Abstract
Background
Current methods to identify people with psychosis risk involve administration of specialized tools such as the Structured Interview for Psychosis-Risk Syndromes (SIPS), but these methods have not been widely adopted. Validation of a more multipurpose assessment tool—such as the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS)—may increase the scope of identification efforts.
Methods
We assessed the correspondence between SIPS-determined clinical high risk/early psychosis (CHR/early psychosis) status and K-SADS psychosis screen (child and parent reports and their combination) in a sample of 147 help-seeking individuals aged 12–25. Detailed classification results are reported.
Results
Both the child and parent interviews on the K-SADS psychosis screen were strongly predictive of CHR/early psychosis status, although parent reports contributed no significant additional information beyond child reports. Across informants, the presence of either subthreshold hallucinations or subthreshold delusions was highly suggestive of CHR/early psychosis status as determined by SIPS interview (78% (child) and 74% (parent) accuracy).
Conclusions
Subthreshold scores on the two-item K-SADS psychosis screen may be good indicators of the presence or absence of early signs of psychosis. The option of using a non-specialized assessment such as the K-SADS as a staged approach to assess for CHR/early psychosis status could increase rates of early psychosis screening and treatment.
Keywords: Clinical high-risk, ultrahigh risk, early psychosis, psychosis, schizophrenia
Introduction
Over the past three decades, a growing body of research suggests that early intervention can reduce symptom severity of psychotic disorders, and forestall or possibly in some cases prevent psychosis. This has led to substantial research focused on the assessment of individuals in early psychosis (i.e. with recent-onset, diagnosable psychotic disorder) or at “Clinical High-Risk” (CHR) for psychosis (Schiffman, 2018; Stafford et al., 2015). CHR states are characterized by the presence of attenuated positive symptoms of psychosis and functional impairment, and are associated with an approximately 25% rate of transition to formal psychotic disorder within 3 years (Fusar et al., 2015). Screening for subthreshold symptoms among individuals seeking mental healthcare may offer information relevant to early identification of early psychosis and could be instrumental for early intervention.
Currently, the North American “gold standard” for assessing subthreshold psychotic symptoms is a clinician-administered semi-structured interview known as the Structured Interview for Psychosis-Risk Syndromes (SIPS; Miller et al., 2003). The training requirements and time involved to administer the SIPS, however, make widespread dissemination of this tool in community care challenging. An estimated 95% of individuals in early phases of psychosis go undetected (Fusar-Poli, 2018), suggesting that additional tools to identify those in the early phases of illness might be useful. Given the potential impact of psychosis on quality of life and the benefits of early intervention, it may be beneficial to consider alternative, more widely implementable strategies for identifying people at early stages of psychosis in clinical practice.
Community assessment and identification of people at-risk or in the early phases of psychosis would likely be more common if it could be done effectively using diagnostic instruments less specialized than those tailored specifically to detecting early psychosis risk syndromes. One promising candidate measure is the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) for School-Age Children (Kaufman et al., 1997), as this semi-structured interview is used as an assessment for a broad range of diagnoses given in the Diagnostic and Statistical Manual (DSM) of Mental Disorders, while containing psychosis-specific questions (First, Gibbon, Hilsenroth, & Segal, 2004). The K-SADS is generally shorter than the SIPS, taking roughly 35–75 minutes to administer depending upon the range and severity of psychopathology (Kaufman et al., 1997), compared to the SIPS interview’s 45–120 minute duration (PRIME Psychosis Prodrome Research Clinic, 2019). Thus, the K-SADS is generally briefer or approximately the same duration as the SIPS, and yet provides the administrator with a characterization of a fuller range of psychopathology, rather than a single syndrome. The emphasis on comprehensiveness within the K-SADS likely makes it more attractive outside of specialty psychosis clinics.
