Abstract
Rationale: Whether critical care improvements over the last 10 years extend to all hospitals has not been described.
Objectives: To examine the temporal trends of critical care outcomes in minority and non–minority-serving hospitals using an inception cohort of critically ill patients.
Measurements and Main Results: Using the Philips Health Care electronic ICU Research Institute Database, we identified minority-serving hospitals as those with an African American or Hispanic ICU census more than twice its regional mean. We examined almost 1.1 million critical illness admissions among 208 ICUs from across the United States admitted between 2006 and 2016. Adjusted hospital mortality (primary) and length of hospitalization (secondary) were the main outcomes. Large pluralities of African American (25%, n = 27,242) and Hispanic individuals (48%, n = 26,743) were cared for in minority-serving hospitals, compared with only 5.2% (n = 42,941) of white individuals. Over the last 10 years, although the risk of critical illness mortality steadily decreased by 2% per year (95% confidence interval [CI], 0.97–0.98) in non–minority-serving hospitals, outcomes within minority-serving hospitals did not improve comparably. This disparity in temporal trends was particularly noticeable among African American individuals, where each additional calendar year was associated with a 3% (95% CI, 0.96–0.97) lower adjusted critical illness mortality within a non–minority-serving hospital, but no change within minority-serving hospitals (hazard ratio, 0.99; 95% CI, 0.97–1.01). Similarly, although ICU and hospital lengths of stay decreased by 0.08 (95% CI, −0.08 to −0.07) and 0.16 (95% CI, −0.16 to −0.15) days per additional calendar year, respectively, in non–minority-serving hospitals, there was little temporal change for African American individuals in minority-serving hospitals.
Conclusions: Critically ill African American individuals are disproportionately cared for in minority-serving hospitals, which have shown significantly less improvement than non–minority-serving hospitals over the last 10 years.
Keywords: disparity, mortality, African American, minority
At a Glance Commentary
Scientific Knowledge on the Subject
Minorities face a wide range of health disparities that extend into the ICU. Whether hospitals that predominantly care for minority patients have evidenced the same improvements in critical care outcomes as non–minority-serving hospitals has not been previously investigated.
What This Study Adds to the Field
We examined the temporal trends of ICU mortality and lengths of stay in minority and non–minority-serving hospitals from 2006 to 2016 in over 200 hospitals from across the United States. We find that minority-serving hospitals have had significantly less temporal improvement in mortality and length of stay than non–minority-serving hospitals. This observation is most apparent for African American patients, who have had no meaningful decrease in mortality or lengths of stay when hospitalized in a minority-serving hospital. Our data highlight the continued disparities facing minorities and minority-serving hospitals in the United States.
Health disparities continue to plague the U.S. medical system (1). Despite higher rates of comorbidities (2), minorities have less access to preventative medicine (3–6), seeking care in lower-performance hospitals with higher complication (7, 8), readmission (9), and mortality rates (10–13). Although the higher acuity and resource utilization of critical illness might seem immune to such disparities, racial differences in the ICU have similarly been described (14–18).
Accordingly, we examined whether improvements in critical care outcomes over the last decade (19–22) extend to minority-serving hospitals. Using a large repository of almost 1.1 million ICU admissions from hospitals across the United States (23–25), we describe the temporal trends of critical illness outcomes according to hospital minority composition and whether these trends differed by ethnicity.
Methods
Data Source
Phillips Healthcare, a major vendor of ICU equipment and services, provides a telehealth ICU platform to over 300 hospitals across the United States. Data from participating hospitals is anonymously curated in the electronic ICU Research Institute Database (eICU-RI), a collaborative partnership between Philips Healthcare and the Laboratory of Computational Physiology at Massachusetts Institute of Technology (23–26). It contains high-resolution patient data, including demographics, vital signs, laboratory tests, illness severity scores, fluid intake and outputs, and diagnostic coding from patients admitted between 2003 and 2016. Participating hospitals trained clinicians to use the Philips platform, using primary data entry and drop-down boxes to adjudicate patient information and diagnoses, with direct synchronization with laboratory and clinical data.
The most up-to-date formulation of the eICU-RI contains 1.7 million unique first critical illness hospitalizations from 301 hospitals. Missing data included hospital regional location (n = 430,137) and APACHE (Acute Physiology and Chronic Health Evaluation) IV severity of illness scoring (n = 104,041). We excluded those admitted before 2006 (n = 30,207) due to low participation and unreliability of data entry, leaving 1,088,109 patients. Of these, 48,514 lacked documentation of length of critical stay, leaving a cohort of 1,039,595 for primary analysis.
