Abstract
Study Design:
International consensus paper on a unified nomenclature for full-endoscopic spine surgery.
Objectives:
Minimally invasive endoscopic spinal procedures have undergone rapid development during the past decade. Evolution of working-channel endoscopes and surgical instruments as well as innovation in surgical techniques have expanded the types of spinal pathology that can be addressed. However, there is in the literature a heterogeneous nomenclature defining approach corridors and procedures, and this lack of common language has hampered communication between endoscopic spine surgeons, patients, hospitals, and insurance providers.
Methods:
The current report summarizes the nomenclature reported for working-channel endoscopic procedures that address cervical, thoracic, and lumbar spinal pathology.
Results:
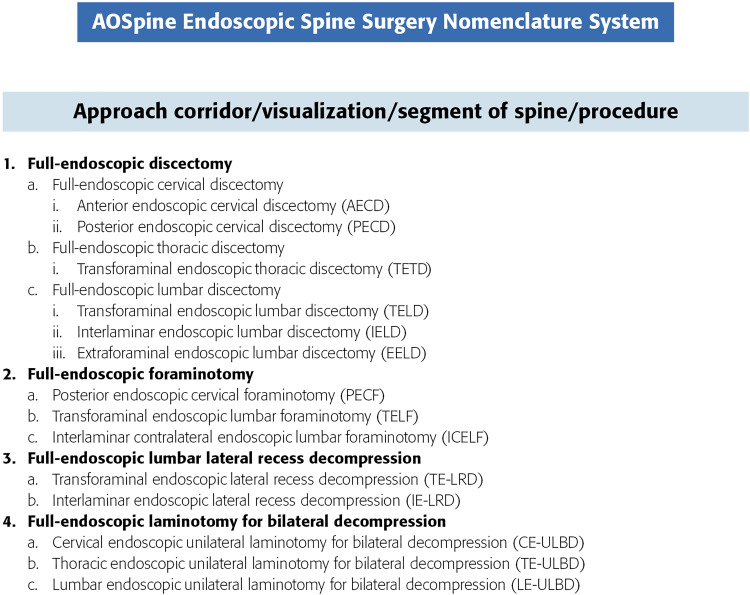
We propose a uniform system that defines the working-channel endoscope (full-endoscopic), approach corridor (anterior, posterior, interlaminar, transforaminal), spinal segment (cervical, thoracic, lumbar), and procedure performed (eg, discectomy, foraminotomy). We suggest the following nomenclature for the most common full-endoscopic procedures: posterior endoscopic cervical foraminotomy (PECF), transforaminal endoscopic thoracic discectomy (TETD), transforaminal endoscopic lumbar discectomy (TELD), transforaminal lumbar foraminotomy (TELF), interlaminar endoscopic lumbar discectomy (IELD), interlaminar endoscopic lateral recess decompression (IE-LRD), and lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD).
Conclusions:
We believe that it is critical to delineate a consensus nomenclature to facilitate uniformity of working-channel endoscopic procedures within academic scholarship. This will hopefully facilitate development, standardization of procedures, teaching, and widespread acceptance of full-endoscopic spinal procedures.
Keywords: consensus, full-endoscopic spine surgery, interlaminar, lateral recess decompression, transforaminal, minimally invasive spinal surgery, nomenclature, working-channel endoscope
Introduction
During the past 30 years, surgeons have developed minimally invasive methods to approach spinal pathology utilizing endoscopes introduced via tubular retractors. As the technology and techniques have advanced, the terminology used to describe these procedures has developed organically and has become heterogeneous and sometimes confusing to patients, providers, and payors. The purpose of this article is to provide the reader with consensus definitions to allow improved communication, study, and understanding of endoscopic techniques.
For our purposes, the endoscope will be defined as a visualization device that is placed into the body. Fundamentally the endoscope can be used as a visualization tool that with an integrated working channel also provides a surgical corridor for tools to manipulate, ablate, and resect tissue. We propose the term “full-endoscopic” to describe procedures performed with a working-channel endoscope. This distinguishes full-endoscopic procedures from “endoscope assisted” operations where tools are passed through trajectories separate from the endoscope (Figure 1).
Figure 1.
Summary of current spinal procedures using endoscopic visualization.