The standard K-SADS protocol involves administration of a psychosis screen consisting of two 3-point items that, respectively, assess for the dimensional severity of hallucinations and delusions (children and parents serve as separate informants for the interview). Although only the highest rating (“threshold”) on either screening item triggers further diagnostic queries to determine the presence of a psychotic disorder, the interviewer is instructed to note the presence of hallucinations or delusions of subthreshold severity regardless of final diagnostic determination. Thus, the K-SADS psychosis screen may contain information sensitive to the presence of questionable and/or subthreshold psychosis risk states. Despite these potential advantages, previous research has not tested whether the K-SADS psychosis screen can reliably determine psychosis risk or early psychosis.
In an effort to evaluate the potential for a more practical and widespread evaluation of early psychosis, this study assessed the utility of the K-SADS psychosis screen as an indicator of CHR and CHR/early psychosis status in a sample of help-seeking adolescents and young adults. Specifically, we assessed the ability of the K-SADS psychosis screen parent and child interviews to predict CHR and CHR/early psychosis status as determined by the “gold standard” SIPS interview. To put the measured performance of the K-SADS screens in context, we also assess the ability of a more commonly used early psychosis screening measure called the Prodromal questionnaire-brief (PQ-B) to predict CHR and CHR/early psychosis status in the same study sample.
Method
Participants
This study was conducted through the Youth FIRST research program/Strive for Wellness clinic affiliated with the University of Maryland, Baltimore County (UMBC) and the University of Maryland School of Medicine. To be eligible for the study, participants must have been between the ages of 12 and 25, receiving mental health services, and willing and able to provide informed consent. If under 18 years old, a parent or legal guardian was present and willing to provide consent and the adolescent provided written assent. Participant characteristics (N = 147) are given in Table 1. Note that, although eligibility was open to all help-seeking youth, the number of participants with psychotic disorders is high relative to most clinical samples, which can be explained in part by the fact that referral sources were not blind to the fact that the study concerned the psychosis spectrum.
Table 1.
Sample characteristics.
| N | % | |
|---|---|---|
| Gender | ||
| Female | 91 | 62 |
| Male | 56 | 38 |
| Race | ||
| Black | 63 | 43 |
| White | 52 | 35 |
| Multiracial | 25 | 17 |
| Native American | 2 | 1 |
| Asian | 1 | 1 |
| Did not endorse | 4 | 3 |
| Diagnosis | ||
| MDD | 63 | 43 |
| Psychotic disorder | 23 | 16 |
| ADHD | 21 | 14 |
| PTSD | 9 | 6 |
| Bipolar | 7 | 5 |
| Anxiety | 6 | 4 |
| Oppositional | 4 | 3 |
| Adjustment | 3 | 2 |
| No diagnosable disorder | 3 | 2 |
| Other | 8 | 5 |
| Age | ||
| Median (SD) | 15 (2.8) |
MDD: major depressive disorder; ADHD: attention deficit hyperactivity disorder; PTSD: posttraumatic stress disorder.
Procedure
Procedures were approved by Institutional Review Boards at UMBC, the University of Maryland School of Medicine, and the Maryland Department of Health IRB. Prior to completion of study procedures, all participants received an overview of the study and consented to their involvement before filling out demographic questionnaires and participating in the two semi-structured interviews.
Participants were assessed with the K-SADS-PL (present and lifetime) followed by the SIPS. Clinicians were trained in administration by experienced clinicians and the principal investigators (PIs). Reliability training included observing and co-rating K-SADS-PL interviews conducted by independent experienced staff and at least one PI, followed by independent administrations observed by the experienced staff, with clinicians considered reliable after reaching perfect diagnostic agreement on at least three interviews during the co-rating process and obtaining approval from the PIs. Team clinical formulation review was conducted after each K-SADS interview to ensure agreement across clinicians and the PIs. All SIPS administrators underwent a 2-day training workshop led by one of the original authors of the SIPS (Barbara C. Walsh) or by a SIPS trainer certified by Dr Walsh (Jason Schiffman). In addition, study staff co-rated audio-recorded and live interviews, and were observed administrating the SIPS by experienced raters. Raters were approved to independently administer SIPS interviews only when reliability coefficients were .80 or greater. All participant interviews were reviewed weekly via individual clinical consultation conferences with experts in the assessment of early psychosis.
