with diaphyseal clavicle fractures from a variety of geographically diverse institutions and treated by a diverse group of pediatric orthopaedic and sports medicine providers. When comparing the current data set with previous epidemiological studies on diaphyseal clavicle fractures in adult populations or combined pediatric and adult populations,18,20 this prospectively studied cohort demonstrated a higher incidence of sport-related injuries (66%) and a higher male-to-female ratio (3.8:1).
Previous descriptive epidemiological studies have been performed by other large multicenter study groups. For example, the Academic Network of Conservational Hip Outcomes Research (ANCHOR) study group provided important demographic baseline data for both femoroacetabular impingement4 and symptomatic acetabular dysplasia,22 while the Multicenter ACL Revision Study (MARS) group investigated the epidemiological characteristics of patients undergoing revision anterior cruciate ligament reconstruction.11 Although there is an increasing emphasis on patient-based outcomes in orthopaedic clinical research, multicenter investigations also have an important responsibility to establish epidemiological baselines for different conditions within a large heterogeneous population. Such data can unearth clinically relevant trends regarding the conditions and their management. For example, the ANCHOR study group demonstrated that the symptom duration for both femoroacetabular impingement4 and symptomatic hip dysplasia22 before undergoing a procedure was greater than 1 year for a majority of patients, establishing this timeline as the norm for these abnormalities or a metric upon which future clinical or research efforts could improve. Such data allow for the creation of quality, safety, and value studies that may improve the speed of diagnosis or decrease the rates of concomitant abnormalities.
The earliest large epidemiological descriptive study on clavicle fractures was by Robinson20 within a combination of pediatric and adult age groups. Although the mean age in that study was 33 years, the most common mechanism and fracture type in the adolescent age group were sport and a displaced diaphyseal fracture, respectively, which are consistent with the data presented in the current cohort. However, the current cohort included fractures from motor vehicle accidents in only 3% of cases, which is much lower than in most adult cohorts. Displacement is likely to be higher in adult cohorts because of the relatively higher energy of motor vehicle accidents as well as a thinner periosteum than that in the pediatric or adolescent population. Postacchini et al18 reported a high rate of completely displaced clavicle fractures in the adolescent age group (67%), which is slightly higher but generally consistent with that of the current study (54%). Interestingly, in a retrospective review of 185 pediatric and adolescent patients with clavicle fractures, Randsborg et al19 found that only 37.8% were displaced. This completely displaced group represents a subset of particular research interest, given that most recent studies comparing surgical versus nonsurgical treatment are limited to completely displaced fractures.16
Historically, male-to-female ratios of clavicle injuries have ranged from 2.8:1 to 7:1.14,19,20,27 The current data corroborate other studies regarding demographic data, such as sex distribution, higher incidence in the nondominant shoulder, and more left shoulder injuries.19,20 In a small retrospective series at a single institution,27 sport (57%) was the most common activity during injury, which is similar to the current study’s rate of 66%. Thus, based on the current data and previous literature,14 adolescent clavicle fractures more frequently occur in the nondominant shoulder, in male patients, in athletes, and during sport activity.21 The most common sports played in the current cohort, football and rugby, are almost exclusively male sports, contributing to this uneven demographic feature of the study population. The phenomenon of the nondominant side may be secondary to slightly less coordination on the nondominant side, leading to less effective bracing during falls or collisions, but the precise cause cannot be gleaned from the current data set. Notably, 2 of the 3 most commonly played contact sports in the cohort, lacrosse and ice hockey, have regional variations in that they are played in northeastern or northern regions, respectively, whereas the most common sport played, football, is generally played across all regions.
Radiographic features, including the most clinically relevant aspects of displacement, comminution, and shortening, are described in the current study, with a particular focus on presenting shortening measurements in 2 different ways. This is critical, given that previous studies by the current study group have demonstrated the end-to-end technique to yield significantly higher values for shortening10 than the cortex-to–corresponding cortex technique. Thus, if some clinicians utilize certain thresholds of shortening as an indication for surgical treatment, awareness of the cortex-to–corresponding cortex method, which may be a truer measure of actual clavicle shortening, is critical for clinicians managing adolescent patients with clavicle fractures.
