Abstract
Cervical cancer (CC) remains a major disease burden on the female population worldwide. Chemotherapy with cisplatin (cis-diamminedichloroplatinum (II); CDDP) and related drugs are the main treatment option for CC; however, their efficacy is limited by the development of drug resistance. Noncoding RNAs (ncRNAs) have been found to play critical roles in numerous physiological and pathological cellular processes, including drug resistance of cancer cells. In this review, we describe some of the ncRNAs, including miRNAs, lncRNAs and circRNAs, that are involved in the sensitivity/resistance of CC to CDDP-based chemotherapy and discuss their mechanisms of action. We also describe some ncRNAs that could be therapeutic targets to improve the sensitivity of CC to CDDP-based chemotherapy.
Keywords: Cervical cancer, Cisplatin resistance, MicroRNA, Long non-coding RNA, Circular RNA, Noncoding RNAs
Introduction
There are 569,847 new cervical cancer (CC) diagnoses and 311,365 deaths from CC annually worldwide (Bray et al., 2018). Although the majority of CC patients with early stage disease can achieve a favorable prognosis with surgery and radiotherapy, patients with advanced or recurrent disease generally have poor outcomes (Pfaendler & Tewari, 2016; Waggoner, 2003). Nowadays, chemotherapy for CC is mainly used in three aspects: (1) neoadjuvant chemotherapy (NACT) to shrink the tumor before operation; (2) concurrent chemoradiotherapy (CCRT) for middle and advanced patients; (3) palliative chemotherapy for patients with recurrence or metastasis (Moore, 2008; Moore et al., 2010; Pfaendler & Tewari, 2016). Based on the guidelines of National Comprehensive Cancer Network (NCCN) for CC, Cisplatin (cis-diamminedichloroplatinum (II); CDDP) is considered as the first line drug of chemotherapy (National Comprehensive Cancer Network, 2020). However, the treatment response to CDDP varies, and the biggest obstacle to its efficacy is the development of drug resistance (Amable, 2016; Ko & Li, 2019). Thus, there is an urgent need to understand the underlying molecular mechanisms and identify strategies to overcome CDDP resistance in CC.
Noncoding RNAs (ncRNAs) make up the majority of the human transcriptome and are involved in many biological processes, including cell proliferation and differentiation, metabolism, the stress response, and apoptosis. Not surprisingly, abnormal expression and/or activity of ncRNAs has a profound effect on normal physiology and is associated with a number of pathologies, including cancer (Aalijahan & Ghorbian, 2019; Anastasiadou, Jacob & Slack, 2018; Djebali et al., 2012). According to the structural property, ncRNAs can be generally divided into linear ncRNAs and circular ncRNAs (circRNAs). And based on the length of linear ncRNAs, they consist of short ncRNAs such as microRNAs (miRNAs), siRNAs, piwi-interacting RNAs (piRNAs), snoRNAs, snRNAs, as well as long non-coding RNA (lncRNAs), including long intergenic ncRNAs, antisense RNAs (Chan & Tay, 2018; Peng & Calin, 2018).
Deregulation of ncRNAs can also affect the outcome of cancer treatment and allow tumors to acquire drug-resistant phenotypes (Corrà et al., 2018; Wang et al., 2019). An increasing number of studies has shown that ncRNAs play an essential role in CC (Chaichian et al., 2020; He et al., 2016; Hosseini et al., 2017; Sharma, Dua & Agarwal, 2014), and several classes of ncRNAs, such as miRNAs, lncRNAs and circRNAs, have been associated with CDDP resistance, making them important potential therapeutic targets (Matsui & Corey, 2017).
In this review, we summarize the current literature on the contribution of ncRNAs to CDDP resistance in CC (Fig. 1). We focus on studies examining the mechanisms of action of ncRNAs and the potential applications of ncRNAs in predicting CDDP sensitivity and improving chemotherapy regimens in CC, which might provide new therapeutic strategies for patients with CDDP-resistant CC.
Figure 1. The trend chart of published articles related to the advanced of non-coding RNA in the CDDP/CC field over the years.
We counted the articles related to the advanced of non-coding RNA in the CDDP/CC field in PubMed databases from their inception to April 8, 2020. Blue represents miRNA, orange represents lncRNA, and gray represents circRNA.
Survey Methodology
The authors conducted a systematic search with PubMed databases for articles published from their inception to April 8, 2020, to identify relevant studies published in English. The keywords for search include “cervical cancer”, “cisplatin”, “chemotherapy resistance”, “chemoresistance”, “chemosensitivity”, “chemotherapy sensitivity”, “microRNA”, “long noncoding RNA”, “non-coding RNA”, and “circular RNA”. Additional keywords, such as “carcinoma of uterine cervix”, “cervical neoplasia”, “cervix cancer”, “cervical carcinoma”, “carcinoma of cervix”, “circRNA”, “lncRNA”, “miRNA”, “ncRNA”, “noncoding RNA”, “cis-platinum”, “CDDP”, “DDP”, “drug-resistance”, “drug resistance”, and “sensitivity of chemotherapy”, were also used. Additional articles were identified by manual search of references found in the primary articles. The screened articles were used as references for this review.
Mechanisms by Which ncRNAs Affect CDDP Resistance in CC
Mechanisms of action of CDDP
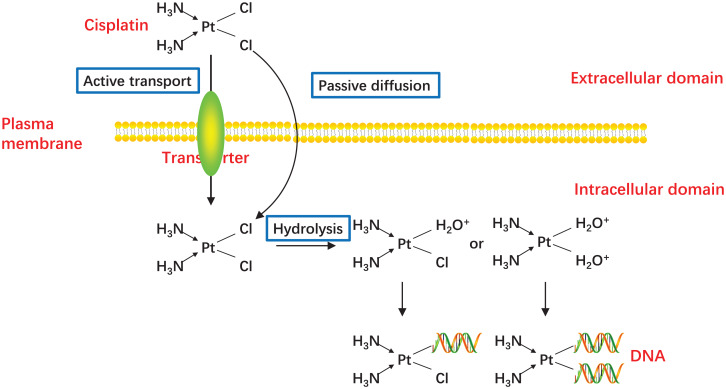
In 1978, CDDP became the first platinum compound to be approved for cancer treatment in the United States (Kelland, 2007), and since then, CDDP has proven to be one of the most effective drugs for the treatment of advanced or recurrent CC (Small et al., 2017). CDDP enters cells mainly by passive diffusion, with contributions from active transport via copper transporters (Holzer, Manorek & Howell, 2006; Ishida et al., 2002). While CDDP itself is inactive, it becomes chemically active in the cytoplasm when one or both of its chlorine atoms are displace by water molecules (Fig. 2) (Galluzzi et al., 2014; Kelland, 2000). Hydrolyzed CDDP exerts its toxic effects by forming DNA-platinum adducts and by simultaneously initiating cellular self-defense systems through the activation or silencing of multiple genes (Eastman, 1987; Yang et al., 2006). DNA damage triggers a complex array of DNA damage response and repair pathways; however, if these processes cannot repair CDDP-induced DNA damage, replication and transcription is blocked, and the cells undergo cell cycle arrest and/or apoptosis (Brabec & Kasparkova, 2005; Dasari & Tchounwou, 2014). The diverse mechanisms by which cells respond to platinum-induced DNA damage provides a wealth of potential mechanisms for cancer cells to evade drug-induced death. Indeed, any factor that influences CDDP binding to DNA, the DNA damage response, or pathways leading to apoptosis could potentially lead to the emergence of drug resistance (Shen et al., 2012). The responsible mechanisms were summarized in Fig. 3.
Figure 2. Activation of CDDP.
CDDP can be passively diffused to tumor cells through the plasma membrane, and the transporter CTR1 is also responsible for CDDP uptake. The concentration of chloride in the blood is relatively high (approximately 100 mM), so the chemical properties of CDDP remain inactive. But the concentration of chloride in the cytoplasm is relatively low (approximately 4–20 mM), one or two of the chloride ligands are replaced by water ligands once CDDP enters into the cells. The hydrolyzed CDDP is highly reactive and mainly targets the nuclear DNA, then the DNA-platinum adducts cause DNA damages.
Figure 3. Schematic representation of intracellular and extracellular mechanisms of the development of CDDP resistance in CC.
Inside the CC cells, decreased uptake of CDDP, increased efflux of CDDP, increased DNA damage repair, alterations in apoptosis-related signaling pathways, oxidative stress, autophagy and epigenetic changes including DNA methylation and ncRNAs are major mechanisms of cisplatin resistance. Outside the CC cells, EMT, cervical CSCs and TME like high cell density, hypoxia and acidity in tumor and the extracellular matrix interactions are also contribute to CDDP resistance. Abbreviation: TME: Tumor microenvironment; EMT: Epithelial-mesenchymal transition; GCL: Glutamate cysteine ligase; CSCs: Cancer stem cells.
