Abstract
Background
Acupuncture and related techniques are promoted as a treatment for smoking cessation in the belief that they may reduce nicotine withdrawal symptoms.
Objectives
The objectives of this review are to determine the effectiveness of acupuncture and the related interventions of acupressure, laser therapy and electrostimulation in smoking cessation, in comparison with no intervention, sham treatment, or other interventions.
Search methods
We searched the Cochrane Tobacco Addiction Group Specialized Register (which includes trials of smoking cessation interventions identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, and PsycINFO) and AMED in October 2013. We also searched four Chinese databases in September 2013: Sino‐Med, China National Knowledge Infrastructure, Wanfang Data and VIP.
Selection criteria
Randomized trials comparing a form of acupuncture, acupressure, laser therapy or electrostimulation with either no intervention, sham treatment or another intervention for smoking cessation.
Data collection and analysis
We extracted data in duplicate on the type of smokers recruited, the nature of the intervention and control procedures, the outcome measures, method of randomization, and completeness of follow‐up.
We assessed abstinence from smoking at the earliest time‐point (before six weeks) and at the last measurement point between six months and one year. We used the most rigorous definition of abstinence for each trial, and biochemically validated rates if available. Those lost to follow‐up were counted as continuing smokers. Where appropriate, we performed meta‐analysis pooling risk ratios using a fixed‐effect model.
Main results
We included 38 studies. Based on three studies, acupuncture was not shown to be more effective than a waiting list control for long‐term abstinence, with wide confidence intervals and evidence of heterogeneity (n = 393, risk ratio [RR] 1.79, 95% confidence interval [CI] 0.98 to 3.28, I² = 57%). Compared with sham acupuncture, the RR for the short‐term effect of acupuncture was 1.22 (95% CI 1.08 to 1.38), and for the long‐term effect was 1.10 (95% CI 0.86 to 1.40). The studies were not judged to be free from bias, and there was evidence of funnel plot asymmetry with larger studies showing smaller effects. The heterogeneity between studies was not explained by the technique used. Acupuncture was less effective than nicotine replacement therapy (NRT). There was no evidence that acupuncture is superior to psychological interventions in the short‐ or long‐term. There is limited evidence that acupressure is superior to sham acupressure for short‐term outcomes (3 trials, n = 325, RR 2.54, 95% CI 1.27 to 5.08), but no trials reported long‐term effects, The pooled estimate for studies testing an intervention that included continuous auricular stimulation suggested a short‐term benefit compared to sham stimulation (14 trials, n = 1155, RR 1.69, 95% CI 1.32 to 2.16); subgroup analysis showed an effect for continuous acupressure (7 studies, n = 496, RR 2.73, 95% CI 1.78 to 4.18) but not acupuncture with indwelling needles (6 studies, n = 659, RR 1.24, 95% CI 0.91 to 1.69). At longer follow‐up the CIs did not exclude no effect (5 trials, n = 570, RR 1.47, 95% CI 0.79 to 2.74). The evidence from two trials using laser stimulation was inconsistent and could not be combined. The combined evidence on electrostimulation suggests it is not superior to sham electrostimulation (short‐term abstinence: 6 trials, n = 634, RR 1.13, 95% CI 0.87 to 1.46; long‐term abstinence: 2 trials, n = 405, RR 0.87, 95% CI 0.61 to 1.23).
Authors' conclusions
Although pooled estimates suggest possible short‐term effects there is no consistent, bias‐free evidence that acupuncture, acupressure, or laser therapy have a sustained benefit on smoking cessation for six months or more. However, lack of evidence and methodological problems mean that no firm conclusions can be drawn. Electrostimulation is not effective for smoking cessation. Well‐designed research into acupuncture, acupressure and laser stimulation is justified since these are popular interventions and safe when correctly applied, though these interventions alone are likely to be less effective than evidence‐based interventions.
Plain language summary
Do acupuncture and related therapies help smokers who are trying to quit
We reviewed the evidence that acupuncture, acupressure, laser therapy or electrical stimulation help people who are trying to stop smoking.
Background
Acupuncture is a traditional Chinese therapy, generally using fine needles inserted through the skin at specific points in the body. Needles may be stimulated by hand or using an electric current (electroacupuncture). Related therapies, in which points are stimulated without the use of needles, include acupressure, laser therapy and electrical stimulation. Needles and acupressure may be used just during treatment sessions, or continuous stimulation may be provided by using indwelling needles or beads or seeds taped to to acupressure points. The aim of these therapies is to reduce the withdrawal symptoms that people experience when they try to quit smoking. The review looked at trials comparing active treatments with sham treatments or other control conditions including advice alone, or an effective treatment such as nicotine replacement therapy (NRT) or counselling. Sham treatment involves inserting needles or applying pressure to other points of the body not believed to have an active effect, or using dummy needles that do not go through the skin, or inactive laser or electrical stimulation devices. Using this type of control means that the patients should not know whether they are receiving active treatment or not.
To assess whether there was a sustained benefit in helping people to stop smoking we looked at the proportion of people who were abstinent at least six months after quit date. We also looked at short term outcomes, up to six weeks after quit date. Evidence of benefit after six months is regarded as necessary to show that a treatment could help people stop smoking permanently.
Study characteristics
We included 38 randomised studies published up to October 2013. Trials tested a variety of different interventions and controls. The specific points used, the number of sessions and whether there was continuous stimulation varied. Three studies (393 people) compared acupuncture to a waiting list control. Nineteen studies (1,588 people) compared active acupuncture to sham acupuncture, but only 11 of these studies included long‐term follow‐up of six months or more. Three studies (253 people) compared acupressure to sham acupressure but none had long‐term follow‐up. Two trials used laser stimulation and six (634 people) used electrostimulation. The overall quality of the evidence was moderate.
Key findings
Three studies comparing acupuncture to a waiting list control and reporting long‐term abstinence did not show clear evidence of benefit. For acupuncture compared with sham acupuncture, there was weak evidence of a small short‐term benefit but not of any long‐term benefit. Acupuncture was less effective than nicotine replacement therapy (NRT) and not shown to be better than counselling. There was limited evidence that acupressure is superior to sham acupressure in the short term but no evidence about long‐term effects. In an analysis of the subgroup of trials where the treatment included continuous stimulation, those trials which used continuous acupressure to points on the ear had the largest short‐term effect. The evidence from two trials using laser stimulation was inconsistent. The seven trials of electrostimulation do not suggest evidence of benefit compared to sham electrostimulation.
The review did not find consistent evidence that active acupuncture or related techniques increased the number of people who could successfully quit smoking. However, some techniques may be better than doing nothing, at least in the short term, and there is not enough evidence to dismiss the possibility that they might have an effect greater than placebo. They are likely to be less effective than current evidence‐based interventions. They are safe when correctly applied.
Summary of findings
Background
Acupuncture has been used in the treatment of nicotine dependence in the West since an incidental observation in Hong Kong (Wen 1973). Opium smokers who had been treated with electroacupuncture for pain relief reported that their opiate withdrawal symptoms were less severe than they expected. Since then, various techniques of needle or electrostimulation have been used as a treatment for dependence on various addictive substances, with the specific aim of reducing withdrawal symptoms and aiding cessation. For smoking cessation, two basic techniques are used. In the first, needles may be inserted for the duration of a treatment session (often lasting 15 to 20 minutes) at the time of cessation. The treatment may be repeated on the following days. Alternatively, or in addition to this intervention, specially designed indwelling needles may be inserted, usually in ear points, and held in position with surgical tape for several days. Patients are instructed to press these indwelling needles when they become aware of withdrawal symptoms. As an alternative to indwelling needles, small seeds or beads may be attached to the ear with adhesive tape and pressed intermittently (acupressure). Descriptions also exist of the use of a surgical suture which is inserted in the ear and knotted with a bead attached (Man 1975).
Acupuncture research is complicated by different fundamental approaches to acupuncture, and by difficulties in choosing placebo controls. Currently, there are two approaches to explain the effect of acupuncture, which seem incompatible. The differences between them have important implications for research into the needle effect. In the traditional approach (Traditional Chinese Acupuncture, TCA), the needles are inserted into particular locations where, it is believed, they can correct disturbances of a force called qi that underlie the patients' illness. Other locations are not believed to have this special property, and therefore can be readily used as placebo control. This is the theory that underlies most trials of acupuncture. In a more recent approach, known as Western Medical Acupuncture (WMA) the needle effect is believed to be obtained by stimulating nerves or connective tissue (White 2009). Since nerves and connective tissue are found throughout the body, the effects of the needles are not restricted to particular locations. Therefore, according to the WMA approach, no site can be needled as a placebo control. Moreover, no truly inert placebo for acupuncture needles has yet been devised. Various devices have been introduced that cause less stimulation than needles do, but none of these has been established as a truly inert placebo (Lund 2009; Lundeberg 2008).
Acupuncture needles are usually stimulated by hand when treating most conditions. For smoking cessation, some acupuncturists stimulate the needles electrically with the intention of more precisely stimulating the release of neurotransmitters that may be involved in suppression of withdrawal symptoms (Clement‐Jones 1979). This is electroacupuncture. Others have argued that the needles are unnecessary and it is sufficient to apply the electrical stimulation through surface electrodes attached to the mastoid process or the ear. This form of treatment is variously known as neuroelectrical therapy or (when used on the head) transcranial electrotherapy. This therapy overlaps, and has to a certain extent merged with, a therapy known as Cranial Electrostimulation (CES) which developed separately, mainly in the former Soviet Union and Eastern Europe, as a treatment for insomnia, anxiety and depression. CES has also been used for treatment of alcohol and drug dependence (Klawansky 1995). The electric current is usually sufficient to cause a mild tingling sensation, though sometimes subthreshold currents are used. Here, we combine all therapies involving application of electrical current to the head, whether to mastoid bones or to auricular acupuncture points, under the heading 'electrostimulation'. It has been argued that the precise placement of electrodes and the parameters of electrostimulation are critical for success (Boutros 1998; Patterson 1993), which we shall consider when there are sufficient studies.
As an alternative method of stimulating acupuncture points, some practitioners use pressure alone (acupressure). As with indwelling needles above, the pressure can be sustained by fixing a small ball or bead to the point with adhesive dressing; traditionally, the seed of the cowherb Semen Vaccariae was used. Others use low level laser, which is sometimes known as 'laser acupuncture' even though it does not involve needles. Low level laser therapy produces no sensation, and there is still some uncertainty whether it has a physiological effect on normal tissue including nerves, though some data suggest it may have anti‐inflammatory effects (Sakurai 2000). From the researcher's point of view, laser therapy has the advantage that both patients and practitioners can remain masked to group allocation by using defunctioned laser apparatus. This also applies to subthreshold electrostimulation therapy.
Uncontrolled studies have suggested that acupuncture reduces the symptoms of nicotine withdrawal and some high rates of initial success have been reported. For example, Fuller 1982 claimed that 95% of 194 subjects were not smoking after three treatments in one week, falling to 34% after 12 months. Choy 1983 claimed 88% success in a large study of 514 subjects but did not state the long‐term results. Clearly, only randomized controlled studies can determine whether this is more than a placebo effect.
Several literature reviews of controlled trials of acupuncture for smoking cessation have been published but their conclusions are not uniform.
We undertook a review and meta‐analysis in order to evaluate the short‐ and long‐term effects of acupuncture, acupressure, laser therapy and electrostimulation for smoking cessation.
Objectives
To evaluate whether acupuncture, acupressure, laser therapy and electrostimulation: a) are more effective than waiting list/no intervention for smoking cessation; b) have a specific effect in smoking cessation beyond placebo effects; c) are more effective than other interventions used for smoking cessation.
Methods
Criteria for considering studies for this review
Types of studies
All randomized controlled trials comparing acupuncture, acupressure, laser therapy or electrostimulation with either no intervention, or a sham form of the intervention, or another intervention, for smoking cessation.
Types of participants
Tobacco smokers of any age who wished to stop smoking.
Types of interventions
Non‐pharmacological stimulation interventions involving needle puncture, finger pressure or laser therapy in areas of the body described by the study's author as acupuncture points, which includes points on the ear, face and body, or the related intervention of electrostimulation to the head region, through surface electrodes. Had we located any, studies using a Western acupuncture approach would have been considered separately from those using a traditional approach.
Types of outcome measures
Complete abstinence from smoking. The review has not been limited to studies where the outcome was confirmed biochemically.
Search methods for identification of studies
We searched the Cochrane Tobacco Addiction Group Specialized Register for trials conducted on any form of acupuncture, acupressure, or related laser or electrotherapy (most recent search October 2013). At the time of the search the Register included the results of searches of the Cochrane Central Register of Controlled trials (CENTRAL), issue 8, 2013; MEDLINE (via OVID) to update 20130906; EMBASE (via OVID) to week 201336; and PsycINFO (via OVID) to update 20130828. See the Tobacco Addiction Group Module in the Cochrane Library for full search strategies and a list of other resources searched. We also searched AMED (via Ovid) on 11 Sept 2013, CNKI (China National Knowledge Infrastructure) on 24 September 2013, Wangfang Data on 25 September 2013, and SinoMed (formerly Chinese Biomedical Database) and VIP on 26 September 2013.
The free text or keyword search strategy was (acupuncture OR acupressure OR transcutaneous OR electric stimulation OR electrostimulation OR electro*acupuncture OR neuro*electric therapy OR laser therapy) combined with (tobacco OR smoking) for AMED and Chinese databases. We included terms other than acupuncture for the first time in 2002 and searches for these terms were retrospective to the earliest date available on all databases. In addition to these searches, we obtained relevant references from published reviews, clinical trials, and conference abstracts.
Data collection and analysis
Two authors (from HR, AW, LS) independently extracted data for smoking cessation rates from each report, but JL alone extracted the Chinese reports. We resolved disagreements by discussion. We were not blinded to the study authors or journal title. Where necessary and possible, we contacted authors to provide missing data.
We extracted data (where present in the report) for two time‐points: short‐term effect, i.e. the first measure after the treatment, up to a maximum of six weeks from the quit date; and long‐term effect i.e. the last time‐point used up to one year, but with a minimum of six months. The two time‐points were selected in an attempt to identify separately the possible effects of the intervention on a) cessation in the acute withdrawal period (i.e. 'Does acupuncture have any effect at all?') and b) sustained abstinence (i.e. 'Is acupuncture a clinically useful intervention?').
Where necessary, we recalculated the published data on an intention‐to‐treat basis, i.e. counting all drop‐outs and subjects lost to follow‐up as continuing smokers. We preferred sustained smoking cessation to point prevalence where these figures were available.
We noted assessment of withdrawal symptoms, but we did not extract data for reported cigarette consumption and concentrations of nicotine breakdown products (carbon monoxide [CO] or cotinine).
The primary analyses grouped studies according to the type of treatment (acupuncture, acupressure alone, laser therapy, or electrostimulation) whether given alone or as an adjunct to other interventions, as long as the other interventions were given to all groups. Studies that compared the effect of sustained stimulation (beads or needles) of auricular points with sham points were included in another analysis (new for this update of the review), regardless of any other intervention used at the time of quitting. Previous versions of this review considered adjunctive acupuncture as a separate group, in case the effect of acupuncture was not measurable because of the other intervention. However, many studies used some level of psychological intervention making it difficult to set a threshold. It seems preferable to combine studies even if the effect of acupuncture might be subsidiary to another intervention and therefore small or even negligible. We considered different acupuncture approaches (needling of body, face, and ear) together for the primary analysis, with a further analysis of studies that used some form of continuous stimulation. We compared short‐ and long‐term outcomes for acupuncture, acupressure, laser therapy and electrostimulation individually with different control procedures (i.e. no intervention, sham therapy, and other active treatment control). We compared interventions with controls in the order appropriate for research into an existing therapy (Fonnebo 2007). In each case, we calculated a weighted estimate of the risk ratio (RR), with a positive outcome shown as greater than 1, using a Mantel‐Haenszel fixed‐effect model with 95% confidence intervals (CI). We assessed the amount of statistical heterogeneity between trials using the I² statistic (Higgins 2003). Values of 30 to 50% can be regarded as representing moderate, and values of over 50% as substantial. We did not report pooled estimates where heterogeneity was high. Where heterogeneity was moderate we assessed whether the size and significance of the estimated effect was sensitive to the choice of meta‐analysis method by testing the effect of pooling using a random effects model.