Multiple full-endoscopic approaches to the spinel have been described and performed over the past 30 years. Transforaminal approaches were established after description of the medial aspect of the foraminal annular window as an area of safe access to the disc space.1 Since then endoscopic discectomy became commonly offered in several surgical centers.2 More recently with improvements in camera technology and the development of better instruments, surgeons have more readily used the endoscope in direct approaches to the spine by interlaminar techniques allowing the treatment of degenerative spinal pathology, resecting yellow ligament, overgrown facet joints, and osteophytes. Thus, current working-channel endoscopy may be utilized to treat foraminal,3 lateral recess,4,5 and central spinal stenosis.6-8 Using a unilateral approach, bilateral decompression of central and lateral recess stenosis in the lumbar spine is feasible and has been demonstrated to result in favorable clinical outcomes.6-8 Endoscopic spine surgery has been shown to be useful in the treatment of cervical foraminal stenosis,9-11 cervical disc herniations,12 and thoracic disc herniations.13 Moreover, endoscopic spine surgery allows for decompression of nerve roots within arthrodesis constructs without removal of instrumentation.14,15 By their nature, minimally invasive techniques require significantly less tissue manipulation and, therefore, cause less collateral tissue damage during the surgical approach. This has objectively been shown to minimize local and systemic inflammation, and iatrogenic muscle injury.16-18 Furthermore, several studies validate that minimally invasive endoscopic techniques do not compromise surgical outcomes, as similar or better results have been reported when compared with traditional open surgery.19-27 Importantly, full-endoscopic spine surgery provides high-resolution, off-axis visualization of the surgical field and is associated with a favorably low rate of perioperative and postoperative complications compared with minimally invasive spine surgery (MISS) or traditional spine surgery.28
Methods
The PubMed database was queried using the terms “spine,” “full-endoscopic,” “working-channel endoscope,” “spine endoscopy,” “percutaneous.” The obtained studies were reviewed, and utilization of full-endoscopic technique was verified. The previously utilized nomenclature was compared and integrated into a systematic nomenclature system (approach corridor/mode of visualization/spinal segment/type of procedure). An additional 27 authors were selected by D. Jin-Sung and Hofstetter according to the following 3 criteria: First, active involvement in teaching cadaveric courses and lecturing on full-endoscopic spine surgery. We consider this most valuable as it makes sure that all authors have a similar understanding of full-endoscopic spine procedures and carry them out utilizing comparable technique. Second, a strong publication record. We considered this important in order involve the majority of surgeons who have utilized various naming systems in the past and were therefore able to contribute, accept, and utilize the novel unified AOSpine nomenclature system. Third, geographic location of the authors played into the selection. This was done in order to also include surgeons as key opinion leaders from countries that are currently less active in full-endoscopic spine surgery. However, the geographic consideration also led to omission of some highly esteemed surgeon in countries with a high density of full-endoscopic spine surgeons. Our nomenclature suggestions were actively discussed and adjusted with all 28 authors of the current report. The nomenclature suggestion was reviewed, discussed, and accepted in the current form by all authors and also discussed at the annual Global Spine meeting with key opinion leaders. The consensus nomenclature was developed within the AOSpine MISS taskforce.
Anterior Endoscopic Cervical Discectomy (AECD)
Background
The anterior approach to the cervical spine utilizes physiological tissue planes between the esophagus and the carotid artery and is associated with only minimal irritation of surrounding soft tissues. In the early 1990s, Courtheoux et al29 adopted the use of automated percutaneous nucleotomy techniques30 for the treatment of cervical radiculopathy and this led to the later development of the endoscopic cervical discectomy. Although Ahn and colleagues31 reported in 2005 that “percutaneous endoscopic cervical discectomy” was an effective treatment option for soft disc herniations in selected patients, it is recognized that surgery may contribute to accelerated disc degeneration, given that the approach corridor includes healthy disc tissue. Whether this matters is not certain,32 but one way of potentially circumventing the problem is to use an anterior transcorporal technique with a working corridor through the vertebral body rather than through the disc space.33 Ruetten and colleagues34 concluded that endoscopic anterior discectomy has similar long-term results to those of conventional procedures and this is borne out in a recent literature review.35 However, the risk of exacerbated index-level disc degeneration and changes in sagittal alignment following these procedures require further study.
Previously Used Nomenclature
Goal of Surgery
Resection of any disc herniation and decompression of the proximal portion of the segmental cervical nerve root.
Proposed Nomenclature
Anterior endoscopic cervical discectomy (AECD).
Rationale
Percutaneous implies a purely image-guided procedure (eg, guided by CT [computed tomography] or fluoroscopy); hence, the term is incorrect, since the endoscope provides continuous direct visualization of the treated pathology. The term “full-endoscopic” was used to distinguish working-channel endoscopy from non–working-channel endoscopic techniques such as micro-endoscopic or biportal. Thus, the current consensus paper proposes the term full-endoscopic as a summary term for working-channel endoscopic procedures.
Posterior Endoscopic Cervical Foraminotomy (PECF) or Discectomy (PECD)
Background
Posterior cervical foraminotomy aims at widening the cervical intervertebral foramen, while preserving segmental motion.38 Several minimally invasive approaches have been developed including microscope-assisted “keyhole” foraminotomy, micro-endoscope, and endoscope-assisted techniques.39-42 Ruetten and colleagues43 were the first to describe “full-endoscopic” cervical approaches introducing the endoscope via a small tubular retractor. Kim and colleagues44 reported similar clinical results comparing posterior tubular-based microscope-assisted with percutaneous endoscopic techniques. A recent publication12 proposed a new technique for posterior percutaneous endoscopic foraminotomy and discectomy using unilateral biportal endoscopy, claiming a wider visualization and more familiar surgical field.
Previously Used Nomenclature
Goal of Surgery
Direct visualization and decompression of the exiting nerve root from its origin to the lateral margin of the caudal pedicle.
Proposed Name
Posterior endoscopic cervical foraminotomy (PECF) or discectomy (PECD).
Rationale
“Percutaneous” is not included as this has been associated with purely image-guided procedures (eg, guided by CT or fluoroscopy); hence, the term is confusing. Only an endoscope provides continuous direct visualization of the treated pathology. The term “full-endoscopic” is used to distinguish working-channel endoscopy from hybrid procedures (mini-open/tubular) that were performed with assistance of a non–working-channel endoscope.
