Abstract
Coal-fired power plants release substantial air pollution, including over 60% of U.S. sulfur dioxide (SO2) emissions in 2014. Such air pollution may exacerbate asthma however direct studies of health impacts linked to power plant air pollution are rare. Here, we take advantage of a natural experiment in Louisville, Kentucky, where one coal-fired power plant retired and converted to natural gas, and three others installed SO2 emission control systems between 2013 and 2016. Dispersion modeling indicated exposure to SO2 emissions from these power plants decreased after the energy transitions. We used several analysis strategies, including difference-in-differences, first-difference, and interrupted time-series modeling to show that the emissions control installations and plant retirements were associated with reduced asthma disease burden related to ZIP code-level hospitalizations and emergency room visits, and individual-level medication use as measured by digital medication sensors.
Coal-fired power plants provide a large amount of electricity worldwide. In 2015, they produced 6 trillion megawatt (MW) hours and 25% of the global supply.1 Simultaneously, coal-fired power plants emit air pollution, including 63% of U.S economy-wide sulfur dioxide (SO2) emissions in 2014,2 as well as nitrogen oxides (NOx), particulate matter (PM2.5 and PM10), mercury, acid gases, polycyclic aromatic hydrocarbons, and volatile organic compounds.3 Such pollutants have been associated with increased asthma symptoms, emergency room visits (ERVs), hospitalizations, and mortality.4-8
Among populations living near coal-fired power plants and fossil fuel refineries, some, though not all,9,10 epidemiologic studies have found a relationship between higher SO2 levels and uncontrolled asthma,11 respiratory symptoms,12-15 and respiratory-related hospitalizations.16 Residential proximity to such facilities alone, without assessed air quality, has also been identified as a risk factor for asthma exacerbation.17-19
Prior scholarship related to asthma and coal-fired power plant exposures often consisted of observational and cross-sectional studies that considered single air pollutants (usually SO2), and either hospitalizations, pulmonary function, or symptoms alone. Studies of symptoms lacked objective measures, usually relying on participant diaries. Some studies have overcome a portion of these limitations; for example, Smargiassi et al. 200916 used a case-crossover design to evaluate the relationship between SO2 concentrations and ERVs and hospitalizations among young children living near a refinery. To build on these prior studies, we incorporate improved exposure and outcome assessment and capitalize on recent abrupt changes in coal-fired power plant emissions.
Between 2000–2015 in the U.S., 49.5 GW of capacity from coal-fired generators retired at 146 coal-fired power plants1,20 and many generating units installed flue-gas desulfurization systems (alternatively, SO2 emission “controls”) to comply with regulations from the U.S. Environmental Protection Agency (USEPA) and individual states, including the Acid Rain Program, the Clean Air Interstate Rule, and Mercury and Air Toxics Standards.2 The discrete nature of these energy transitions and the ensuing abrupt changes in emissions present circumstances for a “natural experiment” to study related changes in health in the timeframe and population exposed to emissions from the coal-fired power plants.21,22 The key feature is that the transition-induced change in exposure occurs for reasons unrelated to a health investigation and produce exposure changes that more closely resemble an experiment than a typical observational study. Such a natural experiment supports the study of the influence of coal-fired power plant emissions on asthma outcomes more directly, without relying on exposure-response functions estimated with different populations across time and space with varying levels of pollution exposure.23 Previous studies framed in this manner have used a steel mill closure,24 ban on coal sales,25 the Olympic Games,26,27 and the Nitrogen Oxides Budget Program28 to study the relationship between air pollution and respiratory-related medication expenditures, hospitalizations, and death.
We use retirements and SO2 emissions control installations at four coal-fired power plant facilities near Louisville, KY, USA between 2013–2016 to frame a natural experiment, which generated abrupt changes in air pollution exposures that varied in extent across the Louisville area. The circumstances of these energy transitions and their resemblance to an experiment that (approximately) randomizes exposure changes motivates a variety of analysis approaches that each mitigate some of the common threats to observational studies. Our approaches include comparing asthma-related endpoints in areas more and less exposed to changes in air pollution and individuals before and after the discrete transition events to evaluate impacts on asthma-related endpoints. Kentucky has historically ranked among the top-five in the U.S. for SO2, NO2, and PM10 emissions from power generation.29 We confirmed air quality improvements after the power plant energy transitions using a longitudinal coal-fired power plant emission exposure model.30 Analyses leveraging different elements of spatial and temporal variability in exposure demonstrated that the coal-fired power plant energy transitions were associated with reductions in asthma-related hospitalizations and ERVs at the ZIP code-level and asthma symptoms measured at the individual-level using digital medication sensors within the Louisville metropolitan area.
Impact of retirement, retrofit, and conversion on emissions
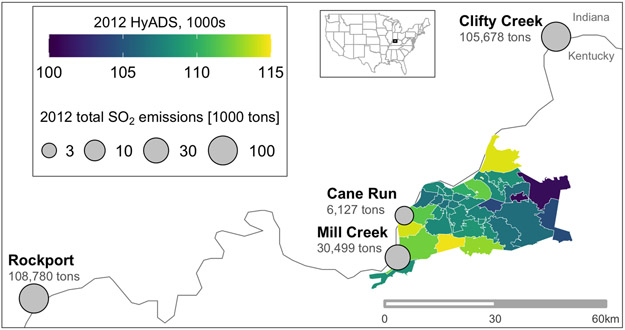
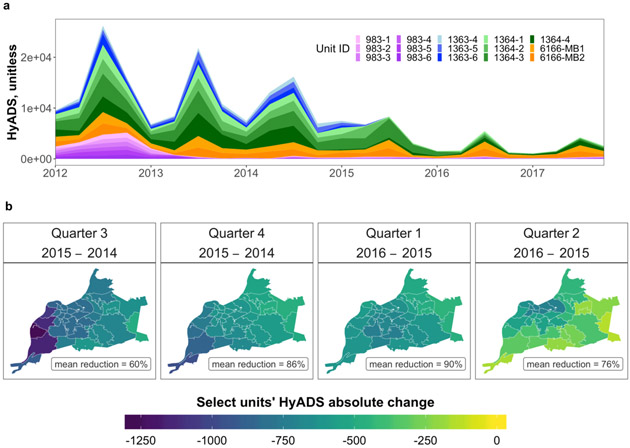
Four coal-fired power plants–Cane Run, Clifty Creek, Mill Creek, and Rockport–with emissions that impacted air quality in Jefferson County, Kentucky either retired or installed SO2 controls between 2012–2016 (Figure 1). We quantified monthly ZIP code variability in SO2 emissions exposure from these plants using the HYSPLIT Average Dispersion (HyADS) model, which aggregates results from 146,000 HYSPLIT runs per power plant.30 During the study period, the quarterly median unitless HyADS exposure was 6553 (IQR: 2283, 9702; maximum 31781). Power plant energy transitions resulted in declining levels over time (Figure 2 and Supplementary Figure 1 and 2). Data from the Louisville Metro Air Pollution Control District confirmed that retirements at Cane Run and scrubbers at Mill Creek reduced annual SO2 emissions by 10,572 tons and 14,208 tons, respectively (Supplementary Figure 3). Comparing years pre/post control installations, SO2 emissions also declined at Clifty Creek (−90%) and Rockport (−%50). These four facilities contributed 36%, 30%, and 16% of total average ZIP code HyADS exposure in Louisville in 2012, 2014, and 2016, respectively. The transitions at the four facilities contributed to overall declining coal-fired power plant emissions exposures in Jefferson County.