Mechanisms by which miRNAs affect CDDP resistance in CC
MiRNAs are short ncRNAs (generally <30 nucleotides) that play roles in post-transcriptional regulation (Lu & Rothenberg, 2018). In most instances, miRNAs act by binding to the 3′-untranslated region (3′-UTR) of the target mRNA, resulting in mRNA destabilization, degradation, or inhibition of translation. Various studies have reported abnormal miRNA expression in CC compared with normal cervical tissue (Juan et al., 2014; Lee et al., 2008), that could affect the proliferation and invasiveness of CC cells and thus their sensitivity to CDDP. Yang et al. (2016c) examined the relative expression of five miRNAs (miR-183, miR-182, miR-30a, miR-15b, and miR-16) and their potential target mRNAs in CDDP-resistant HeLa cell lines compared with their parent HeLa cell line, and they found that miR-182 and miR-15b were upregulated, while miR-30a was significantly downregulated, in the CDDP-resistant cells. Moreover, the mRNA targets of all these miRNAs were shown to be related to drug resistance.
Multiple miRNAs have been shown to influence CC cell growth, survival, and CDDP sensitivity via binding to the target mRNA 3′-UTR (Huang et al., 2017; Li et al., 2015; Sathyanarayanan, Chandrasekaran & Karunagaran, 2017; Yang et al., 2015a). For example, miR-217 binds to KRAS mRNA and directly targets it to mitigate the aggressiveness of CC cells (Yin & Ren, 2019). MiR-181a negatively regulates the expression of the apoptosis-related protein kinase Cδ (PRKCD) by targeting its mRNA for inhibiting apoptosis in CC cells (Chen et al., 2014). MiR-125a binds to STAT3 mRNA and inhibits its translation, resulting in downregulation of CC cell apoptosis and promotion of CDDP resistance (Fan et al., 2016). Finally, miR-144 targeting of the mRNA of LHX2, an oncogenic transcriptional regulator, was found to reverse the CDDP resistance of CC cells (Shi et al., 2019). In addition to these examples, miRNAs may affect CDDP sensitivity through the following mechanisms.
Promotion of drug uptake
Active transport of CDDP into and out of cells occurs via copper transporters, especially copper transporter protein 1 (CTR1, encoded by SLC31A1) (Bompiani et al., 2016; Kalayda, Wagner & Jaehde, 2012; Larson et al., 2009). Accordingly, CDDP-resistant CC cells have been found to express lower levels of CTR1 compared with their CDDP-sensitive counterparts (Zisowsky et al., 2007). Similarly, CTR1 knockdown significantly promotes the proliferation of CC cells in the presence of CDDP, while miR-130a binds directly to SLC31A1 mRNA, thereby regulating CTR1 protein expression (Feng et al., 2018). These results indicate that miRNAs can influence the sensitivity of CC cells to CDDP via regulation of copper transporter expression.
DNA repair
Intrachain and interchain DNA adduct formation by CDDP initiates DNA repair pathways, but a failure to re-establish genomic integrity can lead to cell cycle arrest or apoptosis. DNA repair is mediated predominantly by two processes: nucleotide excision repair and mismatch repair (Shen et al., 2012). Mismatch repair is regulated by several miRNAs, particularly miR-21 and miR-155 (Svrcek et al., 2013). Zhang et al. (2018a) examined gene polymorphisms in 165 chemotherapy-sensitive/resistant CC patients and found that rs1292037 (A > G) locus AG, GG, AG + GG and G allele in miR-21 gene was associated with CDDP sensitivity. Moreover, miR-155 expression also correlates positively with chemosensitivity to CDDP in human CaSki CC cells (Lei et al., 2012). These results indicated a possible link between miRNAs and CDDP sensitivity through the regulation of mismatch repair. Poly (ADP-ribose) polymerase 1 (PARP-1) is an important regulator of DNA repair and is negatively regulated by miR-7-5p, suggesting another mechanism by which miRNAs could contribute to CDDP resistance (Yang et al., 2018). Indeed, the PARP inhibitor olaparib has been shown to enhance the sensitivity of CC cells to CDDP (Prasad et al., 2017), substantiating the potential for miRNAs to provide new therapeutic targets.
Regulation of apoptosis
CDDP can promote cell death through both the external death receptor pathway or the internal mitochondrial pathway, providing a number of mechanisms by which interference with apoptosis might contribute to CDDP resistance. For example, miRNAs could upregulate pro-survival factors such as Bcl-2 and inhibitor of apoptosis protein, or inhibit the expression of tumor suppressor genes such as the caspases. Ectopic expression of miR-214 reduces the expression of the protective Bcl2-like 2 protein and increases the expression of the pro-apoptotic proteins Bax, caspase-9, caspase-8, and caspase-3 in CC cells, leading to enhanced apoptosis and CDDP sensitivity (Wang et al., 2013). Similarly, miRNA-218 can reduce the expression of survivin both in mRNA and protein level, a member of the inhibitor of apoptosis protein family, thereby increasing CDDP sensitivity in CC cells (Yu et al., 2019).
Alterations in signaling pathways that promote cell death can also lead to CDDP resistance, and blockade of these pathways with pharmacological inhibitors and/or RNA interference may have therapeutic effects. A number of miRNAs have been shown to contribute to CDDP resistance in CC cells through such mechanisms. Downregulation of the LDLR–PTEN pathway by miR-92b leads to activation of the AKT pathway in CC cells, which inhibits apoptosis (Sun et al., 2019). Overexpression of miR-218 inhibits proliferation and induces apoptosis in HeLa cells through inhibiting the AKT–mTOR signaling pathway (Li, Ping & Ning, 2012). PKC signaling is another key pathway for the regulation of chemosensitivity in cancer cells (Clark et al., 2003; Mohanty, Huang & Basu, 2005; Yang et al., 2016b). As noted earlier, miR-181a is a negative regulator of PRKCD and inhibits apoptosis in CC cells, thereby enhancing CDDP resistance (Chen et al., 2014). Taken together, these observations identify a large number of miRNAs and related signaling pathways that could serve as novel therapeutic targets to overcome CDDP resistance in CC.
Epithelial-mesenchymal transition
Epithelial-mesenchymal transition (EMT) is the process by which epithelial cells acquire a mesenchymal phenotype and is a critical element in the behavior of cancer cells, including chemotherapy resistance in CC (Goto et al., 2017; Li et al., 2018; Xiong et al., 2017). The crucial role played by miRNAs in regulating the EMT is considered to be another potential mechanism by which CC cells acquire CDDP resistance (Xu et al., 2017). CDDP-resistant CC cells display more EMT characteristics and increased migration and invasion compared with CDDP-sensitive cells (Song & Li, 2017). MiR-25-3p and miR-31-3p reverse the mesenchymal phenotype of CC cells by directly targeting semaphorin 4C, thus increasing CDDP sensitivity (Jing et al., 2019; Song & Li, 2017). MiR-20a mediates EMT that induced by protein phosphatase 1, regulatory subunit 13 like (PPP1R13L) and regulates CDDP resistance in HeLa cells (Xiong et al., 2017). In addition, CDDP sensitivity of CaSki cells is increased by treatment with epidermal growth factor, leading to upregulated miR-155 and reversal of the EMT (Lei et al., 2012). These results suggest that miRNAs regulating the EMT could be targets for reducing CDDP resistance in CC.
Targeting CSCs
As a rule, chemotherapy targets non-stem cell tumor cells, leaving an increased proportion of drug-resistant cancer stem cells (CSCs) in the tumor (Carnero et al., 2016; Leon et al., 2016; Nassar & Blanpain, 2016). Consequently, CSCs have become a potential target for therapeutic intervention for many cancers, including CC (Cao et al., 2017; Chhabra, 2015; Mendoza-Almanza et al., 2019). For example, miR-23b-mediated reduction of ALDH1A1 disturbs the homeostasis of cervical CSCs and promotes the CDDP sensitivity, overexpression of miR-23b re-sensitizes CC cells to CDDP treatment (Wang et al., 2017b).
Oxidative stress
The combination of CDDP and nucleophilic substances or thiol-containing proteins, such as glutathione and glutathione-S-transferase, can consume intracellular antioxidant reserves, thereby promoting oxidative stress, and excessive reactive oxygen species results in cell apoptosis or death (Lewis, Hayes & Wolf, 1988; Zhang et al., 2016). Thus, miR-497, which directly targets transketolase mRNA and promotes the generation of glutathione, reduces oxidant levels, and induces CDDP chemoresistance in CC cells (Yang et al., 2016a).
The mechanisms by which lncRNAs affect CDDP resistance in CC
LncRNAs (>200 nucleotides) play important roles in gene transcription, protein translation, and chromatin remodeling (Kornienko et al., 2013). Not surprisingly, lncRNAs have been shown to be involved in many of the pathological behaviors of CC cells, including aberrant proliferation, migration, and invasion (Dong et al., 2017; Liang et al., 2019; Liu et al., 2018b; Zhu et al., 2018). Recent evidence has confirmed the roles of lncRNAs in CDDP resistance in CC (Iden et al., 2016; Wang et al., 2018).