Measures
K-SADS. The K-SADS-PL is a clinician administered semi-structured interview used for diagnosing common disorders found in the DSM (K-SADS-PL; Kaufman et al., 1997). Children and parents serve as separate informants for the interview. The screening interview (including the psychosis screen) is administered first; if threshold symptoms are detected during the screen, in-depth supplements for each category of diagnosis (e.g. psychotic disorders) are administered. Parents and children were interviewed separately.
The K-SADS psychosis screen consists of two items, one for hallucinations and one for delusions. A score of 0 indicates no information (treated as missing data for these analyses), a score of 1 indicates that the symptom is not present, a score of 2 indicates subthreshold symptoms, or that symptoms are suspected or likely but not confirmed, and a score of 3 indicates the presence of threshold level symptoms.
SIPS
The SIPS is a semi-structured, clinician-administered interview that measures the presence and severity of symptoms associated with early psychosis (Miller et al., 2003). It is among the most widely used measures of clinical high-risk for psychosis, representing a “gold standard” for assessment of psychosis-risk (Fusar-Poli et al., 2016). The presence or absence of three CHR syndromes (attenuated psychosis syndrome, brief intermittent psychosis syndrome, and genetic risk and deterioration syndrome), as well as full threshold psychosis is determined from the SIPS interview protocol. Participants were designated as “Clinical High-Risk” if they were diagnosed with any risk syndrome or schizotypal personality disorder, and designated as early psychosis if they already met full criteria for a psychotic disorder. The within-lab ICC for SIPS positive symptoms was .82, and diagnostic agreement was κ = 1 (Millman et al., 2018).
Prodromal questionnaire-brief
To provide some context for the performance of the K-SADS screens, child responses to the PQ-B were also tested. The PQ-B is a commonly used 21 item self-report scale used to measure the presence and severity of attenuated positive psychosis symptoms (Loewy et al., 2011). Participants indicate presence or absence of attenuated psychosis symptoms through yes/no responses. In the event of a positive endorsement, participants are asked to rate the extent to which the endorsed symptoms causes concern, fright, or impairment, ranging from a score of one (strongly disagree) to a five (strongly agree). Distress ratings are added together to yield a total score.
Analysis
For the purposes of analyses, K-SADS screen score of 0 (“no information”) were considered missing data. (Note that missing data was excluded from all analyses pairwise.) Otherwise, scoring was carried out according to the standard protocol, with 1 indicating “not present,” 2 indicating “subthreshold,” and 3 indicating “threshold” symptoms. Scores on the hallucinations and delusions items were summed to yield a total psychosis screen score for both the parent and child separately.
To evaluate how the K-SADS psychosis screen predicted CHR status and CHR/early psychosis status, logistic regressions were used with Parent and Child K-SADS screen scores as predictors of CHR (with early psychosis excluded from the regression) and on CHR/early psychosis status. We first ran simple logistic regressions with child and parent interview scores entered separately. We then included both informants in the same model to test whether information from either interview could add useful information for the purposes of predicting CHR or CHR/early psychosis status.
To provide some context for the performance of the K-SADS screens, we also ran logistic regressions to test the ability of the PQ-B to predict early psychosis and CHR status, and report correlations between the K-SADS and PQ-B screens.
Results
Out of 147 participants, 52 were classified by the SIPS as meeting criteria for CHR and 23 for early psychosis, resulting in 75 CHR/early psychosis participants. The remaining 72 were classified as help-seeking controls. In all, 27 participants were missing parent psychosis screens and 11 participants were missing child screens, while 28 participants were missing PQ-B total scores.
Child K-SADS-PL psychosis screen scores were statistically significant predictors of CHR (p < .001) and CHR/early psychosis status (p < .001). When entered into a separate regression, parent screen scores also significantly predicted CHR (p < .001) and CHR/early psychosis status (p < .001). When child and parent screens scores were both entered into the same regression, parent screen no longer significantly predicted CHR (p = .22) or CHR/early psychosis status (p = .13), whereas child screen scores continued to significantly predict CHR (p < .001) or CHR/early psychosis status (p < .001). See Tables 2 and 3 for the full table of regression parameter estimates.
Table 2.