We tabulated comparisons between included studies that compared two types of acupuncture, but did not use meta‐analysis.
Acupuncture is a highly distinctive intervention; choosing a suitable sham control for acupuncture is essential for patient blinding, but is not easy (White 2001). Two types of sham acupuncture that are commonly used are a) needling an area that is not a recognised 'point', and b) needling a point which is believed to be ineffective for the condition. It is possible that inserting a needle in any location has some general physiological activity relevant to smoking cessation (Lewith 1995). Therefore, the ideal control procedure for acupuncture research would be one that does not involve penetration or stimulation of the skin and yet appears to the participant to be a needle penetrating the skin. Non‐penetrating sham needles have been developed, but have not so far been used in research into smoking cessation. For smoking cessation, all studies so far have adopted the usual classical convention that the effects of acupuncture are point‐specific, and tested that hypothesis.
However, it has been recognised that the control point that is chosen as an 'ineffective' point might have some specific effect on the condition. For example, in a review of acupuncture for asthma, points that were chosen for control groups in some studies because the researchers considered them to be ineffective for asthma were used by other groups as the active intervention (Jobst 1995). In this review, therefore, in response to earlier comments, we examined the points used as controls in each study and checked these against the active points used in the other studies and in two literature reviews of studies of acupuncture for smoking cessation (Zhang 1992, including 48 studies, and Jiang 1994, including 64 studies). Our principal analysis included all studies, i.e. including those in which the control group may have received active treatment. We performed a sensitivity analysis excluding those studies with possibly active control points.
Assessment of risk of bias in included studies
We assessed the risk of bias in each study based on the adequacy of sequence generation, allocation concealment, blinding, incomplete outcome data and other sources of bias using the methods of the current Cochrane Handbook. We did not consider bias from selective reporting since we only extracted data on smoking cessation. For adequacy of blinding, we assessed participant blinding for acupuncture/placebo acupuncture comparisons, and assumed blinding when the two interventions were designed to appear identical even if the word 'blind' was not stated; we assumed all other comparisons were not blinded. For judging whether incomplete outcome data had been addressed, we classified studies as being at low risk of bias for this item if there was a clear description of numbers randomised and lost to follow‐up in each treatment group, and numbers lost were not high and were not substantially different between groups. Following the recommended methodology for Cochrane Tobacco Addiction Group reviews, we assumed that all randomised participants who withdrew or were lost to follow‐up were smoking. If numbers lost to follow‐up were substantially different between groups, so that the relative effect was sensitive to the inclusion or exclusion of dropouts, we classified the risk of bias as uncertain. If losses to follow‐up seemed to have been ignored so that it was not possible to construct an intention‐to‐treat analysis with drop‐outs as smokers, the risk of bias was regarded as high. In judging whether the study is free from other bias, we mainly considered baseline differences in possible response predictors, such as duration of smoking and number of previous attempts to quit.
We included all studies in the analysis, regardless of the risk of bias, since this was uncertain for a high proportion of studies. We planned to interpret any positive findings by conducting a subgroup analysis of only those studies with low risk of bias.
Results
Description of studies
We identified 38 studies which qualified for inclusion in the review: 23 of acupuncture; five of acupressure; three of laser stimulation and seven of electrostimulation. Twelve studies also used continuous auricular stimulation in combination with acupuncture, acupressure or electrostimulation. Three acupuncture studies, detailed below, are each treated as two studies in the analyses giving a total of 41 in the Characteristics of included studies table. Three studies have only been reported in abstracts (Antoniou 2005; Docherty 2003; Scheuer 2005). Three were published in Chinese (Han 2006; Huang 2012; Li 2009), five in French (Labadie 1983; Lacroix 1977; Lagrue 1980; Vandevenne 1985; Vibes 1977), one in Italian (Circo 1985), and the remainder in English. See Figure 1 for a flow diagram of papers assessed for current update, in which five new included studies were identified.
1.

Flow diagram for Update 2014
Two studies reported short‐ and long‐term results in separate papers (Clavel 1992; He 1997). Two reports each described a four‐arm trial which amounted to two parallel studies, i.e. two different intervention groups each with its own control group. In both cases, we considered these as two separate studies, Martin 1981a/ Martin 1981b and Parker 1977a/ Parker 1977b.
All studies were straightforward parallel arm design except two which were of factorial design. Clavel 1992 evaluated nicotine replacement therapy (NRT) and acupuncture simultaneously in a 2x2 design. For the comparison of acupuncture with sham acupuncture, these data were interpreted as two separate comparisons, combined with real or placebo NRT. We treated the arms using active NRT as a separate study (Clavel 1992 +NG). For the comparison of acupuncture with NRT, acupuncture plus placebo NRT was compared with sham acupuncture plus NRT. Georgiou 1999 evaluated two modes of electrical stimulus, two locations, and active/sham stimulation simultaneously in a 2x2x2 design: data for the two active groups (active stimulation at active location, using either modulated or continuous mode) were combined and compared with the combined data from all control groups.
Thirty‐five studies contributed data to analyses pooling short‐term outcomes. These included three (Labadie 1983; Wing 2010; Zhang 2013) which only assessed abstinence after six weeks but before six months. We included these in the short‐term outcome analysis rather than excluding them; analyses were not sensitive to their inclusion. Seventeen studies contributed data to long‐term analysis one of which did not contribute short term data (Docherty 2003). Table 3 displays lengths of follow‐up available for each included study, grouped by type of intervention.
1. Lengths of follow‐up available for included studies, grouped by intervention type.
| Study ID |
Short‐term outcomes (≤ 6 weeks after quit date) |
Long‐term outcomes (≥ 6 months after quit date) |
Notes |
| Acupressure | |||
| Li 2009 | x | Also in continuous stimulation (acupressure) subgroup | |
| Tian 1996 | x | x | |
| White 2007 | x | ||
| Wing 2010 | x | Short‐term follow up > 6 weeks (3 months from treatment) Also in continuous stimulation (acupressure) subgroup |
|
| Zhang 2013 | x | Short‐term follow up > 6 weeks (8 weeks) Also in continuous stimulation (acupressure) subgroup |
|
| Acupuncture | |||
| Bier 2002 | (x) | (x) | Data not consistent so not included in any meta‐analysis |
| Circo 1985 | x | ||
| Clavel 1985 | x | x | |
| Clavel 1992 | x | x | |
| Cottraux 1983 | x | x | |
| Gilbey 1977 | x | Also in continuous stimulation (indwelling needle) subgroup | |
| Gillams 1984 | x | x | Also in continuous stimulation (indwelling needle) subgroup |
| Han 2006 | (x) | Compares acupuncture with acupuncture, not included in any meta‐analyses | |
| He 1997 | x | x | Also in continuous stimulation (acupressure) subgroup |
| Huang 2012 | x | Also in continuous stimulation (acupressure) subgroup | |
| Labadie 1983 | x | x | Short‐term follow up >6 weeks (8 weeks) |
| Lacroix 1977 | x | ||
| Lagrue 1980 | x | ||
| Lamontagne 1980 | x | x | |
| Leung 1991 | x | x | |
| Martin 1981a; Martin 1981b | x | x | Also in continuous stimulation (indwelling needle) subgroup |
| Parker 1977a; Parker 1977b | x | Parker 1977a also in continuous stimulation (indwelling needle) subgroup | |
| Steiner 1982 | x | ||
| Vandevenne 1985 | x | x | |
| Vibes 1977 | x | Also in continuous stimulation (indwelling needle) subgroup | |
| Waite 1998 | x | x | Also in continuous stimulation (acupressure) subgroup |
| White 1998 | x | x | |
| Wu 2007 | x | x | Also in continuous stimulation (indwelling needle) subgroup |
| Electrostimulation | |||
| Antoniou 2005 | x | ||
| Aycicegi‐Dinn 2011 | x | ||
| Fritz 2013 | x | ||
| Georgiou 1999 | x | ||
| Pickworth 1997 | x | ||
| Scheuer 2005 | x | x | |
| Yeh 2009 | x | Also in continuous stimulation (acupressure) subgroup | |
| Laser therapy | |||
| Cai 2000 | x | ||
| Docherty 2003 | x | ||
| Kerr 2008 | x | x | |
We were unable to interpret the data from one study (Bier 2002) which reported a significant superiority in the quit rate after the combination of education and acupuncture when compared with acupuncture alone or education alone. However, there were inconsistencies in the data as presented which were not clarified by contact with the authors, and therefore it was not possible to extract reliable data from this study for the meta‐analysis.
Research in this area has been conducted over a long period. Four studies were published in the 1970s (Gilbey 1977; Lacroix 1977; Parker 1977a; Vibes 1977), ten in the 1980s (Circo 1985; Clavel 1985; Cottraux 1983; Gillams 1984; Labadie 1983; Lagrue 1980; Lamontagne 1980; Martin 1981a; Steiner 1982; Vandevenne 1985), eight in the 1990s (Clavel 1992; Georgiou 1999; He 1997; Leung 1991; Pickworth 1997; Tian 1996; Waite 1998; White 1998), and the remainder since 2000.
Initial group sizes for Kerr 2008, Martin 1981a and Vibes 1977 were not available in the published reports and data were obtained from the authors. Results for the different arms of Clavel 1992 were obtained from the authors.
Interventions
All acupuncture studies used a traditional approach to acupuncture in choosing points nominated as specific for smoking cessation. Five studies used facial acupuncture (Clavel 1985; Clavel 1992; Cottraux 1983; Lacroix 1977; Lagrue 1980) and ten used auricular acupuncture alone (Circo 1985; Gilbey 1977; Gillams 1984; Lamontagne 1980; Leung 1991; Martin 1981a; Martin 1981b; Parker 1977a; Parker 1977b; Waite 1998; White 1998; Wu 2007). All but three of these (Lamontagne 1980; Parker 1977b; White 1998) used some form of continuous stimulation, either needle or pressure device. Eight studies combined body and auricular acupuncture (Bier 2002; Han 2006; He 1997; Huang 2012; Labadie 1983; Martin 1981b; Steiner 1982; Vandevenne 1985). Three used continuous stimulation with either indwelling needles (Martin 1981a, Martin 1981b) or seeds (He 1997; Huang 2012). Vibes 1977 used facial, body, indwelling, and sham auricular acupuncture in different groups. This review's primary analysis included all forms of acupuncture (see Methods above).
The following studies used interventions related to acupuncture: Li 2009, Tian 1996, White 2007, Wing 2010, and Zhang 2013 used acupressure alone; Cai 2000, Docherty 2003, and Kerr 2008 used laser; Georgiou 1999, Pickworth 1997, and Scheuer 2005 investigated electrostimulation given over the mastoid bone; and Antoniou 2005, Aycicegi‐Dinn 2011, Fritz 2013 and Yeh 2009 gave electrostimulation to the ear (Yeh 2009 also used continuous acupressure stimulation).
Control interventions
All studies used a Traditional Chinese Acupuncture approach in regarding the point location of stimulation as significant and regarding non‐acupuncture points as a control intervention.
Three studies used points for the control group that were intended by the authors to be inactive but could be considered, using a neurological approach, to be active (see Methods). Gilbey 1977 used the auricular point 'Kidney' in the control group, which is reported in a review as used for smoking cessation (Zhang 1992). He 1997 used the point LI10 in the control group, which was used in treatment by another study (Jiang 1994). Lamontagne 1980 used body points including ST36 for relaxation as a control. The point ST36 is reported as an active treatment in the review by Zhang, and in one of the studies in this review (Vibes 1977). We tested the sensitivity of the pooled estimates to the exclusion of these studies
Patients in four control arms were given interventions that are of unknown effect: Circo 1985 compared acupuncture to medical treatment with vitamins and a herbal medicine, extract of hawthorn; Clavel 1992 compared acupuncture with a locked cigarette case controlled by a time‐switch; Cottraux 1983 compared acupuncture with placebo capsules; and Labadie 1983 compared acupuncture with 'medical treatment' consisting of advice, a benzodiazepine drug, lobeline, and a 'detoxicant'.
Four studies had more than one control group and therefore qualified for entry into more than one comparison: Cottraux 1983 compared acupuncture with a counselling and psychological approach, with waiting list, and with placebo capsules; Gillams 1984 compared acupuncture with sham acupuncture and with group therapy; Lamontagne 1980 compared acupuncture with sham body acupuncture and with a no‐treatment control arm; and Leung 1991 compared acupuncture with behaviour therapy and with waiting‐list control.
Han 2006 and Vibes 1977 compared different acupuncture approaches with each other.
Risk of bias in included studies
The risk of bias was judged unclear in many studies because of lack of detail in the reports, mainly associated with the facts that the older studies were published before current standards of reporting were widely applied, and several studies were published only as abstracts. In particular, methods of randomisation and allocation concealment could often not be assessed, and baseline comparisons between groups were often not reported. Apart from the lack of participant blinding in open studies, there was judged to be known risk of bias in the following studies: Antoniou 2005; Aycicegi‐Dinn 2011; Bier 2002; Fritz 2013; Gilbey 1977; Huang 2012; Kerr 2008; Labadie 1983; Lagrue 1980; White 2007; Zhang 2013 (Figure 2).
2.
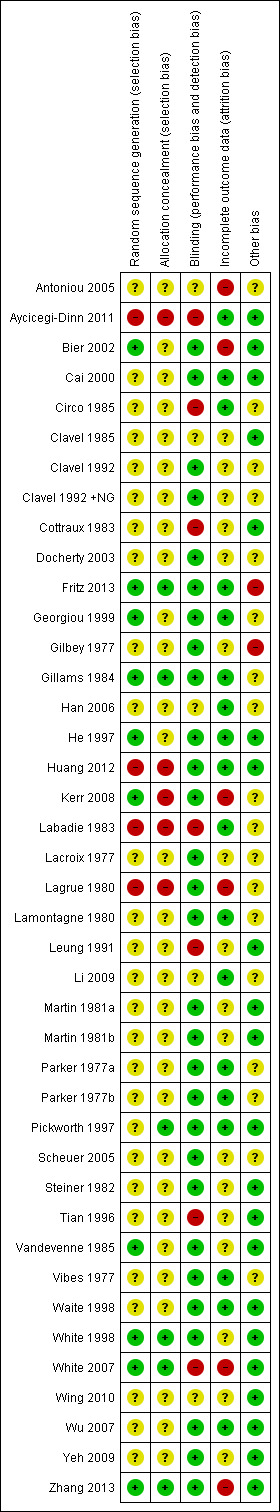
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
Summary of findings for the main comparison. Acupuncture compared to sham acupuncture for smoking cessation.
| Acupuncture compared to sham acupuncture for smoking cessation | ||||||
|
Patient or population: People trying to stop smoking
Intervention: Acupuncture Comparison: Sham acupuncture | ||||||
| Outcomes | Illustrative comparative rates* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed cessation rate | Corresponding rate | |||||
| Sham acupuncture | Acupuncture | |||||
| Smoking cessation Follow‐up: 6+ months | Study population | RR 1.1 (0.86 to 1.4) | 1892 (11 studies) | ⊕⊕⊕⊝ moderate1,2,3 | No evidence of long‐term benefit, though evidence of short‐term effect (RR 1.22, 95% CI 1.08 to 1.38) | |
| 108 per 1000 | 119 per 1000 (93 to 152) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias unclear for some domains in most studies; however, as pooled result did not detect an effect, risk of bias did not significantly alter authors' confidence in result. 2 There was clinical heterogeneity in the type and duration of acupuncture used, but little statistical heterogeneity (I² = 23%). 3 There was some evidence of funnel plot asymmetry.
Summary of findings 2. Acupressure compared to sham acupressure for smoking cessation.
| Acupressure compared to sham acupressure for smoking cessation | ||||||
| Patient or population: People trying to stop smoking Intervention: Acupressure Comparison: Sham acupressure | ||||||
| Outcomes | Illustrative comparative rates* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed cessation rate | Corresponding rate | |||||
| Sham acupressure | Acupressure | |||||
| Smoking cessation ‐ early Follow‐up: 3 to 12 weeks | Study population | RR 2.05 (1.11 to 3.77) | 312 (4 studies) | ⊕⊕⊝⊝ low1,2 | No studies report long‐term follow‐up. | |
| 84 per 1000 | 173 per 1000 (94 to 318) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 One study with significant effect had shortest follow‐up 2 Small number of small studies without long‐term follow‐up
Acupuncture compared with waiting list/no intervention
For short‐term outcomes, the results of two studies showed substantial statistical heterogeneity (I² = 84%) and therefore were not combined. Both studies used auricular acupuncture, but one used sustained treatment with indwelling studs (Leung 1991) and the other used auricular needling during treatment sessions only (Lamontagne 1980). The first, using sustained treatment, was positive whereas the second was negative, which suggests that some of the heterogeneity may be explained by clinical diversity (Analysis 1.1).