Cervical/Thoracic Endoscopic Unilateral Laminotomy for Bilateral Decompression (CE-ULBD/TE-ULBD)
Background
The concept of unilateral laminotomy for bilateral access to the spinal canal was developed in the lumbar spine to minimize postoperative segmental instability50 and adapted to use in the neck.51 Good or fair functional outcomes were reported and the authors concluded that ULBD was a reasonable alternative to open laminectomy or laminoplasty in patients with cervical spinal stenosis from compression by the posterior elements. We are not aware of any reports on the use of working-channel endoscopes for this procedure.
Previously Used Nomenclature
No data.
Proposed Name
Cervical/thoracic endoscopic unilateral laminotomy for bilateral decompression (CE-ULBD/TE-ULBD).
Transforaminal Endoscopic Thoracic Discectomy (TETD)
Background
Few reports have been published on the use of working-channel endoscopy for thoracic disc herniations.13,52-54 Choi et al53 demonstrated the benefits of endoscopic transforaminal thoracic discectomy in 14 patients with soft lateral or central thoracic disc herniation. The approach requires a foraminotomy and is followed by a transforaminal discectomy. Wagner and colleagues presented a case report on a patient with a T8-T9 herniated disc, who was successfully treated by transforaminal endoscopic foraminoplasty and discectomy under local anesthesia.13 Considering the anatomy of thoracic spine and the adjoining ribs, the approach angle is limited. Foraminoplasty is mandatory in order to create a space for the working cannula with a little gain of additional angulation. This approach is well suited for disc herniations that are off midline. This approach is less suited for the upper thoracic spine since the scapula may block the approach corridor.
Previously Used Nomenclature
Goal of Surgery
Visualization of the annulus and adjacent parts of the vertebral bodies and the ventral portion of the thecal sac to the medial aspect of the contralateral pedicle.
Proposed Nomenclature
Transforaminal endoscopic thoracic discectomy (TETD).
Rationale
The use of the terms “percutaneous” is confusing (see above). In order to distinguish this procedure from transthoracic approaches we propose to include “transforaminal” as the designation of the approach corridor.
Transforaminal Endoscopic Lumbar Discectomy (TELD)
Background
The description of the medial aspect of the foraminal annular window “triangle of Kambin,” bordered by the exiting root rostrally, the traversing root medially, and the superior endplate of the lower lumbar vertebra inferiorly, is considered as one of the milestones in the development of transforaminal approaches for endoscopic spine surgery. This safe entry passage to the intervertebral disc allowed for the development of very limited, small needle-like nucleotomy instruments that prepared the path for development of larger instruments and working channels. This approach was pioneered by Kambin who reported the results of 175 patients undergoing bilateral biportal and unilateral uniportal techniques base on the location of the herniation.57 Yeung developed his YESS (Yeung Endoscopic Spine System) system and published his own experience with posterolateral endoscopic decompression in 307 consecutive patients with radiculopathy secondary to lumbar disc herniation.58,59 Yeung’s technique was an “inside out,” which involved advancement of the endoscope into the disc nucleus via the foraminal annular window. Disc material is then resected while withdrawing the endoscope. Recently, “outside in” techniques have been more commonly practiced, which may include partial resection of the superior articular process for access.2,60 This technique allows for visualization and identification of bony anatomical landmarks such as the medial aspect of the pedicle and for direct visualization of the traversing and exiting nerve root.
Previously Used Nomenclature
Goal of Surgery
Resection of any disc herniation visualizing segmentally decompressed nerve roots.
Proposed Nomenclature
Transforaminal endoscopic lumbar discectomy (TELD).
Rationale
The term “arthroscopic” refers to endoscopic surgery within a joint space, which does not reflect the procedure. The approach corridor is more precisely defined with “transforaminal” compared to “posterolateral.” The term “minimally invasive” is currently used for tubular approaches combined with microscopic illumination and visualization.
Transforaminal Endoscopic Lumbar Foraminotomy (TELF)
Background
Shortly after the discovery of the foraminal annular window “triangle of Kambin,” surgeons started to explore and study the intervertebral foramen and associated pathologies in more detail. Mathews66 demonstrated a foraminoscopy utilizing an endoscopic transforaminal technique. In the early 2000s, Knight et al67 reported on their experience regarding an endoscopic-guided foraminal decompression and called it a “foraminoplasty.” These procedures included undercutting of the facet joint, and endoscopic discectomy, mobilization and neurolysis of the exiting and transiting nerves, and ablation of osteophytes. Schubert and Hoogland68 described this technique for removal of a sequestered lumbar disk after decompression of foraminal stenosis (foraminoplasty), which was later popularized as the “outside-in” technique. These reports use the term “foraminoplasty” as the process of widening of foramen through which the endoscopic instruments could access and retrieve the ruptured fragments in the spinal canal. However, the term foraminotomy has been usually used to describe decompression of foramen by which an “exiting” nerve root is released.69 For this reason, we recommend the traditional term “foraminotomy” rather than “foraminoplasty” to describe decompression of a symptomatic foraminal stenosis.
Previously Used Nomenclature
Goal of Surgery
To visualize and decompress the affected nerve root along its passage through the foramen.
Proposed Name
Transforaminal endoscopic lumbar foraminotomy (TELF).
Rationale
The term “foraminoplasty” has been used to describe resection of the superior articular process to gain access to the foramen as a procedural step in transforaminal surgery. However, the more traditional term “foraminotomy” includes both bony decompression and also resection of soft tissue as necessary in order to relieve a compressed symptomatic nerve root. The latter is the main reason for performing this surgery and should therefore guide the nomenclature.