Figure 1:
Power plant locations, emissions, and exposure. The locations of the four coal-fired power plant facilities, total SO2 emissions (larger graduated grey circles indicate higher emissions), and HyADS exposures at the ZIP code level within Jefferson County, KY, USA in 2012. Unit and facility data downloaded from the U.S. Environmental Protection Agency Air Markets Program.50
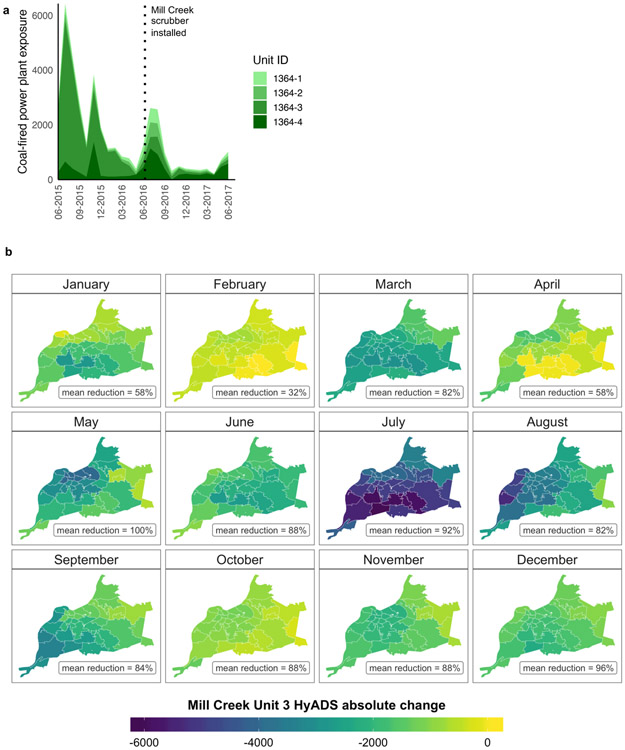
Figure 2:
Quarterly mean ZIP code-level HyADS exposure in Jefferson County, Kentucky, USA. a. From 2012–2017 stratified by coal-fired power plant unit. 983 = Clifty Creek; 1363 = Cane Run; 1364 = Mill Creek; 6166 = Rockport. b. Absolute change in quarterly ZIP code-level HyADS and mean percent reduction across the two stated years in the stated quarter.
HyADS emissions exposures peaked annually during the third quarter (April–June, Figure 2). In a companion analysis, we found that meteorological variability contributed more than emissions reductions to changing HyADS in 2012, 2013, and 2014.31 Table 1 shows that, accounting for seasonality and meteorological factors, the average level of HyADS exposure decreased substantially after three of the four energy transitions, with a 55% decline from baseline after the second quarter 2015 (Q2-2015)
Table 1: Association between coal-fired power plant events and ZIP code-level HyADS emissions exposures in the 35 Jefferson County ZIP codes with population greater than 5.
Percent change was calculated Estimates provided from an ordinary least squares linear regression model adjusted for quarterly mean temperature, wind speed, relative humidity, and atmospheric pressure, and quarter and ZIP code. Included Liang and Zeger cluster-robust standard errors.
| Coal-fired power plant transition date |
% Δ HyADS (95% CI)a,b |
|---|---|
| Q2-2013 | 11 (6, 16) |
| Q4-2014 | −27 (−31, −23) |
| Q2-2015 | −55 (−61, −47) |
| Q2-2016 | −29 (−33, −24) |
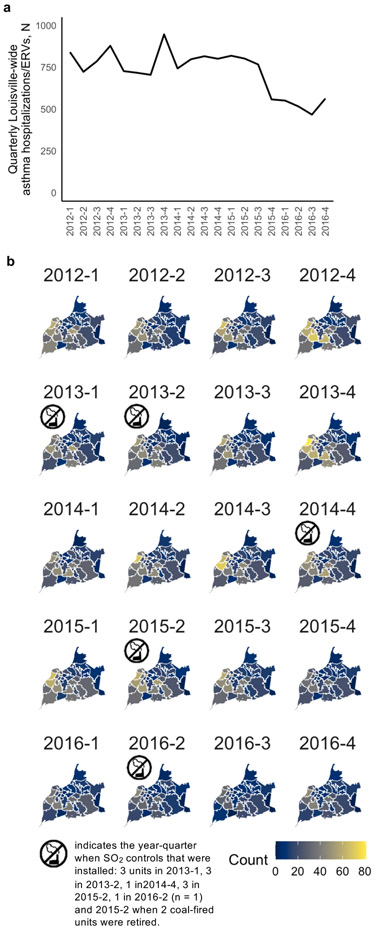
Observed changes in ZIP code-level asthma outcomes
The median (IQR) quarterly asthma hospitalizations/ERV counts across the 35 ZIP codes in Jefferson County between 2012–2016 was 16 (9-31), and counts declined county-wide over time (Figure 3, Supplementary Table 1). Between 2012–2016 rates of uninsured and unemployed individuals also fell. Quarter 4 typically exhibited hospitalization/ERV values higher than other quarters after adjusting for ZIP code and annual specific means.
Figure 3:
Quarterly ZIP code-level counts of asthma hospitalizations/ERVs in Jefferson County, Kentucky, USA. a. County-wide from 2012–2016. b. By ZIP code from 2012–2016. Dates are presented year-quarter. Data provided by the Louisville Metro Department of Public Health and Wellness.
Three of the four energy transitions were associated with reductions in ZIP code-level asthma hospitalizations/ERVs (Table 2), which corresponded to the three transitions associated with reduced HyADS (Table 1). The largest reduction in risk came after the Q2-2015 transitions, rate ratio (RR) = 0.81, 95% CI: 0.70, 0.92. We therefore focused the next stage of analysis on the Q-2015 transitions at Cane Run, Mill Creek, and Rockport. From Q2-2014 to Q2-2016 the average quarterly ZIP code HyADS reduction was 25,281 (SD = 3,638).
Table 2: Estimates of relative risk of a ZIP code-level asthma hospitalization/ERV related to each coal-fired power plant event in the 35 Jefferson ZIP codes with population greater than 5.
Estimates provided from a quasi-Poisson regression model with a ZIP code-level annual population offset and adjusted for annual percent non-Hispanic Black individuals, unemployed individuals, and individuals living below the federal poverty threshold, quarterly mean temperature, wind speed, relative humidity, and atmospheric pressure, and year, quarter, and ZIP code. Includes Liang and Zeger cluster-robust standard errors.
| Coal-fired power plant transition date |
RR (95% CI)a |
|---|---|
| Q2-2013 | 1.08 (0.96, 1.19) |
| Q4-2014 | 0.90 (0.75, 1.06) |
| Q2-2015 | 0.81 (0.70, 0.92) |
| Q2-2016 | 0.91 (0.80, 1.03) |
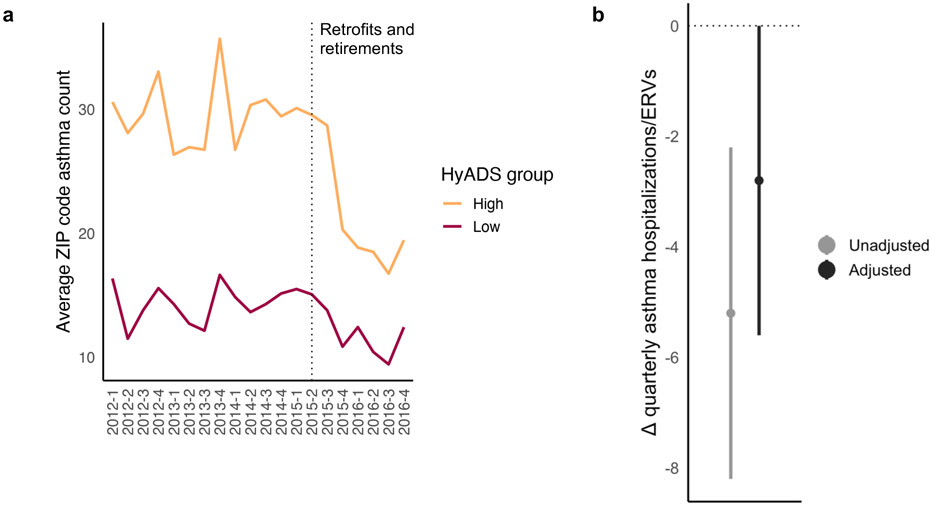
In a difference-in-differences framework, we categorized ZIP codes based on their pre-period HyADS exposure (high vs. low). Results indicated that the Q2-2015 energy transition reduced asthma hospitalizations/ERVs by an additional 2.8 visits per ZIP code per quarter in areas with high pre-transition exposure relative to areas with lower pre-period exposure (Figure 4). When we specified pre-period HyADS as a continuous variable, results were similar when converted to a comparable scale (−0.4 [95% CI: −0.2 −0.7] asthma hospitalizations/ERVs per ZIP code per 1000-unit higher pre-period HyADS exposure, Supplementary Figure 4).