Exposure
We used the 2010 U.S. Census data to determine the African American and Hispanic regional means and defined minority-serving hospitals as those with a greater than twofold African American or Hispanic ICU census than the corresponding regional mean. The cutpoints for African American and Hispanic individuals were 11.30% and 7.0% in the Midwest, 13% and 12.6% in the Northeast, 20.1% and 15.9% in the South, and 5.7% and 28.6% in the West, respectively (27, 28). As an alternate definition, we defined minority-serving hospitals as those with a greater than 25% African American or Hispanic ICU patient census (11).
Outcomes
Our primary outcome was death during critical illness hospitalization. The secondary outcomes were ICU and hospital lengths of stay.
Categorization of Trends
We examined year of admission as a categorical (i.e., as individual 2-yr groups) and continuous variable.
Variables
Basic demographics included age, sex, and ethnicity. Ethnicity was self-reported as white, African American, Hispanic, Asian, Native American, other, or unknown. Admission diagnoses were adjudicated by trained clinicians within the first 24 hours of ICU admission as part of the APACHE IV score system (29), and were categorized into the 15 most common clinical categories, including sepsis, myocardial infarction/angina, trauma, gastrointestinal bleed, arrhythmia, drug/alcohol complications, cerebrovascular accident, coronary artery bypass grafting, pneumonia, malignancy related, congestive heart failure, cardiac arrest, angina, diabetes related, intracranial bleed, other, and unknown. The admission APACHE IV score, obtained within 24 hours of ICU admission, was used to quantify severity of illness. The Charlson comorbidity scoring system was used to describe preexisting illness burden (30). ICU unit type (medical, medical surgical, surgical, cardiac, cardiothoracic, and neurological) was included as a series of indicator variables.
Analysis
Baseline characteristics were presented as percentages for categorical variables and mean and SD for continuous variables by hospital minority composition. We used Cox proportional hazards model to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between categorical year of admission and mortality. Time to event was defined as the length of stay between ICU admission and date of death or censoring. Patients who were discharged were censored at that time. The models were adjusted for age, sex, ethnicity (white, African American, Hispanic, or other), unit type (categorical), admission diagnosis (categorical), APACHE IV severity of illness, and Charlson comorbidity scores (continuous), and year of admission (categorical; 2006–2008 as the reference group). We used multiplicative interactions to determine whether the effect of admission year on mortality differed according to hospital minority composition, and explored whether these findings were consistent across ethnicity.
In secondary analyses, we defined minority-serving hospitals as those with a greater than 25% African American or Hispanic ICU census and conducted survival analyses as in our primary analysis. Second, we applied generalized estimating equations with Poisson error distribution, log link function, and exchangeable covariance structure to examine the associations between categorical admission year and mortality in those hospitals with greater than 500 admissions. This approach allowed us to account for within-hospital correlation. Third, to account for hospital participation, we examined our primary analysis in those hospitals that had consistent participation in four consecutive time periods.
As secondary endpoints, we describe ICU and critical illness hospitalization lengths of stay according to minority-serving hospital composition. Using standard least squares regression, including all variables from the primary analysis and an indicator for hospital mortality, we describe the adjusted differences in lengths of stay in minority-serving and non–minority-serving hospitals and how these trends have changed over time.
To determine whether there were differences in critical illness resource utilization across hospitals, we examined the delay to ICU transfer in those patients admitted directly from the emergency deparment (31). Using all variables above, and an indicator variable for hospital mortality, we describe whether the delay differed by hospital composition and how these trends have changed over time.
All analyses were performed using JMP Pro 12 and PROC PHREG and PROC GENMOD in SAS 9.4 (both produced by SAS Institute).
Results
Usage and Characteristics of Minority-Serving Hospitals
Of almost 1.1 million critically ill patients, 10% (n = 109,022) were cared for in one of 14 (7% of sampled hospitals) minority-serving hospitals. There was significant ethnic variation in usage of such hospitals, with 25% (n = 27,242) of African American and 48% (n = 26,743) of Hispanic patients receiving critical care in a minority-serving hospital, compared with 5.2% (n = 42,941) of white patients. Patients in minority-serving hospitals tended to be younger, with a lower comorbidity burden (Table 1), yet a higher level of illness severity on ICU presentation. Minority-serving hospitals had a higher relative percentage of ICU admissions for trauma, myocardial infarction, and heart failure, and a lower percentage for sepsis and drug and alcohol complications, than non–minority-serving hospitals. Hospital mortality proportions were higher in minority than non–minority-serving hospitals (10.5 vs. 9.5%, P < 0.001), consistently across ethnic groupings.
Table 1.