The current study demonstrates that while 83% of overall clavicle fractures studied in this age group underwent nonoperative treatment, one-third of completely displaced fractures were indicated for surgery. This corresponds to the evolving ratio of nonoperative to operative treatment of adolescent and pediatric clavicle fractures that has mirrored adult clavicle fracture trends over the past decade. A number of different research efforts, including large pediatric institutional studies in the United States,26 database studies from California and New York State,15 a Swedish hospital registry study,6 and a Scandinavian survey study,1 have confirmed this trend. In contrast, Kubiak and Slongo8 reviewed 939 pediatric and adolescent patients with clavicle fractures over a 20-year period. In that series, only 8 diaphyseal clavicle fractures (0.8%) underwent operative management over 2 decades, with the most common reported indication being the “potential for skin perforation.” While the relatively high rate of operatively treated clavicle fractures in the current study may be surprising, it is notable that this is reflective of the independent treatment decisions of more than 50 different pediatric orthopaedic providers, not simply the investigators actively participating in this prospective cohort study. While the elucidation of the details, complications, and comparative outcomes of operative versus nonoperative treatment of adolescent clavicle fractures remains the primary goal of the overall multicenter research effort, with future studies on these topics already under way, the current study was designed specifically to explore only the demographic and descriptive epidemiological features of this particular cohort.
Limitations in the current study include the potential for significant regional variability or diversity among the institutions, which will be the subject of future analyses. Also, the distribution of race within the patient population is not perfectly equivalent to that of the US Census, and the higher percentage of white patients may reflect more access to the tertiary care centers at which the study was conducted. Surgeon diversity may also influence surgical or nonsurgical decision making, the rationale for which was not included in this study. There may also be an element of selection bias in the current study; given that the 8 study institutions represent tertiary care pediatric referral centers, the patient population may represent a subset with more complex adolescent clavicle fractures than the overall population, the majority of whom may present to more local community hospitals or the offices of general orthopaedic surgeons or pediatricians. However, it is the more complex completely displaced fractures that represent the area of greatest clinical controversy, so the potentially higher percentage of such fractures in the overall cohort allows for more focused research on the most clinically significant injuries. While the absence of randomization according to treatment group represents a limitation for future outcome studies, the overall size and relative diversity of the current study population should allow for substratified analyses, statistical regression modeling, and matching techniques to facilitate the assessment of comparative subgroups.
Conclusion
Clavicle fractures in adolescents predominantly occurred in male patients and during sports, and slightly over half of fractures were completely displaced. Compared with historical adolescent data, an increase was seen in this cohort in the operative treatment of completely displaced fractures. Future outcome data are critical to better understand the optimal management of this population.
Acknowledgment
The authors acknowledge the support of the FACTS study research coordinators.
Footnotes
Final revision submitted January 17, 2020; accepted February 1, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study received funding from the Boston Children’s Hospital Program for Patient Safety and Quality (research grant; 2013), Boston Children’s Hospital Trust (private donation; 2015), and Pediatric Orthopaedic Society of North America (POSNA Directed Research Grant; 2015-2018). M.S.K., E.W.E., and B.E.H. have received research funding from AlloSource and Vericel for the Research in OsteoChondritis of the Knee (ROCK) Study Group. H.B.E. has received educational support from Pylant Medical, speaking fees from Smith & Nephew and Synthes, and hospitality payments from Arthrex. P.L.W. has received educational support from Pylant Medical. A.T.P. has received educational support from Sportstek Medical, speaking fees from Smith & Nephew, and consulting fees from OrthoPediatrics. J.J.N. has received educational support from Arthrex and Elite Orthopaedics; speaking fees from Smith & Nephew; and consulting fees from Ceterix Orthopaedics, Responsive Arthroscopy, and Smith & Nephew. S.C.W. has received speaking fees from Arthrex and Smith & Nephew and consulting fees from Smith & Nephew. D.D.S. has received educational support from Gentleman Orthopedics Solutions. N.K.P. has received educational support from Evolution Surgical and consulting fees from OrthoPediatrics. M.S.K. has received consulting fees from OrthoPediatrics, Ossur, and Smith & Nephew; speaking fees from Smith & Nephew; honoraria from Stryker; and royalties from OrthoPediatrics. E.W.E. has received research support from DePuy, consulting fees from OrthoPediatrics, and speaking fees from Arthrex and Ossur. D.M.K. has received speaking fees from Medtronic and consulting fees from WishBone Medical. M.T.B. has received educational support from Arthrex and United Orthopedics, speaking fees from Arthrex, and consulting fees from OrthoPediatrics. B.E.H. has received educational support from Kairos Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Boston Children’s Hospital Institutional Review Board (protocol No. IRB-P00004816).