1.1. Analysis.
Comparison 1 Acupuncture vs waiting list/no intervention, Outcome 1 Short‐term smoking cessation.
Three studies provided long‐term outcome data (6 to 12 months). Combining these results did not demonstrate a significant effect of acupuncture (n = 393; risk ratio [RR] 1.79, 95% confidence interval [CI] 0.98 to 3.28, Analysis 1.2), and there was evidence of substantial heterogeneity (I² = 57%).
1.2. Analysis.
Comparison 1 Acupuncture vs waiting list/no intervention, Outcome 2 Long‐term smoking cessation.
Acupuncture compared with sham acupuncture
Short‐term outcomes
The 16 studies (19 comparisons, 2588 participants) which measured a short‐term outcome of acupuncture compared with sham acupuncture combine to give an overall positive result (RR 1.22, 95% CI 1.08 to 1.38) with moderate heterogeneity (I² = 46%) (Figure 3, Analysis 2.1). A funnel plot shows asymmetry, with larger studies typically showing smaller effects, and an absence of small negative studies (Figure 4). We did not conduct a subgroup analysis of high quality studies since no study was judged to be at low risk of all types of bias. Two studies individually detected a significant effect in favour of the intervention. The first, Lacroix 1977, had 117 participants and an RR of 2.58 (95% CI 1.66 to 4.01). We cannot identify any particular clinical or methodological features that might explain why this study detected a significant positive effect, although we note that the baseline characteristics of the groups are not reported so we cannot exclude confounding of the results by inequality between the groups in predictor variables. The risk of bias was unknown. The second, Huang 2012, had 60 participants and an RR of 5.67 (95% CI 1.85 to 17.34). It used an intensive intervention consisting of continuous acupressure and daily acupuncture, initially. This study was judged to be at high risk of bias.
3.

Analysis 2.1: Acupuncture vs sham acupuncture, Short‐term smoking cessation
2.1. Analysis.
Comparison 2 Acupuncture vs sham acupuncture, Outcome 1 Short‐term smoking cessation.
4.
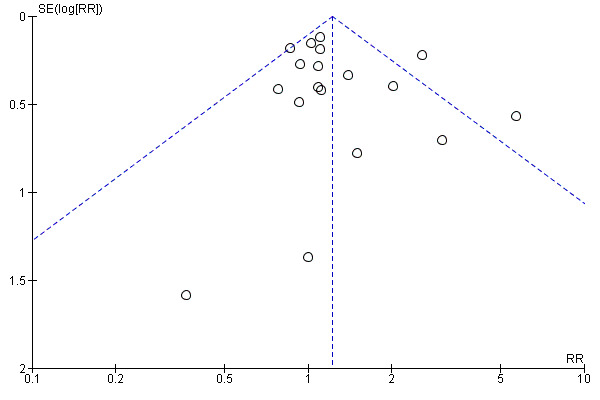
Funnel plot of comparison: 2 Acupuncture vs sham acupuncture, outcome: 2.1 Short‐term smoking cessation
A sensitivity analysis excluding three studies that used possibly active controls (Gilbey 1977; He 1997; Lamontagne 1980) produces a similar RR of 1.22 (95% CI 1.07 to 1.39) with moderate heterogeneity (I² = 50%). This suggests that the theoretical methodological problem of possibly active control interventions has little effect on the outcome in practice.
Longer term outcomes
The nine studies (11 comparisons, 1892 participants) with long‐term (6 to 12 month) outcomes do not show any relative effect of acupuncture compared with sham (RR 1.10, 95% CI 0.86 to 1.40, Figure 5, Analysis 2.2), with little evidence of heterogeneity (I² = 23%). As before, the subgroup that excluded possibly active controls had a similar pooled estimate.
5.

Analysis 2.2: Acupuncture vs sham acupuncture. Long‐term smoking cessation
2.2. Analysis.
Comparison 2 Acupuncture vs sham acupuncture, Outcome 2 Long‐term smoking cessation.
Acupuncture compared with other interventions
Acupuncture was less effective than NRT (two studies, n = 814, Analysis 3.1) both in the short term (RR 0.76, 95% CI 0.59 to 0.98) and in the long term (RR 0.64, 95% CI 0.42 to 0.98), with no heterogeneity. Acupuncture showed no difference of effect from counselling and psychological approaches (three studies, n = 396, Analysis 3.2) at either the short‐ (RR 0.95, 95% CI 0.72 to 1.26) or long‐term (RR 1.34, 95% CI 0.80 to 2.24) time points, but there was evidence of heterogeneity (I² = 43% for short‐ and I² = 64% for long‐term outcomes).
3.1. Analysis.
Comparison 3 Acupuncture vs other intervention, Outcome 1 NRT.
3.2. Analysis.
Comparison 3 Acupuncture vs other intervention, Outcome 2 Counselling and psychological approaches.
There were four trials of acupuncture compared with interventions of unknown effect (Analysis 3.3). In a large trial that was judged to be at risk of bias, acupuncture proved superior to a time‐locked cigarette case (Clavel 1985) in both the short term and long term. Acupuncture was superior to placebo capsules at end of treatment, though not in the long term (Cottraux 1983). Acupuncture was not different in effect from the use of illustration material (Circo 1985) or a combination medication product (Labadie 1983).
3.3. Analysis.
Comparison 3 Acupuncture vs other intervention, Outcome 3 Interventions of unknown effectiveness.
In the studies comparing different types of acupuncture (Table 4), body acupuncture in addition to auricular acupuncture was not more effective than auricular acupuncture alone (Han 2006). Acupuncture to the Zero point in the ear and classical body acupuncture appeared more effective than other approaches, but were not statistically compared (Vibes 1977).
2. Comparisons of different forms of acupuncture.
| Study | Type of acupuncture | N included | Not smoking (early) | Success rate |
| Han 2006 | body points only | 22 | 16 | 73% |
| Han 2006 | body and auricular points | 20 | 11 | 55% |
| Vibes 1977 | classical (body) points | 44 | 14 | 32% |
| Vibes 1977 | Zero point (ear) | 39 | 11 | 28% |
| Vibes 1977 | Lung point (ear) | 34 | 3 | 9% |
| Vibes 1977 | nose points | 48 | 4 | 8% |
| Vibes 1977 | sham control (hands/feet) | 30 | 2 | 7% |
Acupressure compared with usual care or advice only
Two studies compared acupressure with usual care or advice alone in the short term (Analysis 4.1). Their results show considerable heterogeneity (I² = 91%) so we did not combine them. One was a large trial using four ear points, and was positive in both short and long term (Tian 1996). The second was a small pilot study using one or two ear points, and showed no effect (White 2007) at short term, with no long‐term outcome.
4.1. Analysis.
Comparison 4 Acupressure vs waiting list/no intervention, Outcome 1 Short‐term smoking cessation.
Acupressure compared with sham acupressure
Comparing acupressure with sham, three studies (253 participants) combined showed that acupressure to the correct points was more effective for short‐term cessation than acupressure to points deemed ineffective (RR 2.54, 95% CI 1.27 to 5.08) (Analysis 5.1). No studies had long‐term outcomes.
5.1. Analysis.
Comparison 5 Acupressure vs sham acupressure, Outcome 1 Short‐term smoking cessation.
We found no studies comparing acupressure with other smoking cessation interventions.
Continuous auricular stimulation
Nine trials using acupuncture (Gilbey 1977; Gillams 1984; He 1997; Huang 2012; Martin 1981a; Martin 1981b; Parker 1977a; Vibes 1977; Waite 1998; Wu 2007), three using acupressure (Li 2009; Wing 2010; Zhang 2013), and one using electrostimulation (Yeh 2009) also used continuous stimulation. The stimulation was provided by indwelling needles in seven comparisons (Gilbey 1977; Gillams 1984; Martin 1981a; Martin 1981b; Parker 1977a; Vibes 1977; Wu 2007) and acupressure in the others
In the short term, continuous auricular stimulation was more effective than sham stimulation (13 studies, n = 1155, RR 1.69, 95% CI 1.32 to 2.16, I² = 16%, Analysis 6.1, Figure 6). However, for long‐term outcomes, pooled results from five studies (six comparisons, 570 participants) did not detect an effect (RR 1.47, 95% CI 0.79 to 2.74, I² = 22%, Analysis 6.2). In both analyses, there was evidence of funnel plot asymmetry, with larger studies typically reporting smaller effects (funnel plot for short‐term outcomes Figure 7).
6.1. Analysis.
Comparison 6 Continuous auricular stimulation vs sham stimulation, Outcome 1 Short‐term smoking cessation.
6.

Analysis 8.1: Continuous auricular stimulation vs sham stimulation. Short‐term smoking cessation
6.2. Analysis.
Comparison 6 Continuous auricular stimulation vs sham stimulation, Outcome 2 Long‐term smoking cessation.
7.

Funnel plot of continuous auricular stimulation vs sham stimulation, Short‐term smoking cessation
Laser therapy
There are no comparisons of laser therapy with waiting list or no intervention controls or with other interventions for smoking cessation. Two reports of studies comparing laser with sham laser showed considerable heterogeneity in their results (I² = 97%) and were not combined (Analysis 7.2). The heterogeneity may be due, at least partly, to diversity in the participants and dose of laser, and is discussed below.
7.2. Analysis.
Comparison 7 Laser therapy vs sham laser, Outcome 2 Long‐term smoking cessation.
Electrostimulation
There are no comparisons of electrostimulation with waiting list or with other interventions for smoking cessation. Electrostimulation was not more effective than sham electrostimulation either in the short term (six studies, n = 634, RR 1.13, 95% CI 0.87 to 1.46, Analysis 8.1) or the long term (two studies, n = 405, RR 0.87, 95% CI 0.61 to 1.23, Analysis 8.2).
8.1. Analysis.
Comparison 8 Electrostimulation vs sham stimulation, Outcome 1 Short‐term smoking cessation.
8.2. Analysis.
Comparison 8 Electrostimulation vs sham stimulation, Outcome 2 Long‐term smoking cessation.
Discussion
There is a lack of studies on acupuncture and related interventions for smoking cessation with large sample sizes and low risk of bias. This review is also generally limited by having to combine a wide range of interventions often used in combination. Further, the evidence does not have strong theoretical underpinning since interventions are based on traditional practice rather than neurophysiological knowledge. Below, we discuss the evidence in relation to both effectiveness (the overall effect including 'placebo' effects, tested by comparing with waiting list and with other intervention) and efficacy (comparing with sham) for each of the four related interventions, before commenting generally about possible mechanisms of action and difficulties in this research area.
Evidence of effectiveness and efficacy
We found inconsistent evidence on whether acupuncture is effective overall for smoking cessation when compared with no intervention, in open studies. The acupuncture methods used in the studies were dissimilar but not sufficiently different to explain the heterogeneity convincingly: positive results were associated with the use of indwelling needles (Leung 1991) and with three weekly treatment sessions (Cottraux 1983). We found no evidence that acupuncture was more (or less) effective than behavioural interventions used for smoking cessation. The combined results of two large studies (Clavel 1985; Clavel 1992) found acupuncture less effective than NRT, though neither study is free of bias, and in the first the acupuncture was given on only one occasion and so may have been inadequate (see below).
We found evidence of the efficacy of acupuncture compared with sham acupuncture immediately after the intervention (Figure 3) with a RR of 1.22, though there was moderate quality evidence of no effect at the long‐term follow‐up (Figure 5, Table 1). This evidence appears to suggest that acupuncture may have physiological effects relevant to smoking cessation. This result may underestimate the effect of acupuncture, since sham acupuncture may be an effective intervention, as has been suggested by three‐arm studies for painful conditions (Cummings 2009). No studies in this review compared acupuncture with both sham and with no intervention. The strength of the evidence is that it includes 19 comparisons and 2588 smokers from a wide range of countries and settings. However, the findings would be more convincing if a) the effect were sustained, b) the studies were free of bias, and c) the evidence showed consistency, or at least heterogeneity that could be explained. The limitations of the evidence are as follows. Firstly, the eight studies with long‐term follow‐up showed no effect. Both positive studies (Huang 2012; Lacroix 1977) had no long‐term follow‐up. Secondly, no study was judged to be free of the risk of bias (Figure 2). The two studies with least risk of bias were negative (Clavel 1992; White 1998), and the two positive studies were at risk of bias for two or more items (Figure 2). Thirdly, inspection of the forest plot (Figure 3) does not give the overall impression of evidence of an effect: results of twelve studies are very close to the zero line of nil effect, and the positive combined result is highly dependent on two clearly positive studies (Huang 2012; Lacroix 1977). Finally, the funnel plot (Figure 4) shows that larger studies are more likely to show no effect, which suggests the possibility of publication bias.
The combined evidence would seem stronger if the heterogeneity could be explained by the clinical technique used. The two significantly positive studies used different interventions: body acupuncture and continuous acupressure in Huang 2012 and facial acupuncture only in Lacroix 1977. The three studies with strong positive trends used other combinations of different techniques: He 1997 used body electroacupuncture, ear acupuncture and continuous acupressure; Waite 1998 used a single session of electroacupuncture to the ear with continuous stimulation; and Vibes 1977 used body, face, and auricular acupuncture in different groups. The one technique that appears promising is continuous stimulation: pooled results from 14 studies that used continuous stimulation, whether acupuncture or acupressure (Analysis 6.1), showed a positive effect of RR 1.69 (95% CI 1.32 to 2.16) compared with sham stimulation. The positive result persisted in the seven studies that used acupressure (RR 2.49, 95% CI 1.61 to 3.85) but not the seven that used indwelling needles (RR 1.24, 95% CI 0.91 to 1.69). This result suggesting that continuous stimulation could be a useful intervention should be interpreted with caution: there was no effect on long‐term outcomes, which indicate the value of the intervention in practice (Analysis 6.2). Furthermore, this analysis was not included in the original review protocol and was added in response to the large number of studies that used continuous stimulation as a second intervention. Inclusion of this analysis could be a bias in the review process, and the analysis could be regarded as exploratory ‐ although continuous stimulation was described as one of two 'basic techniques' in our Background, so it is logical to include its effectiveness as one of the study objectives.
For acupressure, we found conflicting evidence on acupressure compared with advice alone: one larger study was positive (Tian 1996) though with uncertain quality, and the negative study was a small pilot study (White 2007) not designed to test effectiveness. There was low quality evidence showing that acupressure was superior to sham acupressure in the short term, though of the three included studies, none was free of risk of bias and none included long‐term outcomes (Table 2). Thus we interpret the evidence as insufficient to make conclusions that would change practice, but sufficient to recommend further studies.
For laser stimulation, one study (Kerr 2008) is strongly positive at both short‐ and long‐term outcomes. Its results are inconsistent with the other two studies which show no trend. This heterogeneity may be explained by two factors. The studies differed in participants: Cai 2000 included adolescents smoking as little as five cigarettes a day, Docherty 2003 recruited adults from a socioeconomically deprived area, and Kerr 2008 included adults with no restriction. They also differed in dose of laser: Cai 2000 used 4 minutes at 3mW, whereas Kerr 2008 used 14 minutes at 50mW which is considerably higher; the dose used by Docherty 2003 is not reported in the report available. On this evidence, the effectiveness of laser stimulation for smoking cessation, at adequate dosage, justifies further investigation.
For electrostimulation, six studies are consistent in their results which did not detect an effect at short‐term outcomes, and there is no evidence of long‐term effect. This evidence gives confidence that electrostimulation, used in the locations and regimes tested here, does not have any effect beyond placebo for smoking cessation.