Logistic regressions predicting early psychosis (help-seeking control versus CHR or psychotic disorder).
| Regression | R2 | Predicting early psychosis (CHR or Psychotic Dx) | ||
|---|---|---|---|---|
| 1 | .36 | B (95% CI) | SE B | eB |
| Child K-SADS psychosis screen | 1.337*** (0.91–1.85) | 0.239 | 3.81 (2.5–6.4) | |
| 2 | .24 | |||
| Parent K-SADS psychosis screen | 1.201*** (0.69–1.84) | 0.291 | 3.32 (2–6.3) | |
| 3 | .35 | |||
| Child K-SADS psychosis screen | 1.085*** (0.54–1.71) | 0.354 | 2.96 (1.7–5.6) | |
| Parent K-SADS psychosis screen | 0.529 (−0.12–1.28) | 0.297 | 1.69 (0.9–3.6) | |
CHR: clinical high-risk; CI: confidence interval; K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia.
p < .05.
p < .01.
p < .001.
Table 3.
Logistic regressions predicting CHR (help-seeking control vs CHR, excluding people with psychotic disorders from regressions).
| Regression | R2 | Predicting CHR (excluding Psychotic Dx) | ||
|---|---|---|---|---|
| 1 | .34 | B (95% CI) | SE B | eB |
| Child K-SADS psychosis screen | 1.35*** (0.88–1.92) | 0.26 | 3.86 (2.4–6.8) | |
| 2 | .17 | |||
| Parent K-SADS psychosis screen | 1.05*** (0.5–1.72) | 0.31 | 2.85 (1.7–5.6) | |
| 3 | .33 | |||
| Child K-SADS psychosis screen | 1.15*** (0.57–1.22) | 0.32 | 3.16 (1.8–6.2) | |
| Parent K-SADS psychosis screen | 0.45 (−0.24–1.22) | 0.37 | 1.6 (0.8–3.4) | |
CHR: clinical high-risk; CI: confidence interval; SE: standard error; K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia.
p < .05.
p < .01.
p < .001.
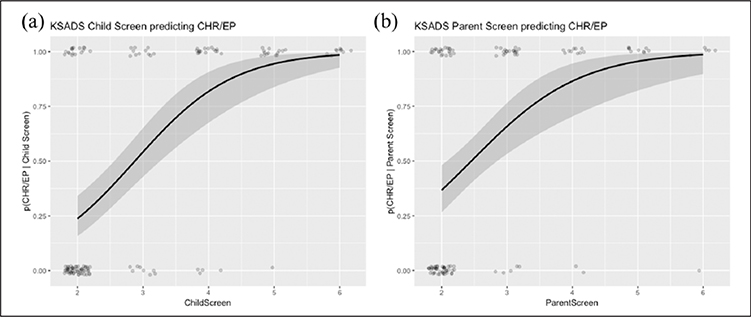
Given that the child screen appeared to drive the ability of the K-SADS screen to predict psychosis risk, we further evaluated the predictive characteristics of the child screen as a sole predictor of CHR/early psychosis status. Figure 1(a) plots child screen scores against CHR/early psychosis status along with the regression lines from the fitted models. A total score of 3 on the child screen—which corresponds to the presence of either subthreshold hallucinations or the presence of subthreshold delusion—indicates that the child has a greater than 50% chance of being CHR/early psychosis.
Figure 1. K-SADS child and parent psychosis screens predicting CHR/EP status.
Points give observed values and lines give the relationship between the predictor and outcome according to logistic regression. For each K-SADS psychosis screen (child or parent), a score of three or more corresponds to a greater than 50% chance of CHR/EP diagnosis. This score corresponds to a “subthreshold” rating on either the hallucinations or delusions screening items.
Tables 4 and 5 give more detailed classification characteristics for the child screen as a predictor of CHR/early psychosis status. Using the presence of either subthreshold hallucinations or subthreshold delusions on the K-SADS psychosis screen as an indicator of CHR/early psychosis status, the child screen achieved 78% accuracy at predicting psychosis risk. Sensitivity (81%) was slightly higher than specificity (75%).
Table 4.