LncRNAs can act as competitive endogenous RNAs (ceRNAs) by inhibiting the ability of miRNAs to interact with the same target mRNAs (Wilusz, Sunwoo & Spector, 2009; Yamamura et al., 2018; Yoon, Abdelmohsen & Gorospe, 2014). Alterations in critical interactions of the ceRNA regulatory network may thus affect CDDP resistance in CC. HOXD antisense growth-associated lncRNA (HAGLR) has been shown to act as a ceRNA for miR-130a-3p, thereby upregulating the expression of the miR-130a-3p target mRNA zinc finger E-box binding homeobox 1 (Chi et al., 2018). Similarly, crosstalk between the lncRNA NCK1-DT, miR-134-5p, and MutS protein homolog 2 has been shown to play a role in CDDP resistance (Zhang et al., 2019). The lncRNAs cancer susceptibility candidate 2 (CASC2) and growth arrest-specific 5 (GAS5) both act as ceRNAs for miR-21. CASC2 binding to miR-21 upregulates PTEN expression, reducing the phosphorylation of AKT (Feng et al., 2017); whereas GAS5 binding to miR-21 decreases CC cell apoptosis via STAT3 mRNA (Yao et al., 2019). LncRNA DANCR functions as a ceRNA for miR-665, which regulates ERK–SMAD signaling in CC cells (Cao et al., 2019).
LncRNAs also affect CDDP resistance by direct regulation of signaling pathway components. Knockdown of the lncRNA plasmacytoma variant translocation 1 (PVT1) in the human CC cell line SiHa upregulates the level of active caspase-3, which increases CDDP-induced apoptosis (Iden et al., 2016). Similarly, lncRNA taurine-upregulated gene 1 (TUG 1) promotes CDDP resistance in the disease progression of CC through activating the MAPK pathway (Wei et al., 2019). Besides, upregulation of lncRNA MALAT1 increases the expression of phosphorylated PI3K and AKT in HeLa and C-33A cells and promotes their CDDP resistance (Wang et al., 2018).
Many other ceRNA–miRNA–mRNA regulatory networks that contribute to CDDP resistance undoubtedly exist, and expanding our understanding of those mechanisms will provide more therapeutic opportunities for overcoming CDDP resistance.
The mechanisms by which circRNAs affect CDDP resistance in CC
CircRNAs are endogenous ncRNAs which characterized by covalently closed loop without any 5′-3′ polarity or a polyadenylated tail (Chen & Yang, 2015). In recent years, increasing studies have found that circRNAs widespread expressed and played critical roles in biological processes such as tumor cell proliferation, apoptosis, invasion, and migration (Guo et al., 2014; Liu et al., 2018a; Memczak et al., 2013; Zhong et al., 2018). A study revealed 45 significantly highly expressed circRNAs in CC tissue through microarray analysis (Gao et al., 2017). Several studies have indicated that circRNAs were involved in CC development and progression by sponging miRNAs (Cai et al., 2019; Mao, Zhang & Li, 2019; Tang et al., 2019; Zhang et al., 2018b).
Since circRNAs can interact with miRNAs and modulate their expressions, they may also regulate the chemosensitivity of CDDP in CC. A study demonstrated that circMTO1 (mitochondrial translation optimization 1 homologue, ID: hsa_circ_0007874) could promote CC cell tumorigenesis and CDDP resistance through sponging miR-6893 (Chen et al., 2019). Another study identified hsa_circ_0023404 directly interacted with miR-5047 and inhibited autophagy-induced apoptosis to confer CDDP resistance of CC cells (Guo et al., 2019). CircRNAs play a significant role in chemoresistance of CC and may serve as future therapeutic biomarkers.
In addition to miRNAs, lncRNAs and circRNAs, piRNAs, as a new class of ncRNAs, have also shown a potential role in regulating CDDP resistance in CC. The upregulated expression of piR-651 was confirmed in HeLa cells, suggested that piRNAs may be involved in the development of CC (Cheng et al., 2011). Moreover, Hiwi, as a human homologue of the Piwi family and interacting with piRNAs, was found to be involved in the resistance of CC cells to CDDP (Liu et al., 2014). For most ncRNAs, our knowledge regarding their biological function is still limited, but their potential roles in pathogenesis and chemotherapy resistance of CC will be recognized in the future.
Perspectives
CDDP effectively prolongs the survival of CC patients, but its efficacy and clinical application are limited by frequent emergence of drug resistance. As noted above, several ncRNAs associated with CDDP sensitivity/resistance of CC have been identified and are potential drug targets based on results of CC cell experiments (Cheng et al., 2018; Ping et al., 2018; Shih et al., 2019; Vella et al., 2015). Such ncRNAs may also be useful biomarkers to predict chemosensitivity and thus improve treatment regimens in this patient population.
The ncRNAs known to be differentially expressed in drug-resistant CC compared with normal tissues include miR-7-5p (Yang et al., 2018), miR-21( Feng et al., 2017), miR-130a (Feng et al., 2018), miR-181a (Chen et al., 2014), which are upregulated, and lncRNA CACS2, which is downregulated in CDDP-resistant CC (Feng et al., 2017). Analysis of the expression of ncRNAs in CC patients in combination with other molecular markers may predict the patient’s response and thus identify those who would most benefit from CDDP. The development of high-throughput technology makes the identification of molecular characteristics and genotypes more accurate and efficient, and will help to identify other differentially expressed ncRNAs with the potential to be predictive biomarkers.
The ncRNAs listed in Table 1 are associated with differential CDDP sensitivity, suggesting that ncRNA analogs or inhibitors may increase CDDP activity in humans, as has been demonstrated in cultured cells. Treatment of CDDP-resistant CC cells with a miR-25-3p mimic significantly sensitized them to growth inhibition by CDDP (Song & Li, 2017). Conversely, blockade of miR-7-5p with antisense oligonucleotide -miR-7-5p increased the apoptosis rate of CDDP-resistant CC cells (Yang et al., 2018). However, there have been no clinical trials or clinically relevant animal trials of these agents for CC to date. Adjuvant therapy with ncRNA-based agents may have advantages over other anti-cancer mechanisms, given that a single ncRNA can not only target multiple genes but also modulate resistance to multiple drugs. Nevertheless, there are also many challenges associated with the use of ncRNA-based agents as therapeutic drugs, including their stability in body fluids and tissues, drug delivery issues, and potential off-target effects that might result in an unfavorable safety profile.
Table 1. Recent advances of ncRNAs in cisplatin resistance for cervical cancer.
| NcRNA | ID | Target | Effect on DDP sensitivity in CC | References |
|---|---|---|---|---|
| microRNA | miR-584 | GLI1 | increase | Wang, Feng & Zhang (2020) |
| microRNA | microRNA-708 | Timeless | increase | Zou et al. (2020) |
| microRNA | microRNA-499a | SOX6 | decrease | Chen et al. (2020) |
| microRNA | microRNA-138 | H2AX | increase | Yuan et al. (2020) |
| microRNA | miR-21 | SMAD7 unknown | decrease | Liu, Liu & Wang (2020) and Zhang et al. (2018a) |
| microRNA | miR-574-5p | QKI | increase | Tong et al. (2019) |
| microRNA | miR-218 | Survivin AKT-mTOR signaling pathway |
increase | Yu et al. (2019) and Li, Ping & Ning (2012) |
| microRNA | miR-217 | KRAS | increase | Yin & Ren (2019) |
| microRNA | miR-31-3p | Sema4C | increase | Jing et al. (2019) |
| microRNA | miR-92b | LDLR, PTEN | decrease | Sun et al. (2019) |
| microRNA | miR-144 | LHX2 | increase | Shi et al. (2019) |
| microRNA | miR-1284 | HMGB1 | increase | Chen & Li (2018) |
| microRNA | miR-7-5p | PARP-1, BCL2 | decrease | Yang et al. (2018) |
| microRNA | miR-130a | CTR1 | decrease | Feng et al. (2018) |
| microRNA | miR-20a | iASPP | decrease | Xiong et al. (2017) |
| microRNA | miR-29b | STAT3 signaling pathway | increase | Li et al. (2017) |
| microRNA | miR-23b | ALDH1A1 | increase | Wang et al. (2017b) |
| microRNA | miR-106a/b | SIRT1 | decrease | Raji et al. (2017) |
| microRNA | miR-139-3p | Unknown | increase | Sannigrahi et al. (2017) |
| microRNA | miR-25-3p | Sema4C | increase | Song & Li (2017) |
| microRNA | miR-125a | STAT3 | decrease | Fan et al. (2016) |
| microRNA | miR-497 | TKT | decrease | Yang et al. (2016a) |
| microRNA | miR-182 | PI3K/PTEN/AKT, PDCD4 | decrease | Yang et al. (2016c) |
| microRNA | miR-183 | KIAA1199, BAX | increase | Yang et al. (2016c) |
| microRNA | miR-30a | Beclin1 | increase | Yang et al. (2016c) |
| microRNA | miR-664 | E-Cadherin | increase | Yang et al. (2015b) |
| microRNA | miR-181a | PRKCD | decrease | Chen et al. (2014) |
| microRNA | miR-214 | TFAM Bcl2l2 |
increase increase |
Wen et al. (2014) and Wang et al. (2013) |
| microRNA | miR-155 | TP53, SMAD2 | increase | Lei et al. (2012) |
| microRNA | miR-199a | Unknown | decrease | Lee et al. (2008) |
| LncRNA | PCAT6 | miR-543/ZEB1 | decrease | Ma et al. (2020) |
| LncRNA | HNF1A-AS1 | microRNA-34b/TUFT1 | decrease | Luo et al. (2019) |
| LncRNA | DANCR | miR-665/TGFBR1, ERK/SMAD | decrease | Cao et al. (2019) |
| LncRNA | TUG1 | RFX7, MAPK pathway | decrease | Wei et al. (2019) |
| LncRNA | ZFAS1 | unknown | decrease | Feng et al. (2019) |
| LncRNA | NCK1-AS1 | miR-134-5p/MSH2 | decrease | Zhang et al. (2019) |
| LncRNA | GAS5 | miR-21/STAT3 | decrease | Yao et al. (2019) and Wen et al. (2017) |
| LncRNA | MALAT1 | BRWD1, PI3K/AKT pathway | decrease | Wang et al. (2018) |
| LncRNA | HAGLR | miR-130a-3p, ZEB1 | decrease | Chi et al. (2018) |
| LncRNA | UCA1 | caspase-3, CKD2, surviving, p21 | decrease | Wang et al. (2017a) |
| LncRNA | CASC2 | miR-21, PTEN | increase | Feng et al. (2017) |
| LncRNA | PVT1 | caspase-3 | decrease | Iden et al. (2016) |
| CircRNA | circMTO1 | miR-6893/S100A1 | decrease | Chen et al. (2019) |
| CircRNA | circ_0023404 | miR-5047/VEGFA and autophagy signaling pathway | decrease | Guo et al. (2019) |
In order to solve the non-specific distributions of CDDP and the instability of miRNA in the systemic circulation, Wang and Liang used a liposome carrier to co-deliver two different therapeutics (miRNA-1284 and CDDP) into CC cells, and the carrier was specific towards its receptor overexpressed in CC cells, which resulted in enhanced accumulation of liposomes and increased chemosensitivity of CDDP (Wang & Liang, 2020). This study provides a new insight for ncRNA-based cancer therapy, and there are still many potential hurdles that need to be overcome before it can be tested clinically.