Possible mechanism of action
Overall, there is not sufficient evidence to rule out an effect of acupuncture, acupressure and laser stimulation on smoking cessation. We should consider their possible mechanism of action in relation to justifying further research. According to current theory, these interventions stimulate peripheral nerves to generate relevant effects in the central nervous system. Animal experiments have suggested that acupuncture might have effects on the acute withdrawal syndrome (Cheng 1980; Choy 1978; Han 1993; Ng 1975). In a classic paper, opioid peptides were released during the acute administration of acupuncture in association with relief of withdrawal symptoms in humans (Clement‐Jones 1979). Acupuncture can modify the nicotine‐induced locomotor activity and neural activity in the nucleus accumbens (Chae 2004), which is known to be a site that is crucial for chemical dependence. Other studies suggest that acupuncture may modulate dopamine release via the GABA mechanism (Yoon 2004; Yoon 2010), though other groups found evidence of enkephalin release (Liang 2010) which accumulates on repeated stimulation over three consecutive days, and yet other groups report serotonin (5‐hydroxytryptamine) release (Yoshimoto 2006). Brain imaging studies of acupuncture have generally focused on the limbic system in relation to pain control, though one study described fMRI (functional magnetic resonance) changes in the nucleus accumbens (Hui 2005).
While we await confirmation of these possible mechanisms and investigation of their clinical relevance, they do imply that any effect of acupuncture is likely to be via release of relevant neurotransmitters. This suggests that the duration of effect is likely to be no more than 24 hours and possibly considerably less. This has implications for both practice and research in this area.
Difficulties in this research area
Controlled trials of acupuncture are challenging in several ways, particularly defining adequate active interventions and inactive controls, and blinding participants. Clinical experience from the earliest observations in drug dependence suggests that adequate treatment involves frequent repetition ‐ at least once a day ‐ for withdrawal from opioid drugs (Smith 1988; Wen 1973). From our understanding of the possible mechanisms of action, adequate dosage with acupuncture for smoking cessation would include either several applications or a continuous stimulation. However, the evidence from the studies in this review does not give consistent support for the most effective form of intervention, presumably because the studies differ in other ways. Many studies used three weekly sessions, or indwelling needles over at least two weeks over the period of planned smoking cessation. Defining inactive controls for acupuncture is a perennial problem, since blinding of participants would seem to necessitate some form of needling. However, if the neurochemical release discussed above is a general effect of acupuncture‐like stimulation at any location (Lewith 1995), then any needle insertion in the control group is likely to be active, even if it is in a point that might be described by classically trained acupuncturists as 'not relevant for this indication'. Blunt, non‐penetrating needles have been used in research into pain control, but not yet in smoking cessation. It is challenging that, in view of the relatively small effect of acupuncture on smoking cessation, comparisons of different techniques and different controls would require large sample sizes.
Non‐pharmaceutical interventions such as those included in this review are popular and safe in the hands of trained practitioners provided that relevant precautions are taken to avoid infection. Economic data were not considered in this review, but some of the techniques related to acupuncture may have the potential to compete economically with other methods of smoking cessation such as pharmaceutical products and psychological interventions.
Agreements and disagreements with other studies or reviews
Vincent and Richardson found that acupuncture appeared to be as effective as other methods in the initial stages of nicotine withdrawal. However there was uncertainty as to what the actual stimulation contributed and whether acupuncture helped prevent relapse (Vincent 1987). Schwartz 1988 found no evidence of a specific effect. Brewington 1994 concluded that acupuncture might be of limited assistance in withdrawal.
Ter Riet 1990 performed a criteria‐based systematic review of randomized controlled trials and concluded that on balance there was no evidence that acupuncture was efficacious in the treatment of nicotine addiction. Lewith 1995 criticised this review and argued that trials in which the controls received needling in inappropriate sites were likely to underestimate the effects of acupuncture: the control procedure was not inactive, since needling random sites could trigger the release of endorphins. He concluded that acupuncture is as effective as NRT.
Law and Tang performed a meta‐analysis of the trials listed in MEDLINE, concluding that acupuncture had "little or no effect" (Law 1995). Ashenden and Silagy (Ashenden 1997) included ten studies in a systematic review looking at the long‐term success of acupuncture in smoking cessation; nine of the studies could be combined in a meta‐analysis which concluded that, while acupuncture appeared to be promising, there was insufficient evidence to recommend it as an effective form of therapy. A meta‐analysis of 19 studies concluded that acupuncture was more effective than no, or minimal intervention, and sham acupuncture (Castera 2002).
Two recent systematic reviews of acupuncture for smoking cessation have reached different conclusions from ours. Cheng 2012 addressed a different question, combining all forms of acupuncture‐related stimulation, and all forms of control intervention in a single analysis at each time point. The review also addressed cigarette consumption. The analysis of 20 studies found that acupuncture was superior to all controls for smoking cessation (RR 1.24 immediately after treatment, 1.70 at 3 months, and 1.79 at 6 months), leading to the conclusion that "acupuncture combined with smoking cessation education or other interventions can help smokers to eschew smoking during treatment and to avoid relapse after treatment." Our review groups studies according to control intervention, addressing different research questions, which likely explains the differences in our results. Tahiri 2012 pooled long term outcomes from six sham‐controlled studies to give an odds ratio of 3.53 with 95% CI 1.03 to 12.07. Both reviews included Bier 2002, not used in a meta‐analysis here because of uncertainty about data; and both included Kerr 2008 which was categorised here as laser therapy rather than acupuncture. These uncertainties in both reviews do, in our view, preclude making conclusions about the benefits of any particular intervention related to acupuncture, and in that sense are not in conflict with our own conclusions.
Authors' conclusions
Implications for practice.
There is no bias‐free, consistent evidence that acupuncture, acupressure, laser therapy, or electrostimulation are effective interventions for smoking cessation. Acupuncture is less effective than nicotine chewing gum.
Implications for research.
The current evidence justifies further studies of acupuncture, acupressure, particularly sustained acupressure, and laser stimulation for smoking cessation provided that the intervention is given in adequate dosage for a sufficient period of time and compared with either no treatment, or another active intervention, or (for efficacy studies) a form of intervention that is likely to be inactive. It is relevant to continue research into acupuncture and related interventions for smoking cessation since they are popular and safe when correctly applied; however, acupuncture alone is likely to be less effective than evidence‐based interventions such as NRT. Studies could also consider economic evaluation, and the potential different roles of acupuncture used as part of a stages‐of‐change based approach. The current evidence does not support further studies of electrostimulation used in the locations and regimes tested in this review.
Feedback
Comment from Nguyen and colleagues (August 2002)
Summary
1. We wish to inform you of a randomized controlled trial (RCT) eligible in the review : Vibes J. Essai thérapeutique sur le r"le de l'acupuncturedans la lutte contre le tabagisme. Acupunct 1977;51:13‐20.
2. Three studies included in the comparison "acupuncture versus sham acupuncture" set methodological problems :
a.Gilbey 1977 should be excluded. Not only because "some authors regard kidney point (used as a control) as an effective treatment for dependency", but above all because kidney ear point is used in several clinical studies for smoking cessation. For instance, in Cui review on acupuncture for smoking abstinence [1], three studies used kidney ear point [2‐4]. b.Lamontagne 1980 should also be excluded. "Acupuncture therapy for relaxation" as control cannot be considered as sham acupuncture. That intervention uses point ST36, also used in one study of Cui review [5] and in one RCT [6] included in the meta‐analysis. Vibes RCT tests ST36, LV3, LI4 GB8, presented as "equilibrating and/or antitoxic general acting intervention". That acupuncture intervention revealed to be superior to sham acupuncture. c.In Martin 1981(a), there is discrepancy between the control group (and the total size) in the table "characteristics of included studies" and the data used in the graph : the selected control group is in fact the group "P + stimulation" of the original study. This group includes electro‐acupuncture at LI4 and "tongue" ear point. For the same motives as in the two previous studies, this control group cannot be chosen as sham acupuncture. LI4 is used in two studies in Cui review [5,7], in two RCT included in the meta‐analysis [8,9] and in Vibes study.
From a general point of view, it seems inadequate to select as sham acupuncture interventions using points employed in clinical studies dealing with the same disease. This criterion (a practical and effective use of a point) is stronger than the theoretical expert opinion, and should lead to exclude these studies in a comparison acupuncture versus sham acupuncture.
3. In the comparison "acupuncture versus sham acupuncture‐early", Waite 1998 trial is omitted without explanation. This trial has data non biochemically validated available at two weeks, that seem to meet the criteria of the review.
4. We also draw your attention to the problematic data following : a. in Parker 1977(a) and (b), the data to be selected for the size of groups seem to be the concordant ones appearing in the text and figure I (Parker (a) 18 patients: 9 for acupuncture, 9 for sham; Parker (b) 23 patients: 11 for acupuncture, 12 for sham) and not data in table 1. b. In the comparison "01 ‐Acupuncture versus sham acupuncture, 01 ‐smoking cessation early": He 1997 8/26 in acupuncture group, not 7/26.
5. In references, Lagrue 1977 is in fact Lagrue 1980.
6. Pickworth 1997 trial uses "the application of electrical currents from surface electrode...placed on each mastoid process". The authors don't identify any acupuncture points, never use the word "acupuncture" and don't mention any acupuncture study in bibliography. For that motives, including this type of studies in a review "Acupuncture for smoking cessation" seems inadequate.
From remarks 1‐4, comparison "acupuncture versus sham acupuncture" should be reconsidered.
1‐ Cui M. Advances in studies on acupuncture abstinence. J Trad Chin Med 1995;15(4):301‐7.
2‐ Cai ZM. [Ear points arousing propagated sensation for stopping smoking in Senegal]. Fujian J Trad Chin Med 1986;17(5):22‐4.
3‐ Li GJ. [33 cases of smoking cessation treated with ear point pressure]. Jianxi J Trad Chin Med 1990;21(4):40.
4‐ Requena Y, Michel D, Fabre J, Pernice C, Nguyen J. Smoking withdrawal therapy by acupuncture. Am J Acupunct 1980;8(1):57‐63.
5‐ Sacks LL. Drug addiction, alcoholism, smoking, obesity treated by auricular staplepuncture. Am J Acupunct 1975;3(2):147‐151.
6‐ Vandevenne A, Rempp M, Burghard G, Kuntzmann Y, Jung F. Etude de l'action spécifique de I'acupuncture dans la cure de sevrage tabagique. Sem H"p Paris 1985;61(29):2155‐60.
7‐ Cheung CKT. Acupuncture treatment and the preventive applications for cigarette smokers. in: Compilation of the abstracts of acupuncture and moxibustion papers. Proceedings of the 1st World Conference on Acupuncture‐Moxibustion. 1987 Nov 22‐26:Beijing,China. p.76‐7.
8‐ Steiner RP, Hay DI, Davis AW. Acupuncture therapy for the treatment of tobacco smoking addiction. Am J Chin Med 1982;10(1‐4):107‐21.
9‐ Labadie JC, Dones JP, Gachie JP, Freour P, Perchoc S, Huynh‐Van‐Thao JP. Désintoxication tabagique : acupuncture et traitement médical.Résultats comparés à 1 an sur 130 cas. Gaz Med Fr 1983;90(29):2741‐7.
I certify that I have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of my criticisms.
Reply
We are grateful to Dr Nguyen for his detailed comments.
1.Thank you for information about this trial of which we were unaware. We shall consider it for inclusion in the next review. 2.The question of appropriate and inappropriate controls runs through the whole of acupuncture research and will not be satisfactorily solved until 'Phase I & II' type studies are conducted. Without hard data, therefore, we took the pragmatic decision to accept each original author's view of what was an acceptable control. We feel it would be wrong to overturn the author's view of the sham, often very well considered and referenced, without strong reason to do so. We acknowledge that this might result in reducing the effect size for acupuncture. However, there are other biases affecting the same issue, such as the psychological equivalence of the sham control (e.g. do acupuncture studs placed in the knee have an equal psychological effect to those in the ear?). The question of whether 'acupuncture for relaxation' was an inactive control was problematic; however, there are many ways of producing 'relaxation' none of which is known to have any benefit in smoking cessation. On balance, then, we decided to keep this group in the analysis. 3.Thank you for pointing out the review omits some data reported in the Waite trial at 2 weeks. I have checked our extraction records and find that neither of the reviewers involved extracted these data, and I guess this is probably because they are only referred to very indirectly in the text, in comparison to the validated data. We therefore did not discuss whether these data are admissible. We note that they were obtained by telephone, and subsequently in the same trial, 2 out of 7 who claimed on the telephone to have stopped smoking actually were still smoking. It seems probably that all verbal reports of smoking are subject to error, but those made face‐to‐face may be more reliable than those made over the telephone; we shall discuss whether to include the latter in the next revision. 4.a) there is a clear discrepancy in group sizes in the report by Parker. We shall reconsider these extracted data at the next revision. b) In the report by He, although 8 subjects reported smoking cessation, only 7 were confirmed biochemically (see 'Tobacco consumption versus cotinine concentration'). 5.Thank you, we shall correct this in the next revision. 6.At the time of our 2nd revision conducted earlier this year, the Cochrane Group recommended including other stimulation techniques, on the basis that they should be reviewed and did not have any other natural home. We did not consider changing the review's title, but will consider this for the next revision. Thank you for the suggestion.
A R White, H Rampes, E Ernst
Contributors
Johan Nguyen (Marseilles France), Philippe Castera (Bordeaux, France), Jean‐Luc Gerlier (Annecy, France)
What's new
| Date | Event | Description |
|---|---|---|
| 14 January 2014 | New citation required but conclusions have not changed | No major change to conclusions |
| 26 November 2013 | New search has been performed | Searches updated. Five new studies included, none with long‐term data. |
History
Protocol first published: Issue 1, 1997 Review first published: Issue 1, 1997
| Date | Event | Description |
|---|---|---|
| 13 April 2011 | Amended | Graph labels corrected (reversed) for Figure 4/Analysis 3.1, Analysis 4.1, Analysis 6 & Analysis 10.2 |
| 24 November 2010 | New search has been performed |
|
| 23 November 2010 | New citation required but conclusions have not changed | A Chinese author has joined the review team |
| 17 June 2008 | Amended | Converted to new review format. |
| 24 October 2005 | New citation required but conclusions have not changed | Title changed to include techniques related to acupuncture. Two newly discovered study included (Bier 2002; Vibes 1977). Outcome time‐points now limited to two: immediately after treatment, and last from 6 months up to one year. Studies in which acupuncture is used as an adjunct (to NRT or counselling) are now analysed separately. Comparisons modified: acupuncture now compared to other effective interventions (NRT, counselling) separately, and no longer compared with interventions of no known effect. The Mantel‐Haenzel method now used for primary method for combining studies. Subgroup analyses performed excluding studies in which the control intervention included points used as active in other studies. Analysis comparing the effectiveness of different styles of intervention is now limited to direct comparisons. |
| 18 February 2002 | New citation required but conclusions have not changed | Inclusion criteria for studies have been widened to cover acupressure, laser therapy, and cranial electrostimulation; which are stimulation therapies related to acupuncture and used for smoking cessation. The age limit for study participants has been removed to increase the relevance of the review. |
Acknowledgements
We are grateful to Ruth Ashenden and Chris Silagy for kindly giving us access to their own review of acupuncture in smoking cessation as the basis for much of the original version of this review.
We are grateful to Prof P Waite of the University of New South Wales, Australia, for providing further data for the Martin 1981a study; and to Dr F Clavel of the Unite de Recherche en Epidemiologie des Cancers, Villejuif France for providing data for the Clavel 1990 study.
We are grateful to Jie Shen, Yi‐Man Au, Jongbae Park and Sun Jin for translating and extracting data from the original Chinese reports.
We are grateful to Johan Nguyen for perceptive comments on this and an earlier version of this review, for providing one trial report of which we were not aware (Vibes 1977), and for contacting that author to obtain baseline group sizes.
Data and analyses
Comparison 1. Acupuncture vs waiting list/no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Long‐term smoking cessation | 3 | 393 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.98, 3.28] |
Comparison 2. Acupuncture vs sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 19 | 2588 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.08, 1.38] |
| 2 Long‐term smoking cessation | 11 | 1892 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.86, 1.40] |
Comparison 3. Acupuncture vs other intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 NRT | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Short‐term smoking cessation | 2 | 914 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.59, 0.98] |
| 1.2 Long‐term smoking cessation | 2 | 914 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.42, 0.98] |
| 2 Counselling and psychological approaches | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Short‐term smoking cessation | 3 | 396 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.72, 1.26] |
| 2.2 Long‐term smoking cessation | 3 | 396 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.80, 2.24] |
| 3 Interventions of unknown effectiveness | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Short‐term smoking cessation | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Long‐term smoking cessation | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Acupressure vs waiting list/no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Long‐term smoking cessation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
4.2. Analysis.
Comparison 4 Acupressure vs waiting list/no intervention, Outcome 2 Long‐term smoking cessation.