Figure 4:
Spring 2015 coal-fired power plant events and counts of ZIP code-level asthma hospitalization/ERVs. a. Trends in count of ZIP code-level asthma hospitalization/ERVs from Q1-2012 to Q4-2016. The dashed line notes Q2-2015, where the transition took place late in the quarter. Prior to Q2-2015, trends in ZIP code-level counts of asthma events appear parallel, providing evidence that we meet the parallel trends assumption of difference-in-differences analysis. b. Difference-in-differences results with 95% CI from an OLS model (Equation [3]) with a binary specification of pre-period HyADS (high [≥ 32,500] vs. low [< 32,500]. The model was adjusted for annual total population, percent non-Hispanic Black individuals, unemployed individuals, and individuals living below the federal poverty threshold, quarterly mean temperature, wind speed, relative humidity, and atmospheric pressure, and included fixed effects for year, quarter, and ZIP code. Liang and Zeger cluster-robust standard errors were used.
With a first-difference linear regression model, we found that a 1000-unit ZIP-code level reduction in HyADS exposure from the year prior to the year after the Q2-2015 energy transitions resulted in, on average, 2.2 fewer asthma hospitalizations/ERVs (95% CI: −4.5, 0.2) per ZIP code per year and a first-difference model specifying categories of ΔHyADS showed the largest effect for the highest ΔHyADS category (Supplementary Figure 4). Inferences remained stable in sensitivity analyses using baseline population weights instead of adjusting models for baseline population (Supplementary Table 2).
Observed changes in individual-level asthma symptoms
We identified 207 study participants in the AIR Louisville program who were under observation during the year prior and the year after the June 8, 2016 Mill Creek power plant scrubber installation. Most participants were female (67%), of White race/ethnicity (63%), and middle-aged (average age = 45 years) (Supplementary Table 3). Participants’ median monthly HyADS exposure was 1915 (IQR: 1172, 3050) (Supplementary Figure 5). Participants had a daily mean of 1 SABA use (SD = 1.5) and a median of 0 SABA uses (IQR = 0, 1). From visual inspection, daily rescue inhaler use was more prevalent and variable earlier in the study period, likely driven by the smaller number of enrolled participants (Supplementary Figure 6) and later trended downward (Supplementary Figure 7).
In a within-person conditional quasi-Poisson model, we observed reduced monthly average daily SABA use associated with reduced monthly HyADS exposure (RR = 0.94, 95% CI: 0.89, 0.98, for each 1000-unit decrease in HyADS).
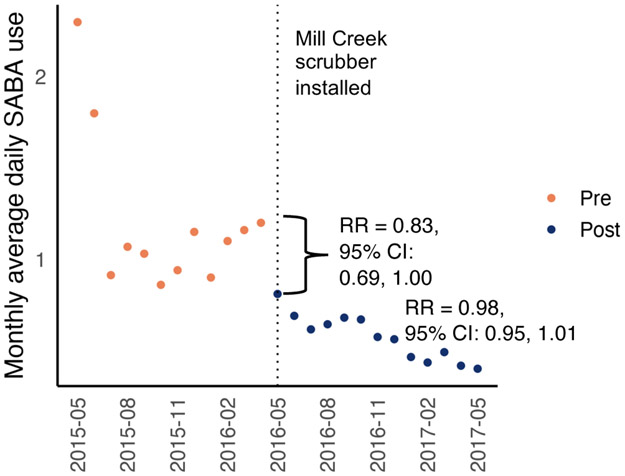
Because the June 2016 Mill Creek scrubber installation resulted in relatively uniform reductions in HyADS exposure across Jefferson county (Figure 5b), we used an interrupted time-series framework. We identified a level shift in SABA use (at the time of scrubber installation) and a possible slope change (decreasing trend in SABA use) (Figure 6). The scrubber installation was associated with a 17% reduction in monthly average daily SABA use (RR = 0.83, 95% CI: 0.69, 1.00) and a 2% reduction (95% CI: −5%, 1%) for each month thereafter.
Figure 5:
Monthly mean ZIP code-level HyADS exposure from Mill Creek power plant in Jefferson County, Kentucky, USA, 2015–2017. a. Stratified by Mill Creek power plant unit. b. Average change in monthly mean ZIP code-level coal-fired power plant air pollution exposure (HyADS) between 2015 and 2016.
Figure 6:
Monthly average daily SABA use before and after the June 2016 Mill Creek SO2 scrubber installation. Orange represents the period prior to the scrubber installation and navy blue after. Points are monthly average daily predicted SABA use from the adjusted model. Relative risks (RR) from a conditional Poisson case interrupted time-series model, which should be interpreted within-individual. Model was adjusted for temperature, humidity, windspeed, ambient pollen (grass, tree, and weed), mold counts, and long-term and seasonal trends. Lagged residuals were used to account for autocorrelation.
In two sensitivity analyses, we evaluated the change in odds of having any daily SABA use (monthly average of ≥1 use/day vs. <1 use/day) and high daily SABA use (monthly average of ≥4 uses/day vs <4 uses/day) at the time of scrubber installation. We found an apparent larger immediate effect on higher monthly average daily SABA use (32% reduction [odds ratio, OR = 0.68, 95% CI: 0.45, 1.02]) and a trend in reduced monthly average daily use of ≥1 uses (17% reduction each month after the scrubber installation [OR = 0.83, 95% CI: 0.71, 0.97]) (Supplementary Table 4).
DISCUSSION
The top four coal-fired power plants in terms of emissions affecting air quality in Louisville, Kentucky in 2012 retired or installed SO2 emission controls between 2012–2016. The resulting air quality improvements translated into reductions in both acute asthma outcomes—measured by quarterly ZIP code-level asthma-related hospitalizations and ERVs—and daily symptoms, as measured by sensor-collected SABA use. In the spring of 2015, coal-fired power plant units retired at Cane Run and SO2 controls were installed at Mill Creek and Rockport. These energy transitions resulted in approximately 3 fewer hospitalizations/ERVs per ZIP code per quarter in the following year, which translates into nearly 400 (−2.8 per ZIP-quarter × 4 quarters × 35 ZIPs) avoided hospitalizations/ERVs in Jefferson County annually. At the individual level, the Mill Creek SO2 scrubber installed in June 2016 was associated with immediate reductions in SABA use and a marginally declining trend in use through May 2017.
