Abstract
Much is being learned about clinical outcomes for adult COVID-19 patients with underlying chronic conditions; however, there is less coverage on how the COVID-19 pandemic impacts the management of chronic medical conditions, such as asthma, in children and youth. Asthma is a common chronic medical condition in children that is uniquely susceptible to changes brought on by COVID-19. Sudden dramatic changes in the environment, medical practice, and medication use have altered the asthma management landscape with potential impacts on asthma outcomes. In this paper, we review how changes in transportation and travel patterns, school attendance, physical activity, and time spent indoors, along with changes in health care delivery since the start of the pandemic, all play a contributing role in asthma control in children. We review potentially important influences of asthma control in children during the COVID-19 pandemic worthy of further study.
Key words: COVID-19, Coronavirus, Asthma, Pediatrics
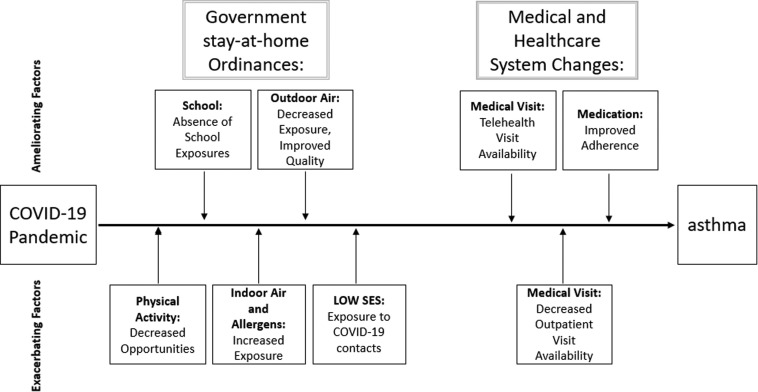
As the COVID-19 pandemic unfolds, we are learning about the multitude of ways, many unforeseen, that response efforts to contain COVID-19 affect people's illnesses and chronic diseases. Although the risk of existing chronic disease on COVID-19 outcomes receives much attention, less discussion has focused on the impact of societal changes resulting from the COVID-19 pandemic on the course of specific chronic conditions. Changes in the environment, medical practice, and medication management and use have rapidly altered the immediate asthma management landscape with likely long-term impacts on asthma outcomes. Where people spend time, daily habits, and travel patterns have altered the natural environment in ways that affect asthma. Changes in health care availability, delivery, and utilization have important implications for asthma and other chronic conditions that require ongoing medical attention. Finally, changes in medication management in asthma represent another important COVID-19-related trend. Chronic asthma has particular vulnerabilities to the changes brought on by COVID-19, with many shared pathways and risk factors, including air quality, the indoor environment, physical activity, weight control, medication management, and health care delivery (see Figure 1 ). Below, we review and postulate how significant changes in 3 domains, environment, medical practice, and medication management, have altered asthma management in the United States with likely longer term implications for asthma outcomes.
Figure 1.
Potentially important influences on asthma control during the COVID-19 pandemic worthy of investigation.
Environmental Changes
As different municipalities and states implement social distancing, including stay-at-home orders, to control the COVID-19 pandemic, they impact many factors that relate to asthma control, morbidity, and mortality. School cancellations mean that children no longer have exposure to viruses from other schoolchildren that can cause upper respiratory illnesses that may exacerbate asthma. Staying at home limits children's opportunities for physical activity, known to be beneficial in asthma. Children now confined to small indoor spaces, without access to school playgrounds or outdoor parks, lose use of spaces that are conducive to physical activity. Children who actively commute to school by walking or bicycling have also lost daily opportunity for physical activity. At the same time, remaining indoors means children have greater exposure to indoor environments that can exacerbate asthma, including secondary tobacco smoke exposure and indoor allergens including mold, mice, and roaches.
With fewer cars on the roads and children spending more time indoors, children will have less exposure to outdoor air pollution. High concentrations of ambient air pollutants, primarily sulfur dioxide, ozone, carbon monoxide, and particulates, worsen asthma. During the summer 1996 Olympics, driving restrictions imposed in downtown Atlanta resulted in lower traffic volume with an accompanying improvement in air quality, all associated with a decrease in emergency department (ED) visits for childhood asthma.1 Air quality has already improved since the start of the COVID-19 pandemic,2 and this improvement should contribute in a positive way to asthma.
Medical Care
Dramatic changes in health care delivery during the COVID-19 pandemic will also impact asthma management and control. Many medical practices in the United States, including primary care and pulmonology practices, have limited office visits to urgent patient needs and have largely moved to telehealth visit formats. These changes have decreased visit volumes in the immediate term; however, the availability of telehealth offers new opportunities for access to care, although some changes exacerbate disparities in access to care. The impact on longer term access to medical providers as the COVID-19 pandemic continues remains unknown and merits careful monitoring. In Boston, we have seen a sharp decrease in asthma-related ED visits since the beginning of the pandemic. At Massachusetts General Hospital, although the number of hospital admissions for COVID-19 gradually increased through March and April, reaching over 1000 confirmed positive patients by the first week of May 2020, the hospital saw a corresponding decline in the usual volume of pediatric asthma–related ED visits (see Table I ). This sharp decrease may reflect families avoiding health care institutions for fear of contracting COVID-19, structural contributing factors based on health care provider recommendations, or early evidence of improved asthma control or beneficial environmental shifts such as improved air quality. Fewer encounters and less use in emergent situations may affect asthma control and outcomes.