Classification results using a cutoff rating of subthreshold hallucinations or delusions on the K-SADS child screen to predict CHR/EP.
| Prediction based on K-SADS Child screen |
|||
|---|---|---|---|
| Not CHR/EP | CHR/EP | ||
| CHR/EP status determined by SIPS | Not CHR/EP CHR/EP |
56 17 |
13 50 |
| Sensitivity (%) | 81 | ||
| Specificity (%) | 75 | ||
| Accuracy (%) | 78 | ||
| Pos. Predictive Value (%) | 77 | ||
| Neg. Predictive Value (%) | 79 | ||
K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia; CHR: clinical high-risk; EP: early psychosis; SIPS: structured interview for psychosis-risk syndromes.
Table 5.
Classification results using a cutoff rating of subthreshold hallucinations or delusions on the K-SADS parent screen to predict CHR/EP.
| Prediction using K-SADS parent screen |
|||
|---|---|---|---|
| Not CHR/EP | CHR/EP | ||
| CHR/EP status determined by SIPS | Not CHR/EP CHR/EP |
46 23 |
8 43 |
| Sensitivity (%) | 85 | ||
| Specificity (%) | 65 | ||
| Accuracy (%) | 74 | ||
| Pos. Predictive Value (%) | 67 | ||
| Neg. Predictive Value (%) | 84 | ||
K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia; CHR: clinical high-risk; EP: early psychosis; SIPS: structured interview for psychosis-risk syndromes.
Although child report appears to account for the most variance, parent report may have clinical utility in situations where the child is unavailable for interview or difficult to engage. We present classification characteristics for the Parent screen in Table 4 (logistic regression plotted in Figure 1(b)). The parent screen achieves reasonable results with 74% accuracy.
PQ-B
To better contextualize the above findings, we compared the K-SADS child and parent screens with a commonly used early psychosis screening measure called the PQ-B. The PQ-B correlated more strongly with the K-SADS child than the K-SADS parent screen (see Tables 6 and 7). Although the PQ-B significantly predicted CHR (p < .001) and CHR/early psychosis (p < .001) status, it accounted for much less variance in the outcome measure than either the K-SADS parent or child screens as measured by R2 (cf. Table 2 and 3).
Table 6.
Correlation between child screen, parent screen, and PQ-B.
PQ-B: prodromal questionnaire-brief.
p < .05.
p < .01.
p < .001.
Table 7.
Logistic regressions with PQ-B predicting CHR status (excluding psychotic disorder) and early psychosis (CHR or psychotic disorder).
| Regression | R2 | Predicting CHR (excluding Psychotic Dx) | ||
|---|---|---|---|---|
| 1 | .17 | B (95% CI) | SE B | eB |
| PQ-B predicting CHR status (excluding participants with psychotic disorder) | 0.039*** (0.02–0.06) | 0.01 | 1.04 (1.02–1.06) | |
| 2 | .18 | |||
| PQ-B predicting early psychosis (CHR or psychotic disorder) | 0.04*** (0.02–0.06) | 0.01 | 1.04 (1.02–1.06) |
PQ-B: prodromal questionnaire-brief; CHR: clinical high-risk; CI: confidence interval; SE: standard error.
p < .05.
p < .01.
p < .001.
Discussion
As clinical high-risk and early psychosis states become generally accepted as a promising opportunity for both indicated and preventive intervention, there is a growing need to validate (or independently develop) practical tools to allow clinicians to identify individuals who are in early stages of psychosis in applied clinical settings. One barrier to accurate assessment is that the current gold standard for assessing CHR/early psychosis status (the SIPS in North America) requires specialized training. A recent publishing of certified SIPS interviewers (“Structured Interview For Psychosis-Risk Syndromes,” 2018) reveals a dearth of trained clinicians, and only three certified trainers in the United States. In addition, the SIPS is relatively time-consuming, especially given that it provides clinicians with information about just one category of mental health concerns among many. (The SIPS assessment for positive symptoms alone requires the clinician to administer 48 prompts.) The present results suggest that the K-SADS, a non-specialty diagnostic interview, may be used as a screening for further specialty psychosis risk evaluation such as afforded by the SIPS.