Uniquely, this study found coal-fired power plant emissions exposure reductions consistently associated with reduced asthma morbidity at two spatial and temporal resolutions: monthly average daily SABA use within individuals and acute quarterly ERVs and hospitalizations at the ZIP code-level. Acute outcomes like hospitalizations represent an important, yet more infrequent, severe, and costly32 signal of asthma morbidity. SABA use can represent the daily burden of disease and future risk of adverse outcomes.33 Our analyses used digital medication sensors to objectively track the time and location of SABA use and avoids potential recall bias associated with the diaries used in previous studies of short-term air pollution levels and asthma.15,34,35
In 2014, US power plants accounted for 64% of SO2, 14% of NOx, and 7% of PM2.5 economy-wide emissions, with coal power comprising 98% of SO2 and >82% of NOx and PM2.5 power plant emissions.2 Exposure to these air pollutants, even at relatively low levels, have been associated with asthma morbidity.7,8,10,36 Four main mechanisms–oxidative stress; airway remodeling; inflammation or immunological response; and enhanced response to inhaled allergens37–likely explain how air pollution contributes to asthma onset and exacerbation. Laboratory studies of SO2 exposure among asthmatics have demonstrated bronchoconstriction in humans38 and airway inflammatory and immune responses in rats.39
In a 2017 report for the U.S. Department of Energy, Massetti and colleagues characterized SO2 as the main source of air pollution-related economic damage associated with coal-fired power plants due to its high volume of emissions and because SO2 is a PM2.5 precursor.2 Among populations living close to coal-fired power plants, SO2 has been associated with wheeze and asthma prevalence,13,40 asthma attacks, and ERVs,12,15,16 though it is likely that other pollutants play a role. Coal electricity generation contributes to anthropogenic PM2.5 levels (which accounts for 1-3% of all asthma-related ERVs in the Americas41) and NO2 exposures (which may cause 19% of asthma incidence in high-income countries42). Among children living near Israel’s 2580 MW Orot Rabin coal-fired plant, combined NOx and SO2 exposure was more strongly associated with reduced pulmonary function test performance than either pollutant alone.14
Several studies have characterized exposure via residential proximity to coal-fired power plants, a metric which incorporates, albeit crudely, multiple coal-related pollutants.17-19 The continuous and quantitative HyADS metric improves exposure characterization around coal-fired power plants and attempts to isolate the effect of collective coal emissions on health. However, the temporal resolution of our data and the HyADS metric make it difficult to compare our findings, in magnitude, to prior research that reports relationships between coal-fired power plant exposure and increased diary-reported respiratory symptoms12,13,40 and SABA use,15 as well as ERVs and hospitalizations.16,19
Epidemiologists cannot randomize individuals to differing levels of air pollution, which can make causal inference challenging. Quasi-experimental designs23 that leverage the circumstances of natural experiments provide one alternative method, that, when paired with appropriate analytic approaches, can mimic pseudo-randomization of individuals and populations to varying levels of environmental exposures.21,22 Compared to traditional observational studies, quasi-experimental techniques are better equipped to handle unobserved differences in populations that might otherwise confound exposure-outcome associations.43 A few prior studies of asthma exacerbations have used quasi-experimental designs,24,26-28 for example, monitoring changes in asthma-related hospitalizations and acute care visits before, during, and after an Olympic Games that reduced local air pollution.26,27 Environmental exposures tend to follow a social gradient44 and co-occurring factors like high body mass index, smoking, low socioeconomic status, and area-level racial segregation are risk factors for asthma.45 Therefore, an abrupt change in an environmental exposure improves our ability to disentangle social and environmental determinants of health.
To our knowledge, no study has focused on SO2 emission control installations or power plant retirements to assess potential asthma-related health benefits. We examined multiple interventions across several years and tracked intervention impacts at several phases (i.e., intervention, emissions, exposure, health outcome). An important analytic decision in quasi-experimental studies is the choice of control group. Our difference-in-differences analysis compared changes between ZIP codes that were initially most exposed to the power plants generating the transition and the control ZIP codes that were comparatively less subject to exposure from these plants. In our first-difference analysis, we used ZIP codes that experienced less reduction in HyADS exposure during the study period to control for time trends in hospitalizations and ERVs and other factors over the study period thereby minimizing the threat of confounding due to such factors. Both designs control for variation in observed and unobserved fixed characteristics of place.46 At the individual-level we implemented a within-person analysis, which regards each person as his or her own control to reduce the threat of bias associated with confounding variables related to differences across people. This case time-series analysis only controlled for overall linear temporal trends. Individual- and ZIP code-level analyses consistently supported the notion that the energy transitions improved asthma outcomes.
This study had limitations. AIR Louisville cohort participants were enrolled through a number of channels and did not have standardized clinical oversight. We lacked access to individual-level data on participants, (e.g., healthcare utilization, socioeconomic status, smoking or tobacco smoke exposure), though most of these factors are considered time-invariant and controlled for by study design. Time-varying factors, however, both at the individual and area-level could have confounded our results. A prior study found that the digital health intervention (i.e., Propeller inhaler system) may have helped reduce SABA use, with the largest improvements during the first few months.47 If enrollment in the program coincided with plant changes, this could have resulted in overestimated effects. However, our within-person interrupted time-series design suggested an abrupt change in SABA use at the time of a SO2 control installation and continued decline thereafter. We assumed a linear trend in outcome, while changes may have followed a non-linear pattern. Although results in Figure 6 suggested the largest change in SABA use corresponded to the largest drop in HyADS in Q2-2015, we lacked the individual-level data in the pre-period to assess this statistically. At the ZIP code level, due to data limitations, we could not consider asthma-related hospitalizations and ERVs separately, nor could we track multiple events within-individuals. Finally, we were not able to assess cumulative impacts; for example, the relationship between chronic coal-fired power plant-related exposures and asthma prevalence or co-occurrence of asthma and chronic disease. As evidence is mixed regarding the association between long-term air pollution exposure and asthma,10,48 this presents an area for future research.
Our study focused specifically on the impact of four coal-fired power plants but took place against the backdrop of changing emissions at other power plants and reductions in vehicle emissions. We did not explicitly include air pollutants that might affect asthmatics, for example, SO2, PM2.5, NO2, or ozone, but HyADS does represent an index of the mixture of pollutants emitted by power plants. Changes in air quality unrelated to power plants but that trended in time were controlled for in our models. While the HyADS model provided a summary of coal-fired power plant-specific exposure, it did so at the monthly-level, limiting our ability to assess the relationship between short-term exposure fluctuations and SABA use.
In conclusion, this study showed reductions in coal-fired power plant air pollution exposure after retirements and SO2 control installations near Louisville, Kentucky. These reductions appeared to translate into substantially fewer asthma-related ERVs and hospitalizations, as well as fewer average daily SABA uses. Given that 20.4 million adults, or about 9% of the population, suffered from current asthma in 2016,49 the shift in U.S. energy trends away from coal-fired electricity generation may reduce asthma morbidity below otherwise expected levels. Future research should evaluate this potential impact so that plant controls and retirement sites can be phased to affect neighborhoods and schools at highest risk for asthma.
METHODS
The natural experiment
The circumstances supporting the natural experiment arose in Jefferson County, which fully contains Louisville, a city covering 842 km2 and a population of 600,000 people in 2010. We hypothesized that: coal-fired power plant emissions and subsequent population exposures dropped after coal-fired power plant energy transitions; and lower exposures resulting from energy transitions translated into fewer healthcare utilization events and symptoms. Our analyses used two health outcomes (acute asthma-related healthcare utilization and asthma symptoms) at two spatial scales (ZIP code and individual-level) and employed a measure of coal-fired power plant emission exposure.
Exposure to power plant emissions
From the USEPA Air Markets Program,50 we downloaded data on power plant facilities (typically comprising multiple generating units) nationwide with at least one unit using coal as its primary fuel between 2008–2017. These data included power plant latitude and longitude, number of units and fuel type by unit, monthly SO2 emissions, SO2 control type and installation date, and retirement date. We obtained further information on the timing of Jefferson County coal-fired power plant control installations, retirements, and SO2 emissions from the Louisville Metro Air Pollution Control District.
We estimated exposure to power plant emissions over time using the recently-developed HYSPLIT average dispersion (HyADS) model.30 HyADS uses the HYSPLIT air parcel trajectory model51 to quantify the extent to which any power plant influences air quality across U.S. ZIP codes (see Supplementary Note 1 and Henneman et al. 201930 for details). This method produces a unitless measure of emissions influence that is highly correlated with related measured and modeled exposure metrics for coal emissions exposure.30,52 HyADS has previously been applied to estimate U.S.-wide health benefits achieved through reduced coal-fired power plant SO2 emissions.53
We ran HyADS for each of the over 1009 U.S. coal-fired power plant units in operation (located at 478 facilities) nationwide in 2012, 2014, and 2016. In 2012, we ranked each unit’s exposure contribution in each Louisville ZIP code and identified the four facilities that had the highest influence on Louisville ZIP codes (Supplementary Figure 8). These four facilities subsequently underwent retirement or control installations before 2017. We ran HyADS for each facility’s units for years 2012-2017 to estimate the ZIP code-level monthly (used in individual-level analyses) and quarterly (as the average of monthly, used in ZIP code-level analyses) influence of each unit’s emissions on Louisville air quality over time (see Supplementary Data).