Comparison 5. Acupressure vs sham acupressure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 3 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 2.54 [1.27, 5.08] |
Comparison 6. Continuous auricular stimulation vs sham stimulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 14 | 1155 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.32, 2.16] |
| 1.1 Indwelling needles | 7 | 659 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.91, 1.69] |
| 1.2 Continuous acupressure | 7 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.73 [1.78, 4.18] |
| 2 Long‐term smoking cessation | 6 | 570 | Risk Ratio (IV, Fixed, 95% CI) | 1.47 [0.79, 2.74] |
| 2.1 Indwelling needles | 4 | 446 | Risk Ratio (IV, Fixed, 95% CI) | 1.20 [0.62, 2.32] |
| 2.2 Continuous acupressure | 2 | 124 | Risk Ratio (IV, Fixed, 95% CI) | 9.45 [1.26, 70.92] |
Comparison 7. Laser therapy vs sham laser.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Long‐term smoking cessation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
7.1. Analysis.
Comparison 7 Laser therapy vs sham laser, Outcome 1 Short‐term smoking cessation.
Comparison 8. Electrostimulation vs sham stimulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Short‐term smoking cessation | 6 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.87, 1.46] |
| 2 Long‐term smoking cessation | 2 | 405 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.61, 1.23] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Antoniou 2005.
| Methods | Randomized trial of electrostimulation Country: Greece Recruitment. no details |
|
| Participants | Smokers (no other details) | |
| Interventions | Single application of an electrical probe to the ear, (duration not stated) giving a) electrical stimulus with current intensity between 12‐20 mAmp, or b) no current |
|
| Outcomes | Smoking cessation at 12 months, no details on how data were collected or verified | |
| Notes | Abstract only. 390 smokers randomised, but group sizes at baseline not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomized in a 2:1 manner |
| Allocation concealment (selection bias) | Unclear risk | no details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | described as 'double‐blind' in the title, but stimulation was at a level that could be detected in the intervention group; blinding was not checked |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 390 smokers enrolled, 339 evaluated. No group size at baseline so dropouts cannot be accounted for by allocation group |
| Other bias | Unclear risk | no baseline details |
Aycicegi‐Dinn 2011.
| Methods | Randomized trial of electrostimulation Country: Turkey Recruitment: media advertisements & personal contact |
|
| Participants | 47 smokers aged 18 to 65 scoring ≥5 on FTND | |
| Interventions | a) Three sessions of auriculotherapy with electrical stimulation (points, stimulation parameters and duration not specified; use of surface electrodes implied, not stated; not stated whether uni‐ or bilateral) at 0, 2 days & 3 weeks b) Sham therapy (device turned off) on same schedule |
|
| Outcomes | Cessation 30 day after last treatment. CO validation planned but not used due to low quit rates. Average CO levels reported | |
| Notes | Controls offered active treatment after 3rd session so longer term outcomes not used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "we were forced to match participants on two key variables (i.e., age and educational level) after approximately 30 patients had been [randomly] assigned to treatment or placebo groups" |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding (performance bias and detection bias) All outcomes | High risk | "after the initial treatment session, research technicians were not blind to group status. Research Technicians were not aware of the patients’ group status when conducting interviews and administering measures during the initial baseline assessment and treatment session." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 active group lost at 30 day follow‐up |
| Other bias | Low risk | No significant differences between groups; but "placebo group more likely to report that their spouses/partners used tobacco" (ns trend) |
Bier 2002.
| Methods | Randomized trial of acupuncture Country: United States Recruitment: media advertisements |
|
| Participants | 141 smokers aged 18 or over, at least one previous attempt to stop, no major medical condition, not taking listed drugs e.g. phenothiazines, ephedrine | |
| Interventions | a) true acupuncture b) true acupuncture and intensive education programme c) sham acupuncture plus intensive education programme True acupuncture consisted of 5 auricular points and LI4. Sham acupuncture consisted of sham points 5mm away from real points. In both groups, needles were inserted for 30 minutes, and not stimulated. Acupuncture and sham were given in 20 sessions in 4 weeks. Educational programme was 7 x 1.5 hour sessions over 5 weeks | |
| Outcomes | Reported smoking cessation at 1, 3, 6, 12, 15 and 18 months. Outcome not validated. Percentage decrease in cigarette consumption also reported. Depression and anxiety scores analysed, not reported in detail. | |
| Notes | Data inconsistent and cannot be interpreted, not included in meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | 'Randomization ... conducted by a research associate blind to treatment assignment' |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Groups b) and c) blinded: 'participants remained unaware of their [acupuncture] treatment group assignment' |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Numbers lost substantially different in different groups |
| Other bias | Low risk | No baseline differences for important variables |
Cai 2000.
| Methods | Randomized trial of laser therapy Country: Singapore Recruitment: not stated |
|
| Participants | 330 smokers, aged 12 to 18 smoking 3 yrs and minimum 5 cigs/day | |
| Interventions | a) laser (wavelength 633 nm, 2.5‐3mW for total 4 minutes) or b) deactivated laser to points in left ear, 12 times in 4 weeks. Patients wore blindfolds during treatment. | |
| Outcomes | Smoking cessation immediately after and 3 months later reported. Validation: expired air CO concentration taken after 6th and 11th treatments (not at the first measurement point, which was after 12th treatment) and at 3 month follow‐up | |
| Notes | Therapist not blinded: blinded assessor. Some indexing systems cite authors as Yiming C, Changxin Z, Ung WS, Lei Z, Kean LS |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomization, no details given |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blindfolded; independent observer not involved in the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rates 19%, similar in both groups |
| Other bias | Low risk | No meaningful differences in baseline variables |
Circo 1985.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: Italy Recruitment: from patients with cardiovascular disorders, method of recruitment unclear |
|
| Participants | 90 adults (80 male), no inclusion or exclusion criteria reported | |
| Interventions | All participants received information and personalized advice, in addition to: a) illustration material b) medical treatment combining quinine ascorbate, vitamins and herbal extract (hawthorn), for 30 days c) auricular acupuncture to 9 ear points ('Nogier' anti‐smoking programme) given for 15 minutes, 6 hours after stopping smoking and repeated after 4 and a further 7 days; combined with 3 indwelling auricular needles for 15 days. Other ear points (Shenmen, Sympathetic, Lung) could be added bilaterally | |
| Outcomes | Reported cessation, time‐point unspecified (we assume end‐of‐treatment) Validation: none reported | |
| Notes | [in Italian]. Combine groups a) and b) as Intervention of unknown effectiveness | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported: 'suddivisi in modo random' |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes reported for all included smokers |
| Other bias | Unclear risk | No baseline variables reported |
Clavel 1985.
| Methods | Randomized trial of acupuncture Country: France Recruitment: Community volunteers, per advertisement |
|
| Participants | 651 adults smoking >5 cigs/day | |
| Interventions | a) facial acupuncture using two points bilaterally, single session b) nicotine gum ‐ 105 pieces of 2mg gum c) cigarette case with lock controlled by time‐switch All groups also received 3 one‐hour sessions of group therapy in first month | |
| Outcomes | Sustained cessation at 1 and 13 months Validation: none at 1 month; at 13 months, expired air CO concentration was tested in half of those claiming success (method of selection not reported) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Balanced randomization' no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants not blinded. No report of blinding observer |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropout rates over 80%, higher in control group |
| Other bias | Low risk | No significant differences in baseline variables |
Clavel 1992.
| Methods | Randomized trial of acupuncture Country: France Recruitment: Community volunteers responding to circulated leaflet 2x2 factorial design (Smokers in this study who were randomized to active nicotine gum are represented by the study labelled 'Clavel 1992 +NG') |
|
| Participants | 515 adults aged over 18, smoking >10 cigs/day | |
| Interventions | a) facial acupuncture to two points (GB8 and Bitong), with placebo nicotine gum b) sham acupuncture (wrong points 2cm from the above), with placebo nicotine gum Acupuncture given on days 0, 7 and 28 | |
| Outcomes | Sustained abstinence at 1 and 13 months. (Outcome at 4 years reported in Clavel 1997) 'Need for cigarette' estimated weekly for 1 month Validation: nil | |
| Notes | This study was first reported in French as Clavel 1990 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: 'Tirés au sort' |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Factorial, double‐dummy design; described as double blind; no details of blinding of the observer |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 80% dropout at one month |
| Other bias | Unclear risk | No description of baseline differences |
Clavel 1992 +NG.
| Methods | Randomized trial of acupuncture Country: France Recruitment: Community volunteers responding to circulated leaflet 2x2 factorial design (Smokers in this study who were randomized to placebo nicotine gum are represented by the study labelled 'Clavel 1992') |
|
| Participants | 481 adults aged over 18, smoking >10 cigs/day | |
| Interventions | a) facial acupuncture to two points (GB8 and Bitong), with active nicotine gum (2mg dose, up to 30 pieces/day, during first 6 months) b) sham acupuncture (wrong points 2cm from the above), with active nicotine gum (administration as above) Acupuncture given on days 0, 7 and 28 | |
| Outcomes | Sustained abstinence at 1 and 13 months. (Outcome at 4 years reported in another publication) 'Need for cigarette' estimated weekly for 1 month Validation: nil | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: 'Tirés au sort' |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Factorial, double‐dummy design; described as double blind; no details of blinding of the observer |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 80% dropout at one month |
| Other bias | Unclear risk | No description of baseline differences |
Cottraux 1983.
| Methods | Randomized trial of acupuncture Country: France Recruitment: Community volunteers responding to TV and radio adverts |
|
| Participants | 558 French citizens, aged 18‐50, smoking >10 cigs/day for 2 years | |
| Interventions | a) facial acupuncture, 3 weekly sessions b) behaviour therapy, weekly for 3 weeks c) placebo capsules prescribed at 2 consultations, labelled 'Medel 50' with instructions to avoid alcohol and stating that an overdose would result in gastric side‐effects d) waiting‐list control (assessed at 12 months only) |
|
| Outcomes | Sustained abstinence at 2 weeks, and 3, 6, 9 and 12 months Validation: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization stratified by presence of smoker at home, but no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study, though the observers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5% lost to follow up, 5% lost to follow up, included in ITT analysis |
| Other bias | Low risk | Groups balanced at baseline for several variables |
Docherty 2003.
| Methods | Randomized trial of laser therapy Country: Scotland Recruitment: via social marketing campaign & general practitioners (GPs) |
|
| Participants | 355 smokers from a community with high levels of social deprivation, No other details in abstract | |
| Interventions | a) Laser therapy. Duration and number of sessions not specified
b) Placebo laser All participants received counselling and access to a telephone helpline |
|
| Outcomes | Cessation at 6 and 12 months, CO measured, cut off not specified | |
| Notes | Abstract only. No further information available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized, no details given |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | 'Subjects and laser therapist blind' |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No description of dropouts or explanation for different group sizes |
| Other bias | Unclear risk | No baseline information reported |
Fritz 2013.
| Methods | Randomized trial of electrostimulation Country: USA Recruitment: Veterans Affairs Medical Centres |
|
| Participants | 152 military veterans aged ≥19, smoking ≥10 cpd | |
| Interventions | a) 5 weekly 20 min sessions of auriculotherapy (80Hz; Lung, Shen Men, Nicotine, Point Zero, and Palate), bilateral b) Sham auriculotherapy (unit disabled) All participants attended a stop smoking class before enrolment |
|
| Outcomes | Cessation at week 6 (point prevalence) Validation: urine cotinine (<200 ng/mL) |
|
| Notes | Cotinine based abstinence were higher than self reported (i.e. some people admitting smoking did not have cotinine levels above cut off) so self reported used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Permuted block assignments were generated … from a random‐number generator in advance of the trial’s start date." |
| Allocation concealment (selection bias) | Low risk | "Treatment assignment was indicated inside sealed, sequentially numbered opaque envelopes, opened … at the time of randomization." |
| Blinding (performance bias and detection bias) All outcomes | Low risk | All personnel with patient access remained blinded to which machine had been altered and which provided the stimulation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop out rate low and similar between groups, analysis not sensitive to alternative assumptions |
| Other bias | High risk | "Intervention group reported higher motivation to quit (p = 0.003). More patients in the active group (67%) believed they received the intervention than those in the placebo group (46%) (P = 0.03) at week 6." |
Georgiou 1999.
| Methods | Randomized trial of electrostimulation Country: England Recruitment: general public, nursing staff, government employees 2x2x2 factorial design to test the following factors: electrical stimulation; stimulation frequency (constant or modulated); location (mastoid process as active, back as the control) |
|
| Participants | 265 adults smoking at least 10 cigs/day for 1 year | |
| Interventions | Either electrical stimulation (0.150 msec biphasic pulse, 0.5 to 0.8 mA into 1 KΩ load) or sham (control, no output) stimulation; with either continuous 10Hz or modulated 7‐14Hz current (both active); to disposable pre‐gelled electrodes placed on either mastoid (active) or upper back (location control); total of 8 groups Active groups: a) modulated current to mastoid process b) continuous current to mastoid Control groups: c) modulated current to back d) continuous current to back. e) sham modulated current to mastoid f) sham modulated current to back g) sham continuous current to mastoid h) sham continuous current to back. After initial stimulation, home use as required for 7 days | |
| Outcomes | Smoking cessation at end of treatment, validated by expired air CO; withdrawal symptoms by VAS; follow‐up data were collected for up to 12 months, but data are not presented by group | |
| Notes | 18% dropouts, numbers in each group are unknown. Follow‐up data given as aggregate only. No significant differences. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participant blinded. 'Treatment was administered by a single clinician blinded ... to ... treatment' |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts 18% 'Atrrition rates did not differ significantly across treatment conditions' |
| Other bias | Unclear risk | No description of baseline differences between treatment groups |
Gilbey 1977.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: Canada Recruitment: Community volunteers responding to newspaper adverts |
|
| Participants | 92 subjects aged 30‐39 who smoked >15 cigs/day for 3 years | |
| Interventions | a) indwelling needle in active auricular point ('Lung') for 1 week b) indwelling needle in inactive auricular point ('Kidney') for 1 week | |
| Outcomes | Sustained abstinence at 1 week, 1 month and 3 months Validation: none | |
| Notes | Some authors regard 'Kidney' point (used as a control) as an effective treatment for dependency | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly assigned', no details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and person collecting the follow‐up data were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on dropout rate |
| Other bias | High risk | 39% of treatment group and 65% of control group reported that they had been advised by their doctor to stop smoking |
Gillams 1984.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: UK Recruitment: volunteers responding to poster in health centre |
|
| Participants | 81 adults smoking >50 cigs/week for 5 years | |
| Interventions | a) indwelling needle in active auricular point ('Lung') for 4 weeks b) indwelling needle in inactive auricular point (as far from 'Lung' as possible) for 4 weeks c) group therapy sessions, one hour/ week for 4 weeks | |
| Outcomes | Sustained abstinence at 4 weeks, 3 months, and 6 months Validation: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer programme |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes containing cards defining the treatment group |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants in the two acupuncture groups blinded. Acupuncturist not blinded, and no blinded observer |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data collection was completed for all patients entered into the study |
| Other bias | Unclear risk | No report of baseline differences |
Han 2006.