Baseline Patient and Hospital Characteristics
| Patient and Hospital Characteristics | Minority-Serving Hospitals | Non–Minority-Serving Hospitals |
|---|---|---|
| No. of patients | 109,022 | 979,087 |
| No. of hospitals | 14 | 194 |
| Patient characteristics | ||
| Age, yr | 61.8 (18.2) | 62.8 (17.6) |
| Sex, F | 46.5 | 45.8 |
| Ethnicity/race | ||
| White | 39.4 | 80.6 |
| African American | 25.0 | 8.6 |
| Hispanic | 24.5 | 3.0 |
| Other/unknown | 11.1 | 7.8 |
| ICU type | ||
| Cardiac/cardiothoracic | 27.9 | 22.5 |
| Medical | 14.7 | 15.7 |
| Medical/surgical | 48.7 | 55.4 |
| Surgical | 8.7 | 6.4 |
| Charlson comorbidity index | 3.4 (2.7) | 3.5 (2.7) |
| APACHE IV | 55.7 (27.0) | 53.4 (25.5) |
| Admission diagnosis | ||
| Sepsis | 7.7 | 10.2 |
| MI/angina | 9.3 | 8.0 |
| CABG | 3.8 | 3.9 |
| CHF | 3.7 | 3.0 |
| Trauma | 5.5 | 5.1 |
| Drug and alcohol related | 2.6 | 4.4 |
| CVA | 3.6 | 4.0 |
| Pneumonia | 3.6 | 3.6 |
| Intracranial bleed | 2.6 | 1.6 |
| Hospital characteristics | ||
| Academic | 28.6 | 6.7 |
| Hospital beds | ||
| >500 | 14.2 | 11.3 |
| 250 to <500 | 36.0 | 15.4 |
| Hospital mortality | 10.5 | 9.5 |
Definition of abbreviations: APACHE IV = Acute Physiology and Chronic Health Evaluation IV; CABG = coronary artery bypass grafting; CHF = congestive heart failure; CVA = cerebrovascular accident; MI = myocardial infarction.
Percentages for categorical variables and mean (SD) for continuous variables are provided.
Temporal Trends in Critical Care Mortality
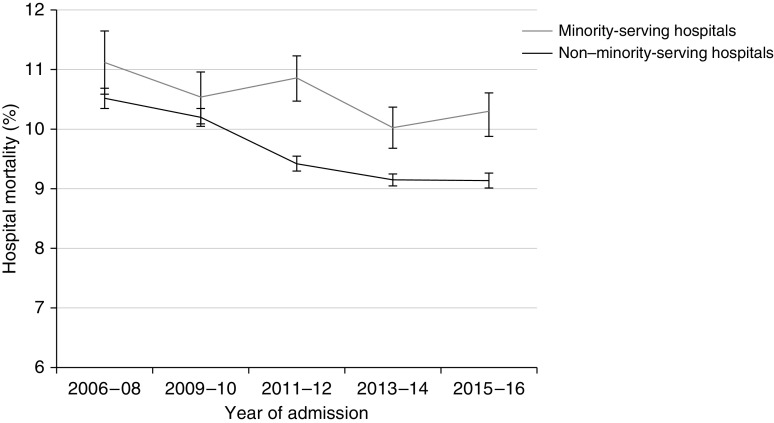
Although the incidence of critical illness mortality (Figure 1) and adjusted mortality (Table 2) steadily decreased from 2006 to 2016, the trends differed between minority and non–minority-serving hospitals (multiplicative interaction between calendar year and minority-serving hospital, P < 0.001). A steady decline in critical illness mortality (HR, 0.98; 95% CI, 0.97–0.98 per additional calendar year) was observed in non–minority-serving hospitals, but not in minority-serving hospitals (Table 2 and Table E1 in the online supplement).
Figure 1.
Critical illness mortality (95% confidence interval) in minority and non–minority-serving hospitals from 2006 to 2016 in the United States (n = 1,088,109). Trend P values for minority-serving and non–minority-serving hospitals were 0.002 and <0.001, respectively.
Table 2.