Emissions exposures for the four plants of interest
The four highest-ranked facilities by HyADS impact in 2012 included Cane Run, a 943 MW plant located 14 kilometers southwest of downtown Louisville; Clifty Creek, a 1303 MW plant located about 75 kilometers northeast of Louisville that had the greatest impact of any coal-fired power plant in the country on east Jefferson County; Mill Creek, a 1717 MW plant located 25 kilometers southwest of downtown Louisville that had the greatest impact of any coal-fired power plant in the country on west Jefferson County; and Rockport, a 2600 MW plant located about 100 kilometers west of Louisville.
Clifty Creek installed wet limestone scrubbers for units 1-3 on March 20, 2013 and for units 4-6 on May 15, 2013. The Mill Creek plant installed wet limestone scrubbers for unit 4 on December 9, 2014, for units 1 and 2 on May 27, 2015, and for unit 3 on June 8, 2016.54 Cane Run retired its three active units in May 2015, after which a 650 MW natural gas combined cycle plant began operating at the site. Rockport installed dry sodium scrubbers on its 2 coal units in April 2015.
Area-level confounders of asthma symptoms
We assembled several indicators of community socioeconomic status and demographic composition at the ZIP code-level from the U.S. American Community Survey (ACS).55 These were variables potentially associated with coal-fired power plant exposure that might also predict asthma hospitalizations56 and included: total population; number of non-Hispanic Black individuals; number of individuals without health insurance coverage; number of individuals 16 years and older that were unemployed; number of individuals 25 years and older without a high school diploma or equivalent; and number of individuals with income in the past 12 months below the federal poverty level. To create a time-varying dataset, we linked multiple 5-year surveys because annual ZIP code-level estimates were not available. For example, we used the 2008-2012 ACS to estimate ZIP code characteristics in 2012 and the 2009-2013 ACS for 2013. Finally, we downloaded ZIP code-level meteorological data on ambient temperature, relative humidity, windspeed, and atmospheric pressure from the USEPA.57
Jefferson County quarterly ZIP code-level asthma data
The Louisville Metro Department of Public Health and Wellness provided quarterly combined counts of asthma-related hospitalizations and ERVs among all ages for the years 2012–2016 for all Louisville ZIP codes, which we restricted to the 35 ZIP codes with non-zero population in 2012. Hospitalizations/ERVs were considered asthma-related if the following International Classification of Diseases 9 (ICD-9) or ICD-10 diagnosis codes were present in the first through third diagnosis positions: 493.XX or J45.X.
Participant recruitment for individual level asthma data
Data for the individual-level analyses came from the AIR Louisville pilot (2012–2014) and full program (2015–2017).47 Eligible participants (n = 1,021 from pilot and full program) were enrolled from 2012–2016 through multiple channels, including employer partner wellness programs, clinics, community events, and social media campaigns. Inclusion criteria consisted of a self-reported diagnosis of asthma, a current prescription for a compatible inhaled medication for asthma, and a home or work address in Jefferson County, Kentucky. Additional details on the study can be found elsewhere.47 Participants all agreed to and signed Propeller Health’s Terms of Service, which stated that their data may be used in an aggregated fashion for public health-oriented analyses. We also received a waiver of consent and exemption (PRH1-17-508) from the Copernicus Group Independent Review Board. The protocol was additionally approved by the UC Berkeley Committee for Protection of Human Subjects.
We included participants in analyses if they had inhaler use data collected in the year before and the year after the coal-fired power plant energy transitions. We focused on the June 8, 2016 SO2 scrubber installation on Mill Creek Unit 3, because this date supported the largest participation cohort for the individual-level analyses (N = 207, 20.3% of the entire AIR Louisville cohort) (Supplementary Figure 9).
Digital Health Platform
All participants received digital sensors (Propeller Health, Madison, WI) to attach to their inhaled short-acting beta agonist (SABA, i.e., “rescue”) medications. The sensor and platform comprised a U.S. Food and Drug Administration-cleared digital health intervention that combined inhaler sensors, mobile apps, web-based dashboards and predictive analytics for patients and clinicians.47,58,59 The sensor objectively monitored the use of inhalers, capturing the date, time of day, and number of actuations, and wirelessly transmitted these data back to secure servers through a smartphone application or hub base station. Actuations occurring within 2 minutes were grouped into a single use event, therefore each use could represent multiple actuations. The sensors regularly transmitted medication use data back to the server (“sync”) through the smartphone or hub, and also transmitted a “heartbeat” signal, which reported sensor battery life, confirmed no actuations had occurred since the last sync and recorded the participant’s GPS location from which we assigned HyADS exposure estimates. Heartbeats occurred approximately every 3 hours.
The majority (98%) of participants entered the cohort in 2015 or 2016 with the mean (SD) duration of follow-up of 602 (321) days from first to last day under observation. We used the monthly-average count of SABA use events per person per day as our outcome of interest.
Individual meteorological data and plant-specific exposures
Over 85% of SABA use events and heartbeats had a recorded location. For those SABA events missing a GPS location (about 6%), we retro-filled location information with the most recent recorded location within 24 hours before or after the index event. If no location was available, we assigned the participant’s home address location. At the time and place of inhaler use or sensor heartbeat, we assigned hourly meteorological data, including temperature, wind speed, atmospheric pressure, and relative humidity from the National Oceanic and Atmospheric Administration for the years 2008–2016.60 These data were averaged first to daily and then to monthly means. A specialty clinic, Family Allergy & Asthma, provided daily counts of grass, weed, and tree pollen, as well as mold spores from their National Allergy Bureau-certified pollen counting station in Louisville. We assigned each SABA use or heartbeat event daily pollen or mold counts based on event date, with events occurring on the same day assigned the same pollen or mold counts. For analyses, we took the monthly mean of pollen or mold count. We assigned monthly HyADS exposures based on the ZIP code where the participant spent the most time that month. We linked a measure of community social vulnerability in 2014 from the U.S Centers for Disease Control and Prevention to each individual’s census tract of residence.61
Statistical analysis
We conducted ZIP code and individual-level analyses to test the hypothesis that coal-fired power plant energy transitions altered air quality and thereby asthma morbidity among populations living nearby. In Supplementary Table 5, we provide a roadmap for all analyses including questions, datasets, analyses, and locations of results. We performed analyses using R Statistical Software version 3.5.1 (R Core Team [2018], Vienna, Austria, https://www.R-project.org/). Individual-level analyses were conducted using the gnm package (https://cran.rproject.org/package=gnm). All tests were two-sided.
ZIP code level HyADS analysis
We first tested whether the energy transitions were associated with reduced HyADS exposures throughout Louisville, KY. To do so, we used linear regression to fit the following equation:
| (1) |
HyADSpqr is the level of HyADS in ZIP code p, quarter q, and year r. Transition1pqr−Transition4pqr are indicator variables equal to 1 if the energy transition has occurred and 0 otherwise. For example, Transition1pqr equals 1 after Q2-2013 and 0 beforehand, Transition2pqr equals 1 after Q4-2014 and 0 beforehand. Pp and Qq are indicator variables for ZIP code and quarter of year. λpqr is a set of quarterly meteorological variables that included temperature, wind speed, relative humidity and atmospheric pressure. Negative values for β1-β4 indicate decreased HyADS associated with the respective energy transition.
ZIP code-level quasi-Poisson asthma analysis
We then used three approaches to estimate the relationship between energy transitions and ZIP code level asthma hospitalizations/ERV counts. The first was a generalized linear model with a quasi-Poisson distribution, which accommodates over-dispersion, and a log link:
| (2) |
where E(Asthmapqr) represents the expected quarterly asthma hospitalization/ERV counts, totpoppr is the estimated ZIP code-level population, Transition1pqr−Transition4pqr are indicator variables equal to 1 if the energy transition has occurred and 0 otherwise. λpqr is a set of quarterly meteorological variables that included temperature, wind speed, relative humidity and atmospheric pressure, and θpr is a set of demographic variables from the ACS that included percent non-Hispanic Black individuals, percent individuals living in poverty, and percent unemployed individuals. Pp, Qq, and Rr are ZIP code, quarter, and year indicator variables that control for factors common to a ZIP code within a quarter or year. We included population as an offset.