Conclusions
In this review, we have summarized some of our current understanding of ncRNAs that affect CDDP sensitivity in CC. These studies have improved our understanding of the involvement of ncRNAs in drug resistance and provide a starting point for the development of agents to improve the efficacy of CDDP-based chemotherapy regimens and thus the quality of life and prognosis of CC patients.
Funding Statement
This work was supported by grants from Natural Science Foundation of China (No. 81902484) and Medical and Health Talents Project of Jilin Province (2019SCZT003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Xin Wen conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft.
Shui Liu conceived and designed the experiments, prepared figures and/or tables, and approved the final draft.
Jiyao Sheng analyzed the data, prepared figures and/or tables, and approved the final draft.
Manhua Cui conceived and designed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
This is a literature review, and the research in this article did not generate any data or code.
References
- Aalijahan & Ghorbian (2019).Aalijahan H, Ghorbian S. Long non-coding RNAs and cervical cancer. Experimental and Molecular Pathology. 2019;106:7–16. doi: 10.1016/j.yexmp.2018.11.010. [DOI] [PubMed] [Google Scholar]
- Amable (2016).Amable L. Cisplatin resistance and opportunities for precision medicine. Pharmacological Research. 2016;106:27–36. doi: 10.1016/j.phrs.2016.01.001. [DOI] [PubMed] [Google Scholar]
- Anastasiadou, Jacob & Slack (2018).Anastasiadou E, Jacob LS, Slack FJ. Non-coding RNA networks in cancer. Nature Reviews Cancer. 2018;18(1):5–18. doi: 10.1038/nrc.2017.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bompiani et al. (2016).Bompiani KM, Tsai C-Y, Achatz FP, Liebig JK, Howell SB. Copper transporters and chaperones CTR1, CTR2, ATOX1, and CCS as determinants of cisplatin sensitivity. Metallomics: Integrated Biometal Science. 2016;8(9):951–962. doi: 10.1039/C6MT00076B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brabec & Kasparkova (2005).Brabec V, Kasparkova J. Modifications of DNA by platinum complexes: relation to resistance of tumors to platinum antitumor drugs. Drug Resistance Updates. 2005;8(3):131–146. doi: 10.1016/j.drup.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Bray et al. (2018).Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- Cai et al. (2019).Cai H, Zhang P, Xu M, Yan L, Liu N, Wu X. Circular RNA hsa_circ_0000263 participates in cervical cancer development by regulating target gene of miR-150-5p. Journal of Cellular Physiology. 2019;234(7):11391–11400. doi: 10.1002/jcp.27796. [DOI] [PubMed] [Google Scholar]
- Cao et al. (2017).Cao H-Z, Liu X-F, Yang W-T, Chen Q, Zheng P-S. LGR5 promotes cancer stem cell traits and chemoresistance in cervical cancer. Cell Death & Disease. 2017;8(9):e3039. doi: 10.1038/cddis.2017.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao et al. (2019).Cao L, Jin H, Zheng Y, Mao Y, Fu Z, Li X, Dong L. DANCR-mediated microRNA-665 regulates proliferation and metastasis of cervical cancer through the ERK/SMAD pathway. Cancer Science. 2019;110(3):913–925. doi: 10.1111/cas.13921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnero et al. (2016).Carnero A, Garcia-Mayea Y, Mir C, Lorente J, Rubio IT, Lleonart ME. The cancer stem-cell signaling network and resistance to therapy. Cancer Treatment Reviews. 2016;49:25–36. doi: 10.1016/j.ctrv.2016.07.001. [DOI] [PubMed] [Google Scholar]
- Chaichian et al. (2020).Chaichian S, Shafabakhsh R, Mirhashemi SM, Moazzami B, Asemi Z. Circular RNAs: a novel biomarker for cervical cancer. Journal of Cellular Physiology. 2020;235(2):718–724. doi: 10.1002/jcp.29009. [DOI] [PubMed] [Google Scholar]
- Chan & Tay (2018).Chan JJ, Tay Y. Noncoding RNA: RNA regulatory networks in cancer. International Journal of Molecular Sciences. 2018;19(5):1310. doi: 10.3390/ijms19051310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen & Li (2018).Chen J, Li G. MiR-1284 enhances sensitivity of cervical cancer cells to cisplatin via downregulating HMGB1. Biomedicine & Pharmacotherapy. 2018;107:997–1003. doi: 10.1016/j.biopha.2018.08.059. [DOI] [PubMed] [Google Scholar]
- Chen & Yang (2015).Chen LL, Yang L. Regulation of circRNA biogenesis. RNA Biology. 2015;12(4):381–388. doi: 10.1080/15476286.2015.1020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2019).Chen M, Ai G, Zhou J, Mao W, Li H, Guo J. circMTO1 promotes tumorigenesis and chemoresistance of cervical cancer via regulating miR-6893. Biomedicine & Pharmacotherapy. 2019;117:109064. doi: 10.1016/j.biopha.2019.109064. [DOI] [PubMed] [Google Scholar]
- Chen et al. (2014).Chen Y, Ke G, Han D, Liang S, Yang G, Wu X. MicroRNA-181a enhances the chemoresistance of human cervical squamous cell carcinoma to cisplatin by targeting PRKCD. Experimental Cell Research. 2014;320(1):12–20. doi: 10.1016/j.yexcr.2013.10.014. [DOI] [PubMed] [Google Scholar]
- Chen et al. (2020).Chen Y, Song Y, Mi Y, Jin H, Cao J, Li H, Han L, Huang T, Zhang X, Ren S, Ma Q, Zou Z. microRNA-499a promotes the progression and chemoresistance of cervical cancer cells by targeting SOX6. Apoptosis. 2020;25(3–4):205–216. doi: 10.1007/s10495-019-01588-y. [DOI] [PubMed] [Google Scholar]
- Cheng et al. (2018).Cheng C, Qin Y, Zhi Q, Wang J, Qin C. Knockdown of long non-coding RNA HOTAIR inhibits cisplatin resistance of gastric cancer cells through inhibiting the PI3K/Akt and Wnt/β-catenin signaling pathways by up-regulating miR-34a. International Journal of Biological Macromolecules. 2018;107:2620–2629. doi: 10.1016/j.ijbiomac.2017.10.154. [DOI] [PubMed] [Google Scholar]
- Cheng et al. (2011).Cheng J, Guo JM, Xiao BX, Miao Y, Jiang Z, Zhou H, Li QN. piRNA, the new non-coding RNA, is aberrantly expressed in human cancer cells. Clinica Chimica Acta. 2011;412(17–18):1621–1625. doi: 10.1016/j.cca.2011.05.015. [DOI] [PubMed] [Google Scholar]
- Chhabra (2015).Chhabra R. Cervical cancer stem cells: opportunities and challenges. Journal of Cancer Research and Clinical Oncology. 2015;141(11):1889–1897. doi: 10.1007/s00432-014-1905-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi et al. (2018).Chi C, Mao M, Shen Z, Chen Y, Chen J, Hou W. HOXD-AS1 exerts oncogenic functions and promotes chemoresistance in cisplatin-resistant cervical cancer cells. Human Gene Therapy. 2018;29(12):1438–1448. doi: 10.1089/hum.2017.256. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Clark et al. (2003).Clark AS, West KA, Blumberg PM, Dennis PA. Altered protein kinase C (PKC) isoforms in non-small cell lung cancer cells: PKCdelta promotes cellular survival and chemotherapeutic resistance. Cancer Research. 2003;63:780–786. [PubMed] [Google Scholar]
- Corrà et al. (2018).Corrà F, Agnoletto C, Minotti L, Baldassari F, Volinia S. The network of non-coding RNAs in cancer drug resistance. Frontiers in Oncology. 2018;8:327. doi: 10.3389/fonc.2018.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasari & Tchounwou (2014).Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. European Journal of Pharmacology. 2014;740:364–378. doi: 10.1016/j.ejphar.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djebali et al. (2012).Djebali S, Davis CA, Merkel A, Dobin A, Lassmann T, Mortazavi A, Tanzer A, Lagarde J, Lin W, Schlesinger F, Xue C, Marinov GK, Khatun J, Williams BA, Zaleski C, Rozowsky J, Röder M, Kokocinski F, Abdelhamid RF, Alioto T, Antoshechkin I, Baer MT, Bar NS, Batut P, Bell K, Bell I, Chakrabortty S, Chen X, Chrast J, Curado J, Derrien T, Drenkow J, Dumais E, Dumais J, Duttagupta R, Falconnet E, Fastuca M, Fejes-Toth K, Ferreira P, Foissac S, Fullwood MJ, Gao H, Gonzalez D, Gordon A, Gunawardena H, Howald C, Jha S, Johnson R, Kapranov P, King B, Kingswood C, Luo OJ, Park E, Persaud K, Preall JB, Ribeca P, Risk B, Robyr D, Sammeth M, Schaffer L, See L-H, Shahab A, Skancke J, Suzuki AM, Takahashi H, Tilgner H, Trout D, Walters N, Wang H, Wrobel J, Yu Y, Ruan X, Hayashizaki Y, Harrow J, Gerstein M, Hubbard T, Reymond A, Antonarakis SE, Hannon G, Giddings MC, Ruan Y, Wold B, Carninci P, Guigó R, Gingeras TR. Landscape of transcription in human cells. Nature. 2012;489(7414):101–108. doi: 10.1038/nature11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong et al. (2017).Dong J, Su M, Chang W, Zhang K, Wu S, Xu T. Long non-coding RNAs on the stage of cervical cancer (Review) Oncology Reports. 2017;38(4):1923–1931. doi: 10.3892/or.2017.5905. [DOI] [PubMed] [Google Scholar]