Hazard Ratio (95% Confidence Interval) of Critical Illness Mortality per Admission Year Category Provided, with 2006–2008 Considered as Reference for All Analyses
| Admission Year |
Multiplicative Interaction Term P Value | |||||
|---|---|---|---|---|---|---|
| 2006–2008 | 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | ||
| All hospitals | Ref. | 0.86 (0.84–0.89) | 0.82 (0.80–0.84) | 0.81 (0.79–0.82) | 0.80 (0.78–0.82) | — |
| Minority-serving hospitals | Ref. | 0.83 (0.77–0.89) | 0.88 (0.82–0.95) | 0.79 (0.74–0.85) | 0.88 (0.81–0.94) | <0.001 |
| Non–minority-serving hospitals | Ref. | 0.87 (0.85–0.89) | 0.80 (0.79–0.82) | 0.81 (0.79–0.82) | 0.79 (0.77–0.81) | |
| Minority hospital defined as having greater than 25% African American or Hispanic census | ||||||
| Minority-serving hospitals | Ref. | 0.85 (0.80–0.90) | 0.83 (0.78–0.87) | 0.79 (0.75–0.83) | 0.85 (0.80–0.90) | 0.05 |
| Non–minority-serving hospitals | Ref. | 0.87 (0.84–0.89) | 0.81 (0.79–0.83) | 0.81 (0.79–0.83) | 0.79 (0.77–0.81) | |
| GEE analysis in hospitals with >500 admissions to account for hospital correlation | ||||||
| Minority-serving hospitals | Ref. | 0.94 (0.92–0.95) | 0.93 (0.91–0.95) | 0.90 (0.88–0.93) | 0.94 (0.91–0.97) | 0.05 |
| Non–minority-serving hospitals | Ref. | 0.94 (0.92–0.95) | 0.90 (0.88–0.92) | 0.89 (0.87–0.91) | 0.88 (0.86–0.90) | |
| Cox regression in hospitals with participation in four consecutive time periods | ||||||
| Minority-serving hospitals | Ref. | 0.82 (0.76–0.88) | 0.87 (0.81–0.94) | 0.75 (0.70–0.81) | 0.87 (0.81–0.94) | 0.003 |
| Non–minority-serving hospitals | Ref. | 0.87 (0.85–0.89) | 0.81 (0.79–0.83) | 0.82 (0.80–0.84) | 0.80 (0.77–0.82) | |
Definition of abbreviations: GEE = generalized estimating equation; Ref. = reference.
Adjusted hazard ratios for critical illness mortality according to admission year and hospital minority composition. Adjusted for age, sex, ethnicity, unit type, admission diagnosis, Charlson comorbidity score, and illness severity. In addition, alternative definition of hospital minority composition, and analytic approaches to account for within hospital correlation and hospital participation, are provided. Multiplicative interaction P value between indicator for minority-serving hospitals and admission year (defined continuously) provided.
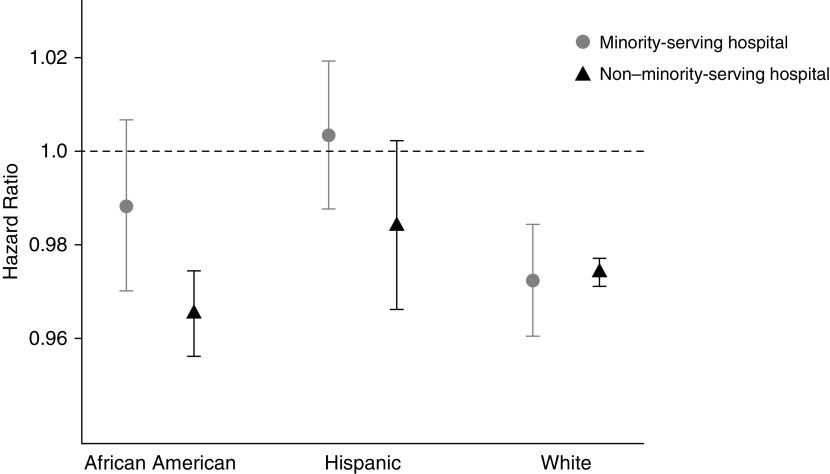
This temporal inequality was most apparent among African American patients (multiplicative interaction between calendar year and minority-serving hospital P values 0.02, 0.07, and 0.04 among African American, Hispanic, and white patients, respectively), where each additional calendar year was associated with 3% lower adjusted mortality (HR, 0.97; 95% CI, 0.96–0.97) in non–minority-serving hospitals, compared with no change in minority-serving hospitals (HR, 0.99; 95% CI, 0.97–1.01) (Figure 2).
Figure 2.
The adjusted hazard ratio (95% confidence interval) of hospital mortality per additional calendar year of admission between 2006 and 2016, stratified by ethnicity. The hazard ratios were adjusted for age, sex, unit type, admission diagnosis, Charlson comorbidity score, illness severity, and year of admission (defined continuously). The P values for the multiplicative interaction between calendar year and minority-serving hospital were 0.02, 0.07, and 0.04 among African American, Hispanic, and white patients, respectively. N = 1,039,595 patients in 208 hospitals.