| Methods | Randomized trial of acupuncture Country: Heilongjiang province, China Recruitment: Hospital based acupuncture clinic |
|
| Participants | 42 participants (25 male, 17 female); age:19‐72 (female), 23‐70 (male). Average age: 40 years; history of smoking > 10 years; 20‐40 cigarettes per day | |
| Interventions | 10 day course of treatment in both conditions a) body + auricular acupuncture. Body points: tianmi point (the sensitive point on the line of lieque point and yangxi point); auricular points: mouth, lung, pizhixia, neifenmi, heart, thirst points b) auricular acupuncture. Auricular points: mouth, lung, pizhixia, neifenmi, heart, thirst points. | |
| Outcomes | Abstinence at end of treatment sustained until 1 month follow‐up | |
| Notes | Acupuncture vs acupuncture [in Chinese] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated, no details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No cases lost to follow‐up |
| Other bias | Unclear risk | No information |
He 1997.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: Norway Recruitment: employees recruited by internal advertisement through occupational health service |
|
| Participants | 46 adults smoking for at least 5 years, daily average of 10‐30 cigarettes in the last year; no other form of treatment for smoking cessation: no current acupuncture Exclusions: diabetes, coronary heart disease, pregnancy, breast‐feeding | |
| Interventions | Both groups received a combination of body electroacupuncture, ear acupuncture and ear acupressure: a) using genuine points described for smoking cessation: Body: LU6, LU7; Ear: Shenmen, mouth, lung; Ear sustained acupressure: Shenmen, mouth, lung, trachea, hunger, endocrine b) using sham points described for treating musculoskeletal conditions: Body: LI10, TE8; Ear: knees, lumbar vertebra, neck; Ear sustained acupressure: knees, lumbar vertebra, neck, shoulder, shoulder joint, buttock. 6 treatments over 3 weeks Manual and electrical stimulation were the same in the 2 groups In addition, 6 plant seeds were placed on either a) 'correct' or b) 'incorrect' points in the ear, according to group, and retained in place with adhesive tape: subjects were instructed to press on each seed 100 times on 4 occasions each day | |
| Outcomes | Abstinence at 1 week and 8 months after the last acupuncture treatment (sustained at each previous point). Outcomes at 5 years are also reported. Validation: cessation confirmed by serum cotinine and thiocyanate concentrations. (Serum concentrations of fibrinogen and lipid peroxide were also measured) Daily cigarette consumption, taste for tobacco and desire to smoke were assessed by questionnaire | |
| Notes | Standardized interaction
8 month data used in 6 month meta‐analysis. 5 yr data used in 1 yr + comparison does not include participants lost to follow‐up due to change of address etc LI10 used in the control group was used as an active treatment point in another study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Drawing lots with replacement' |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participant blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 10% loss to follow‐up, equal in the two groups |
| Other bias | Low risk | No baseline differences |
Huang 2012.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: China Recruitment: volunteers, invitation letter |
|
| Participants | 60 smokers ≥ 15 cigs/day, aged 18‐70, FTND >5 | |
| Interventions | a) Acupressure with vaccinia seed fixed to 5 auricular points [TF4, CO14, CO15, TG2P, AT4]. Participants had to apply 3‐5 minute’s pressure 3‐5 times a day. Active acupuncture at ‘Three‐Needles’ [Tim Mee Point, Yang‐xi Point (LI5) and Lie‐que Point (LU7)], needles retained for 15 minutes after “deqi”. Daily for 6 days, then 6 times in 14 days. b) Sham acupressure with sponge similar to vaccinia seed in colour and size. Instructed to apply pressure, as intervention group. Sham acupuncture by bringing the needle point in contact with skin without penetration to same points with the same course of treatment. |
|
| Outcomes | Reported smoking cessation at end of treatment and 3 months follow‐up. Outcome not validated by expired air CO Other outcomes: cigarette consumption, Fagerstrom Test for Nicotine Dependence (FTND), Self‐rating Tobacco Dependence Scale. |
|
| Notes | Claimed no dropouts, no mention about any previous attempts to quit | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | “Participants were randomly divided into the treatment group and placebo group according to their order of hospitalization in turn by the method of simple randomization” |
| Allocation concealment (selection bias) | High risk | Allocation cannot be concealed because patients are allocated alternately |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Single blinding (participants were blinded by covering the points with flexible dressing) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes reported for all included smokers |
| Other bias | Low risk | No significant differences in baseline variables |
Kerr 2008.
| Methods | Randomized trial of laser therapy Country: UK Recruitment: media announcement |
|
| Participants | 387 motivated smokers without previous use of laser randomised. Excluded for age <16 years, pregnancy, uncontrolled Ischaemic heart disease, asthma, unstable diabetes mellitus and unstable epilepsy | |
| Interventions | a) Low‐level laser treatment (Omega, power output 50mW, wavelength 820 nm, pulse repetition 20 Hz, radiant exposure 24J/cm sq) for 1 minute to 4 auricular and 3 wrist points bilaterally, total duration 14 minutes: on days 1, 3, and 7, plus sham laser on day 14 b) same active laser used on days 1, 3, 7 and 14 c) sham laser inactivated by manufacturer and identical except for no laser output, on days 1, 3, 7 and 14 |
|
| Outcomes | Self‐reported smoking cessation at end of treatment and after 3 and 6 months | |
| Notes | Author provided additional data on group size at baseline. Data from group a) could not be used in meta‐analysis (mixed interventions) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Not clear, but mentions use of random number table, selecting and allocating them sequentially to each of the study groups |
| Allocation concealment (selection bias) | High risk | Allocation of next patient could be ascertained from table |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Sham or inactive probe |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 23 lost before treatment, 24 did not complete treatment. Unequal dropouts, 38/47 were in group C. Effect is likely small bias in favour of intervention |
| Other bias | Unclear risk | No baseline characteristics reported |
Labadie 1983.
| Methods | Randomized trial of acupuncture Country: France Recruitment: Community volunteers attending anti‐smoking clinic |
|
| Participants | 130 smokers (criteria not specified) | |
| Interventions | a) medical treatment (advice plus benzodiazepine, lobeline and a 'detoxicant') b) acupuncture to auricular and body points; not stated whether repeated Both groups followed up weekly for 1 month, fortnightly for 3 months, monthly for a year |
|
| Outcomes | Abstinence and reduction of smoking at 8 weeks and 1 yr Validation: none | |
| Notes | Control data deemed as 'intervention of unknown effectiveness'. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | By alternation |
| Allocation concealment (selection bias) | High risk | (alternation) |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout during treatment a) 25% b) 17%. 8.5% loss to follow‐up |
| Other bias | Unclear risk | Only age reported at baseline |
Lacroix 1977.
| Methods | Randomized trial of acupuncture Country: France Recruitment: not stated |
|
| Participants | 117 smokers; the only inclusion criterion was the wish to stop | |
| Interventions | a) facial acupuncture, 3 points on each side for 30 minutes, weekly for 3 weeks
b) sham acupuncture, 2 non‐points on each side (duration not stated), weekly for 3 weeks All smokers also given standardised advice |
|
| Outcomes | Abstinence at 3 weeks Validation: none | |
| Notes | [in French] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised but no details presented |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Not specifically described as blinded, but overtly designed for participant‐ (but not practitioner‐) blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropout rate 16% in treatment group, 34% in sham/placebo group |
| Other bias | Unclear risk | No baseline information |
Lagrue 1980.
| Methods | Randomized trial of acupuncture Country: France Recruitment: not stated |
|
| Participants | 154 smokers (criteria not specified) | |
| Interventions | a) facial acupuncture, repeated after 1 week
b) sham acupuncture, (using facial points called 'placebo' but not further described) repeated after 1 week All smokers also given standardised advice |
|
| Outcomes | Abstinence and 80% reduction in consumption at 1 week Validation: none | |
| Notes | Practitioner specially trained to give both treatments without knowing which was active (i.e. a truly double‐blind study) [in French] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocated into groups of 5‐7 receiving the same treatment |
| Allocation concealment (selection bias) | High risk | Groups were pre‐arranged |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Truly double‐blind: both participant and practitioner blinded ‐ practitioner was non‐acupuncturist, specially trained for this study |
| Incomplete outcome data (attrition bias) All outcomes | High risk | over 20% dropout in both groups |
| Other bias | Unclear risk | No baseline information |
Lamontagne 1980.
| Methods | Randomized trial of acupuncture Country: Canada Recruitment: Community volunteers responding to newspaper advert |
|
| Participants | 75 subjects aged 20‐50, smoking between 15 and 50 cigs/day, not taking drugs, and in good health | |
| Interventions | a) acupuncture to auricular points ('Zero' and 'Lung') b) acupuncture to body points used for 'relaxation' c) self‐monitor and report back All subjects given 2 appointments 1 week apart. All smokers also given written advice on smoking cessation | |
| Outcomes | Abstinence at 2 weeks, 3 months, and 6 months; mean smoking rates for 14 day periods during study Validation: none | |
| Notes | Poor choice of acupuncture control procedure, since anti‐smoking effect of 'relaxation' treatment cannot be ruled out | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly' with no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Acupuncture control clearly designed to ensure blinding of participants, though not described as 'blind' |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One smoker in each group dropped out |
| Other bias | Unclear risk | No baseline information reported |
Leung 1991.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: Hong Kong Recruitment: Community volunteers responding to newspaper and radio adverts |
|
| Participants | 95 subjects who had smoked for at least 1 year and were motivated to stop | |
| Interventions | a) 10 daily sessions of behaviour therapy lasting 1.5 hours b) Indwelling needles in auricular points ('Shenmen' and 'Lung') checked every 7 days ; two introductory information sessions followed by eight attendances in total, for supervision of the needles; not stated whether the indwelling needles were in place throughout the course c) waiting‐list control | |
| Outcomes | Abstinence and percentage reduction in consumption immediately after treatment and at 1, 3, and 6 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly assigned' no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study, no description of observer blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition 18%, some difference between groups |
| Other bias | Low risk | No major differences at baseline |
Li 2009.
| Methods | Randomized trial of acupressure (continuous stimulation) Country: Shanghai, China Recruitment: 140 smokers from the community. The clinical trial was carried out in the outpatient department of acupuncture‐moxibustion in Tian Shan TCM hospital, Shanghai. 20 cases of healthy non‐smokers were also recruited to provide data for normal levels of sulfocyanide in urine. Statistics: Ridit test |
|
| Participants | Inclusion criteria: smoking >1 year; > 10 cigs/day, desire to give up smoking in 3 months; age: l8‐65 years old Intervention group: 70 (52 male, 18 female), age ranging from l8‐58 (38.23±9.79) years old; smoking duration:1‐29 years (10.46±7.08); daily intake: l0‐35 cigarettes (17.07±5.02). Control group: 70 (55 male, 15 female), age ranging from 20‐59 (38.26±9.56) years old; smoking duration: 1‐30 years (10.67±7.60); daily intake: l0‐33 cigarettes (16.97±5.03). Baseline comparability: age, gender, smoking age, smoking amount. |
|
| Interventions | Acupressure using the seed of cowherb a) auricular points: mouth, lung, shenmen, shenshangxian, stomach, neifenmi. b) (control): auricular points: thyroid, shoulder, sciatic nerve, clavicle, cervical vertebrae, eye. Seed applied to the main points in one ear and the accompanying points in the other ear: replaced every two days. Course of treatment: 20 days. Follow‐up visit in 3 months. |
|
| Outcomes | Abstinence at 20 days (early) and 3 months (not used in meta‐analysis). Confirmed by concentrations of sulfocyanide of urine tested in the morning | |
| Notes | A sulfocyanide concentration of <(2.23±2.41)mg/L was observed in the non‐smokers. Values above mean 2.23 mg/L were therefore taken to indicate smoking, i.e. that the intervention was not successful. No intention‐to‐treat (ITT) analysis was applied. 3 month follow‐up too short for long‐term abstinence outcome [in Chinese] |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The cases are randomly allocated into the two groups, but method of sequence generation is not described. |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of participants with loss to follow‐up reported; 1/70 in intervention group, 3/70 in control group |
| Other bias | Unclear risk | No information reported |
Martin 1981a.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: New Zealand Recruitment: Community volunteers |
|
| Participants | 126 smokers (criteria not specified) | |
| Interventions | a) indwelling needles to 'effective' auricular points (lung and hunger) for 3 weeks b) indwelling needles to 'ineffective' auricular points (elbow and eye) Other groups with needling in the ankle or with cut‐off studs were not conducted in parallel with the above and have been excluded from the review | |
| Outcomes | Abstinence and reduction in cigarette consumption at 3 weeks, 3 months and 6 months Validation: nil | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study run in three phases, randomisation method not described |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Described as single blind, and the interventions were appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropout rate 22%, 31% overall |
| Other bias | Low risk | Groups similar in sex, age and smoking habits |
Martin 1981b.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: New Zealand Recruitment: Community volunteers Randomization: in groups, method not stated |
|
| Participants | 134 smokers (unspecified) | |
| Interventions | a) indwelling needles to 'effective' auricular points (lung and hunger) for 3 weeks plus electroacupuncture for 20 minutes to LI4 in the hand and tongue point in the ear at the second attendance b) indwelling needles to 'ineffective' auricular points (elbow and eye) plus electroacupuncture for 20 minutes to LI4 in the hand and tongue point in the ear at the second attendance Other groups with needling in the ankle or with cut‐off studs were not conducted in parallel with the above and have been excluded from the review | |
| Outcomes | Abstinence and reduction in cigarette consumption at 3 weeks, 3 months and 6 months Validation: nil | |
| Notes | LI4 was used as an active intervention in other studies: but since it was given to both groups in this study, and only at week 2, it does not annul the comparison between 'effective' and 'ineffective' points. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study run in three phases, randomisation method not described |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Described as single blind, and the interventions were appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropout rate 22% in short term, 31% overall |
| Other bias | Low risk | Groups similar in sex, age and smoking habits |
Parker 1977a.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: USA Recruitment: Volunteers from hospital employees |
|
| Participants | 18 smokers (aged 19 to 60 years, other characteristics unspecified) | |
| Interventions | a) indwelling needles placed in effective auricular points ('Shenmen' and 'Lung') b) indwelling needles placed in points considered inactive ('Shoulder' and 'Eye') Needles replaced in both groups twice weekly for 3 weeks | |
| Outcomes | Abstinence and reduction in consumption at 6 weeks Validation: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly' no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Designed to be participant blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Other bias | Unclear risk | Baseline data not reported |
Parker 1977b.
| Methods | Randomized trial of acupuncture Country: USA Recruitment: Volunteers from hospital employees |
|
| Participants | 23 smokers (aged 19 to 60 years, other characteristics unspecified) | |
| Interventions | a) electrical stimulation to effective auricular points ('Shenmen' and 'Lung') b) electrical stimulation to points considered inactive ('Shoulder' and 'Eye') Both groups treated for 20 minutes twice weekly for 3 weeks | |
| Outcomes | Abstinence and reduction in consumption at 6 weeks Validation: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly' no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Designed to be participant blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Other bias | Unclear risk | Baseline data not reported |
Pickworth 1997.
| Methods | Randomized trial of electrostimulation Country: USA Recruitment: 'from community' |
|
| Participants | 121 adults aged over 21 yrs, smoking >20/day for at least 1 yrs, no psychoactive medications; without pregnancy, drug history, medical condition, implanted device, history of seizures or migraine | |
| Interventions | 5 consecutive days of 60 min of a) electrostimulation, 10Hz 2 msec pulse, 30 µamp to mastoid, or b) sham electrostimulation | |
| Outcomes | Abstinence after 5 days and 1 month, verified by exhaled CO. Withdrawal symptoms. | |
| Notes | Stimulation parameters were criticised by Boutros 1998 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "the instrument manufacturer 'prepared sealed envelopes containing a cartridge and an insert that was randomly assigned to each subject' but method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes prepared with cartridge and insert |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Described as double‐blind, and interventions were appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rates 16% and 17% |
| Other bias | Low risk | No baseline differences |
Scheuer 2005.
| Methods | Randomized trial of electrostimulation Country: Switzerland Recruitment: method not stated |
|
| Participants | Smokers willing to quit (66 randomized, 64 followed up) | |
| Interventions | Neuroelectric therapy (NET) in region of mastoid bone for 96 hours. Devices delivered a constant current of 10.0 mA and 35.0 V. Devices were fully automated and programmed to deliver either a) active treatment at 300 Hz b) placebo at 700 Hz (no justification or explanation given) |
|
| Outcomes | Smoking cessation at 4 days, 2 and 6 weeks, 3 and 6 months, validated by cotinine tests (no details) | |
| Notes | Abstract only. No group sizes were given, only percentages of quitters in each group, and we were unable to contact the author. We therefore assumed two equal groups. [We imputed denominators at follow‐up from percentages that lead to whole numbers] The authors concluded that the 'placebo' stimulation might be active |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | no details given |
| Blinding (performance bias and detection bias) All outcomes | Low risk | 'Placebo' used, no information on blinding of therapists |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no details given for dropouts |
| Other bias | Unclear risk | no baseline details given |
Steiner 1982.