- Eastman (1987).Eastman A. The formation, isolation and characterization of DNA adducts produced by anticancer platinum complexes. Pharmacology & Therapeutics. 1987;34(2):155–166. doi: 10.1016/0163-7258(87)90009-X. [DOI] [PubMed] [Google Scholar]
- Fan et al. (2016).Fan Z, Cui H, Yu H, Ji Q, Kang L, Han B, Wang J, Dong Q, Li Y, Yan Z, Yan X, Zhang X, Lin Z, Hu Y, Jiao S. MiR-125a promotes paclitaxel sensitivity in cervical cancer through altering STAT3 expression. Oncogenesis. 2016;5(2):e197. doi: 10.1038/oncsis.2016.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng et al. (2018).Feng C, Ma F, Hu C, Ma J-A, Wang J, Zhang Y, Wu F, Hou T, Jiang S, Wang Y, Feng Y. SOX9/miR-130a/CTR1 axis modulates DDP-resistance of cervical cancer cell. Cell Cycle. 2018;17(4):448–458. doi: 10.1080/15384101.2017.1395533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng et al. (2019).Feng LL, Shen FR, Zhou JH, Chen YG. Expression of the lncRNA ZFAS1 in cervical cancer and its correlation with prognosis and chemosensitivity. Gene. 2019;696:105–112. doi: 10.1016/j.gene.2019.01.025. [DOI] [PubMed] [Google Scholar]
- Feng et al. (2017).Feng Y, Zou W, Hu C, Li G, Zhou S, He Y, Ma F, Deng C, Sun L. Modulation of CASC2/miR-21/PTEN pathway sensitizes cervical cancer to cisplatin. Archives of Biochemistry and Biophysics. 2017;623-624:20–30. doi: 10.1016/j.abb.2017.05.001. [DOI] [PubMed] [Google Scholar]
- Galluzzi et al. (2014).Galluzzi L, Vitale I, Michels J, Brenner C, Szabadkai G, Harel-Bellan A, Castedo M, Kroemer G. Systems biology of cisplatin resistance: past, present and future. Cell Death & Disease. 2014;5(5):e1257. doi: 10.1038/cddis.2013.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao et al. (2017).Gao YL, Zhang MY, Xu B, Han LJ, Lan SF, Chen J, Dong YJ, Cao LL. Circular RNA expression profiles reveal that hsa_circ_0018289 is up-regulated in cervical cancer and promotes the tumorigenesis. Oncotarget. 2017;8(49):86625–86633. doi: 10.18632/oncotarget.21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto et al. (2017).Goto M, Osada S, Imagawa M, Nishizuka M. FAD104, a regulator of adipogenesis, is a novel suppressor of TGF-β-mediated EMT in cervical cancer cells. Scientific Reports. 2017;7(1):16365. doi: 10.1038/s41598-017-16555-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo et al. (2019).Guo J, Chen M, Ai G, Mao W, Li H, Zhou J. Hsa_circ_0023404 enhances cervical cancer metastasis and chemoresistance through VEGFA and autophagy signaling by sponging miR-5047. Biomedicine & Pharmacotherapy. 2019;115:108957. doi: 10.1016/j.biopha.2019.108957. [DOI] [PubMed] [Google Scholar]
- Guo et al. (2014).Guo JU, Agarwal V, Guo H, Bartel DP. Expanded identification and characterization of mammalian circular RNAs. Genome Biology. 2014;15(7):409. doi: 10.1186/s13059-014-0409-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He et al. (2016).He Y, Lin J, Ding Y, Liu G, Luo Y, Huang M, Xu C, Kim T-K, Etheridge A, Lin M, Kong D, Wang K. A systematic study on dysregulated microRNAs in cervical cancer development. International Journal of Cancer. 2016;138(6):1312–1327. doi: 10.1002/ijc.29618. [DOI] [PubMed] [Google Scholar]
- Holzer, Manorek & Howell (2006).Holzer AK, Manorek GH, Howell SB. Contribution of the major copper influx transporter CTR1 to the cellular accumulation of cisplatin, carboplatin, and oxaliplatin. Molecular Pharmacology. 2006;70(4):1390–1394. doi: 10.1124/mol.106.022624. [DOI] [PubMed] [Google Scholar]
- Hosseini et al. (2017).Hosseini ES, Meryet-Figuiere M, Sabzalipoor H, Kashani HH, Nikzad H, Asemi Z. Dysregulated expression of long noncoding RNAs in gynecologic cancers. Molecular Cancer. 2017;16(1):107. doi: 10.1186/s12943-017-0671-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang et al. (2017).Huang Y, Huang H, Li M, Zhang X, Liu Y, Wang Y. MicroRNA-374c-5p regulates the invasion and migration of cervical cancer by acting on the Foxc1/snail pathway. Biomedicine & Pharmacotherapy. 2017;94:1038–1047. doi: 10.1016/j.biopha.2017.07.150. [DOI] [PubMed] [Google Scholar]
- Iden et al. (2016).Iden M, Fye S, Li K, Chowdhury T, Ramchandran R, Rader JS. The lncRNA PVT1 contributes to the cervical cancer phenotype and associates with poor patient prognosis. PLOS ONE. 2016;11(5):e0156274. doi: 10.1371/journal.pone.0156274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishida et al. (2002).Ishida S, Lee J, Thiele DJ, Herskowitz I. Uptake of the anticancer drug cisplatin mediated by the copper transporter Ctr1 in yeast and mammals. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(22):14298–14302. doi: 10.1073/pnas.162491399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing et al. (2019).Jing L, Bo W, Yourong F, Tian W, Shixuan W, Mingfu W. Sema4C mediates EMT inducing chemotherapeutic resistance of miR-31-3p in cervical cancer cells. Scientific Reports. 2019;9(1):87. doi: 10.1038/s41598-019-54177-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan et al. (2014).Juan L, Tong HL, Zhang P, Guo G, Wang Z, Wen X, Dong Z, Tian YP. Identification and characterization of novel serum microRNA candidates from deep sequencing in cervical cancer patients. Scientific Reports. 2014;4(1):6277. doi: 10.1038/srep06277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalayda, Wagner & Jaehde (2012).Kalayda GV, Wagner CH, Jaehde U. Relevance of copper transporter 1 for cisplatin resistance in human ovarian carcinoma cells. Journal of Inorganic Biochemistry. 2012;116:1–10. doi: 10.1016/j.jinorgbio.2012.07.010. [DOI] [PubMed] [Google Scholar]
- Kelland (2007).Kelland L. The resurgence of platinum-based cancer chemotherapy. Nature Reviews Cancer. 2007;7(8):573–584. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- Kelland (2000).Kelland LR. Preclinical perspectives on platinum resistance. Drugs. 2000;59(Suppl. 4):1–8. doi: 10.2165/00003495-200059004-00001. [DOI] [PubMed] [Google Scholar]
- Ko & Li (2019).Ko T, Li S. Genome-wide screening identifies novel genes and biological processes implicated in cisplatin resistance. FASEB Journal. 2019;33(6):7143–7154. doi: 10.1096/fj.201801534RR. [DOI] [PubMed] [Google Scholar]
- Kornienko et al. (2013).Kornienko AE, Guenzl PM, Barlow DP, Pauler FM. Gene regulation by the act of long non-coding RNA transcription. BMC Biology. 2013;11(1):59. doi: 10.1186/1741-7007-11-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson et al. (2009).Larson CA, Blair BG, Safaei R, Howell SB. The role of the mammalian copper transporter 1 in the cellular accumulation of platinum-based drugs. Molecular Pharmacology. 2009;75(2):324–330. doi: 10.1124/mol.108.052381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2008).Lee JW, Choi CH, Choi JJ, Park YA, Kim SJ, Hwang SY, Kim WY, Kim TJ, Lee JH, Kim BG, Bae DS. Altered MicroRNA expression in cervical carcinomas. Clinical Cancer Research. 2008;14(9):2535–2542. doi: 10.1158/1078-0432.CCR-07-1231. [DOI] [PubMed] [Google Scholar]