Endoscopic Interlaminar Discectomy
Background
The traditional surgical approach for lumbar disc herniations has been via the interlaminar space. Endoscope-assisted techniques via tubular retractors have been described as posterior endoscopic discectomy,70 endoscopic lumbar discectomy,71 or microendoscopic discectomy (MED).72 Other terminology was introduced with full-endoscopic techniques as detailed below.
Previously Used Nomenclature:
Goal of Surgery
Resection of any disc herniation and visualization of the decompressed nerve roots.
Proposed Nomenclature
Interlaminar endoscopic lumbar discectomy (IELD).
Rationale
The use of the terms “percutaneous” and “full-endoscopic” are redundant as outlined above. It is critical that the term for this procedure includes the approach corridor, which is “interlaminar,” to distinguish it from the transforaminal approach.
Interlaminar Endoscopic Lateral Recess Decompression (IE-LRD)
Background
Medial facetectomies aim to decompress neural elements impinged in the lateral recess underneath the superior articular process. This may be done minimally invasively using a 16 mm tubular retractor in combination with microendoscopic techniques83 but also by interlaminar lateral recess decompression using a working-channel endoscope.4 Indeed, a prospective randomized controlled trial demonstrated similar clinical effectiveness of endoscopic compared to minimally invasive lateral recess decompression.7
Previously Used Nomenclature
Goal of Surgery
Decompression and visualization of the neural elements within the lateral recess from the tip of the superior articular process (SAP) to the midportion of the caudal pedicle.
Proposed Nomenclature
Interlaminar endoscopic lateral recess decompression (IE-LRD).
Rationale
The use of the terms “percutaneous” and “full-endoscopic” are redundant as outlined above. It is critical that the term for this procedure includes the approach corridor, which is “interlaminar,” to distinguish it from the transforaminal approach, which also allows for lateral recess decompression.
Transforaminal Endoscopic Lateral Recess Decompression (TE-LRD)
Background
Symptomatic lateral recess stenosis is typically caused by impingement of the traversing nerve root between the annulus of the disc and SAP. Traditionally, interlaminar approaches have been utilized for decompression neural elements impinged within the lateral recess. Kambin et al first introduced the concept of transforaminal decompression of the lateral recess.84 The authors described decompression of the traversing nerve root by annulectomy and resection of marginal osteophytes originating from the posterior aspect of the vertebral body end plate. A recent cadaveric study demonstrated that the transforaminal approach combined with an extensive foraminoplasty allows for access to the lateral recess both ventral as well as dorsal to the traversing nerve root.85 Thus, yellow ligament and SAP dorsal to the traversing nerve root can be removed, which the authors referred to as a “ventral facetectomy.” A retrospective case series of 48 patients reports on transforaminal decompression of foraminal or lateral recess stenosis in patients with previous spinal surgery.86 Endoscopic transforaminal decompression resulted in “excellent” or “good” results according to Macnab criteria in 79% of patients. However, while the area of stenosis was meticulously defined according to criteria by Lee et al,87 no diagnostic effort was made to distinguish whether symptoms were caused by either the traversing or exiting nerve root.
Previously Used Nomenclature
Goal of Surgery
Ventral and dorsal decompression and visualization of the traversing nerve root within the lateral recess from the rostral aspect of the annulus to the rostral portion of the caudal pedicle.
Proposed Nomenclature
Transforaminal endoscopic lateral recess decompression (TE-LRD).
Rationale
The use of the term “percutaneous” is redundant as outlined above. We prefer the term “lateral recess decompression” to “ventral facetectomy” since the transforaminal route allows both ventral and dorsal decompression of the traversing nerve root. Ventral decompression includes resection of the posterior marginal endplate osteophytes and the disc annulus.
Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression (LE-ULBD)
Background
Degenerative symptomatic lumbar spinal stenosis occurs typically at the level of the disc-facet joint complex. Unilateral laminotomy for bilateral access to the spinal canal is now more commonly performed than laminectomy and aims to minimize postoperative segmental instability.50 Endoscopic decompression has been developed as an extension of transforaminal and interlaminar discectomy.4 A recent cadaveric study demonstrated that the transforaminal approach combined with an extensive foraminoplasty allowed access to the lateral recess both ventral and dorsal to the traversing nerve root.85 Minimally invasive tubular decompression for lumbar spinal stenosis has demonstrated favorable reduction in Oswestry Disability Index and leg pain while maintaining a low complication profile.88-91 Adaptation of the techniques for a working-channel endoscope have recently been described for decompression of central and lateral recess stenosis in the lumbar spine.6,8,86,92
Previously Used Nomenclature
Goal of Surgery
Complete central and lateral recess decompression of the neural elements spanning from the tip of the SAP to the midportion of the caudal pedicle.
Proposed Nomenclature
Lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD).
Rationale
The use of the terms “percutaneous” and “full-endoscopic” are redundant as outlined above. The term “laminectomy” is traditionally utilized to signify complete removal of the lamina and spinous process, although, colloquially, the term is often interchanged with “laminotomy.” Given that with this technique the entire lamina is not removed but rather undercut, the term “laminotomy” will be used to reflect removal of only a portion of the lamina. The approach is performed unilaterally with bilateral decompression of the neural elements both centrally and in the lateral recess. Hence, the nomenclature “endoscopic unilateral laminotomy for bilateral decompression” reflects the procedure most accurately.