Sensitivity Analyses of Mortality
Using a threshold of more than a 25% African American or Hispanic ICU census to define a minority-serving hospital resulted in 26 minority-serving hospitals serving 177,186 patients. Patients within these hospitals had higher mortality rates and similarly less temporal improvement (multiplicative interaction between each additional calendar year and minority-serving hospital P value of 0.05) than those in non–minority-serving hospitals (Table 3). Analyses that accounted for within-hospital correlation and participation resulted in similar findings.
Table 3.
Change (95% Confidence Interval) in Length of ICU and Critical Illness Hospital Stay (in Days), Relative to 2006–2008, Adjusted for Age, Sex, Ethnicity, Unit Type, Admission Diagnosis, Charlson Comorbidity Score, Illness Severity, Admission Year Category, and Hospital Mortality
| Admission Year |
Multiplicative Interaction Term P Value | |||||
|---|---|---|---|---|---|---|
| 2006–2008 | 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | ||
| Adjusted change in ICU length of stay | ||||||
| Minority-serving hospitals | Ref. | −0.35 (−0.43 to −0.27) | −0.48 (−0.56 to −0.40) | −0.41 (−0.49 to −0.34) | −0.44 (−0.52 to −0.36) | <0.001 |
| Non–minority-serving hospitals | Ref. | −0.42 (−0.45 to −0.39) | −0.56 (−0.59 to −0.53) | −0.64 (−0.66 to −0.61) | −0.67 (−0.70 to −0.65) | |
| Adjusted change in hospital length of stay | ||||||
| Minority-serving hospitals | Ref. | −0.74 (−0.91 to −0.59) | −1.12 (−1.27 to −0.96) | −1.01 (−1.17 to −0.87) | −0.98 (−1.13 to −0.81) | <0.001 |
| Non–minority-serving hospitals | Ref. | −0.56 (−0.63 to −0.50) | −0.90 (−0.95 to−0.85) | −1.14 (−1.18 to −1.09) | −1.37 (−1.41 to −1.32) | |
Definition of abbreviation: Ref. = reference.
Adjusted change of ICU and critical illness hospitalization lengths of stay from 2006 to 2016. Multiplicative interaction between indicator for minority-serving hospitals and admission year (defined continuously) are provided.
Temporal Trends in ICU and Hospital Lengths of Stay
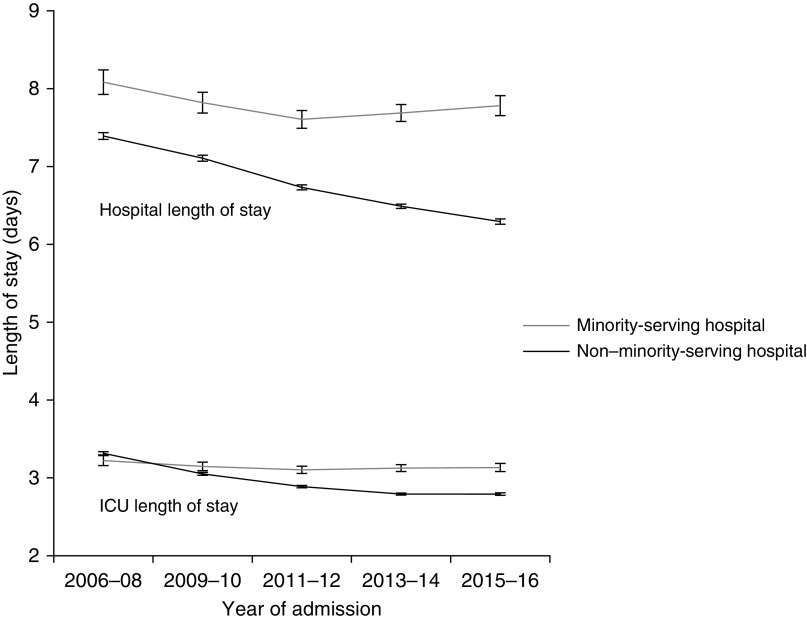
The lengths of ICU stay and critical illness hospitalization were higher among minority than non–minority-serving hospitals (3.1 ± 3.9 and 7.3 ± 6.9 d compared with 2.9 ± 3.6 and 6.4 ± 6.2 d, respectively), a difference that remained in an adjusted analysis that included hospital mortality of 0.03 (95% CI, 0.02–0.04; P < 0.001) and 0.21 (95% CI, 0.20–0.23; P < 0.001) days longer ICU and hospital stays in minority-serving hospitals, respectively. ICU and hospital lengths of stay steadily decreased in non–minority-serving hospitals (−0.08 [95% CI, −0.08 to −0.07] d, P < 0.001; and −0.16 [95% CI, −0.16 to −0.15] d, P < 0.001) per additional calendar year, respectively, but significantly less so among minority-serving hospitals (multiplicative interaction between minority-serving hospital and admission year P < 0.001 for both ICU and hospital lengths of stay), remaining essentially constant from 2011 to 2016 (Figure 3 and Table 3). This temporal disparity was most apparent in African American patients, for whom length of stay decreased in non–minority-serving hospitals, but not in minority-serving hospitals (Table 4).