Findings from this study suggest that subthreshold scores on the hallucinations and delusions items from the K-SADS psychosis screen child and parent interview are good indicators of CHR/early psychosis status, with 78% and 74% (respectively) accuracy at identifying people at CHR/early psychosis. The K-SADS psychosis screen interview assesses for a broader range of mental health conditions than psychosis alone, is available in more languages, and is more widely used relative to specialized interviews. With respect to early psychosis screening, the K-SADS may serve as a strong pre-screen complement to the SIPS that could trigger a more in-depth evaluation. Although no substitute for the depth of psychosis risk probes afforded by the SIPS, for many clinicians without access to specialized early psychosis assessors, the K-SADS screening questions along with the more in-depth psychosis supplement probes may in some cases be a reasonable alternative to the SIPS depending on their needs.
When clinicians deliver the K-SADS Psychosis screen, subthreshold scores (in contrast to a full threshold screen score of 3) do not automatically trigger further evaluation for psychosis spectrum conditions within the K-SADS and subsequently do not lead to a diagnosis of a psychotic disorder. The present results suggest that subthreshold psychotic symptoms identified during the screen should in many cases warrant increased vigilance on the part of the clinician, as this level of endorsement can indicate risk, if not diagnosable psychosis. Available estimates suggest that approximately 25% of young people who are at CHR convert to psychotic disorder at a later date (Fusar-Poli et al., 2012), and mental health interventions (McGorry et al., 2013) may forestall illness progression and increase psychosocial functioning more generally for those who are in early phases of illness (Kane et al., 2015). In addition, a large portion of those who do not convert to psychosis still struggle with a range of mental health concerns (Thompson et al., 2015). Therefore, even if a positive K-SADS psychosis screen does not lead to a full psychotic disorder diagnosis, the screening portion—both child and parent interview version—may still function as an important guide for clinical treatment and assessment.
It is noteworthy that the parent interview did not explain significant additional variance in CHR/early psychosis status over and above the child interview. The SIPS interview is not delivered to parents, and so the better concordance between the SIPS and the K-SADS Child screen is logical. In addition, given that the questions were identical in both interviews, and that they probe for very specific aspects of psychosis, it is not very surprising that the parent screens explained little additional variance. Nevertheless, although the child interview was more predictive than the parent screen, in the context of this study, both child and parent interviews were strong proxies for the SIPS.
A notable limitation was our relatively small sample size. It will be important to replicate the current findings in a larger sample to ensure that the results hold and generalize. We are encouraged, however, by the fact that logistic regression yielded the same cut point for CHR/early psychosis status (viz., one “subthreshold” rating for either hallucinations or delusions). In addition, our interviewers were not blinded across interviews as the K-SADS was administered first, followed by the SIPS, by the same interviewer. Although both interviews are semi-structured to promote objectivity and reliability, it is likely that responses from the K-SADS influenced the interviewer’s approach to the SIPS. In addition, the training that raters received to administer the SIPS could have made them more sensitive to psychosis-related questions within the K-SADS. These factors could have made the rating practices of study clinicians less representative of clinicians in the community, leading to the potential for a reduction in the size of the effect when transporting outside specialty settings. Future studies where independent interviewers conduct the K-SADS and the SIPS would yield improved confidence in the findings related to the confluence of these two instruments. It is also important to note that the K-SADS-PL is usually used in individuals < 18 years old, whereas we used the interview for young people up to age 25 to maintain consistency. Other groups have similarly used the K-SADS to determine DSM diagnoses in young adults up to age 25 (Tang et al., 2014; Weissman, 1990) and in young adults at CHR specifically (Cornblatt et al., 2015), but in using this strategy it is possible that we may have sacrificed validity to some extent. Finally, all of the statistical tests reported in this study must be understood against the backdrop of the uncertainty in the SIPS assessment and the CHR construct: the majority of people who are identified as CHR by the SIPS do not go on to develop a psychotic disorder (Cannon et al., 2008), so any screening tool that imperfectly predicts SIPS-determined CHR status can be expected to have an even less perfect ability to track conversion to psychotic disorder. With this in mind, it seems clinically prudent to refer people who screen high on the K-SADS for additional evaluation vis-a-vis the SIPS.