| Methods | Randomized trial of acupuncture Country: USA Recruitment: Community volunteers responding to newspaper and radio adverts |
|
| Participants | 32 subjects over 21, smoking over 20 cigs/day for 2 consecutive years, not pregnant and not on chronic pain medication or mood‐altering drugs Selected from 82 volunteers, matched according to age, sex, and cigarette consumption | |
| Interventions | a) acupuncture to genuine body and ear points; needle sensation achieved. b) sham acupuncture to nearby areas without needling sensation Both interventions given twice weekly for 2 weeks | |
| Outcomes | Abstinence and cigarette consumption at 4 weeks Validation: none | |
| Notes | Subjects were not advised to stop smoking at any particular time, but to 'follow your motivation and appetite to the best of your ability' | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Matched pairs selected from volunteers, one of each pair randomly assigned, method not stated |
| Allocation concealment (selection bias) | Unclear risk | The description of the timing of randomisation does not provide reliable information that it was concealed |
| Blinding (performance bias and detection bias) All outcomes | Low risk | 'Neither research volunteer nor data gatherers were aware of group assignments' |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 28% dropout rate |
| Other bias | Low risk | Matched for age, sex and smoking history |
Tian 1996.
| Methods | Randomized trial of acupressure (continuous stimulation) Country: China Recruitment: not stated |
|
| Participants | 120 smokers over 20 yrs old, regularly smoking >10 cigs/day, exhaled CO>10ppm, and 'likely to attend follow‐up for 1 year' | |
| Interventions | a) acupressure, 'Ear Point Seed Pressing' method: seed fixed to 4 points in one ear, treatment changed to alternate ear twice/wk for course of 1 month, repeated for 2 or 3 months. Seeds to be pressed by smoker 6 times daily b) advice: no description given | |
| Outcomes | Abstinence at 1 month and 1 yr, confirmed by CO measurement | |
| Notes | Report lacks details (e.g.. randomization, advice given, baseline characteristics) Error in results table: figures at 1 month do not reach correct total of 60 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomly' with no details |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts not reported, estimated at 77% |
| Other bias | Low risk | Groups similar at baseline |
Vandevenne 1985.
| Methods | Randomized trial of acupuncture Country: France Recruitment: volunteers attending anti‐smoking clinic |
|
| Participants | 200 self‐referred smokers, no criteria stated | |
| Interventions | a) acupuncture to 3 auricular and 2 body points b) sham acupuncture to nearby areas both interventions given on days 1, 4, 10 and 20 | |
| Outcomes | Abstinence (point‐prevalence) at 6 weeks, 6 months and 1 year Not validated | |
| Notes | [in French] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Described as blinded, and interventions appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 42% dropout at 6 weeks |
| Other bias | Low risk | Groups similar in smoking history at baseline |
Vibes 1977.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: France Recruitment: not stated |
|
| Participants | 200 smokers of at least 20 cigs /day; already tried to reduce their consumption; no previous acupuncture; not using any other therapy for smoking cessation | |
| Interventions | 6 treatment sessions 3 times a week for groups a) b) e). Indwelling needle for groups c) and d) a) 3 or 4 traditional acupuncture body points for cessation b) two nasal points c) auricular point Zero d) auricular point Lung e) control group: 2 points on hands/feet | |
| Outcomes | Smoking cessation at 14 days (not validated); reduction in cigarette consumption | |
| Notes | [in French] | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomised, no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | All groups received needling treatments, differences unlikely to lead to unblinding in the context |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate reported as less than 5% |
| Other bias | Unclear risk | No baseline data presented |
Waite 1998.
| Methods | Randomized trial of acupuncture and continuous stimulation Country: UK Recruitment: community volunteers recruited by advertisements in on‐line news pages, posters in hospital and word of mouth. |
|
| Participants | 78 adults over 18 years old who were smoking at least 10 cigs/day. Exclusions: cardiac pacemaker, previous acupuncture | |
| Interventions | Both groups received one 20‐minute session of acupuncture with electrical stimulation followed by placement of a seed on the needle site held in place with adhesive tape. Participants were instructed to keep the seed in place as long as they found it helpful and press it when they experienced the desire to smoke
Points used were:
a) active group, lung point in ear
b) control group, medial aspect of the patella, not on recognised acupuncture point All smokers received structured counselling and written information before randomisation |
|
| Outcomes | Cessation at 2 weeks, and 2, 4 and 6 months (point prevalence) Validation at 6 months only: urinary cotinine | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization, no further details |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | described as single blind, and interventions appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% follow‐up at 6 months |
| Other bias | Low risk | Slightly heavier smokers in active group |
White 1998.
| Methods | Randomized trial of acupuncture Country: UK Recruitment: community volunteers from media invitation |
|
| Participants | 76 adults over 21 years smoking at least 15 cigs/day Exclusions: previous acupuncture, pregnancy, breast‐feeding, cardiac pacemaker, known bleeding tendency | |
| Interventions | a) acupuncture with electrical stimulation to lung point in both ears b) sham acupuncture consisting of either needle or carbon pad placed over the mastoid bone attached to sham (inactivated) stimulator Interventions were given on day 1, 3 and 7 of the smoking cessation All smokers also received counselling by a nurse | |
| Outcomes | Sustained cessation at 2 weeks Validation: expired air CO concentration Withdrawal symptoms assessed by Visual Analogue Scale Reported cessation at 9 months (not validated) | |
| Notes | Credibility of interventions tested by questionnaire Standardized, minimal interaction by acupuncturist All counselling by blinded nurse | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes opened immediately before intervention |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded participant (though control group felt no electrical stimulation), blinded assessor |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 32% dropout or withdrawal rate |
| Other bias | Low risk | Marginally heavier smokers in active treatment group |
White 2007.
| Methods | Randomized trial of acupressure (continuous stimulation) Country: England Recruitment: smoking cessation clinic |
|
| Participants | 19 smokers, aged ≥18 years, smoked ≥10 cigs/day, prescribed NRT; no general or auricular medical conditions or specified medications | |
| Interventions | All participants received the usual NRT and group counselling and support. In addition, Pyonex type acupressure beads (specially manufactured for the study) were used. a) two beads, in Lung and Shenmen points b) one bead in Lung point c) no bead. Beads worn for 4 weeks, replaced when necessary or every 14 days |
|
| Outcomes | Reported cessation at 4 weeks verified by expired air CO ≤9 ppm | |
| Notes | Pilot study, mainly testing recruitment and feasibility. Data from two intervention groups combined | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | code generated by computerised blocked randomisation prepared by researcher unconnected with the study |
| Allocation concealment (selection bias) | Low risk | participant opened opaque, numbered envelope |
| Blinding (performance bias and detection bias) All outcomes | High risk | open study |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5 randomised patients not included in the analysis, and no information on group allocation |
| Other bias | Low risk | no major baseline differences |
Wing 2010.
| Methods | Randomized trial of acupressure (continuous stimulation) Country: Hong Kong Recruitment: outpatient clinics and community |
|
| Participants | 70 smokers. Aged ≥18, motivated to quit | |
| Interventions | a) active acupressure using hard beads on ear (Shenmen, Lung, Mouth, and Brain) and hand (LI4 and PC6) for 3 weeks. Not stated whether uni‐ or bilateral. To be pressed 3/day or whenever urge to smoke b) sham acupressure beads |
|
| Outcomes | Cessation 3 months after end of treatment Validation: CO < 6 ppm |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Blocked randomization, no further details |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear |
| Other bias | Low risk | "no major differences between the active and sham groups at baseline level" |
Wu 2007.
| Methods | Randomized trial of acupuncture (continuous stimulation) Country: Taipei, Taiwan Recruitment: advertisements through hospital; those attending smoking cessation clinic |
|
| Participants | 131 smokers aged ≥18 years, smoking ≥10 cigs/day, and smoked ≥1 year; has no specified diseases, not taking specified medication, not abusing drugs | |
| Interventions | Indwelling needles inserted into four auricular points and retained for one week, then replaced. Total treatment period 8 weeks. Points used: a) 'real' points Shenmen, Lung, Mouth, Sympathetic b) 'irrelevant' points Eye, Elbow, Shoulder, Knee All participants also received counselling from a nurse |
|
| Outcomes | Reported cessation at end of treatment and 6 months follow‐up; verbal report validated by exhaled air CO concentration in those who could attend clinic; telephone call to defaulters (numbers of defaulters not reported) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | block randomization method with random number table |
| Allocation concealment (selection bias) | Unclear risk | no details given |
| Blinding (performance bias and detection bias) All outcomes | Low risk | study not described as blinded, but clearly designed subject‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | full details of dropouts and reasons: 5 in group a) and 8 in group b) |
| Other bias | Low risk | no baseline differences |
Yeh 2009.
| Methods | Randomized trial of electrostimulation and continuous stimulation Country: Taiwan Recruitment: community volunteers |
|
| Participants | 79 healthy smokers, serum cotinine >100 ng/ml, daily consumption >1 CPD | |
| Interventions | a) active acupoint stimulation; shenmen, lung, stomach, mouth, endocrine & tim mee
b) sham stimulation, 5mm away from real acupoint locations (We were unable to clarify whether the intervention was applied uni‐ or bilaterally) All participants used the electron acupuncture with low frequency (9V,< 60Hz) once a week for 6 weeks, for twenty minutes each time. A seed‐embedding method was then used on these auricular points. All participants were instructed to apply pressure on the auricular points for one minute each time, and three to five times each day for six weeks. The auricular seeds were replaced with new ones each week. |
|
| Outcomes | Cessation based on serum cotinine <100 ng/ml at 6 weeks, participant self‐ report not used | |
| Notes | Groups only differed in the site that the stimulation was given, i.e. a true test of point location. Included in both continuous stimulation and electrostimulation analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘Randomly assigned’, no further details |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) All outcomes | Low risk | study not described as blinded, but clearly designed subject‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 9 I and 11 C withdrew before end of treatment, excluded from reported outcomes, reincluded in denominators for MA |
| Other bias | Low risk | no major baseline differences |
Zhang 2013.
| Methods | Randomized trial of acupressure (continuous stimulation) Country: Australia Recruitment: community volunteers |
|
| Participants | 43 smokers aged ≥18 years, >10 cpd | |
| Interventions | a) Acupressure (stainless steel beads) to ear points Shenmen (TF4), Lung [AW1] (CO14), Mouth (CO1), Hunger (extra), and Liver (CO12) for 4 weeks. b) Sham acupressure; pressure on non specific points Helix 2 (HX10), Shoulder (SF4, 5), Clavicle (SF6), Occiput (AT3), and Tooth (LO1). All participants instructed to press all beads 3 times daily. Beads unilateral, alternated between ears every week |
|
| Outcomes | Cessation at 8 weeks & 5 months Validation: CO ≤ 10ppm |
|
| Notes | (Outcomes same at 8 weeks & 5 months) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "An independent researcher conducted block randomisation using a computer generated randomisation list." |
| Allocation concealment (selection bias) | Low risk | "The randomised group codes were placed into sealed, opaque envelopes by another independent person. Participants, data entry personnel, and data analysts were blinded to treatment allocation." "participants randomly selected a sealed opaque envelope with their randomisation code inside" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "The single acupuncturist was trained to perform the same procedures at each consultation and was instructed not to discuss any aspect of the treatment procedures with the participants, to ensure participant blinding and consistency of treatment." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Less than half of each group reached at 5 months |
| Other bias | Low risk | "At baseline, no significant differences between the two groups were found ..." |
CPD: cigarettes per day CO: carbon monoxide FTND: Fagerstrom Test for Nicotine Dependence yr: year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Boureau 1978 | This study compared 2 groups who both received identical acupuncture following an injection: one group were injected with saline, the other with naloxone. Therefore, 2 hypotheses are tested simultaneously: does acupuncture help smoking cessation by releasing endogenous opioid peptides? |
| Boutros 1998 | This letter in response to the study of Pickworth commented on the stimulus parameters used in the study, but included no original data |
| Chen 2006 | All participants received acupressure; test of an internet programme; not randomised |
| Fang 1983 | Outcome was reduction in amount smoked by half or more, not cessation |
| He 2012 | Outcome depression, not smoking cessation |
| Huang 2001 | Compares acupressure to acupuncture |
| Hyun 2010 | Cessation outcomes not reported |
| Kang 2005 | School children in two schools allocated according to which school they attended, without mention of randomisation. One case of smoking cessation recorded, so exclusion unlikely to bias review |
| MacHovec 1978 | This study does not specify that the subjects were randomized |
| Man 1975 | Subjects were allocated by place of residence, not randomly |
| Sun 2000 | The two intervention groups received the same acupuncture, and differed only in the use of psychological nursing care |
| Tan 1987 | Not described as randomized: complete abstinence not reported. |
| Wang 2010 | All participants received acupressure; test of a multimedia programme. Not randomised |
| Wang 2013 | Compares two types of acupuncture. |
| Zhang 1989 | Compares two active acupuncture conditions: both use 'Lung' auricular point which is widely considered an active intervention. |
| Zhou 2010 | The trial compared electronic acupuncture combined with ear acupressure with magnetic balls against electronic acupuncture alone, therefore, electronic acupuncture is considered as co‐intervention, and any potential effect would be come from acupressure combined with magnetic balls on ear acupoints. |
Characteristics of studies awaiting assessment [ordered by study ID]
Shahrokhi 2013.
| Methods | "Participants were divided to two groups by randomized sample method" |
| Participants | "One hundred and thirty‐two men smokers who were ready to quit smoking" |
| Interventions | "One group was for acupuncture and another group was for acupuncture in sham points." |
| Outcomes | "All participants followed for 1 year and the quit rate evaluated in 1, 6, 12 months of the study." |
| Notes | Information from conference abstract with insufficient detail to include. Attempts to contact authors so far unsuccessful. |
Characteristics of ongoing studies [ordered by study ID]
Leung 2012.
| Trial name or title | Effect of Self‐administered Auricular Acupressure on Smoking Cessation—a Pilot Study |
| Methods | Three arm RCT, partially double blind |
| Participants | 60 smokers aged between 18 and 75 years of age, wanting to quit, no more than 2 failed attempts in previous 3 years |
| Interventions | 1. National Acupuncture Detoxification Association (NADA) points + digital pressure 2. Random acupuncture points + digital pressure 3. Advice & support only |
| Outcomes | Continuous abstinence during treatment weeks (1‐6), week 13 and week 26 |
| Starting date | July 2011 |
| Contact information | lawrence.leung@dfm.queensu.ca, jyoti.kotecha@cspc.queensu.ca |
| Notes |
Differences between protocol and review
Risk ratio used instead of odds ratio.
Contributions of authors
AW, HR, JL and LS extracted data. AW drafted the review with intellectual contributions and textual revisions by all other authors.
Sources of support
Internal sources
General Practice & Primary Care, Peninsula Medical School, Universities of Exeter and Plymouth, UK.
-
NAFKAM National Research Centre for Complementary Medicine, Tromsø, Norway.
Part of 2010 update conducted by AW while funded by NAFKAM
External sources
NHS Research and Development National Cancer Programme, England, UK.
Adrian White is supported by the DH National Coordinating Centre for Research Capacity Development, UK.