ZIP code-level difference-in-differences asthma analysis
A second analysis of the natural experiment posed by the Q2-2015 transitions used a quasi-experimental difference-in-differences design to evaluate how asthma outcomes differentially changed in ZIP codes defined as either “low” or “high” HyADS exposure based on average pre-period (Q2-2014 to Q2-2015) HyADS exposure. The post-period spanned the year after Q2-2015, so the analysis covered the time period surrounding the installation of scrubbers on units 1 and 2 of the Mill Creek plant and both units of the Rockport plant, and the retirement of Cane Run’s three units. Difference-in-differences analysis is commonly used in studies of natural experiments and can effectively eliminate both observed and unobserved confounding variables that do not vary in time.46,62 We categorized ZIP codes as “low” when their pre-period average HyADS was <32,500 (near the median) and “high” when pre-period HyADS was ≥32,500, selecting the cutoff based on the change’s distribution (Supplementary Figure 10). By estimating the change in asthma hospitalization/ERVs from the pre- to the post-period (difference 1) and subtracting off the difference between the exposed and control exposure ZIP codes (difference 2) we estimated the effect of the Q2–2015 energy transitions in Jefferson County. We used the following parametric equation:
| (3) |
where p stands for ZIP code, q for quarter-year, and r for calendar year. Asthmapqr represents the count of asthma hospitalizations/ERVs in ZIP code p during quarter-year q. Hpqr is an indicator variable equal to one for ZIP codes with pre-period HyADS ≥ 32,500 (i.e., exposed). The group of ZIP codes with pre-period HyADS <32,500 served as the control group because these ZIP codes were less exposed in the pre-period and therefore benefitted less from the Q2-2015 energy transitions but experienced similar secular trends as the high HyADS change group. Cpqr is an indicator variable equal to one when the quarter is after Q2-2015. β3 represents the difference-in-differences estimate of interest. λpqr is a set of quarterly meteorological variables that included temperature, wind speed, relative humidity and atmospheric pressure, and θpq is a set of demographic variables from the ACS that included total population, percent non-Hispanic Black individuals, percent individuals living in poverty, and percent unemployed individuals. Pp, Qq, and Rr are indicators of ZIP code, quarter, and year. We also specified a continuous model by comparing ZIP codes with differing levels of pre-period HyADS rather than creating a cut-point. To do so, we replaced the Hpqr indicator variable with the pre-period continuous HyADS level. We opted to include the described set of potential confounding variables in Equation (3) based on a priori hypotheses, causal diagrams,63 and the correlation structure of potential covariates (Supplementary Figure 11). For example, annual unemployment and uninsured status had a Spearman correlation of 0.84, so we included only unemployment in our models to avoid instability in parameter estimation due to multicollinearity. Difference-in-difference analysis relies on the parallel trends assumption, that in the absence of intervention, trends in the outcome in the pre-period would continue.62 We visually inspected trends over time by low and high pre-Q2-2015 HyADS and found no evidence of a violation (Figure 4a).
ZIP code level first-difference analysis
In a secondary analysis, we used a first-difference design,64 to evaluate the relationship between the pre-post change in HyADS and pre-post change in ZIP code-level hospitalization/ERVs (Supplementary Note 2). This model took the form:
| (4) |
where ΔAsthmapr represents the differences between counts of ZIP code-level asthma hospitalization/ERVs in the year prior to Q2-2015 and the year after Q2-2015 and ΔHyADSpr represents the ZIP code-level difference in HyADS exposure to the three facilities with energy transitions from the year prior to Q2-2015 to the year after Q2-2015. We took differences in meteorological and demographic variables (Δλpr and Δθpr) by subtracting the average value between Q2-2014 and Q1-2015 from the average value between Q3-2015 and Q2-2016. This estimator is unbiased when εpr is independent of ΔHyADSpr, Δλpr, and Δθpr. In a separate model, we allowed for non-linearity in the association between ΔHyADSpr and ΔAsthmapr by specifying quintiles of ΔHyADSpr. In both the difference-in-differences and first-difference models, we accounted for correlation within ZIP codes using Liang and Zeger cluster-robust standard errors.65 We also completed a sensitivity analysis, using baseline population weights rather than adjusting equation (3) or (4) for population.
Individual-level case time-series analysis
We used a case time-series analysis that included 207 participants under observation in the year prior and year after the June 2016 Mill Creek scrubber installation. The case time-series design is a within-person analysis that allows for control of individual-level confounders similar to other case-only methods such as case-crossover and self-controlled case-series designs.66,67 Unlike the case-crossover design, the case time-series design does not rely on the assumptions of risk-set sampling.68 It maintains the temporal structure of the time series format, which allows for modelling of trends over time. It can also accommodate count data and account for over-dispersion and autocorrelation in counts within stratum (i.e., the individual). The conditional Poisson model assumes no unmeasured confounding that is not homogeneous within strata. We have adjusted for measured time-varying meteorological variables and seasonal trends. The model also assumes no residual autocorrelation of counts (to this end we adjust for the lagged residuals). We also relax the assumption of the Poisson distribution to allow for overdispersion of counts and assessed the relationship between exposure to coal-fired power plant emissions and monthly average daily SABA use with the following conditional quasi-Poisson model:
| (5) |
assuming a quasi-Poisson distribution to account for overdispersion. Inhaler_useim is the average daily count of SABA uses for individual i in month m (conditional on the total number of SABA uses for individual i), αi is a parameter for individual level effects (see Equation (6) for more detail), T is the number of days elapsed since May 2015, HyADSjm is the total HyADS exposure in participant i’s ZIP code in month m, λim is a vector of meteorological variables including natural cubic splines for temperature, relative humidity, wind speed, atmospheric pressure, and mold counts, and linear terms for ambient pollen concentrations (i.e., weed, tree, grass), and sm, a harmonic term with 2 sine-cosine pairs and a period of 12 months to account for seasonal trends. The model adjusts for autocorrelation by adding the residuals rim-1 for individual i in month m-1, which were estimated as the residuals of a model fitted as in Equation (5) without the residual term and lagged by one month.66,69 The parameters αi are not estimated by the model, but are rather conditioned out, by conditioning on the sum of total number of inhaler uses for each individual i, ∑i Inhaler_useim, resulting in a multinomial model with likelihood:
| (6) |
where j ∈ the subset of months, m, with observations for each participant i. Next, we sought to directly test the relationship between the June 2016 Mill Creek energy transition and SABA use. Unlike the Q2-2015 energy transitions, the June 2016 Mill Creek unit 3 scrubber installation resulted in fairly uniform reductions in exposure to plant emissions across Jefferson County (Figure 4b). This precluded the assembly of a control group based on exposure change analogous to that in the ZIP code-level difference-in-differences analysis. Instead, we implemented an interrupted time-series design, which construes each person’s study time during the pre-installation period as a control for his or her time during the post-installation period. To do so, we modified Equation (5), replacing HyADSim with a single indicator variable–cntrlim–of exposure to the SO2 control installation at Mill Creek in June 2016, which took the value of 1 beginning May 2016 (Mill Creek unit 3 was turned off in May for the June control installation) and 0 otherwise. We also added an interaction between cntrlim and T to estimate trends in changing SABA use over time. A negative coefficient for the cntrlim variable would indicate that the average number rescue inhaler uses decreased after the scrubber installation. Likewise, a negative β on cntrlim*T would indicate a downward linear trend in rescue inhaler use over time after the installation.
To assess the sensitivity of the individual-level analysis, we evaluated the association between the June 2016 Mill Creek event and two different binary specifications of SABA use: any use and high use. We followed a similar model specification as in Equation (5), but used a logistic regression model and substituted for the Inhaler_useim variable an any SABA use variable (monthly average of ≥1 use/day vs. <1 use/day) and a high SABA use variable (monthly average of ≥4 uses/day vs <4 uses/day).
Data availability
The ZIP code-level asthma hospitalization/ERV data are available from the authors following submission of an analysis proposal and written approval granted by the Louisville Metro Public Health and Wellness. The AIR Louisville monthly medication use data are considered Protected Health Information (PHI) under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) in the U.S., and as such may be accessible from the authors for analysis only after specific written authorization of access following HIPAA guidelines and IRB approval. We provide Jefferson County ZIP code-level monthly HyADS estimates on GitHub at https://github.com/joanacasey/ky_asthma_coal.