Figure 3.
Temporal trends in hospital and ICU length of stay in minority- and non–minority-serving hospitals. Mean (95% confidence interval) lengths of stay according to year of admission are provided. Trend P values were all less than 0.001, except for ICU length of stay in minority-serving hospitals (P = 0.06).
Table 4.
Adjusted Change (95% CI) per Additional Calendar Year in the Length (in Days) of ICU and Critical Illness Hospital Stay according to Ethnicity
| ICU Length of Stay |
Hospital Length of Stay |
|||
|---|---|---|---|---|
| Minority-Serving Hospital | Non–Minority-Serving Hospital | Minority-Serving Hospital | Non–Minority-Serving Hospital | |
| African American | ||||
| Adjusted change (95% CI), d | −0.01 (−0.02 to 0.01) | −0.09 (−0.10 to −0.08) | −0.03 (−0.07 to 0.01) | −0.21 (−0.23 to −0.20) |
| P value | 0.46 | <0.001 | 0.19 | <0.001 |
| Hispanic | ||||
| Adjusted change (95% CI), d | −0.09 (−0.10 to −0.07) | −0.06 (−0.07 to −0.04) | −0.20 (−0.23 to −0.16) | −0.12 (−0.15 to −0.09) |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
| White | ||||
| Adjusted change (95% CI), d | −0.04 (−0.05 to −0.02) | −0.08 (−0.08 to −0.07) | −0.08 (−0.11 to −0.06) | −0.16 (−0.17 to −0.16) |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
Definition of abbreviation: CI = confidence interval.
Adjusted change in length of stay per additional calendar year according to ethnicity. The change in length of stay was adjusted for age, sex, ethnicity, unit type, admission diagnosis, Charlson comorbidity score, illness severity, admission year (defined continuously), and hospital mortality. Multiplicative interaction P values between indicator for minority-serving hospitals and admission year (defined continuously) were less than 0.001 within each ethnic stratum.
Temporal Trends in Delay to ICU Transfer in Patients Admitted from the Emergency Department
Among 567,325 ICU admissions from the emergency department, the mean (±SD) delay until ICU admission was 3.9 (±16.3) hours among non–minority-serving hospitals and 5.9 (±19.4) hours among minority-serving hospitals (P < 0.001). Over the last 10 years, the adjusted delay decreased by 7.6 minutes (95% CI, −8.66 to −6.51, P < 0.001) per additional calendar year in non–minority-serving hospitals, yet had little change (1.0 min; 95% CI, −2.62 to 4.67, P = 0.58) in minority-serving hospitals.
Discussion
In our sampling of approximately 200 hospitals across the United States, almost a third of critically ill African American and half of critically ill Hispanic patients received critical care in just 7% of surveyed hospitals. These minority-serving hospitals showed significantly less decline in critical illness mortality and length of stay over the last decade compared with non–minority-serving hospitals. Although this inequality was consistent across ethnicities, it was most pronounced among African American individuals, in whom we observed no temporal improvement in critical care mortality or reduction in length of stay during this period.
Minority-serving hospitals tended to care for younger patients, with a lower overall burden of disease comorbidity, yet with a paradoxically higher severity of illness severity and mortality. Accordingly, it is difficult to determine whether our findings reflect caring for an increasingly disadvantaged population or differences in hospital resource utilization. As a proxy for hospital practice patterns, we examined the delay to ICU admission for those patients admitted through the emergency department, a clinically important indicator (31–34). We found that minority-serving hospitals had significantly longer delays with little temporal improvement, whereas the adjusted delay to ICU admission decreased by almost 8 minutes per year in non–minority-serving hospitals.
Regardless of how much of the increased mortality risk is due to patient- or hospital-specific issues, the high minority usage of these hospitals highlights the obstacles facing African American individuals in the United States. The “neighborhood effect,” whereby location of residence has a profound effect on outcomes (35–39), highlights the socioeconomic barriers to achieving equitable health care access, compounded by differences in practice patterns and resource utilization that extend into the ICU (18, 40, 41). From the perspective of health care delivery, recognizing the challenges facing minority-serving hospitals is particularly important in the current “pay for performance” reimbursement paradigm (42) so as not to unfairly penalize the most vulnerable hospitals (43). Our data provide clinical context for this concern, and underscores the need for additional support for minority-serving hospitals to ensure that they have the appropriate resources to meet their strenuous clinical demand.