Discussion
Full endoscopic spine surgery represents the evolution of minimally invasive surgical access to spinal pathology. Although the first spinal endoscopic procedures were performed in the early 1980s in the United States,61 there has been a steady and persistent increase in popularity, particularly in Europe and Asia. Multiple studies6,7,60,63-65,93 have demonstrated endoscopic techniques provide equivalent outcomes to microsurgical or tubular techniques with shorter hospital stay,94 less local collateral tissue injury,95 and systemic stress.96,97 With continued evolution in surgical techniques and technological innovations, endoscopic techniques have been gaining broader appeal with techniques expanding to the cervical98,99 and thoracic spine.55,56
As this field continues to expand and evolve, it is critical for surgeons to address the mélange of endoscopic procedures within the literature to provide a solid foundation for future scholarship. The authors believe that it is therefore critical to construct and define a consistent nomenclature framework within endoscopic spine surgery to clearly define full-endoscopic procedures and delineate their clinical effectiveness.
Moreover, a standardized nomenclature will promote scientific exchange and should facilitate further refinement of full-endoscopic procedures (Figure 2). Perhaps the most crucial function of standardization of nomenclature and techniques is to facilitate teaching of these techniques to allow the field of spine surgery to concomitantly evolve with our technological advancements. The AOspine (Arbeitsgemeinschaft für Osteosynthesefragen) poses an ideal international community to deliver knowledge, experience, and evidence regarding full-endoscopic spine surgery with the ultimate goal to improve patient care and outcomes.
Figure 2.
Suggested new nomenclature for endoscopic spinal procedures.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This supplement was supported by funding from the Carl Zeiss Meditec Group.
ORCID iD: Christoph P. Hofstetter, MD, PhD  https://orcid.org/0000-0002-5324-950X
https://orcid.org/0000-0002-5324-950X
Jun-Ho Lee, MD, PhD  https://orcid.org/0000-0001-6246-8053
https://orcid.org/0000-0001-6246-8053
References
- 1. Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res. 1986;(207):37–43. [PubMed] [Google Scholar]
- 2. Gibson JN, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: the future “gold standard” for discectomy? A review. Surgeon. 2012;10:290–296. [DOI] [PubMed] [Google Scholar]
- 3. Evins AI, Banu MA, Njoku I, Jr, et al. Endoscopic lumbar foraminotomy. J Clin Neurosci. 2015;22:730–734. [DOI] [PubMed] [Google Scholar]
- 4. Birjandian Z, Emerson S, Telfeian AE, Hofstetter CP. Interlaminar endoscopic lateral recess decompression-surgical technique and early clinical results. J Spine Surg. 2017;3:123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krzok G, Telfeian AE, Wagner R, Hofstetter CP, Iprenburg M. Contralateral facet-sparing sublaminar endoscopic foraminotomy for the treatment of lumbar lateral recess stenosis: technical note. J Spine Surg (Hong Kong). 2017;3:260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18:61–70. [PubMed] [Google Scholar]
- 7. Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009;10:476–485. [DOI] [PubMed] [Google Scholar]
- 8. Wagner R, Telfeian AE, Kzrok G, Iprenburg M. Fully-endoscopic lumbar laminectomy for central and lateral recess stenosis: Technical note. Interdiscip Neurosurg. 2018;13:6–9. [Google Scholar]
- 9. Wagner R, Telfeian AE, Iprenburg M, Krzok G. Minimally invasive fully endoscopic two-level posterior cervical foraminotomy: technical note. J Spine Surg. 2017;3:238–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ye ZY, Kong WJ, Xin ZJ, et al. Clinical observation of posterior percutaneous full-endoscopic cervical foraminotomy as a treatment for osseous foraminal stenosis. World Neurosurg. 2017;106:945–952. [DOI] [PubMed] [Google Scholar]
- 11. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:940–948. [DOI] [PubMed] [Google Scholar]
- 12. Park JH, Jun SG, Jung JT, Lee SJ. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics. 2017;40:e779–e783. [DOI] [PubMed] [Google Scholar]
- 13. Wagner R, Telfeian AE, Iprenburg M, et al. Transforaminal endoscopic foraminoplasty and discectomy for the treatment of a thoracic disc herniation. World Neurosurg. 2016;90:194–198. [DOI] [PubMed] [Google Scholar]
- 14. Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 2017;43:E8. [DOI] [PubMed] [Google Scholar]
- 15. McGrath LB, Jr, Madhavan K, Chieng LO, Wang MY, Hofstetter CP. Early experience with endoscopic revision of lumbar spinal fusions. Neurosurg Focus. 2016;40:E10. [DOI] [PubMed] [Google Scholar]
- 16. Sasaoka R, Nakamura H, Konishi S, et al. Objective assessment of reduced invasiveness in MED. Compared with conventional one-level laminotomy. Eur Spine J. 2006;15:577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schick U, Dohnert J, Richter A, Konig A, Vitzthum HE. Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur Spine J. 2002;11:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shin DA, Kim KN, Shin HC, Yoon DH. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. [DOI] [PubMed] [Google Scholar]
- 19. Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong). 2011;19:30–34. [DOI] [PubMed] [Google Scholar]
- 20. Hussein M, Abdeldayem A, Mattar MM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. 2014;23:1992–1999. [DOI] [PubMed] [Google Scholar]
- 21. Kim HS, Patel R, Paudel B, et al. Early outcomes of endoscopic contralateral foraminal and lateral recess decompression via an interlaminar approach in patients with unilateral radiculopathy from unilateral foraminal stenosis. World Neurosurg. 2017;108:763–773. [DOI] [PubMed] [Google Scholar]
- 22. Lawton CD, Smith ZA, Lam SK, Habib A, Wong RH, Fessler RG. Clinical outcomes of microendoscopic foraminotomy and decompression in the cervical spine. World Neurosurg. 2014;81:422–427. [DOI] [PubMed] [Google Scholar]
- 23. Minamide A, Yoshida M, Simpson AK, et al. Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study. J Neurosurg Spine. 2017;27:403–409. [DOI] [PubMed] [Google Scholar]
- 24. Minamide A, Yoshida M, Yamada H, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J. 2010;19:487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61:545–549. [DOI] [PubMed] [Google Scholar]
- 26. Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach—technique and prospective results of 463 patients. Spine (Phila Pa 1976). 2005;30:2570–2578. [DOI] [PubMed] [Google Scholar]
- 27. Li XC, Zhong CF, Deng GB, Liang RW, Huang CM. Full-endoscopic procedures versus traditional discectomy surgery for discectomy: a systematic review and meta-analysis of current global clinical trials. Pain Physician. 2016;19:103–118. [PubMed] [Google Scholar]
- 28. Sen RD, White-Dzuro G, Ruzevick J, et al. Intra- and peri-operative complications associated with endoscopic spine surgery: a multi-institutional study. World Neurosurg. 2018;120:e1054–e1060. [DOI] [PubMed] [Google Scholar]
- 29. Courtheoux F, Theron J. Automated percutaneous nucleotomy in the treatment of cervicobrachial neuralgia due to disc herniation. J Neuroradiol. 1992;19:211–216. [PubMed] [Google Scholar]
- 30. Onik G, Helms CA, Ginsburg L, Hoaglund FT, Morris J. Percutaneous lumbar diskectomy using a new aspiration probe. AJR Am J Roentgenol. 1985;144:1137–1140. [DOI] [PubMed] [Google Scholar]
- 31. Ahn Y, Lee SH, Shin SW. Percutaneous endoscopic cervical discectomy: clinical outcome and radiographic changes. Photomed Laser Surg. 2005;23:362–368. [DOI] [PubMed] [Google Scholar]
- 32. Lee JH, Lee SH. Clinical and radiographic changes after percutaneous endoscopic cervical discectomy: a long-term follow-up. Photomed Laser Surg. 2014;32:663–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J. 2007;16:1387–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Int Orthop. 2009;33:1677–1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bucknall V, Gibson JA. Cervical endoscopic spinal surgery: a review of the current literature. J Orthop Surg (Hong Kong). 2018;26:2309499018758520. [DOI] [PubMed] [Google Scholar]
- 36. Ahn Y, Lee SH, Lee SC, Shin SW, Chung SE. Factors predicting excellent outcome of percutaneous cervical discectomy: analysis of 111 consecutive cases. Neuroradiology. 2004;46:378–384. [DOI] [PubMed] [Google Scholar]
- 37. Lee SH, Lee JH, Choi WC, Jung B, Mehta R. Anterior minimally invasive approaches for the cervical spine. Orthop Clin North Am. 2007;38:327–337. [DOI] [PubMed] [Google Scholar]
- 38. Epstein NE. A review of laminoforaminotomy for the management of lateral and foraminal cervical disc herniations or spurs. Surg Neurol. 2002;57:226–233. [DOI] [PubMed] [Google Scholar]
- 39. Roh SW, Kim DH, Cardoso AC, Fessler RG. Endoscopic foraminotomy using MED system in cadaveric specimens. Spine (Phila Pa 1976). 2000;25:260–264. [DOI] [PubMed] [Google Scholar]
- 40. Burke TG, Caputy A. Microendoscopic posterior cervical foraminotomy: a cadaveric model and clinical application for cervical radiculopathy. J Neurosurg. 2000;93(1 suppl):126–129. [DOI] [PubMed] [Google Scholar]
- 41. Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery. 2002;51(5 suppl):S37–S45. [PubMed] [Google Scholar]
- 42. O’Toole JE, Sheikh H, Eichholz KM, Fessler RG, Perez-Cruet MJ. Endoscopic posterior cervical foraminotomy and discectomy. Neurosurg Clin N Am. 2006;17:411–422. [DOI] [PubMed] [Google Scholar]
- 43. Ruetten S, Komp M, Merk H, Godolias G. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg. 2007;50:219–226. [DOI] [PubMed] [Google Scholar]
- 44. Kim CH, Kim KT, Chung CK, et al. Minimally invasive cervical foraminotomy and diskectomy for laterally located soft disk herniation. Eur Spine J. 2015;24:3005–3012. [DOI] [PubMed] [Google Scholar]
- 45. Kim CH, Chung CK, Kim HJ, Jahng TA, Kim DG. Early outcome of posterior cervical endoscopic discectomy: an alternative treatment choice for physically/socially active patients. J Korean Med Sci. 2009;24:302–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yang JS, Chu L, Chen L, Chen F, Ke ZY, Deng ZL. Anterior or posterior approach of full-endoscopic cervical discectomy for cervical intervertebral disc herniation? A comparative cohort study. Spine (Phila Pa 1976) 2014;39:1743–1750. [DOI] [PubMed] [Google Scholar]
- 47. Ahn Y. Percutaneous endoscopic cervical discectomy using working channel endoscopes. Expert Rev Med Devices. 2016;13:601–610. [DOI] [PubMed] [Google Scholar]
- 48. Quillo-Olvera J, Lin GX, Kim JS. Percutaneous endoscopic cervical discectomy: a technical review. Ann Transl Med. 2018;6:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Youn MS, Shon MH, Seong YJ, Shin JK, Goh TS, Lee JS. Clinical and radiological outcomes of two-level endoscopic posterior cervical foraminotomy. Eur Spine J. 2017;26:2450–2458. [DOI] [PubMed] [Google Scholar]
- 50. Spetzger U, Bertalanffy H, Naujokat C, von Keyserlingk DG, Gilsbach JM. Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis. Part I: anatomical and surgical considerations. Acta Neurochir (Wien). 1997;139:392–396. [DOI] [PubMed] [Google Scholar]
- 51. Dahdaleh NS, Wong AP, Smith ZA, Wong RH, Lam SK, Fessler RG. Microendoscopic decompression for cervical spondylotic myelopathy. Neurosurg Focus. 2013;35:E8. [DOI] [PubMed] [Google Scholar]
- 52. Nie HF, Liu KX. Endoscopic transforaminal thoracic foraminotomy and discectomy for the treatment of thoracic disc herniation. Minim Invasive Surg. 2013;2013:264105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Choi KY, Eun SS, Lee SH, Lee HY. Percutaneous endoscopic thoracic discectomy; transforaminal approach. Minim Invasive Neurosurg. 2010;53:25–28. [DOI] [PubMed] [Google Scholar]
- 54. Krzok G, Telfeian AE, Wagner R, Iprenburg M. Transpedicular endoscopic surgery for lumbar spinal synovial cyst-report of two cases. J Spine Surg (Hong Kong). 2016;2:310–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ruetten S, Hahn P, Oezdemir S, Baraliakos X, Godolias G, Komp M. Operation of soft or calcified thoracic disc herniations in the full-endoscopic uniportal extraforaminal technique. Pain Physician. 2018;21:E331–E340. [PubMed] [Google Scholar]
- 56. Shen J. Fully endoscopic transforaminal discectomy under local anesthesia for thoracic disc herniations: a case series. J Spine. 2018;7:13. [Google Scholar]
- 57. Kambin P, O’Brien E, Zhou L, Schaffer JL. Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop Relat Res. 1998;(347):150–167. [PubMed] [Google Scholar]
- 58. Yeung AT. Minimally invasive disc surgery with the Yeung Endoscopic Spine System (YESS). Surg Technol Int. 1999;8:267–277. [PubMed] [Google Scholar]
- 59. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 2002;27:722–731. [DOI] [PubMed] [Google Scholar]
- 60. Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976). 2006;31:E890–E897. [DOI] [PubMed] [Google Scholar]
- 61. Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res. 1987;(223):145–154. [PubMed] [Google Scholar]
- 62. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:931–939. [DOI] [PubMed] [Google Scholar]
- 63. Gibson JNA, Subramanian AS, Scott CEH. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur Spine J. 2017;26:847–856. [DOI] [PubMed] [Google Scholar]
- 64. Chen Z, Zhang L, Dong J, et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine. 2018;28:300–310. [DOI] [PubMed] [Google Scholar]
- 65. Sinkemani A, Hong X, Gao ZX, et al. Outcomes of microendoscopic discectomy and percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation: a comparative retrospective study. Asian Spine J. 2015;9:833–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Mathews HH. Transforaminal endoscopic microdiscectomy. Neurosurg Clin N Am. 1996;7:59–63. [PubMed] [Google Scholar]
- 67. Knight MT, Goswami A, Patko JT, Buxton N. Endoscopic foraminoplasty: a prospective study on 250 consecutive patients with independent evaluation. J Clin Laser Med Surg. 2001;19:73–81. [DOI] [PubMed] [Google Scholar]
- 68. Schubert M, Hoogland T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol. 2005;17:641–661. [DOI] [PubMed] [Google Scholar]
- 69. Ahn Y, Oh HK, Kim H, Lee SH, Lee HN. Percutaneous endoscopic lumbar foraminotomy: an advanced surgical technique and clinical outcomes. Neurosurgery. 2014;75:124–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Brayda-Bruno M, Cinnella P. Posterior endoscopic discectomy (and other procedures). Eur Spine J. 2000;9(suppl 1):S24–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Destandau J. A special device for endoscopic surgery of lumbar disc herniation. Neurol Res. 1999;21:39–42. [DOI] [PubMed] [Google Scholar]
- 72. Perez-Cruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery. 2002;51(5 suppl):S129–S136. [PubMed] [Google Scholar]
- 73. Wang B, Lu G, Liu W, Cheng I, Patel AA. Full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation: the causes and prophylaxis of conversion to open. Arch Orthop Trauma Surg. 2012;132:1531–1538. [DOI] [PubMed] [Google Scholar]
- 74. Ruetten S, Komp M, Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49:80–87. [DOI] [PubMed] [Google Scholar]
- 75. Casimiro M. Short-term outcome comparison between full-endoscopic interlaminar approach and open minimally invasive microsurgical technique for treatment of lumbar disc herniation. World Neurosurg. 2017;108:894–900.e1. [DOI] [PubMed] [Google Scholar]
- 76. Shi C, Kong W, Liao W, et al. The early clinical outcomes of a percutaneous full-endoscopic interlaminar approach via a surrounding nerve root discectomy operative route for the treatment of ventral-type lumbar disc herniation. Biomed Res Int. 2018;2018:9157089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58(1 suppl):ONS59–ONS68. [DOI] [PubMed] [Google Scholar]
- 78. Dabo X, Ziqiang C, Yinchuan Z, et al. The clinical results of percutaneous endoscopic interlaminar discectomy (PEID) in the treatment of calcified lumbar disc herniation: a case-control study. Pain Physician. 2016;19:69–76. [PubMed] [Google Scholar]
- 79. Kim CH, Chung CK, Woo JW. Surgical outcome of percutaneous endoscopic interlaminar lumbar discectomy for highly migrated disk herniation. Clin Spine Surg. 2016;29:E259–E266. [DOI] [PubMed] [Google Scholar]
- 80. Kim HS, Park JY. Comparative assessment of different percutaneous endoscopic interlaminar lumbar discectomy (PEID) techniques. Pain Physician. 2013;16:359–367. [PubMed] [Google Scholar]
- 81. Sasani M, Ozer AF, Oktenoglu T, Canbulat N, Sarioglu AC. Percutaneous endoscopic discectomy for far lateral lumbar disc herniations: prospective study and outcome of 66 patients. Minim Invasive Neurosurg. 2007;50:91–97. [DOI] [PubMed] [Google Scholar]
- 82. Koga S, Sairyo K, Shibuya I, et al. Minimally invasive removal of a recurrent lumbar herniated nucleus pulposus by the small incised microendoscopic discectomy interlaminar approach. Asian J Endosc Surg. 2012;5:34–37. [DOI] [PubMed] [Google Scholar]
- 83. Hayashi A, Oshima Y, Shiboi R, et al. Microendoscopic posterior decompression for the treatment of lumbar lateral recess stenosis. J Spine. 2016;5:317. [Google Scholar]
- 84. Kambin P, Casey K, O’Brien E, Zhou L. Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg. 1996;84:462–467. [DOI] [PubMed] [Google Scholar]
- 85. Sairyo K, Higashino K, Yamashita K, et al. A new concept of transforaminal ventral facetectomy including simultaneous decompression of foraminal and lateral recess stenosis: technical considerations in a fresh cadaver model and a literature review. J Med Invest. 2017;64:1–6. [DOI] [PubMed] [Google Scholar]
- 86. Lewandrowski KU. Endoscopic transforaminal and lateral recess decompression after previous spinal surgery. Int J Spine Surg. 2018;12:98–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine (Phila Pa 1976). 1988;13:313–320. [DOI] [PubMed] [Google Scholar]
- 88. Boukebir MA, Berlin CD, Navarro-Ramirez M, et al. Ten-step minimally invasive spine lumbar decompression and dural repair through tubular retractors. Oper Neurosurg (Hagerstown). 2017;13:232–245. [DOI] [PubMed] [Google Scholar]
- 89. Alimi M, Hofstetter CP, Pyo SY, Paulo D, Härtl R. Minimally invasive laminectomy for lumbar spinal stenosis in patients with and without preoperative spondylolisthesis: clinical outcome and reoperation rates. J Neurosurg Spine. 2015;22:339–352. [DOI] [PubMed] [Google Scholar]
- 90. Alimi M, Hofstetter CP, Torres-Campa JM, et al. Unilateral tubular approach for bilateral laminotomy: effect on ipsilateral and contralateral buttock and leg pain. Eur Spine J. 2017;26:389–396. [DOI] [PubMed] [Google Scholar]
- 91. Thome C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3:129–141. [DOI] [PubMed] [Google Scholar]
- 92. Lee CW, Yoon KJ, Jun JH. Percutaneous endoscopic laminotomy with flavectomy by uniportal, unilateral approach for the lumbar canal or lateral recess stenosis. World Neurosurg. 2018;113:e129–e137. [DOI] [PubMed] [Google Scholar]
- 93. Tacconi L, Baldo S, Merci G, Serra G. Transforaminal percutaneous endoscopic lumbar discectomy: outcome and complications in 270 cases [published online March 26, 2018]. J Neurosurg Sci. doi:10.23736/S0390-5616.18.04395-3 [DOI] [PubMed] [Google Scholar]
- 94. Choi KC, Shim HK, Hwang JS, et al. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. 2018;116:e750–e758. [DOI] [PubMed] [Google Scholar]
- 95. Pan L, Zhang P, Yin Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg. 2014;12:534–537. [DOI] [PubMed] [Google Scholar]
- 96. Chang F, Zhang T, Gao G, et al. Therapeutic effect of percutaneous endoscopic lumbar discectomy on lumbar disc herniation and its effect on oxidative stress in patients with lumbar disc herniation. Exp Ther Med. 2018;15:295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Tao XZ, Jing L, Li JH. Therapeutic effect of transforaminal endoscopic spine system in the treatment of prolapse of lumbar intervertebral disc. Eur Rev Med Pharmacol Sci. 2018;22(1 suppl):103–110. [DOI] [PubMed] [Google Scholar]
- 98. Parihar VS, Yadav N, Ratre S, Dubey A, Yadav YR. Endoscopic anterior approach for cervical disc disease (disc preserving surgery). World Neurosurg. 2018;115:e599–e609. [DOI] [PubMed] [Google Scholar]
- 99. Liao C, Ren Q, Chu L, et al. Modified posterior percutaneous endoscopic cervical discectomy for lateral cervical disc herniation: the vertical anchoring technique. Eur Spine J. 2018;27:1460–1468. [DOI] [PubMed] [Google Scholar]