References
- 1. Ban I, Nowak J, Virtanen K, Troelsen A. Overtreatment of displaced midshaft clavicle fractures. Acta Orthop. 2016;87(6):541–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1–10. [DOI] [PubMed] [Google Scholar]
- 3. Carry PM, Koonce R, Pan Z, Polousky JD. A survey of physician opinion: adolescent midshaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop. 2011;31(1):44–49. [DOI] [PubMed] [Google Scholar]
- 4. Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 5. Hill J, McGuire M, Crosby L. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79(4):537–539. [DOI] [PubMed] [Google Scholar]
- 6. Huttunen TT, Launonen AP, Berg HE, Lepola V, Felländer-Tsai L, Mattila VM. Trends in the incidence of clavicle fractures and surgical repair in Sweden. J Bone Joint Surg Am. 2016;98(21):1837–1842. [DOI] [PubMed] [Google Scholar]
- 7. Jones GL, Bishop JY, Lewis B, et al. Intraobserver and interobserver agreement in the classification and treatment of midshaft clavicle fractures. Am J Sports Med. 2014;42(5):1176–1181. [DOI] [PubMed] [Google Scholar]
- 8. Kubiak R, Slongo T. Operative treatment of clavicle fractures in children: a review of 21 years. J Pediatr Orthop. 2002;22(6):736–739. [PubMed] [Google Scholar]
- 9. Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg. 2006;15:191–194. [DOI] [PubMed] [Google Scholar]
- 10. Li Y, Donohue KS, Robbins CB, et al. Reliability of radiographic assessments of adolescent midshaft clavicle fractures by the FACTS multicenter study group. J Orthop Trauma. 2017;31(9):479–484. [DOI] [PubMed] [Google Scholar]
- 11. MARS Group, Wright RW, Huston LJ, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium–2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21 (10)(suppl):S1–S133. [DOI] [PubMed] [Google Scholar]
- 13. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675–684. [DOI] [PubMed] [Google Scholar]
- 14. Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851–855. [DOI] [PubMed] [Google Scholar]
- 15. Micev AJ. The rising incidence of operative treatment of mid-shaft clavicle fractures. Orthop Muscular Syst. 2016;5(2):1–6. [Google Scholar]
- 16. Namdari S, Ganley TJ, Baldwin K, et al. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop. 2011;31(5):507–511. [DOI] [PubMed] [Google Scholar]
- 17. Pandya NK, Namdari S, Hosalkar HS. Displaced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20(8):498–505. [DOI] [PubMed] [Google Scholar]
- 18. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11(5):452–456. [DOI] [PubMed] [Google Scholar]
- 19. Randsborg P-H, Fuglesang HFS, Røtterud JH, Hammer O-L, Sivertsen EA. Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years. J Pediatr Orthop. 2014;34(4):393–399. [DOI] [PubMed] [Google Scholar]
- 20. Robinson CM. Fractures of the clavicle in the adult: epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476–484. [DOI] [PubMed] [Google Scholar]
- 21. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2013;95(17):1576–1584. [DOI] [PubMed] [Google Scholar]
- 22. Sankar WN, Duncan ST, Baca GR, et al. Descriptive epidemiology of acetabular dysplasia: the Academic Network of Conservational Hip Outcomes Research (ANCHOR) periacetabular osteotomy. J Am Acad Orthop Surg. 2017;25(2):150–159. [DOI] [PubMed] [Google Scholar]
- 23. Silva SR, Fox J, Speers M, et al. Reliability of measurements of clavicle shaft fracture shortening in adolescents. J Pediatr Orthop. 2013;33(3):e19–e22. [DOI] [PubMed] [Google Scholar]
- 24. Smekal V, Deml C, Irenberger A, et al. Length determination in midshaft clavicle fractures: validation of measurement. J Orthop Trauma. 2008;22(7):458–462. [DOI] [PubMed] [Google Scholar]
- 25. Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures: a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23(2):106–112. [DOI] [PubMed] [Google Scholar]
- 26. Suppan CA, Bae DS, Donohue KS, Miller PE, Kocher MS, Heyworth BE. Trends in the volume of operative treatment of midshaft clavicle fractures in children and adolescents: a retrospective, 12-year, single-institution analysis. J Pediatr Orthop B. 2016;25(4):305–309. [DOI] [PubMed] [Google Scholar]
- 27. Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30(4):307–312. [DOI] [PubMed] [Google Scholar]
- 28. Wick M, Muller EJ, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg. 2001;121(4):207–211. [DOI] [PubMed] [Google Scholar]
- 29. Yang S, Werner BC, Gwathmey FW. Treatment trends in adolescent clavicle fractures. J Pediatr Orthop. 2015;35(3):229–233. [DOI] [PubMed] [Google Scholar]