Our analysis has several notable limitations. Confounding due to either admission or discharge bias is possible, particularly because minority patients tend to receive more intensive therapy and testing toward the end of life. Whether the ethnic distributions in the ICU were similar to those of the hospital were not known. In addition, how representative hospitals that choose to use the Phillips platform are is not known, and important patient characteristics, such as income, insurance type, and lifestyle choices, as well as hospital information, were not available. Finally, using more granular population census definitions, such as county codes, could improve the precision of minority-serving hospital definitions. However, we examined two different definitions of minority-serving hospitals, with similar results, and our primary findings were consistent through a range of sensitivity analyses and statistical approaches. Despite these limitations, the sheer size and granularity of this dataset are important strengths, providing a unique snapshot of modern American critical care over the last 10 years.
Conclusions
A large proportion of minority patients receive critical illness care in a small number of minority-serving hospitals, which, over the last 10 years, have not enjoyed the steady decrease in mortality and length of stay that non–minority-serving hospitals have. Whether this reflects a more systemic disparity, whereby African American individuals are more medically disadvantaged upon presentation, or differences in hospital care and resources, is not known, but regardless, this observation highlights the profound obstacles facing minorities and minority-serving hospitals.
Supplementary Material
Footnotes
Author Contributions: Conception and design—J.D.; analysis and interpretation—J.D., M.Á.A.d.l.H, W.L., M.K., R.O.D., B.N.M.R., L.C., and O.B.; drafting the manuscript for important intellectual content—J.D., K.J.M., and O.B.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.201903-0623OC on January 17, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. 2002;287:1288–1294. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services, Office of Minority Services. Profile: black/African Americans [accessed 2019 Jul 1]. Available from: https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61.
- 3.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 4.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 5.Kendrick J, Nuccio E, Leiferman JA, Sauaia A. Primary care providers perceptions of racial/ethnic and socioeconomic disparities in hypertension control. Am J Hypertens. 2015;28:1091–1097. doi: 10.1093/ajh/hpu294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kogan MD, Kotelchuck M, Alexander GR, Johnson WE. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. 1994;84:82–88. doi: 10.2105/ajph.84.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ly DP, Lopez L, Isaac T, Jha AK. How do black-serving hospitals perform on patient safety indicators? Implications for national public reporting and pay-for-performance. Med Care. 2010;48:1133–1137. doi: 10.1097/MLR.0b013e3181f81c7e. [DOI] [PubMed] [Google Scholar]
- 8.Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014;211:647, e1–e16. doi: 10.1016/j.ajog.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 11.Haider AH, Ong’uti S, Efron DT, Oyetunji TA, Crandall ML, Scott VK, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012;147:63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López L, Jha AK. Outcomes for whites and blacks at hospitals that disproportionately care for black Medicare beneficiaries. Health Serv Res. 2013;48:114–128. doi: 10.1111/j.1475-6773.2012.01445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bime C, Poongkunran C, Borgstrom M, Natt B, Desai H, Parthasarathy S, et al. Racial differences in mortality from severe acute respiratory failure in the United States, 2008–2012. Ann Am Thorac Soc. 2016;13:2184–2189. doi: 10.1513/AnnalsATS.201605-359OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lauerman M, Herrera A, Klyushnenkova E, Narayan M, Bruns B, Tesoriero R, et al. Racial disparities in ICU resource utilization in emergency general surgery. Crit Care Med. 2015;43:281–282. [Google Scholar]
- 16.Tyler PD, Stone DJ, Geisler BP, McLennan S, Celi LA, Rush B. Racial and geographic disparities in interhospital ICU transfers. Crit Care Med. 2018;46:e76–e80. doi: 10.1097/CCM.0000000000002776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soto GJ, Martin GS, Gong MN. Healthcare disparities in critical illness. Crit Care Med. 2013;41:2784–2793. doi: 10.1097/CCM.0b013e3182a84a43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rapoport J, Teres D, Steingrub J, Higgins T, McGee W, Lemeshow S. Patient characteristics and ICU organizational factors that influence frequency of pulmonary artery catheterization. JAMA. 2000;283:2559–2567. doi: 10.1001/jama.283.19.2559. [DOI] [PubMed] [Google Scholar]