- Lei et al. (2012).Lei C, Wang Y, Huang Y, Yu H, Huang Y, Wu L, Huang L. Up-regulated miR155 reverses the epithelial-mesenchymal transition induced by EGF and increases chemo-sensitivity to cisplatin in human Caski cervical cancer cells. PLOS ONE. 2012;7(12):e52310. doi: 10.1371/journal.pone.0052310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon et al. (2016).Leon G, MacDonagh L, Finn SP, Cuffe S, Barr MP. Cancer stem cells in drug resistant lung cancer: targeting cell surface markers and signaling pathways. Pharmacology & Therapeutics. 2016;158:71–90. doi: 10.1016/j.pharmthera.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Lewis, Hayes & Wolf (1988).Lewis AD, Hayes JD, Wolf CR. Glutathione and glutathione-dependent enzymes in ovarian adenocarcinoma cell lines derived from a patient before and after the onset of drug resistance: intrinsic differences and cell cycle effects. Carcinogenesis. 1988;9(7):1283–1287. doi: 10.1093/carcin/9.7.1283. [DOI] [PubMed] [Google Scholar]
- Li et al. (2015).Li J, Hu L, Tian C, Lu F, Wu J, Liu L. microRNA-150 promotes cervical cancer cell growth and survival by targeting FOXO4. BMC Molecular Biology. 2015;16(1):24. doi: 10.1186/s12867-015-0052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Ping & Ning (2012).Li J, Ping Z, Ning H. MiR-218 impairs tumor growth and increases chemo-sensitivity to cisplatin in cervical cancer. International Journal of Molecular Sciences. 2012;13(12):16053–16064. doi: 10.3390/ijms131216053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2018).Li RM, Nai MM, Duan SJ, Li SX, Yin BN, An F, Zhai YQ, Liu J, Chu YR, Yu Y, Song WY. Down-expression of GOLM1 enhances the chemo-sensitivity of cervical cancer to methotrexate through modulation of the MMP13/EMT axis. American Journal of Cancer Research. 2018;8:964–980. [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2017).Li Y, Zhang Z, Xiao Z, Lin Y, Luo T, Zhou Q, Zhang X. Chemotherapy-mediated miR-29b expression inhibits the invasion and angiogenesis of cervical cancer. Oncotarget. 2017;8(9):14655–14665. doi: 10.18632/oncotarget.14738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang et al. (2019).Liang H, Zhang C, Guan H, Liu J, Cui Y. LncRNA DANCR promotes cervical cancer progression by upregulating ROCK1 via sponging miR-335-5p. Journal of Cellular Physiology. 2019;234(5):7266–7278. doi: 10.1002/jcp.27484. [DOI] [PubMed] [Google Scholar]
- Liu et al. (2018a).Liu H, Chen D, Bi J, Han J, Yang M, Dong W, Lin T, Huang J. Circular RNA circUBXN7 represses cell growth and invasion by sponging miR-1247-3p to enhance B4GALT3 expression in bladder cancer. Aging. 2018a;10(10):2606–2623. doi: 10.18632/aging.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Liu & Wang (2020).Liu Q, Liu S, Wang D. Overexpression of microRNA-21 decreased the sensitivity of advanced cervical cancer to chemoradiotherapy through SMAD7. Anticancer Drugs. 2020;31(3):272–281. doi: 10.1097/CAD.0000000000000871. [DOI] [PubMed] [Google Scholar]
- Liu et al. (2014).Liu W, Gao Q, Chen K, Xue X, Li M, Chen Q, Zhu G, Gao Y. Hiwi facilitates chemoresistance as a cancer stem cell marker in cervical cancer. Oncology Reports. 2014;32(5):1853–1860. doi: 10.3892/or.2014.3401. [DOI] [PubMed] [Google Scholar]
- Liu et al. (2018b).Liu Y, Yang Y, Li L, Liu Y, Geng P, Li G, Song H. LncRNA SNHG1 enhances cell proliferation, migration, and invasion in cervical cancer. Biochemistry and Cell Biology. 2018b;96(1):38–43. doi: 10.1139/bcb-2017-0188. [DOI] [PubMed] [Google Scholar]
- Lu & Rothenberg (2018).Lu TX, Rothenberg ME. MicroRNA. Journal of Allergy and Clinical Immunology. 2018;141(4):1202–1207. doi: 10.1016/j.jaci.2017.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo et al. (2019).Luo X, Wei J, Yang FL, Pang XX, Shi F, Wei YX, Liao BY, Wang JL. Exosomal lncRNA HNF1A-AS1 affects cisplatin resistance in cervical cancer cells through regulating microRNA-34b/TUFT1 axis. Cancer Cell International. 2019;19(1):323. doi: 10.1186/s12935-019-1042-4. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Ma et al. (2020).Ma Z, Gu G, Pan W, Chen X. LncRNA PCAT6 accelerates the progression and chemoresistance of cervical cancer through up-regulating ZEB1 by sponging miR-543. OncoTargets and Therapy. 2020;13:1159–1170. doi: 10.2147/ott.S232354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao, Zhang & Li (2019).Mao Y, Zhang L, Li Y. circEIF4G2 modulates the malignant features of cervical cancer via the miR218/HOXA1 pathway. Molecular Medicine Reports. 2019;19:3714–3722. doi: 10.3892/mmr.2019.10032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsui & Corey (2017).Matsui M, Corey DR. Non-coding RNAs as drug targets. Nature Reviews Drug Discovery. 2017;16(3):167–179. doi: 10.1038/nrd.2016.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memczak et al. (2013).Memczak S, Jens M, Elefsinioti A, Torti F, Krueger J, Rybak A, Maier L, Mackowiak SD, Gregersen LH, Munschauer M, Loewer A, Ziebold U, Landthaler M, Kocks C, Le Noble F, Rajewsky N. Circular RNAs are a large class of animal RNAs with regulatory potency. Nature. 2013;495(7441):333–338. doi: 10.1038/nature11928. [DOI] [PubMed] [Google Scholar]
- Mendoza-Almanza et al. (2019).Mendoza-Almanza G, Ortíz-Sánchez E, Rocha-Zavaleta L, Rivas-Santiago C, Esparza-Ibarra E, Olmos J. Cervical cancer stem cells and other leading factors associated with cervical cancer development. Oncology Letters. 2019;18:3423–3432. doi: 10.3892/ol.2019.10718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanty, Huang & Basu (2005).Mohanty S, Huang J, Basu A. Enhancement of cisplatin sensitivity of cisplatin-resistant human cervical carcinoma cells by bryostatin 1. Clinical Cancer Research. 2005;11(18):6730–6737. doi: 10.1158/1078-0432.CCR-05-0450. [DOI] [PubMed] [Google Scholar]
- Moore (2008).Moore DH. Chemotherapy for advanced, recurrent, and metastatic cervical cancer. Journal of the National Comprehensive Cancer Network. 2008;6(1):53–57. doi: 10.6004/jnccn.2008.0006. [DOI] [PubMed] [Google Scholar]
- Moore et al. (2010).Moore DH, Tian C, Monk BJ, Long HJ, Omura GA, Bloss JD. Prognostic factors for response to cisplatin-based chemotherapy in advanced cervical carcinoma: a gynecologic oncology group study. Gynecologic Oncology. 2010;116(1):44–49. doi: 10.1016/j.ygyno.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassar & Blanpain (2016).Nassar D, Blanpain C. Cancer stem cells: basic concepts and therapeutic implications. Annual Review of Pathology. 2016;11(1):47–76. doi: 10.1146/annurev-pathol-012615-044438. [DOI] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network (2020).National Comprehensive Cancer Network NCCN Clinical Practice Guidelines in Oncology, Cervical Cancer. Version 1https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf 2020
- Peng & Calin (2018).Peng Y, Calin GA. Crucial role of non-coding RNAs in disease. Cancer Letters. 2018;420:127–128. doi: 10.1016/j.canlet.2018.02.001. [DOI] [PubMed] [Google Scholar]
- Pfaendler & Tewari (2016).Pfaendler KS, Tewari KS. Changing paradigms in the systemic treatment of advanced cervical cancer. American Journal of Obstetrics and Gynecology. 2016;214(1):22–30. doi: 10.1016/j.ajog.2015.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ping et al. (2018).Ping G, Xiong W, Zhang L, Li Y, Zhang Y, Zhao Y. Silencing long noncoding RNA PVT1 inhibits tumorigenesis and cisplatin resistance of colorectal cancer. American Journal of Translational Research. 2018;10:138–149. [PMC free article] [PubMed] [Google Scholar]