Table I.
Change in volume of pediatric asthma emergency department visits during the COVID-19 pandemic
| Timeframe | 2019 | 2020 | % Difference |
|---|---|---|---|
| January | 77 | 82 | 6.5 |
| February | 87 | 80 | −8.0 |
| March | 98 | 60 | −38.8 |
| April | 92 | 14 | −84.8 |
Includes patients under 20 years of age with a J45 International Classification of Diseases, Tenth Revision primary or secondary asthma diagnosis code. The average monthly number of asthma visits in 2019 was 69 patients.
Medication Management
COVID-19 also likely impacts medication prescriptions and adherence. Parents of children with asthma may have heightened concerns about asthma control during a respiratory illness pandemic, potentially increasing medication adherence in their children.3 Parents may be both more likely to fill prescriptions and more vigilant that children take their medications regularly as prescribed. Although increased medication adherence may improve asthma control, altered prescribed medication regimens may also contribute, but in the opposite direction. Preliminary data suggest that corticosteroid use may delay viral clearance4 and be associated with increased mortality in patients infected with COVID-19,5 and some medical providers have moved to limit the use of corticosteroids, both systemic use for acute exacerbations and inhaled corticosteroids for maintenance therapy. How this change in treatment will impact asthma outcomes remains unknown; however, they may well contribute to decreased asthma control and an increase in acute asthma exacerbations and asthma severity.
Although many of these contributing factors are common and ubiquitous across the United States, they likely vary depending on where a child lives and a family's socioeconomic status. Shifts in air quality may have greater consequence in large urban areas, such as New York City and Boston, where COVID-19 hot spots have been reported. Variation in governmental stay-at-home orders will directly impact many of the risk factors listed above, including physical activity and exposure to indoor and outdoor air quality. Accordingly, the impact of COVID-19 on asthma control and outcomes will likely vary from state to state and especially by municipality within states. The associations of asthma prevalence and severity with socioeconomic status, especially income and racial variations, are well described, as well as in asthma management.6 The COVID-19 pandemic may exacerbate these disparities from variations in exposure to risk factors in the home environment. Lower income children in urban environments have more limited access to safe spaces for physical activity. Their families may have unstable housing with a greater risk of exposure to indoor allergens such as mold, rodents, roaches, and tobacco smoke. Low-income children are more likely to live with adults who have ongoing contact with outside populations due to financial stressors or instability. Adults in low-income households are more likely to be essential workers and to take public transportation to work, increasing their exposure risk to COVID-19-infected persons. Children with asthma living in households where 1 or more adults are infected with COVID-19 face an increased risk for medical and psychosocial complications. Although children appear to suffer a lower burden of illness with COVID-19 infection, they are at risk for developing rare but severe complications including a multisystem inflammatory syndrome unique to children.7 It is unclear whether underlying conditions such as asthma place children at greater risk for these rare outcomes. Even in households with infected adults where children do not contract COVID-19, there may be heightened emotional distress that may worsen the child's asthma symptoms. As we approach the warmer spring and summer months, financial complications, where infected low-income adults are unable to work and may not have sufficient finances to pay utility bills, including air conditioning, may in turn impact indoor air quality and children's asthma control.
These COVID-19 changes in the environment, in medical practice, and medication management will likely have a major impact on childhood asthma, with many already manifesting. These several risk factors will often work in opposite directions at the same time. With the pandemic natural experiment absent a control group, it is difficult to foretell the ultimate impacts these broad societal changes will have on childhood asthma. Despite these difficulties, this paper aims to start by identifying key changes in some of the underlying associated risk factors to help the scientific community learn from the pandemic, better guide management of pediatric asthma, and indicate research questions that merit study during these unprecedented times. The exact relationship and impact of the many contributing risk factors will be difficult to measure. Many of the potential influences we highlight in this paper are not typically collected in datasets available for study. Data on some key variables that could help understand the changes and impacts of the COVID-19 pandemic on asthma control are available, including pharmacy claims data, health care utilization measures including asthma-related ED visits and hospitalizations, air quality data, and school closure dates. Innovative studies that combine these disparate datasets will be important to help the scientific community more broadly understand the pandemic's full impact.
Acknowledgments
The authors wish to thank Dr. Ari Cohen and Cassie Kraus for their assistance with providing pediatric emergency department data.
Footnotes
No funding was received for this work.
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
References
- 1.Friedman M.S., Powell K.E., Hutwagner L., Graham L.M., Teague W.G. Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA. 2001;285:897–905. doi: 10.1001/jama.285.7.897. [DOI] [PubMed] [Google Scholar]
- 2.Freedman A, Tierney L The silver lining to coronavirus lockdowns: air quality is improving. The Washington Post. April 9, 2020. https://www.washingtonpost.com/weather/2020/04/09/air-quality-improving-coronavirus/ Available from:
- 3.Propeller Health Propeller data shows 14.5% med adherence lift since COVID-19 outbreak began. https://www.propellerhealth.com/press/clinical-blog/propeller-data-shows-14-5-med-adherence-lift-since-covid-19-outbreak-began/ Available from:
- 4.Xu K., Chen Y., Yuan J., Yi P., Ding C., Wu W. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020;71:799–806. doi: 10.1093/cid/ciaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Z., Liu J., Zhou Y., Zhao X., Zhao Q., Liu J. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020;81:e13–e20. doi: 10.1016/j.jinf.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akinbami L.J., Moorman J.E., Garbe P.L., Sondik E.J. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(Suppl 3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html Available from: