Abstract
Objectives:
to determine if health literacy is associated with mortality, hospitalizations or emergency department (ED) visits among patients living with HF.
Background:
Growing evidence suggests an association between health literacy and health-related outcomes in patients with heart failure (HF).
Methods:
We searched EMBASE, MEDLINE, PsycInfo and EBSCO CINAHL from inception to 1/1/2019 with the help of a medical librarian. Eligible studies evaluated health literacy among patients with HF and assessed mortality, hospitalizations and ED visits for all causes with no exclusion by time, geography or language. Two reviewers independently selected studies, extracted data, and assessed the methodological quality of the identified studies.
Results:
We included 15 studies, 11 with an overall high methodological quality. Among the observational studies, an average of 24% of patients had inadequate or marginal health literacy. Inadequate health literacy was associated with higher unadjusted risk for mortality (RR: 1.67, 95%CI: 1.18, 2.36), hospitalizations (RR: 1.19, 95%CI: 1.09, 1.29) and ED visits (RR: 1.17, 95%CI: 1.03, 1.32). Combining the adjusted measurements, inadequate health literacy remained statistically associated with mortality (RR: 1.41, 95%CI: 1.06, 1.88) and hospitalizations (RR: 1.12, 95%CI: 1.01, 1.25). Among the 4 interventional studies, 2 effectively improved outcomes among patients with inadequate health literacy.
Conclusions:
In this study, the estimated prevalence of inadequate health literacy was high and inadequate health literacy was associated with increased risk of death and hospitalizations. These findings have important clinical and public health implications and warrant measurement of health literacy and deployment of interventions to improve outcomes.
Keywords: Heart Failure, Health literacy, Mortality, Hospitalization, ED visits
INTRODUCTION
Heart failure (HF) is a highly prevalent disease (1). Patients with HF have almost 50% mortality at 5 years (2) and hospitalizations are common (3). HF requires complex management skills like monitoring weight and blood pressure, glycaemia control, drug and diet adherence and sometimes exercise and weight loss. Thus, greater attention has been directed towards health literacy, which is important to manage a chronic condition such as HF (4-6). Health literacy has been defined as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions” (7). Some studies have suggested that low health literacy may be associated with poor outcomes such as higher risk of mortality (8-10), hospitalizations (8) and emergency department (ED) visits (11), however results across studies are not consistent. A recent systematic review (12) assessed the prevalence and predictors of low health literacy, summarizing the literature available through August 2014, while another systematic review assessed the impact of health literacy on mortality without adjusting for confounders (13). Since it is well established that patients with inadequate health literacy are older, with lower socioeconomic status, lower education attainment and more comorbidities (8-10, 14), failing to combine the adjusted measurements overestimates the effect of health literacy on clinical important outcomes. Moreover, to the best of our knowledge, no meta-analysis has been conducted to estimate the effect of health literacy on hospitalizations and ED visits among patients with HF, which are important public health outcomes.
Identifying health literacy as a factor that affects health outcomes and measuring its effect on patients with HF is essential to allocate more resources for, and research on, interventions to improve health literacy.
METHODS
A protocol for this systematic review was developed a priori and registered in PROSPERO with the following number: CDR42019129094. This review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement(15) and Meta-analysis of Observational Studies in Epidemiology (MOOSE) (16).
Data Source
We conducted a comprehensive literature search among 4 databases: MEDLINE, EMBASE, EBSCO CINAHL and PsycInfo from database inception to January 1st 2019. We also searched systematic reviews on the topic to find additional articles. Authors of relevant conference abstracts were contacted to obtain the eventual full article. A medical librarian (P.J.E.) conducted the research following the inputs of the principal investigator. The main search strategy included key words such as “health”, “literacy”, “illiterate”, “education” and “heart failure”. A more extensive and detailed search strategy has been reported in Online Table 5.
Study Selection
We included observational studies that 1) evaluated health literacy among patients with HF, 2) had at least one of these three outcomes: mortality, hospitalizations, and ED visits for all causes, and 3) focused on adult patients 18 years or older with HF not using a left ventricular assist device (LVAD). We also included all interventional studies that 1) proposed an intervention for patients with inadequate health literacy or a health literacy-sensitive intervention, 2) had at least one or a combination of these three outcomes: mortality, hospitalizations and ED visits for all causes and 3) were focused on patients 18 years or older with HF.
We excluded editorials, conference abstracts, narrative reviews, letters and errata and qualitative research. When a conference abstract was found to fit our inclusion criteria, finding the related published article was attempted through search in our databases and direct contact with the author. We also did not restrict our search to any geographic area, publication time nor language and we searched in the grey literature to identify possible unpublished studies.
The selection of the articles proceeded in two phases. In phase one, two independent reviewers (M.F and A.M.W.) screened through the title and abstract reading all the publications obtained. In case of disagreement, the article was included into the next phase of full text review. In the second phase of the screening, M.F. and A.M.W. independently reviewed all the articles obtained through full text review. Agreement between the two independent reviewers in the second phase was calculated as kappa of 1.0.
For each study included in the systematic review, we extracted the year and place where the study was conducted, age and sex characteristics of the cohort, the type of study design, how the diagnosis of HF was made, if the cases of HF were prevalent or incident, how health literacy was evaluated and which outcome was assessed.
Independent Variable
In the identified body of literature, health literacy was evaluated and reported with different tools. Measurement instruments for health literacy are categorized as objective or subjective measures. While objective health literacy measurement tools evaluate how much the patient comprehends medical information, subjective measurement tools evaluate how much the patients think they understood (17). In our review, objective measures of health literacy include the Short-Test of Functional Health Literacy in Adults (S-TOFHLA) (18) and Short-Assessment of Health Literacy for Spanish Adults (SAHLSA) (19), while subjective measures of health literacy include the Brief Health Literacy Screen (BHLS) (20) and the brief screener created by Chew et al (21,22). Based on the literature, we believe that this categorization provides a useful framework for comparing the approaches (17,22,23). The majority of the studies divided their cohorts of patients in two categories: adequate and inadequate health literacy based on very similar cut points. When the results were presented for adequate, marginal, and inadequate health literacy, we combined the marginal and inadequate health literacy categories based on the findings of previous studies, which state that anything less than adequate health literacy represents a risk factor for outcomes (8,10,24). When the patients were divided into tertiles based on the sample-dependent distribution of a health literacy evaluation tool, we contacted the author to have the data based on standardized cut points. In situations where health literacy was evaluated with the S-TOFHLA in combination with another measurement tool, the choice was to take into consideration the results taken from the S-TOFHLA.
Outcome Measurements
Outcomes of interest included: all-cause death, hospitalizations, and ED visits. For the outcomes of hospitalizations and ED visits, we considered only the first event from the time of enrollment. When the study considered the number of multiple subsequent events, we contacted the author to have the number of first events only. Two attempts to contact authors who presented composite outcomes or unadjusted results were made to obtain the outcomes of interest for meta-analysis. When no response was received from the authors, the study was not included in the meta-analysis but was reported narratively.
Assessment of Methodological Quality
We used the Newcastle-Ottawa scale for cohort studies to assess the methodological quality of individual studies and individual outcomes (25). The scale contains 3 main sections: selection, comparability and outcomes. For the comparability, we considered the domain adequate if results were adjusted for age and sex, and ideal if they adjusted for other confounders relevant to HF. An adequate time of follow-up was considered as 1 year for mortality, 6 months for hospitalizations and 30 days for ED visits.
Based on the results of the Newcastle-Ottawa scale, we divided the studies into high, moderate and low overall methodological quality based on the most important factors in the Newcastle Ottawa Scale, in particular the absence of adjustment was considered as an indicator of low methodological quality, while a less than optimal quality in the selection and outcome part of the scale or lack of adjustment for age and sex were considered indicators of moderate quality.
For interventional studies, we used the Revised Cochrane risk-of-bias tool for randomized trials (RoB 2.0) (26). The scale is composed of various sections, each one evaluating the specific risk of bias regarding the randomization process, deviations from the intended interventions, missing outcomes, measurement of the outcomes and the selection of the reported results. Based on the results from the specific sections, the two reviewers independently assigned each interventional study an overall risk of bias.
Methodological quality was assessed independently by two reviewers (M.F. and A.M.W.) with excellent agreement k=0.85. In case of disagreement, the two reviewers met and came to a consensus decision. The overall quality of the evidence for every outcome was evaluated with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.
Statistical Analysis
We assessed inter-observer agreement between reviewers with Cohen’s kappa. Since heterogeneity was anticipated in comparing different populations with limited health literacy, the random effects model was selected a priori (27). We evaluated the association between inadequate health literacy and the following outcomes: mortality, hospitalizations and ED visits for all causes. We converted Hazard Ratios to Risk Ratios (28) and used these measures for the meta-analysis. Heterogeneity was assessed using I2, which estimates the proportion of total variability between studies due to heterogeneity rather than chance alone (29). A value of 50% or above for I2 was considered to represent substantial heterogeneity. We assessed statistical significance with a two-tailed test and p<0.05. As decided a priori as per protocol, we conducted subgroup analyses based on overall methodological quality, geography and adjustment of results. All the analyses were performed with Open-meta (30).
RESULTS
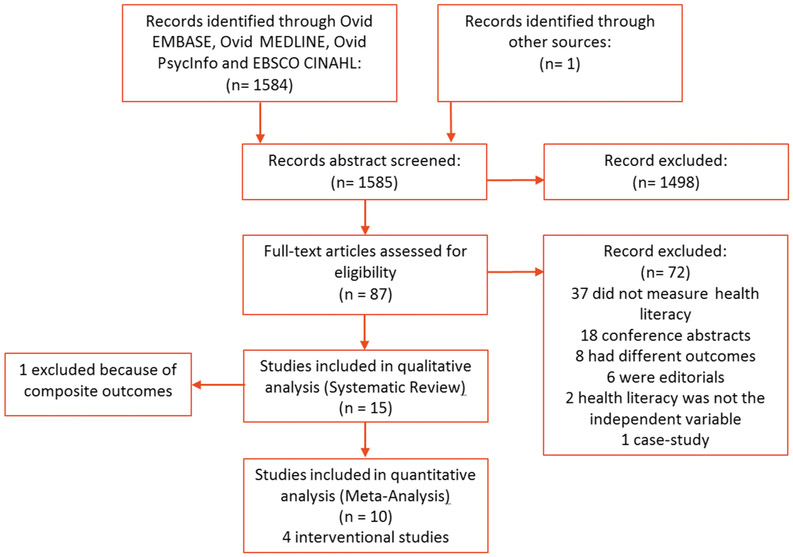
Among 1585 articles identified through our search, 87 were selected through title and abstract review. The 1498 articles that were not selected were excluded because they did not evaluate health literacy, were not among patient with HF or did not evaluate our outcomes of interest. During the full text review, 15 articles were selected and included in the systematic review, 10 of which were included in the meta-analysis (Figure 1). All the studies included in the meta-analysis are cohort studies. Overall, 8 out of 11 observational studies and 3 out of 4 interventional studies had high methodological quality (Online Tables 1 and 2).
Figure 1. Selection of studies.
Flow diagram of the literature search and study selection.
Among the 11 observational articles, 9171 patients were included, of which 2207 (24%) had inadequate or marginal health literacy. Considering only the studies conducted in the USA, 23% (1942 out of 8615) of the patients had inadequate health literacy. The results from the individual observational studies are summarized in Table 1. The quality of evidence for the outcomes of the meta-analysis following the GRADE system is included in Online Table 3. Overall, the quality of these outcomes was low to very low, mainly due to the observational nature of these studies and not because of methodological flaws. All of the studies included in the adjusted meta-analysis have adjusted their results for the main demographic (age, sex, education) and clinical confounders including comorbidities making us comfortable combining the adjusted results (Online Table 4).
Table 1.
Associations * between inadequate health literacy and outcomes among patients with HF
| Study | Health literacy evaluation tool |
Low health literacy N (%) |
Associations between inadequate health literacy and outcomes* | ||||
|---|---|---|---|---|---|---|---|
| Mortality | Hospitalizations | ED visits | Combined mortality and hospitalizations |
Combined hospitalizations and ED visits |
|||
| Murray, 2009(45) | S-TOFHLA (objective) |
61 (29) | + | no association | |||
| Dennison, 2011(46) | S-TOFHLA (objective) |
58 (61) | no association | ||||
| Peterson, 2011(9) | Brief screener (subjective) |
262 (18) | + | no association | |||
| Wu, 2013(37) | S-TOFHLA (objective) |
220 (37) | + | ||||
| McNaughton, 2013(47) | BHLS (subjective) |
258 (36) | no association | ||||
| McNaughton, 2015(10) | BHLS (subjective) |
324 (23) | + | no association | no association | ||
| Moser, 2015(24) | S-TOFHLA (objective) |
206 (36) | + | ||||
| Cox, 2016(11) | BHLS (subjective) |
89 (34) | + | ||||
| León-González, 2017(31) | SAHLSA (objective) |
258 (46) | no association | ||||
| Fabbri, 2018(8) | Brief screener (subjective) |
261 (10) | + | + | |||
| Sterling, 2018(23) | S-TOFHLA (objective) AND BHLS (subjective) |
210 (34) | no association | ||||
after adjustment for confounders listed in Online Table 4
positive association between inadequate health literacy and outcome
not adjusted for confounders
Mortality
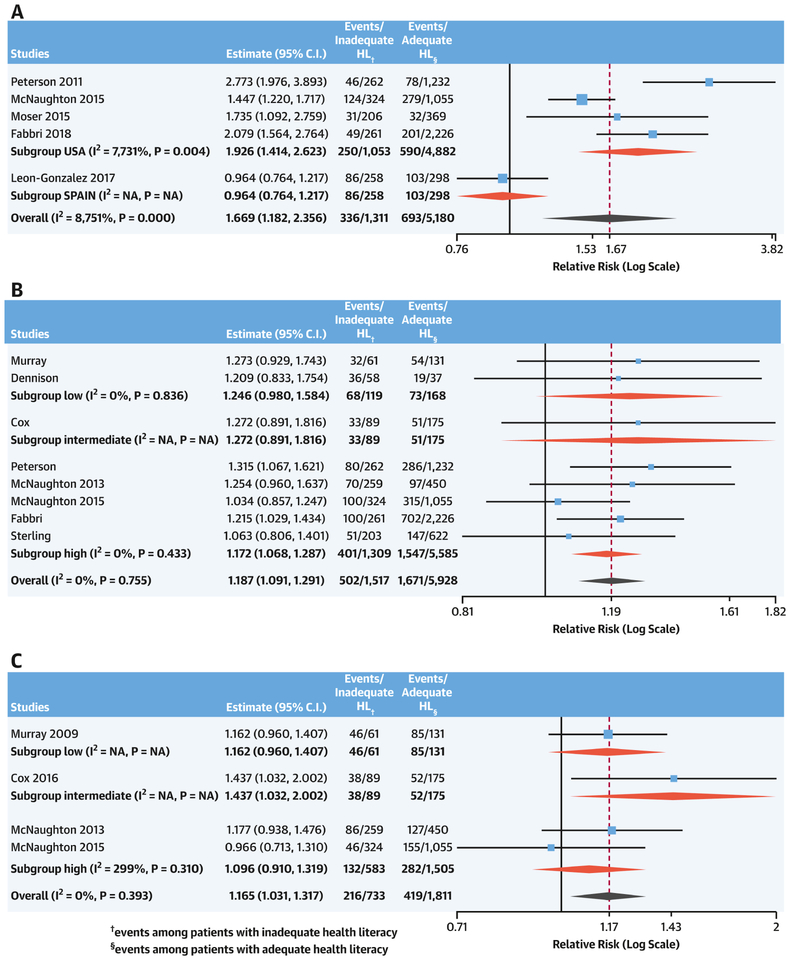
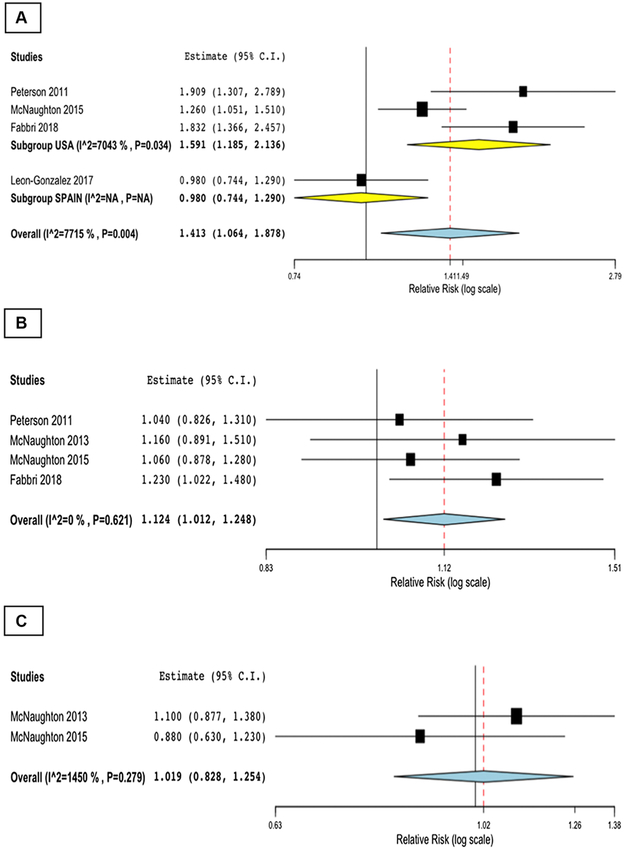
5 studies evaluated the association between inadequate health literacy and mortality, for a total of 6491 patients with HF, of which 1311 (20%) had inadequate health literacy. All studies were conducted in the USA, except for one study completed in Spain (31). Mortality was strongly associated with inadequate health literacy (Central illustration). In particular we first combined unadjusted RRs for each study, finding a 67% increased risk of mortality (I2=88%). In an attempt to explain this high heterogeneity, we conducted subgroup analysis based on the geographical area. We found that among the unadjusted results there was a 93% increased risk of death among patients with HF living in the USA (I2=77%; Central illustration). Further sensitivity analysis for subjective versus objective measurement tools was not informative (Online Figure 1A and 2). Considering the adjusted RRs from each individual study, the association with mortality decreased, albeit remaining statistically significant (RR: 1.41, 95%CI: 1.06, 1.87; I2=77%, Figure 2A). Sensitivity analysis for geographical location, reduced the heterogeneity among studies conducted in the USA (RR: 1.59, 95%CI: 1.18, 2.14; I2=70%, Figure 2A). A funnel plot for this outcome was not created, since the number of studies was limited.
Central Illustration. Meta-analysis of the unadjusted association between inadequate health literacy and outcomes.
Meta-analysis of the unadjusted association between inadequate health literacy and mortality with subgroups analysis for geographical area (A), hospitalizations (B) and ED visits (C) with subgroup analysis for overall methodological quality
Figure 2. Meta-analysis of the adjusted association between inadequate health literacy and outcomes.
Meta-analysis of the adjusted associations between inadequate health literacy and mortality with subgroups analysis for geographical area (A), hospitalizations (B) and ED visits (C)
Hospitalization
For hospitalization, we included 8 studies in the meta-analysis for a total of 7445 patients with HF, of which 1517 (20%) had inadequate health literacy. In the meta-analysis of unadjusted results, an inadequate level of health literacy was associated with a nearly 20% increased risk in hospitalization (Central illustration). Sensitivity analysis for overall methodological quality (Central illustration) as for objective versus subjective measurement tools (Online Figure 1B) was not informative. We also obtained the adjusted measurements and combined them in the meta-analysis. Combining the adjusted results, the association between hospitalization and inadequate health literacy remained statistically significant (RR: 1.12, 95%CI: 1.01, 1.25; I2=0%, Figure 2B).
ED Visits
For this outcome we included 4 studies for a total of 2544 patients with HF, of which 733 (29%) had inadequate health literacy. In the unadjusted analysis, an inadequate level of health literacy was associated with a more than 15% increased risk of ED visits (Central illustration). Sensitivity analysis for overall methodological quality (Central illustration) and sensitivity analysis for objective versus subjective measurement of health literacy (Online Figure 1C) were not informative. We were able to retrieve only two adjusted measurements for this outcome, and after combining the adjusted results the association was not statistically significant (RR= 1.02, 95% CI: 0.83, 1.25, I2=15%; Figure 2C).
Interventional Studies
We included 4 interventional studies, 3 of which were randomized and had low risk of bias (Online Table 2). The intervention by DeWalt included a one hour educational session followed by follow-up phone calls designed to teach patients how to recognize signs and symptoms of acute HF (32), while Murray’s intervention lasted 9 months during which pharmacists identified patients’ barriers to appropriate drug use and taught them how to overcome these barriers (33). In a subsequent paper, DeWalt demonstrated that a multi-session intervention is not superior to the single intervention used in his previous trial (34), while Di Palo implemented a Patient Navigator Program, which included a nurse and pharmacist assessment of the patient and education on self-management of disease and medication counseling (35). Details about inclusion, exclusion criteria and main results are provided in Table 2.
Table 2.
Summary of Interventional Studies
| Study | Nature of the study |
Type of intervention | Outcomes | Main result |
|---|---|---|---|---|
| DeWalt, 2006(32) | RCT | Education on self-care emphasizing daily weight measurement, diuretic dose selfadjustment, and symptoms’ recognition and response. | Combined death and hospitalization after 12 months. | Patients in the intervention group had a lower rate of combined death and hospitalization. This effect was larger among patients with low health literacy (IRR: 0.39; CI: 0.16-0.91). |
| Murray, 2007(48) | RCT | In person education provided by a pharmacist on for 9 months. The intervention was design to support medication management by patients with low health literacy and low resources. | Medication adherence and hospitalizations and ED visits. | The intervention group had better medication adherence and lower incidence of hospitalizations and ED visits (IRR: 0.82, 95%CI: 0.73-0.93) |
| DeWalt, 2012(34) | RCT | 40 minute in-person, literacy-sensitive training versus multisession education based on the same 40 minute in-person education and ongoing telephone-based support. | Combined death and hospitalization. | The multisession intervention did not change clinical outcomes compared to single intervention. |
| Di Palo, 2017(35) | Interventional nonrandomized study | Implementation of a Patient Navigator Program lead by a pharmacist and a nurse. | Readmission rate | Patients in the Patient Navigator Program had a readmission rate of 17.6%, while the controls had a 25.6% readmission rate. Results were not adjusted nor presented with a 95% CI. |
DISCUSSION
In our systematic review almost one patient out of four with HF has inadequate health literacy. This prevalence is not equally distributed among the studies taken into consideration. In a previous systematic review, the prevalence of inadequate health literacy ranged from 19% to 61% with an average prevalence of 39% across all studies (12), while another systematic review found 87.2% of patients with inadequate health literacy among older Latinos with HF (36). We can conclude that the percentage of patients with inadequate health literacy varies dramatically according to geography, ethnicity and socioeconomic status (14). Our findings showed that an inadequate level of health literacy is associated with increased risks in mortality and hospitalization among patients with HF.
An inadequate level of health literacy is associated with higher risk of mortality. Interestingly, the single study conducted outside of the USA from León-González et al. was the only study that did not find an association between health literacy and mortality. This could reflect several factors: the cohort of patients with HF was much older than among other studies and the study was conducted in Spain, in an inherently different care delivery system, underscoring the need for further studies to be conducted outside the USA. Mortality had high statistical heterogeneity, possibly due to different populations of the study.
An inadequate level of health literacy was also associated with increased risk of hospitalizations and ED visits in the unadjusted model. Only two articles found a statistically significant association with hospitalizations even though only one of them adjusted for confounders. No association was found for ED visits after adjustment. Cox et al. (11) found a statistically significant association after 30 days when combining ED visits and hospitalizations, while composite mortality and hospitalizations for all causes (37) and composite mortality and hospitalizations for HF (24) were found to be associated with inadequate health literacy.
This systematic review also includes interventional studies that aimed to improve mortality, hospitalizations or ED visits. Among the four articles included, DeWalt and Murray (32,33) reported significant results. Although randomized controlled trials (RCTs) bring the highest level of evidence, these studies were not included in the meta-analysis, because the nature of the intervention was too different to allow us to comfortably combine these results.
The mechanism that links health literacy and outcomes is complex and likely involves other social determinants of health (38). Some studies mentioned that these patients are less likely to access healthcare services, and when they do, they are less likely to engage in an effective physician-patient communication (6,38). This could be due to several reasons. For example, patients with inadequate health literacy might be less likely to seek clarifications (39), possibly due to feelings of shame of their literacy status (40,41). These missed opportunities to seek clarifications are even more critical when considering that educational materials provided often exceed the reading ability of a patient with inadequate health literacy (7). All of these barriers may explain why these patients are less likely to engage in efficient self-care management (4,5,42) and ultimately more likely to experience adverse outcomes.
Clinical Implications
Given the staggering mortality and hospitalization burden in HF, any opportunity to improve outcomes is essential to pursue underscoring the crucial importance of health literacy among patients with HF. An inadequate level of health literacy constitutes a barrier to the achievement of adequate self-care in HF (4). This is even more relevant considering a recent report which highlights how self-management programs effectively reduce readmissions among patients with HF (43) and tailored interventions for inadequate health literacy have been proven to reduce adverse outcomes (32,33). Therefore, the evaluation of health literacy could lead to identification of patients who can benefit the most from these interventions and ultimately improve outcomes.
Finally, as previous studies have reported (44), inadequate health literacy is associated with lower quality of life, which is extremely important. Further studies on this association are warranted.
Limitations and Strengths
We were unable to statistically evaluate publication bias because of the limited number of studies for each outcome. To mitigate this concern, we searched the grey literature. Moreover, we were not able to retrieve the adjusted measurement for all the studies. In addition, studies included in this review evaluated health literacy with different tools, which could limit comparability. However, our results did not change in the sensitivity analysis conducted for objective versus subjective health literacy measurements. This is important since subjective and objective health literacy are related, but can evaluate different concepts (17). Finally, it was not always clear if the assessment of health literacy took place in the outpatient or inpatient setting, which may have influenced the measurement.
This study has several strengths. To the best of our knowledge, this is the first systematic review to quantify the magnitude of the association between inadequate health literacy and hospitalizations and ED visits. Moreover, we were able to combine the adjusted results giving a more accurate measure of these associations. The study search was extensive and we examined these associations with subgroup analyses to explain the high heterogeneity. We contacted the authors when we could not to retrieve important data. We conducted extensive sensitivity and subgroup analysis in this review. Finally, the majority of our studies were conducted in different parts of the USA, therefore we believe that within the USA this data is highly generalizable.
CONCLUSION
Among patients with HF, an inadequate level of health literacy is frequent and associated with an increased risk of deaths and hospitalizations. These findings have important clinical and public health implications and support the deployment of interventions to improve health literacy in order to improve outcomes among patients living with HF.
Supplementary Material
PERSPECTIVES.
Competency in Patient care: It has been shown that patients with better health literacy, have reduced risk for outcomes like mortality and hospitalizations, although evidence in the literature is sometimes not consistent.
Translational Outlook 1: An inadequate level of health literacy is associated with higher risk for mortality and hospitalizations in patients with heart failure. Measuring health literacy is easy and not time-consuming, thus, screening for health literacy should be implemented in the clinical practice in order to identify those patients who are at increased risk for adverse outcomes.
Translational Outlook 2: Interventions to improve adverse outcomes among patients with inadequate health literacy have been proven to be effective. Adoption of such interventions should be implemented in the clinical practice.
Acknowledgments
Funding Sources: This publication was made possible by CTSA Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and the National Heart, Lung and Blood Institute (R01 HL120859). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
ABBREVIATIONS
- ED
emergency department
- GRADE
grading of recommendations assessment development and evaluation
- HF
heart failure
Footnotes
Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report from the American Heart Association. Circulation 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. JAMA 2004;292:344–50. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay SM, Redfield MM, Weston SA, et al. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol 2009;54:1695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsuoka S, Tsuchihashi-Makaya M, Kayane T, et al. Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Educ Couns 2016;99:1026–32. [DOI] [PubMed] [Google Scholar]
- 5.Mixon AS, Myers AP, Leak CL, et al. Characteristics associated with postdischarge medication errors. Mayo Clin Proc 2014;89:1042–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav 2007;31 Suppl 1:S19–26. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion 2004. [PubMed] [Google Scholar]
- 8.Fabbri M, Yost K, Finney Rutten LJ, et al. Health literacy and outcomes in patients with heart failure: A prospective community study. Mayo Clin Proc 2018;93:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA 2011;305:1695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cox SR, Liebl MG, McComb MN, et al. Association between health literacy and 30-day healthcare use after hospital discharge in the heart failure population. Res Social Adm Pharm 2017;13:754–8. [DOI] [PubMed] [Google Scholar]
- 12.Cajita MI, Cajita TR, Han HR. Health literacy and heart failure: A systematic review. J Cardiovasc Nurs 2016;31:121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu XB, Ayatollahi Y, Yamashita T, et al. Health literacy and mortality in patients with heart failure: A systematic review and meta-analysis. Res Gerontol Nurs 2018:1–10. [DOI] [PubMed] [Google Scholar]
- 14.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med 2005;20:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9, W64. [DOI] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 17.Waters EA, Biddle C, Kaphingst KA, et al. Examining the interrelations among objective and subjective health literacy and numeracy and their associations with health knowledge. J Gen Intern Med 2018;33:1945–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 19.Lee SY, Bender DE, Ruiz RE, Cho YI. Development of an easy-to-use Spanish health literacy test. Health Serv Res 2006;41:1392–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sand-Jecklin K, Coyle S. Efficiently assessing patient health literacy: the BHLS instrument. Clin Nurs Res 2014;23:581–600. [DOI] [PubMed] [Google Scholar]
- 21.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23:561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–94. [PubMed] [Google Scholar]
- 23.Sterling MR, Safford MM, Goggins K, et al. Numeracy, health literacy, cognition, and 30-day readmissions among patients with heart failure. J Hosp Med 2018;13:145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail 2015;21:612–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stang A Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- 26.Higgins J, Altman D, Sterne JAC. Assessing risk of bias in included studies Cochrane Handbook for Systematic Reviews of Interventions. Hoboken: 2008;NJ: John Wiley & Sons, Ltd. [Google Scholar]
- 27.Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res 1993;2:121–45. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JPT GSe. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011. [Google Scholar]
- 29.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- 30.Wallace BC DI, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. Wiley Interdiscip Rev Comput; 2012;49:1–15. [Google Scholar]
- 31.Leon-Gonzalez R, Garcia-Esquinas E, Paredes-Galan E, et al. Health literacy and health outcomes in very old patients with heart failure. Rev Esp Cardiol (Engl Ed) 2018;71:178–84. [DOI] [PubMed] [Google Scholar]
- 32.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170]. BMC Health Serv Res 2006;6:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murray MD, Young J, Hoke S, et al. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med 2007;146:714–25. [DOI] [PubMed] [Google Scholar]
- 34.DeWalt DA, Schillinger D, Ruo B, et al. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation 2012;125:2854–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Palo KE, Patel K, Assafin M, Pina IL. Implementation of a patient navigator program to reduce 30-day heart failure readmission rate. Prog Cardiovasc Dis 2017;60:259–66. [DOI] [PubMed] [Google Scholar]
- 36.Delgado JM, Ruppar TM. Health literacy in older latinos with heart failure: A systematic review. J Cardiovasc Nurs 2017;32:125–34. [DOI] [PubMed] [Google Scholar]
- 37.Wu JR, Holmes GM, DeWalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med 2013;28:1174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Magnani JW, Mujahid MS, Aronow HD, et al. Health literacy and cardiovascular disease: Fundamental relevance to primary and secondary prevention: A scientific statement from the american heart association. Circulation 2018;138:e48–e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. J Gen Intern Med 2007;22:782–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baker DW, Parker RM, Williams MV, et al. The health care experience of patients with low literacy. Arch Fam Med 1996;5:329–34. [DOI] [PubMed] [Google Scholar]
- 41.Farrell TW, Chandran R, Gramling R. Understanding the role of shame in the clinical assessment of health literacy. Fam Med 2008;40:235–6. [PubMed] [Google Scholar]
- 42.Meyers AG, Salanitro A, Wallston KA, et al. Determinants of health after hospital discharge: rationale and design of the Vanderbilt Inpatient Cohort Study (VICS). BMC Health Serv Res 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Macabasco-O'Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med 2011;26:979–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther 2009;85:651–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dennison CR, McEntee ML, Samuel L, et al. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs 2011;26:359–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McNaughton CD, Collins SP, Kripalani S, et al. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail 2013;6:40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murray MD. Medication instruction by pharmacists: making good on an offer. N C Med J 2007;68:343–5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.