- Prasad et al. (2017).Prasad CB, Prasad SB, Yadav SS, Pandey LK, Singh S, Pradhan S, Narayan G. Olaparib modulates DNA repair efficiency, sensitizes cervical cancer cells to cisplatin and exhibits anti-metastatic property. Scientific Reports. 2017;7(1):12876. doi: 10.1038/s41598-017-13232-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raji et al. (2017).Raji GR, Sruthi TV, Edatt L, Haritha K, Sharath Shankar S, Sameer Kumar VB. Horizontal transfer of miR-106a/b from cisplatin resistant hepatocarcinoma cells can alter the sensitivity of cervical cancer cells to cisplatin. Cellular Signalling. 2017;38:146–158. doi: 10.1016/j.cellsig.2017.07.005. [DOI] [PubMed] [Google Scholar]
- Sannigrahi et al. (2017).Sannigrahi MK, Sharma R, Singh V, Panda NK, Rattan V, Khullar M. Role of Host miRNA Hsa-miR-139-3p in HPV-16-Induced Carcinomas. Clinical Cancer Research. 2017;23(14):3884–3895. doi: 10.1158/1078-0432.CCR-16-2936. [DOI] [PubMed] [Google Scholar]
- Sathyanarayanan, Chandrasekaran & Karunagaran (2017).Sathyanarayanan A, Chandrasekaran KS, Karunagaran D. microRNA-145 modulates epithelial-mesenchymal transition and suppresses proliferation, migration and invasion by targeting SIP1 in human cervical cancer cells. Cellular Oncology. 2017;40(2):119–131. doi: 10.1007/s13402-016-0307-3. [DOI] [PubMed] [Google Scholar]
- Sharma, Dua & Agarwal (2014).Sharma G, Dua P, Agarwal SM. A comprehensive review of dysregulated miRNAs involved in cervical cancer. Current Genomics. 2014;15(4):310–323. doi: 10.2174/1389202915666140528003249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen et al. (2012).Shen DW, Pouliot LM, Hall MD, Gottesman MM. Cisplatin resistance: a cellular self-defense mechanism resulting from multiple epigenetic and genetic changes. Pharmacological Reviews. 2012;64(3):706–721. doi: 10.1124/pr.111.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi et al. (2019).Shi F, Su J, Liu Z, Wang J, Wang T. miR-144 reverses cisplatin resistance in cervical cancer via targeting LHX2. Journal of Cellular Biochemistry. 2019;120(9):15018–15026. doi: 10.1002/jcb.28763. [DOI] [PubMed] [Google Scholar]
- Shih et al. (2019).Shih J-H, Chen H-Y, Lin S-C, Yeh Y-C, Shen R, Lang Y-D, Wu D-C, Chen C-Y, Chen R-H, Chou T-Y, Jou Y-S. Integrative analyses of noncoding RNAs reveal the potential mechanisms augmenting tumor malignancy in lung adenocarcinoma. Nucleic Acids Research. 2019;48(3):1175–1191. doi: 10.1093/nar/gkz1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small et al. (2017).Small W, Bacon MA, Bajaj A, Chuang LT, Fisher BJ, Harkenrider MM, Jhingran A, Kitchener HC, Mileshkin LR, Viswanathan AN, Gaffney DK. Cervical cancer: a global health crisis. Cancer. 2017;123(13):2404–2412. doi: 10.1002/cncr.30667. [DOI] [PubMed] [Google Scholar]
- Song & Li (2017).Song J, Li Y. miR-25-3p reverses epithelial-mesenchymal transition via targeting Sema4C in cisplatin-resistance cervical cancer cells. Cancer Science. 2017;108(1):23–31. doi: 10.1111/cas.13104. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Sun et al. (2019).Sun Y, Feng Y, Zhang G, Xu Y. The endonuclease APE1 processes miR-92b formation, thereby regulating expression of the tumor suppressor LDLR in cervical cancer cells. Therapeutic Advances in Medical Oncology. 2019;11:1758835919855859. doi: 10.1177/1758835919855859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svrcek et al. (2013).Svrcek M, El-Murr N, Wanherdrick K, Dumont S, Beaugerie L, Cosnes J, Colombel JF, Tiret E, Fléjou JF, Lesuffleur T, Duval A. Overexpression of microRNAs-155 and 21 targeting mismatch repair proteins in inflammatory bowel diseases. Carcinogenesis. 2013;34(4):828–834. doi: 10.1093/carcin/bgs408. [DOI] [PubMed] [Google Scholar]
- Tang et al. (2019).Tang Q, Chen Z, Zhao L, Xu H. Circular RNA hsa_circ_0000515 acts as a miR-326 sponge to promote cervical cancer progression through up-regulation of ELK1. Aging. 2019;11(22):9982–9999. doi: 10.18632/aging.102356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong et al. (2019).Tong R, Zhang J, Wang C, Li Q, Wang L, Ju M. Inhibition of miR-574-5p suppresses cell growth and metastasis and enhances chemosensitivity by targeting RNA binding protein QKI in cervical cancer cells. Naunyn-Schmiedeberg’s Archives of Pharmacology. 2019;118(10):3028. doi: 10.1007/s00210-019-01772-6. [DOI] [PubMed] [Google Scholar]
- Vella et al. (2015).Vella S, Penna I, Longo L, Pioggia G, Garbati P, Florio T, Rossi F, Pagano A. Perhexiline maleate enhances antitumor efficacy of cisplatin in neuroblastoma by inducing over-expression of NDM29 ncRNA. Scientific Reports. 2015;5(1):18144. doi: 10.1038/srep18144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waggoner (2003).Waggoner SE. Cervical cancer. Lancet. 2003;361(9376):2217–2225. doi: 10.1016/S0140-6736(03)13778-6. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2017a).Wang B, Huang Z, Gao R, Zeng Z, Yang W, Sun Y, Wei W, Wu Z, Yu L, Li Q, Zhang S, Li F, Liu G, Liu B, Leng L, Zhan W, Yu Y, Yang G, Zhou S. Expression of long noncoding RNA urothelial cancer associated 1 promotes cisplatin resistance in cervical cancer. Cancer Biotherapy and Radiopharmaceuticals. 2017a;32:101–110. doi: 10.1089/cbr.2016.2156. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2013).Wang F, Liu M, Li X, Tang H. MiR-214 reduces cell survival and enhances cisplatin-induced cytotoxicity via down-regulation of Bcl2l2 in cervical cancer cells. FEBS Letters. 2013;587(5):488–495. doi: 10.1016/j.febslet.2013.01.016. [DOI] [PubMed] [Google Scholar]
- Wang & Liang (2020).Wang L, Liang TT. CD59 receptor targeted delivery of miRNA-1284 and cisplatin-loaded liposomes for effective therapeutic efficacy against cervical cancer cells. AMB Express. 2020;10(1):54. doi: 10.1186/s13568-020-00990-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2018).Wang N, Hou MS, Zhan Y, Shen XB, Xue HY. MALAT1 promotes cisplatin resistance in cervical cancer by activating the PI3K/AKT pathway. European Review for Medical and Pharmacological Sciences. 2018;22:7653–7659. doi: 10.26355/eurrev_201811_16382. [DOI] [PubMed] [Google Scholar]
- Wang, Feng & Zhang (2020).Wang T, Feng J, Zhang A. miR-584 inhibits cell proliferation, migration and invasion in vitro and enhances the sensitivity to cisplatin in human cervical cancer by negatively targeting GLI1. Experimental and Therapeutic Medicine. 2020;19:2059–2066. doi: 10.3892/etm.2020.8449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2019).Wang W-T, Han C, Sun Y-M, Chen T-Q, Chen Y-Q. Noncoding RNAs in cancer therapy resistance and targeted drug development. Journal of Hematology & Oncology. 2019;12(1):55. doi: 10.1186/s13045-019-0748-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2017b).Wang W, Li Y, Liu N, Gao Y, Li L. MiR-23b controls ALDH1A1 expression in cervical cancer stem cells. BMC Cancer. 2017b;17(1):292. doi: 10.1186/s12885-017-3192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei et al. (2019).Wei X, Zhou Y, Qiu J, Wang X, Xia Y, Sui L. Low expression of TUG1 promotes cisplatin sensitivity in cervical cancer by activating the MAPK pathway. Journal of Buon. 2019;24:1020–1026. [PubMed] [Google Scholar]
- Wen et al. (2017).Wen Q, Liu Y, Lyu H, Xu X, Wu Q, Liu N, Yin Q, Li J, Sheng X. Long noncoding RNA GAS5, which acts as a tumor suppressor via microRNA 21, regulates cisplatin resistance expression in cervical cancer. International Journal of Gynecological Cancer. 2017;27(6):1096–1108. doi: 10.1097/IGC.0000000000001028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen et al. (2014).Wen Z, Lei Z, Jin-An M, Xue-Zhen L, Xing-Nan Z, Xiu-Wen D. The inhibitory role of miR-214 in cervical cancer cells through directly targeting mitochondrial transcription factor A (TFAM) European Journal of Gynaecological Oncology. 2014;35:676–682. [PubMed] [Google Scholar]