Code availability
An R package is available on GitHub for running the HyADS model (https://github.com/lhenneman/disperseR). We also provide analysis code on GitHub at https://github.com/joanacasey/ky_asthma_coal.
Supplementary Material
Acknowledgments
We would like to acknowledge the network of local partners that made the AIR Louisville program possible, including the Center for Healthy Air, Water and Soil, Louisville Metro, the Community Foundation of Louisville, and all the AIR Louisville participants. Partners within the Louisville Metro Government include: Mayor Greg Fischer, the Office of Civic Innovation, Louisville Metro Department of Public Health and Wellness, the Office of Sustainability, the Office of Advanced Planning, the Louisville Jefferson County Information Consortium, and Louisville Forward. Specifically, Keith Talley, Michelle King and Rachael Hamilton of the Air Pollution Control District provided critical information and review of this manuscript. We also thank Paul Tarini and Oktawia Wójcik at the Robert Wood Johnson Foundation for helpful guidance throughout the project.
The main funding for the project was provided by the Robert Wood Johnson Foundation. Support was also provided by the Foundation for a Healthy Kentucky, Norton Healthcare Foundation, Owsley Brown Charitable Foundation, the American Lung Association, the National Institute of Environmental Health Sciences (J.A.C., K99/R00 ES027023; A.M.N, K99/R00 ES027511; C.Z., R01 ES026217), and the U.S. Environmental Protection Agency (C.Z., EPA 83587201). The contents of this work are solely the responsibility of the grantee and do not necessarily represent the official views of the USEPA or the Robert Wood Johnson Foundation. Further, the USEPA does not endorse the purchase of any commercial products or services mentioned in the publication.
REFERENCES
- 1.International Energy Agency. IEA Statistics, <http://www.iea.org/statistics/> (2018).
- 2.Massetti E et al. Environmental Quality and the US Power Sector: Air Quality, Water Quality, Land Use and Environmental Justice. Prepared by: Oak Ridge National Laboratory for the U.S. Department of Energy, <https://www.energy.gov/sites/prod/files/2017/01/f34/Environment%20Baseline%20Vol.%202--Environmental%20Quality%20and%20the%20U.S.%20Power%20Sector--Air%20Quality%2C%20Water%20Quality%2C%20Land%20Use%2C%20and%20Environmental%20Justice.pdf> (2017). [Google Scholar]
- 3.American Lung Association. Toxic Air: The Case for Cleaning Up Coal-Fired Power Plants, <http://www.lung.org/assets/documents/healthy-air/toxic-air-report.pdf> (2011).
- 4.Zheng X.-y. et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. Plos One 10, e0138146 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orellano P, Quaranta N, Reynoso J, Balbi B & Vasquez J Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. Plos One 12, e0174050 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams AM, Phaneuf DJ, Barrett MA & Su JG Short-term impact of PM2.5 on contemporaneous asthma medication use: Behavior and the value of pollution reductions. Proc. Natl. Acad. Sci. USA 116, 5246–5253 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Environmental Protection Agency. Integrated Science Assessment for Oxides of Nitrogen-Health Criteria, <http://ofmpub.epa.gov/eims/eimscomm.getfile?p_download_id=526855> (2016).
- 8.U.S. Environmental Protection Agency. Integrated Review Plan for the Primary National Ambient Air Quality Standard for Sulfur Dioxide. EPA-452/R-14-007, <https://www3.epa.gov/ttn/naaqs/standards/so2/data/20141028so2reviewplan.pdf> (2014).
- 9.Ramadour M et al. Prevalence of asthma and rhinitis in relation to long-term exposure to gaseous air pollutants. Allergy 55, 1163–1169 (2000). [DOI] [PubMed] [Google Scholar]
- 10.Guarnieri M & Balmes JR Outdoor air pollution and asthma. Lancet 383, 1581–1592 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deger L et al. Active and uncontrolled asthma among children exposed to air stack emissions of sulphur dioxide from petroleum refineries in Montreal, Quebec: a cross-sectional study. Can. Respir. J 19, 97–102 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charpin D et al. Respiratory symptoms and air pollution changes in children: the Gardanne Coal-Basin Study. Arch. Environ. Health 43, 22–27 (1988). [DOI] [PubMed] [Google Scholar]
- 13.Schenker MB, Speizer FE, Samet JM, Gruhl J & Batterman S Health effects of air pollution due to coal combustion in the Chestnut Ridge Region of Pennsylvania: results of cross-sectional analysis in adults. Arch. Environ. Health 38, 325–330 (1983). [DOI] [PubMed] [Google Scholar]
- 14.Dubnov J et al. Estimating the effect of air pollution from a coal-fired power station on the development of children's pulmonary function. Environ. Res 103, 87–98 (2007). [DOI] [PubMed] [Google Scholar]
- 15.Cohen AA, Bromberg S, Buechley RW, Heiderscheit LT & Shy CM Asthma and air pollution from a coal-fueled power plant. Am. J. Public Health 62, 1181–1188 (1972). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smargiassi A et al. Risk of asthmatic episodes in children exposed to sulfur dioxide stack emissions from a refinery point source in Montreal, Canada. Environ. Health. Perspect 117, 653 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodriguez-Villamizar LA, Rosychuk RJ, Osornio-Vargas A, Villeneuve PJ & Rowe BH Proximity to two main sources of industrial outdoor air pollution and emergency department visits for childhood asthma in Edmonton, Canada. Can. J. Public Health 108, e523–e529 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Middleton N, Kolokotroni O, Lamnisos D, Koutrakis P & Yiallouros PK Prevalence of asthma and respiratory symptoms in 15–17 year-old Greek-Cypriots by proximity of their community of residence to power plants: Cyprus 2006–07. Public Health 128, 288–296 (2014). [DOI] [PubMed] [Google Scholar]
- 19.Liu X, Lessner L & Carpenter DO Association between residential proximity to fuel-fired power plants and hospitalization rate for respiratory diseases. Environ. Health. Perspect 120, 807–810 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Energy Information Administration. Form EIA-860, <https://www.eia.gov/electricity/data/eia860/> (2019).
- 21.Humphreys DK, Panter J, Sahlqvist S, Goodman A & Ogilvie D Changing the environment to improve population health: a framework for considering exposure in natural experimental studies. J. Epidemiol. Community Health 70, 941–946 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rich DQ Accountability studies of air pollution and health effects: lessons learned and recommendations for future natural experiment opportunities. Environ. Int 100, 62–78 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zigler CM & Dominici F Point: clarifying policy evidence with potential-outcomes thinking--beyond exposure-response estimation in air pollution epidemiology. Am. J. Epidemiol 180, 1133–1140 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pope CA 3rd Respiratory disease associated with community air pollution and a steel mill, Utah Valley. Am. J. Public Health 79, 623–628 (1989). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clancy L, Goodman P, Sinclair H & Dockery DW Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet 360, 1210–1214 (2002). [DOI] [PubMed] [Google Scholar]
- 26.Friedman MS, Powell KE, Hutwagner L, Graham LM & Teague WG Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA 285, 897–905 (2001). [DOI] [PubMed] [Google Scholar]
- 27.Li Y, Wang W, Kan H, Xu X & Chen B Air quality and outpatient visits for asthma in adults during the 2008 Summer Olympic Games in Beijing. Sci. Total. Environ 408, 1226–1227 (2010). [DOI] [PubMed] [Google Scholar]
- 28.Deschenes O, Greenstone M & Shapiro JS Defensive investments and the demand for air quality: Evidence from the NOx budget program. Am. Econ. Rev 107, 2958–2989 (2017). [Google Scholar]
- 29.U.S. Environmental Protection Agency. National Emissions Inventory, < https://www.epa.gov/air-emissions-inventories/2011-national-emissions-inventory-nei-data> (2011).