- 19.Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42:625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD NIH NHLBI ARDS Network. Recent trends in acute lung injury mortality: 1996–2005. Crit Care Med. 2009;37:1574–1579. doi: 10.1097/CCM.0b013e31819fefdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lilly CM, Swami S, Liu X, Riker RR, Badawi O. Five-year trends of critical care practice and outcomes. Chest. 2017;152:723–735. doi: 10.1016/j.chest.2017.06.050. [DOI] [PubMed] [Google Scholar]
- 22.Oud L, Watkins P. Contemporary trends of the clinical characteristics, resource utilization and outcomes among patients with dementia admitted to ICU: a population-based study [abstract] Am J Respir Crit Care Med. 2015;191:A4014. doi: 10.1155/2015/618067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU collaborative research database, a freely available multi-center database for critical care research. Sci Data. 2018;5:180178. doi: 10.1038/sdata.2018.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson AEW, Pollard TJ, Celi LA, Mark RG. Analyzing the eICU collaborative research database. Presented at the Proceedings of the 8th ACM International Conference on Bioinformatics, Computational Biology, and Health Informatics. August 20–23, 2017, Boston, MA. [Google Scholar]
- 25.Komorowski M, Celi LA, Badawi O, Gordon AC, Faisal AA. The artificial intelligence clinician learns optimal treatment strategies for sepsis in intensive care. Nat Med. 2018;24:1716–1720. doi: 10.1038/s41591-018-0213-5. [DOI] [PubMed] [Google Scholar]
- 26.McShea M, Holl R, Badawi O, Riker RR, Silfen E. The eICU research institute: a collaboration between industry, health-care providers, and academia. IEEE Eng Med Biol Mag. 2010;29:18–25. doi: 10.1109/MEMB.2009.935720. [DOI] [PubMed] [Google Scholar]
- 27.Ennis SR, Rios-Vargas M, Albert NG. Washington, DC: U.S. Census Bureau; 2011. The Hispanic population: 2010. 2010 Census briefs. Report Number C2010BR-04. [Google Scholar]
- 28.Rastogi S, Johnson TD, Hoeffel EM, Drewery MPJ. Washington, DC: U.S. Census Bureau; 2011. The black population: 2010. 2010 Census briefs. Report Number C2010BR-06. [Google Scholar]
- 29.Harris K, Zhou J, Liu X, Hassan E, Badawi O. The obesity paradox is not observed in critically ill patients on early enteral nutrition. Crit Care Med. 2017;45:828–834. doi: 10.1097/CCM.0000000000002326. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 31.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP DELAY-ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 32.Intas D, Stergiannis P, Vassilopoulos G, Fildissis A. Impact of critically ill patients in regards to the boarding time from the emergency department to the intensive care unit. To Vima tou Asklipiou. 2011;10:417–436. [Google Scholar]
- 33.Rincon F, Mayer SA, Rivolta J, Stillman J, Boden-Albala B, Elkind MS, et al. Impact of delayed transfer of critically ill stroke patients from the emergency department to the Neuro-ICU. Neurocrit Care. 2010;13:75–81. doi: 10.1007/s12028-010-9347-0. [DOI] [PubMed] [Google Scholar]
- 34.Churpek MM, Yuen TC, Edelson DP. Delayed intensive care unit transfer is associated with increased mortality in ward patients [abstract] Am J Respir Crit Care Med. 2013;187:A6074. [Google Scholar]
- 35.Frei CR, Mortensen EM, Copeland LA, Attridge RT, Pugh MJ, Restrepo MI, et al. Disparities of care for African-Americans and Caucasians with community-acquired pneumonia: a retrospective cohort study. BMC Health Serv Res. 2010;10:143. doi: 10.1186/1472-6963-10-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., III Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 37.Yergan J, Flood AB, LoGerfo JP, Diehr P. Relationship between patient race and the intensity of hospital services. Med Care. 1987;25:592–603. doi: 10.1097/00005650-198707000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Fowler RA, Noyahr LA, Thornton JD, Pinto R, Kahn JM, Adhikari NK, et al. American Thoracic Society Disparities in Healthcare Group. An official American Thoracic Society systematic review: the association between health insurance status and access, care delivery, and outcomes for patients who are critically ill. Am J Respir Crit Care Med. 2010;181:1003–1011. doi: 10.1164/rccm.200902-0281ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kind AJH, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams JF, Zimmerman JE, Wagner DP, Hawkins M, Knaus WA. African-American and white patients admitted to the intensive care unit: is there a difference in therapy and outcome? Crit Care Med. 1995;23:626–636. doi: 10.1097/00003246-199504000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Shippee TP, Ferraro KF, Thorpe RJ. Racial disparity in access to cardiac intensive care over 20 years. Ethn Health. 2011;16:145–165. doi: 10.1080/13557858.2010.544292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan AM. Will value-based purchasing increase disparities in care? N Engl J Med. 2013;369:2472–2474. doi: 10.1056/NEJMp1312654. [DOI] [PubMed] [Google Scholar]
- 43.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309:342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.