- Wilusz, Sunwoo & Spector (2009).Wilusz JE, Sunwoo H, Spector DL. Long noncoding RNAs: functional surprises from the RNA world. Genes & Development. 2009;23(13):1494–1504. doi: 10.1101/gad.1800909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong et al. (2017).Xiong Y, Sun F, Dong P, Watari H, Yue J, Yu MF, Lan CY, Wang Y, Ma ZB. iASPP induces EMT and cisplatin resistance in human cervical cancer through miR-20a-FBXL5/BTG3 signaling. Journal of Experimental & Clinical Cancer Research. 2017;36(1):48. doi: 10.1186/s13046-017-0520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu et al. (2017).Xu D, Liu S, Zhang L, Song L. MiR-211 inhibits invasion and epithelial-to-mesenchymal transition (EMT) of cervical cancer cells via targeting MUC4. Biochemical and Biophysical Research Communications. 2017;485(2):556–562. doi: 10.1016/j.bbrc.2016.12.020. [DOI] [PubMed] [Google Scholar]
- Yamamura et al. (2018).Yamamura S, Imai-Sumida M, Tanaka Y, Dahiya R. Interaction and cross-talk between non-coding RNAs. Cellular and Molecular Life Sciences. 2018;75(3):467–484. doi: 10.1007/s00018-017-2626-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2018).Yang F, Guo L, Cao Y, Li S, Li J, Liu M. MicroRNA-7-5p promotes cisplatin resistance of cervical cancer cells and modulation of cellular energy homeostasis by regulating the expression of the PARP-1 and BCL2 genes. Medical Science Monitor. 2018;24:6506–6516. doi: 10.12659/MSM.910969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2016a).Yang H, Wu XL, Wu KH, Zhang R, Ju LL, Ji Y, Zhang YW, Xue SL, Zhang YX, Yang YF, Yu MM. MicroRNA-497 regulates cisplatin chemosensitivity of cervical cancer by targeting transketolase. American Journal of Cancer Research. 2016a;6:2690–2699. [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2016b).Yang J, Zhang K, Wu J, Shi J, Xue J, Li J, Chen J, Zhu Y, Wei J, He J, Liu X. Wnt5a increases properties of lung cancer stem cells and resistance to cisplatin through activation of Wnt5a/PKC signaling pathway. Stem Cells International. 2016b;2016:1690896. doi: 10.1155/2016/1690896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2015a).Yang Y-K, Xi W-Y, Xi R-X, Li J-Y, Li Q, Gao Y-E. MicroRNA-494 promotes cervical cancer proliferation through the regulation of PTEN. Oncology Reports. 2015a;33(5):2393–2401. doi: 10.3892/or.2015.3821. [DOI] [PubMed] [Google Scholar]
- Yang et al. (2016c).Yang Y, Dai C, Cai Z, Hou A, Cheng D, Wu G, Li J, Cui J, Xu D. The pathway analysis of micrornas regulated drug-resistant responses in HeLa cells. IEEE Transactions on NanoBioscience. 2016c;15(2):113–118. doi: 10.1109/TNB.2016.2539365. [DOI] [PubMed] [Google Scholar]
- Yang et al. (2015b).Yang Y, Liu H, Wang X, Chen L. Up-regulation of microRNA-664 inhibits cell growth and increases cisplatin sensitivity in cervical cancer. International Journal of Clinical and Experimental Medicine. 2015b;8:18123–18129. [PMC free article] [PubMed] [Google Scholar]
- Yang et al. (2006).Yang Z, Schumaker LM, Egorin MJ, Zuhowski EG, Guo Z, Cullen KJ. Cisplatin preferentially binds mitochondrial DNA and voltage-dependent anion channel protein in the mitochondrial membrane of head and neck squamous cell carcinoma: possible role in apoptosis. Clinical Cancer Research. 2006;12(19):5817–5825. doi: 10.1158/1078-0432.CCR-06-1037. [DOI] [PubMed] [Google Scholar]
- Yao et al. (2019).Yao T, Lu R, Zhang J, Fang X, Fan L, Huang C, Lin R, Lin Z. Growth arrest-specific 5 attenuates cisplatin-induced apoptosis in cervical cancer by regulating STAT3 signaling via miR-21. Journal of Cellular Physiology. 2019;234(6):9605–9615. doi: 10.1002/jcp.27647. [DOI] [PubMed] [Google Scholar]
- Yin & Ren (2019).Yin Z, Ren W. MicroRNA-217 acts as a tumor suppressor and correlates with the chemoresistance of cervical carcinoma to cisplatin. OncoTargets and Therapy. 2019;12:759–771. doi: 10.2147/ott.S176618. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Yoon, Abdelmohsen & Gorospe (2014).Yoon JH, Abdelmohsen K, Gorospe M. Functional interactions among microRNAs and long noncoding RNAs. Seminars in Cell & Developmental Biology. 2014;34:9–14. doi: 10.1016/j.semcdb.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu et al. (2019).Yu M, Xu B, Yang H, Xue S, Zhang R, Zhang H, Ying X, Dai Z. MicroRNA-218 regulates the chemo-sensitivity of cervical cancer cells through targeting survivin. Cancer Management and Research. 2019;11:6511–6519. doi: 10.2147/cmar.S199659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan et al. (2020).Yuan M, Zhao S, Chen R, Wang G, Bie Y, Wu Q, Cheng J. MicroRNA-138 inhibits tumor growth and enhances chemosensitivity in human cervical cancer by targeting H2AX. Experimental and Therapeutic Medicine. 2020;19:630–638. doi: 10.3892/etm.2019.8238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2018a).Zhang J, Li YH, Liu HL, Zhang Y, Zhang QS, Li SZ. Correlations of MicroRNA-21 gene polymorphisms with chemosensitivity and prognosis of cervical cancer. American Journal of the Medical Sciences. 2018a;356(6):544–551. doi: 10.1016/j.amjms.2018.08.014. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2018b).Zhang J, Zhao X, Zhang J, Zheng X, Li F. Circular RNA hsa_circ_0023404 exerts an oncogenic role in cervical cancer through regulating miR-136/TFCP2/YAP pathway. Biochemical and Biophysical Research Communications. 2018b;501(2):428–433. doi: 10.1016/j.bbrc.2018.05.006. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2016).Zhang L, Li J, Zong L, Chen X, Chen K, Jiang Z, Nan L, Li X, Li W, Shan T, Ma Q, Ma Z. Reactive oxygen species and targeted therapy for pancreatic cancer. Oxidative Medicine and Cellular Longevity. 2016;2016:1616781. doi: 10.1155/2016/1616781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2019).Zhang WY, Liu YJ, He Y, Chen P. Suppression of long noncoding RNA NCK1-AS1 increases chemosensitivity to cisplatin in cervical cancer. Journal of Cellular Physiology. 2019;234(4):4302–4313. doi: 10.1002/jcp.27198. [DOI] [PubMed] [Google Scholar]
- Zhong et al. (2018).Zhong Y, Du Y, Yang X, Mo Y, Fan C, Xiong F, Ren D, Ye X, Li C, Wang Y, Wei F, Guo C, Wu X, Li X, Li Y, Li G, Zeng Z, Xiong W. Circular RNAs function as ceRNAs to regulate and control human cancer progression. Molecular Cancer. 2018;17(1):79. doi: 10.1186/s12943-018-0827-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu et al. (2018).Zhu H, Zheng T, Yu J, Zhou L, Wang L. LncRNA XIST accelerates cervical cancer progression via upregulating Fus through competitively binding with miR-200a. Biomedicine & Pharmacotherapy. 2018;105:789–797. doi: 10.1016/j.biopha.2018.05.053. [DOI] [PubMed] [Google Scholar]
- Zisowsky et al. (2007).Zisowsky J, Koegel S, Leyers S, Devarakonda K, Kassack MU, Osmak M, Jaehde U. Relevance of drug uptake and efflux for cisplatin sensitivity of tumor cells. Biochemical Pharmacology. 2007;73(2):298–307. doi: 10.1016/j.bcp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Zou et al. (2020).Zou X, Zhu C, Zhang L, Zhang Y, Fu F, Chen Y, Zhou J. MicroRNA-708 suppresses cell proliferation and enhances chemosensitivity of cervical cancer cells to cDDP by negatively targeting timeless. OncoTargets and Therapy. 2020;13:225–235. doi: 10.2147/ott.S227015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
This is a literature review, and the research in this article did not generate any data or code.