Assessment protocols such as the SIPS are well suited for research settings where accuracy and depth are paramount, but the same protocols are less practical in community settings where psychosis is just one of a range of symptom dimensions and limited time and resources are available to assess for any given condition. At the same time, the vast majority of people with CHR/early psychosis are never identified, suggesting a strong need for broader identification strategies. Findings from this study suggest that the K-SADS psychosis screen, both the child and parent versions, can provide a reasonable and convenient opportunity for clinicians to identify need for further psychosis-risk evaluation within the context of a broader mental health evaluation.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Mental Health (grants R01MH112612 and R34MH110506 to J.S.) and the Maryland Department of Health and Mental Hygiene, Behavioral Health Administration through the Center for Excellence on Early Intervention for Serious Mental Illness (OPASS#14–13717G/M00B4400241to J.S.).
Author biographies
Thomas Tsuji, PhD, is a Staff Psychologist at the Perry Point VA Medical Center in a psychosocial residential rehabilitation treatment program for serious mental illness. He completed his internship at the Baltimore VA Consortium. He has worked with people with serious mental illness through all stages of life (child, adolescent, adult) and is interested in improving assessment, treatment, and their quality of life.
Peter Phalen, PsyD, is a postdoctoral fellow at the University of Maryland School of Medicine and the VA
Capitol Health Care Network (VISN 5) in Baltimore, Maryland, where he is both a researcher and a clinician.
He is especially passionate about improving the culture of clinical care for people who have experiences that are believed to be psychotic, and for people who are chronically suicidal.
Pamela Rakhshan Rouhakhtar, MA, is a graduate student in the Clinical Psychology program at the University of Maryland, Baltimore County. Her clinical training has focused on serving youth and their families experiencing early psychosis. Pamela’s research includes work evaluating psychometric properties and cultural/contextual sensitivity of psychosis and psychosis-risk assessment.
Zachary Millman, MA, is a PhD candidate at the University of Maryland, Baltimore County, and a doctoral intern in clinical psychology at McLean Hospital / Harvard Medical School. His clinical and research interests involve early identification and intervention in serious mental illness.
Kristin Bussell, PhD, CRNP is a Family Psychiatric Nurse Practitioner who specializes in child & adolescent psychiatry. She provides clinical care in a private practice and is a researcher on several studies focused on youth treated with antipsychotic medications and those at risk for psychosis with a focus on healthy lifestyle education and interventions.
Elizabeth Thompson, PhD, is a Clinical Psychologist who specializes in adolescent and young adult mental health. After completing her doctoral degree at University of Maryland, Baltimore County, she joined Warren Alpert Medical School for residency and now a postdoctoral fellowship in child mental health research. Her research interests focus on understanding risk factors for psychosis, developing and promoting engagement in specialized services for early psychosis, and reducing mental health stigma.
Caroline Demro earned her PhD at the University of Maryland, Baltimore County and completed her clinical internship at Harvard Medical School/Beth Israel Deaconess Medical Center. She is currently in Minnesota completing a research postdoc and continues to study mechanisms involved in the development of psychosis.
Caroline Roemer, MS, is a Research Coordinator in Jason Schiffman’s YouthFirst lab at University of Maryland, Baltimore County. She received her master’s degree from King’s College London in Early Intervention in Psychosis. She is interested in individualized treatment for individuals at risk for psychosis.
Gloria Reeves, MD, is a Child and Adolescent Psychiatrist and Associate Professor at University of Maryland School of Medicine. Reeves is a Clinical Researcher who conducts “Family-Centered” research on medication safety issues, obesity-related health concerns, and parent peer support strategies.
Jason Schiffman is Professor of Psychology and Director of Clinical Training at the University of Maryland, Baltimore County. Graduating from USC in 2003. Schiffman is the Co-Director of the Maryland Early Intervention Program’s Strive for Wellness clinic, a research, training, and services program designed to improve the lives of young people at risk for psychosis, as well as their families. Dr. Schiffman’s research seeks to refine the identification of young people at risk for psychotic disorders, better understand the effects of psychosocial interventions for adolescents with psychosis, and uncover mechanisms that can reduce stigma against people with serious mental health concerns.