- 30.Henneman LRF, Choirat C, Ivey CE, Cummiskey K & Zigler CM Characterizing population exposure to coal emissions sources in the United States using the HyADS model. Atmos. Environ 203, 271–280 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henneman LRF, Mickley LJ & Zigler CM Air pollution accountability of energy transitions: the relative importance of wind fields and emissions in exposure changes. Environ. Res. Lett 14, 115003 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zein JG et al. Impact of sge and sex on outcomes and hospital cost of acute asthma in the United States, 2011-2012. Plos One 11, e0157301 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel M et al. Metrics of salbutamol use as predictors of future adverse outcomes in asthma. Clin. Exp. Allergy 43, 1144–1151 (2013). [DOI] [PubMed] [Google Scholar]
- 34.Prieto-Parra L et al. Air pollution, PM2.5 composition, source factors, and respiratory symptoms in asthmatic and nonasthmatic children in Santiago, Chile. Environ. Int 101, 190–200 (2017). [DOI] [PubMed] [Google Scholar]
- 35.Schildcrout JS et al. Ambient air pollution and asthma exacerbations in children: an eight-city analysis. Am. J. Epidemiol 164, 505–517 (2006). [DOI] [PubMed] [Google Scholar]
- 36.U.S. Environmental Protection Agency. Federal Registrar. Primary National Ambient Air Quality Standard for Sulfur Dioxide, Final Rule, 40 CFR Parts 50, 53, and 58. , <https://www.govinfo.gov/content/pkg/FR-2010-06-22/pdf/2010-13947.pdf> (2010).
- 37.Gowers AM et al. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology 17, 887–898 (2012). [DOI] [PubMed] [Google Scholar]
- 38.Johns DO & Linn WS A review of controlled human SO2 exposure studies contributing to the US EPA integrated science assessment for sulfur oxides. Inhal. Toxicol 23, 33–43 (2011). [DOI] [PubMed] [Google Scholar]
- 39.Li R et al. Effect of sulfur dioxide on inflammatory and immune regulation in asthmatic rats. Chemosphere 112, 296–304 (2014). [DOI] [PubMed] [Google Scholar]
- 40.Amster ED, Haim M, Dubnov J & Broday DM Contribution of nitrogen oxide and sulfur dioxide exposure from power plant emissions on respiratory symptom and disease prevalence. Envrion. Pollut 186, 20–28 (2014). [DOI] [PubMed] [Google Scholar]
- 41.Anenberg SC et al. Estimates of the global burden of ambient PM 2.5, ozone, and NO2 on asthma incidence and emergency room visits. Environ. Health. Perspect 126, 107004 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Achakulwisut P, Brauer M, Hystad P & Anenberg SC Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: estimates from global datasets. Lancet Planet. Health 3, e166–e178 (2019). [DOI] [PubMed] [Google Scholar]
- 43.Dominici F, Greenstone M & Sunstein CR Science and regulation. Particulate matter matters. Science 344, 257–259 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cushing L, Morello-Frosch R, Wander M & Pastor M The haves, the have-nots, and the health of everyone: the relationship between social inequality and environmental quality. Annu. Rev. Public Health 36, 193–209 (2015). [DOI] [PubMed] [Google Scholar]
- 45.Baltrus P et al. Individual and county level predictors of asthma related emergency department visits among children on Medicaid: a multilevel approach. J. Asthma 54, 53–61 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Craig P, Katikireddi SV, Leyland A & Popham F Natural experiments: An overview of methods, approaches, and contributions to public health intervention research. Annu. Rev. Public Health 38, 39–56 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barrett M et al. AIR Louisville: addressing asthma with technology, crowdsourcing, cross-sector collaboration, and policy. Health Aff. 37, 525–534 (2018). [DOI] [PubMed] [Google Scholar]
- 48.Anderson HR, Favarato G & Atkinson RW Long-term exposure to outdoor air pollution and the prevalence of asthma: meta-analysis of multi-community prevalence studies. Air. Qual. Atmos. Health 6, 57–68 (2013). [Google Scholar]
- 49.U.S. Centers for Disease Control & Prevention. 2016 National Health Interview Survey (NHIS) Data, <https://www.cdc.gov/asthma/nhis/2016/table3-1.htm> (2016). [Google Scholar]
- 50.U.S. Environmental Protection Agency. Air Markets Program Data, <https://ampd.epa.gov/ampd/> (2018).
- 51.Stein A et al. NOAA’s HYSPLIT atmospheric transport and dispersion modeling system. Bull. Am. Meteorol. Soc 96, 2059–2077 (2015). [Google Scholar]
- 52.Henneman LRF, Dedoussi IC, Casey JA, Choirat C & Zigler CM Comparisons of simple and complex methods for quantifying exposure to point source air pollution emissions. Accepted. J. Expo. Sci. Environ. Epidemiol (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Henneman LRF, Choirat C & Zigler CM Accountability assessment of health improvements in the United States associated with reduced coal emissions between 2005 and 2012. Epidemiology 30, 477–485 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Louisville Gas & Electric. Mill Creek Station Wins 2016 Project of the Year Award, <https://lge-ku.com/newsroom/articles/2017/01/09/mill-creek-station-wins-2016-project-year-award> (2017).
- 55.Manson S, Schroeder J, Riper DV & Ruggles S IPUMS National Historical Geographic Information System: Version 13.0 [Database], < 10.18128/D050.V12.0> (2018.). [DOI] [Google Scholar]
- 56.Gottlieb DJ, Beiser AS & O'Connor GT Poverty, race, and medication use are correlates of asthma hospitalization rates: a small area analysis in Boston. Chest 108, 28–35 (1995). [DOI] [PubMed] [Google Scholar]
- 57.U.S. Environmental Protection Agency. Air Data Pre-generated Data Files <https://aqs.epa.gov/aqsweb/airdata/download_files.html> (2017).
- 58.Merchant RK, Inamdar R & Quade RC Effectiveness of population health management using the propeller health asthma platform: a randomized clinical trial. J. Allergy Clin. Immunol. Pract 4, 455–463 (2016). [DOI] [PubMed] [Google Scholar]
- 59.Van Sickle D, Magzamen S, Truelove S & Morrison T Remote monitoring of inhaled bronchodilator use and weekly feedback about asthma management: an open-group, short-term pilot study of the impact on asthma control. Plos One 8, e55335 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.National Oceanic and Atmospheric Administration. National Centers for Environmental Information, Weather and Climate Data, <https://www.ncdc.noaa.gov/orders/qclcd/> (2017).
- 61.U.S. Centers for Disease Control & Prevention. CDC's Social Vulnerability Index (SVI), <https://svi.cdc.gov/data-and-tools-download.html> (2016).
- 62.Angrist JD & Pischke J-S Mostly Harmless Econometrics: An Empiricist's Companion. (Princeton University Press, 2009). [Google Scholar]
- 63.Glymour M & Greenland S in Modern Epidemiology, 3rd Edition (eds Rothman KJ, Greenland S, & Lash TL) 183–209 (Lippincott Williams and Wilkins, 2008). [Google Scholar]
- 64.Pope CA 3rd, Ezzati M & Dockery DW Fine-particulate air pollution and life expectancy in the United States. N. Engl. J. Med 360, 376–386 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abadie A, Athey S, Imbens GW & Wooldridge J When should you adjust standard errors for clustering? NBER, <https://www.nber.org/papers/w24003> (2017). [Google Scholar]
- 66.Armstrong BG, Gasparrini A & Tobias A Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med. Res. Methodol 14, 122 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bernal JL, Cummins S & Gasparrini A Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol 46, 348–355 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Petersen I, Douglas I & Whitaker H Self controlled case series methods: an alternative to standard epidemiological study designs. BMJ 354, i4515 (2016). [DOI] [PubMed] [Google Scholar]
- 69.Brumback BA et al. Transitional regression models, with application to environmental time series. J. Am. Stat. Assoc 95, 16–27 (2000). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The ZIP code-level asthma hospitalization/ERV data are available from the authors following submission of an analysis proposal and written approval granted by the Louisville Metro Public Health and Wellness. The AIR Louisville monthly medication use data are considered Protected Health Information (PHI) under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) in the U.S., and as such may be accessible from the authors for analysis only after specific written authorization of access following HIPAA guidelines and IRB approval. We provide Jefferson County ZIP code-level monthly HyADS estimates on GitHub at https://github.com/joanacasey/ky_asthma_coal.