References
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, & . . . Heinssen R (2008). Prediction of psychosis in youth at high clinical risk: A multisite longitudinal study in North America. Archives of General Psychiatry, 65, 28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Carrión RE, Auther A, McLaughlin D, Olsen RH, John M, & Correll CU (2015). Psychosis prevention: A modified clinical high risk perspective from the recognition and prevention (RAP) program. American Journal of Psychiatry, 172, 986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Hilsenroth MJ, & Segal DL (2004). Comprehensive handbook of psychological assessment: Personality assessment (Vol. 2). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Fusar-Poli P, Cappucciati M, Rutigliano G, Schultze-Lutter F, Bonoldi I, Borgwardt S, . . . McGlashan TH (2015). At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry, 14, 322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P (2018). The hype cycle of the clinical high risk state for psychosis: The need of a refined approach. Schizophrenia Bulletin, 44, 250–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, & McGuire P (2012). Predicting psychosis: Meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry, 69, 220–229. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Rutigliano G, Lee TY, Beverly Q, Bonoldi I, & Patel R (2016). Towards a standard psychometric diagnostic interview for subjects at ultra high risk of psychosis: CAARMS versus SIPS. Psychiatry Journal, 2016, Article 7146341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, . . . Marcy P (2015). Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. American Journal of Psychiatry, 173, 362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, . . . Ryan N (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, & Cannon TD (2011). Psychosis risk screening with the prodromal questionnaire—Brief version (PQ-B). Schizophrenia Research, 129, 42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry PD, Nelson B, Phillips LJ, Yuen HP, Francey SM, Thampi A, & Thompson AD (2013). Randomized controlled trial of interventions for young people at ultra-high risk of psychosis: Twelve-month outcome. The Journal of Clinical Psychiatry, 74, 349–356. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, & Woods SW (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin, 29, 703–715. [DOI] [PubMed] [Google Scholar]
- Millman ZB, Pitts SC, Thompson E, Kline ER, Demro C, Weintraub MJ, & Schiffman J (2018). Perceived social stress and symptom severity among help-seeking adolescents with versus without clinical high-risk for psychosis. Schizophrenia research, 192, 364–370. [DOI] [PubMed] [Google Scholar]
- PRIME Psychosis Prodrome Research Clinic. (2019, January 10). Retrieved from https://medicine.yale.edu/psychiatry/research/programs/clinical_people/prodome.aspx?organizationId=109519?organizationId=109519
- Schiffman J (2018). Considerations for the development and implementation of brief screening tools in the identification of early psychosis. Journal of Schizophrenia Research, 199, 41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford MR, Mayo-Wilson E, Loucas CE, James A, Hollis C, Birchwood M, & Kendall T (2015). Efficacy and safety of pharmacological and psychological interventions for the treatment of psychosis and schizophrenia in children, adolescents and young adults: A systematic review and meta-analysis. PLoS ONE, 10(2), e0117166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Structured Interview For Psychosis-Risk Syndromes (2018, October 23). Retrieved from https://thesipstraining.com/
- Tang SX, Yi JJ, Calkins ME, Whinna DA, Kohler CG, Souders MC, & . . . Gur RE (2014). Psychiatric disorders in 22q11. 2 deletion syndrome are prevalent but undertreated. Psychological Medicine, 44, 1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson E, Kline E, Ellman LM, Mittal V, Reeves GM, & Schiffman J (2015). Emotional and behavioral symptomatology reported by help-seeking youth at clinical high-risk for psychosis. Schizophrenia Research, 162, 79–85. [DOI] [PubMed] [Google Scholar]
- Weissman MM (1990). Evidence for comorbidity of anxiety and depression: Family and genetic studies of children In Maser JD & Cloninger CR (Eds.), Comorbidity of mood and anxiety disorders (pp. 349–365). Arlington, VA: American Psychiatric Association. [Google Scholar]