Declarations of interest
AW is author of two trials included in this review, and is in part‐time private acupuncture practice; he received no financial support from any commercial entity. JL, LS, HR, and JC have no conflict of interest.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Antoniou 2005 {unpublished data only}
- Antoniou D, Bouros D, Pavlakou G, Chaimala D, Papageorgiou C, Beltegris, et al. Aural electrical stimulation for smoking cessation ‐ a double blind, placebo controlled study [abstract]. European Respiratory Journal 2005;26(Suppl 49):388s. [Google Scholar]
Aycicegi‐Dinn 2011 {published data only}
- Aycicegi‐Dinn A, Dinn W. Efficacy of an alternative smoking cessation treatment. Journal of Addictive Diseases 2011;30(4):368‐81. [] [DOI] [PubMed] [Google Scholar]
Bier 2002 {published data only}
- Bier ID, Wilson J, Studt P, Shakleton M. Auricular acupuncture, education, and smoking cessation: a randomized, sham‐controlled trial. American Journal of Public Health 2002;92(10):1642‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cai 2000 {published data only}
- Cai Y, Zhao C, Wong SU, Zhang L, Lim SK. Laser acupuncture for adolescent smokers ‐ a randomized double‐blind controlled trial. American Journal of Chinese Medicine 2000;25(3‐4):443‐9. [DOI] [PubMed] [Google Scholar]
Circo 1985 {published data only}
- Circo A, Tosto A, Raciti S, Cardillo R, Gulizia M, Oliveri M, et al. First results of an anti‐smoke outpatient unit: Comparison among three methods [Primi risultati di un ambulatori antifumo. Confronto fra tre metodice]. Rivista di Cardiologia Preventiva e Riabilitativa 1985;3(2):147‐51. [Google Scholar]
Clavel 1985 {published data only}
- Clavel F, Benhamou S. Tobacco withdrawal. Comparison of the efficacy of various methods. Intermediate results of a comparative study [Desintoxication tabagique. Comparaison de l'efficacite de differentes methodes. Resultats intermediaires d'une etude comparative]. Presse Medicale 1984;13(16):975‐7. [PubMed] [Google Scholar]
- Clavel F, Benhamou S, Company‐Huertas A, Flamant R. Helping people to stop smoking: randomised comparison of groups being treated with acupuncture and nicotine gum with control group. British Medical Journal Clinical Research Edition 1985;291:1538‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clavel 1992 {published and unpublished data}
- Clavel F, Paoletti C. [Une étude de différents programmes de désintoxication tabagique portant sur près de 1000 volontaires recrutés dans la population générale : résultats à 1 mois]. Revue d'Epidemiologie et de Sante Publique 1990;38:133‐8. [PubMed] [Google Scholar]
- Clavel F, Paoletti C, Benhamou S. A randomised 2x2 factorial design to evaluate different smoking cessation methods. Revue d'Epidemiologie et de Sante Publique 1992;40:187‐90. [PubMed] [Google Scholar]
- Clavel‐Chapelon F, Paoletti C, Benhamou S. Smoking cessation rates 4 years after treatment by nicotine gum and acupuncture. Preventive Medicine 1997;26:25‐8. [DOI] [PubMed] [Google Scholar]
Clavel 1992 +NG {published data only}
- Clavel F, Paoletti C, Benhamou S. A randomised 2x2 factorial design to evaluate different smoking cessation methods. Revue d'Epidemiologie et de Sante Publique 1992;40(3):187‐90. [PubMed] [Google Scholar]
- Clavel‐Chapelon F, Paoletti C, Benhamou S. Smoking cessation rates 4 years after treatment by nicotine gum and acupuncture. Preventive Medicine 1997;26:25‐8. [DOI] [PubMed] [Google Scholar]
Cottraux 1983 {published data only}
- Cottraux J, Schbath J, Messy P, Mollard E, Juenet C, Collet L. Predictive value of MMPI scales on smoking cessation programs outcomes. Acta Psychiatrica Belgiques 1986;86:463‐9. [PubMed] [Google Scholar]
- Cottraux JA, Harf R, Boissel JP, Schbath J, Bouvard M, Gillet J. Smoking cessation with behaviour therapy or acupuncture ‐ a controlled study. Behaviour Research and Therapy 1983;21(4):417‐24. [DOI] [PubMed] [Google Scholar]
Docherty 2003 {unpublished data only}
- Docherty G, Gordon D, McAlpine L. Laser and NRT smoking cessation programmes in areas of high social deprivation [Abstract]. Thorax 2003;58(Suppl 3):iii43. [Google Scholar]
Fritz 2013 {published data only}
- Fritz DJ, Carney RM, Steinmeyer B, Ditson G, Hill N, Zee‐Cheng J. The efficacy of auriculotherapy for smoking cessation: A randomized, placebo‐controlled trial. Journal of the American Board of Family Medicine 2013;26(1):61‐70. [] [DOI] [PubMed] [Google Scholar]
Georgiou 1999 {published data only}
- Georgiou AJ, Spencer CP, Davies GK, Stamp J. Electrical stimulation therapy in the treatment of cigarette smoking. Journal of Substance Abuse 1998;10:265‐74. [DOI] [PubMed] [Google Scholar]
Gilbey 1977 {published data only}
- Gilbey V, Neumann B. Auricular acupuncture for smoking withdrawal. American Journal of Acupuncture 1977;5:239‐47. [Google Scholar]
Gillams 1984 {published data only}
- Gillams J, Lewith GT, Machin D. Acupuncture and group therapy in stopping smoking. Practitioner 1984;228:341‐4. [PubMed] [Google Scholar]
Han 2006 {published data only}
- Han Y. Combining of acupuncture and auricular points applying for treatment of 42 cases of tobacco withdrawal syndrome. Journal of Clinical Acupuncture and Moxibustion 2006;22(11):16. [Google Scholar]
He 1997 {published data only}
- He D, Berg JE, Hostmark AT. Effects of acupuncture on smoking cessation or reduction for motivated smokers. Preventive Medicine 1997;26:208‐14. [DOI] [PubMed] [Google Scholar]
- He D, Medbo JI, Hostmark AT. Effect of acupuncture on smoking cessation or reduction: an 8‐month and 5‐year follow‐up study. Preventive Medicine 2001;33(5):364‐72. [DOI] [PubMed] [Google Scholar]
Huang 2012 {published data only}
- Huang Y. The Clinical Observation of Nicotine Dependence Treated with Smoke Three‐Needles Combine Auricular Pressure Therapy. Masters dissertation, Guangzhou University of Chinese Medicine.
Kerr 2008 {published and unpublished data}
- Kerr CM, Lowe PB, Spielholz NI. Low level laser for the stimulation of acupoints for smoking cessation: A double blind, placebo controlled randomised trial and semi structured interviews. Journal of Chinese Medicine 2008;86:46‐51. [Google Scholar]
Labadie 1983 {published data only}
- Labadie JC, Dones JP, Gachie JP, Fréour P, Perchoc S, et al. [Désintoxication tabagique: acupuncture et traitement médical]. Gazette Medicale de France 1983;90:2741‐7. [Google Scholar]
Lacroix 1977 {published data only}
- Lacroix JC, Besancon F. [Le sevrage du tabac. Efficacité de l'acupuncture dans un essai comparatif]. Annals Medicales Internes Paris 1977;128:405‐8. [PubMed] [Google Scholar]
Lagrue 1980 {published data only}
- Lagrue G, Poupy JL, Grillot A, Ansquer JC. Antismoking acupuncture. Short‐term results of a double‐blind comparative study [Acupuncture anti‐tabagique. Resultats a court terme d'une etude comparative menee a double insu]. Nouvelle Presse Medicale 1980;9:966. [PubMed] [Google Scholar]
Lamontagne 1980 {published data only}
- Lamontagne Y, Annable L, Gagnon MA. Acupuncture for smokers: lack of long‐term therapeutic effect in a controlled study. Canadian Medical Association Journal 1980;5:787‐90. [PMC free article] [PubMed] [Google Scholar]
Leung 1991 {published data only}
- Leung JP. Smoking cessation by auricular acupuncture and behavioral therapy. Psychologia 1991;34:177‐87. [Google Scholar]
Li 2009 {published data only}
- Li Y, Shen T, Cao L, et al. Clinical research of the seed of cowherb auricular pressing in treating 70 cases of quitting smoking. Jilin Journal of Traditional Chinese Medicine 2009;29(6):505‐6. [Google Scholar]
Martin 1981a {published data only}
- Martin GP, Waite PME. The efficacy of acupuncture as an aid to stopping smoking. New Zealand Medical Journal 1981;93:421‐3. [PubMed] [Google Scholar]
Martin 1981b {published data only}
- Martin GP, Waite PME. The efficacy of acupuncture as an aid to stopping smoking. New Zealand Medical Journal 1981;93:421‐3. [PubMed] [Google Scholar]
Parker 1977a {published data only}
- Parker LN, Mok MS. The use of acupuncture for smoking withdrawal. American Journal of Acupuncture 1977;5:363‐6. [Google Scholar]
Parker 1977b {published data only}
- Parker LN, Mok MS. The use of acupuncture for smoking withdrawal. Amercian Journal of Acupuncture 1977;5:363‐6. [Google Scholar]
Pickworth 1997 {published data only}
- Pickworth W, Fant R, Goffman A, Henningfield J. Cranial electrostimulation therapy: Response. Biological Psychiatry 1998;43:468‐9. [Google Scholar]
- Pickworth W, Fant R, Goffman A, Henningfield J. Evaluation of cranial electrostimulation therapy on short‐term smoking cessation. Biological Psychiatry 1997;42:116‐21. [DOI] [PubMed] [Google Scholar]
Scheuer 2005 {unpublished data only}
- Scheuer E. Effectiveness of neuroelectric therapy in inducing smoking cessation. Nicotine & Tobacco Research 2005;7(4):648‐9. [Google Scholar]
Steiner 1982 {published data only}
- Steiner RP, Hay DL, Davis AW. Acupuncture therapy for the treatment of tobacco smoking addiction. American Journal of Chinese Medicine 1982;10:107‐21. [DOI] [PubMed] [Google Scholar]
Tian 1996 {published data only}
- Tian Z, Chu Y. Treating smoking addiction with the ear point seed pressing method. Journal of Chinese Medicine 1996;52:5‐6. [Google Scholar]
Vandevenne 1985 {published data only}
- Vandevenne A, Rempp M, Burghard G. Study of the specific contribution of acupuncture to tobacco detoxication [Etude de l'action spécifique de l'acupuncture dans la cure de sevrage tabagique]. Sem Hôpital Paris 1985;61:2155‐60. [Google Scholar]
Vibes 1977 {published and unpublished data}
- Vibes J. Clinical trial of the role of acupuncture in the fight against tobacco addiction [Essai therapeutique sur le role de l'acupuncture dans la lutte contre le tabagisme]. Acupuncture 1977;51:13‐20. [Google Scholar]
Waite 1998 {published data only}
- Waite NR, Clough JB. A single‐blind, placebo‐controlled trial of a simple acupuncture treatment in the cessation of smoking. British Journal of General Practice 1998;48:1487‐90. [PMC free article] [PubMed] [Google Scholar]
White 1998 {published data only}
- White AR, Resch KL, Ernst E. Randomized trial of acupuncture for nicotine withdrawal symptoms. Archives of Internal Medicine 1998;158:2251‐5. [DOI] [PubMed] [Google Scholar]
White 2007 {published data only}
- White AR, Moody RC, Campbell JL. Acupressure for smoking cessation‐‐a pilot study. BMC Complementary & Alternative Medicine 2007;7:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wing 2010 {published data only}
- Wing YK, Lee A, Wong ELY, Leung PC, Zhang L, Pang ESY. Auricular acupressure for smoking cessation: A pilot randomized controlled trial. Medical Acupuncture 2010;22(4):265‐71. [] [Google Scholar]
Wu 2007 {published data only}
- Wu TP, Chen FP, Liu JY, Lin MH, Hwang SJ. A randomized controlled clinical trial of auricular acupuncture in smoking cessation. Journal of the Chinese Medical Association: JCMA 2007;70(8):331‐8. [DOI] [PubMed] [Google Scholar]
Yeh 2009 {published data only}
- Yeh ML, Chang CY, Chu NF, Chen HH. A six‐week acupoint stimulation intervention for quitting smoking. American Journal of Chinese Medicine 2009;37(5):829‐36. [DOI] [PubMed] [Google Scholar]
Zhang 2013 {published data only}
- Zhang AL, Di YM, Worsnop C, May BH, Xue CC. Ear acupressure for smoking cessation: study protocol for a randomised controlled trial. Forschende Komplementarmedizin (2006) 2013;20(4):290‐4. [] [DOI] [PubMed] [Google Scholar]
- Zhang AL, Di YM, Worsnop C, May BH, Costa C, Xue CCL. Ear acupressure for smoking cessation: A randomised controlled trial. Evidence‐Based Complementary and Alternative Medicine 2013;2013:Article ID 637073. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Boureau 1978 {published data only}
- Boureau F, Willer JC. Failure of naloxone to modify the anti‐tobacco effect of acupuncture [Desintoxification tabagique par l'acupuncture: essai negative de blocage par la naloxone]. Nouvelle Presse Medicale 1978;7:1401. [PubMed] [Google Scholar]
Boutros 1998 {published data only}
- Boutros NN, Krupitsky EM. Cranial electrostimulation therapy. Biological Psychiatry 1998;43(6):468. [DOI] [PubMed] [Google Scholar]
Chen 2006 {published data only}
- Chen HH, Yeh ML, Chao YH. Comparing effects of auricular acupressure with and without an Internet‐assisted program on smoking cessation and self‐efficacy of adolescents. Journal of Alternative & Complementary Medicine 2006;12:147‐52. [DOI] [PubMed] [Google Scholar]
Fang 1983 {published data only}
- Fang YA. [Clinical study on auricular acupuncture for treatment of smoking addiction] [Chinese]. Shanghai Journal of Acupuncture and Moxibustion 1983;2:30‐1. [Google Scholar]
He 2012 {published data only}
- He Y‐S, Wu Y‐S, Ouyang, M‐F, Li G‐X, Li H‐J, Xie H‐E. Efficacy observation of depression in nicotine withdrawal treated with acupuncture. World Journal of Acupuncture‐Moxibustion 2012;22(1):13‐16, 61. [Google Scholar]
Huang 2001 {published data only}
- Huang W. [Smoking cessation with ear point vacaria seed pressure in 158 cases]. Journal of Guangxi Medical University 2001;18:430. [] [Google Scholar]
Hyun 2010 {published data only}
- Hyun MK, Kang KW, Koo CM, Han SS, Kim AR, Jung SY, et al. A randomized controlled trial of whole‐body acupuncture for tobacco withdrawal symptoms. Journal of Alternative and Complementary Medicine 2007;13(8):889. [] [Google Scholar]
- Hyun MK, Lee MS, Kang K, Choi SM. Body acupuncture for nicotine withdrawal symptoms: A randomized placebo‐controlled trial. Evididence Based Complementary Alternative Medicine 2010;7:233‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kang 2005 {published data only}
- Kang H‐C, Shin K‐K, Kim K‐K, Youn B‐B. The effects of the acupuncture treatment for smoking cessation in high school student smokers. Yonsie Medical Journal 2005;46:206‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacHovec 1978 {published data only}
- MacHovec FJ, Man SC. Acupuncture and hypnosis compared: fifty‐eight cases. American Journal of Clinical Hypnosis 1978;21(1):45‐7. [DOI] [PubMed] [Google Scholar]
Man 1975 {published data only}
- Man SC. A preliminary clinical study of smoking treated by stitch‐auriculo‐acupuncture. Proceedings of the Third World Symposium on Acupuncture and Chinese Medicine. New York, March 1975.
Sun 2000 {published data only}
- Sun C. [Roles of psychological nursing played in the course of auricle point applying to help individuals giving up smoking] [Chinese]. Shanxi Nursing Journal 2000;14(2):69‐70. [Google Scholar]
Tan 1987 {published data only}
- Tan CH. The use of laser on acupuncture points for smoking cessation. American Journal of Acupuncture 1987;15(2):137‐41. [Google Scholar]
Wang 2010 {published data only}
- Wang YZ, Chen HH, Yeh ML, Lin SD. Auricular acupressure combined with multimedia instruction or alone for quitting smoking in young adults: A quasi‐experimental study. International Journal of Nursing Studies 2010;47:1089‐95. [DOI] [PubMed] [Google Scholar]
Wang 2013 {published data only}
- Wang W‐H, Song Y‐X. Clinical trial of acupuncture plus moxibustion for smoke cessation. Shanghai Journal of Acupuncture and Moxibustion 2013;32(4):287‐88. [Google Scholar]
Zhang 1989 {published data only}
- Zhang J, Tan S, Yu J. [120 cases of quitting smoking by pressing seeds on body points and auricular points]. Modern Traditional Chinese Medicine 1989;4:28‐9. [Google Scholar]
Zhou 2010 {published data only}
- Zhou JH, Wang RF. Observation of therapeutic effect of electronic acupuncture combined with ear acupressure with magnetic balls. Journal of NanJing TCM University 2010;26(1):79‐80. [Google Scholar]
References to studies awaiting assessment
Shahrokhi 2013 {published data only}
- Shahrokhi S, Kian M, Eftekhari F, Baum A, Shirkhanloo H. The short and long term abstinence rate of smoking by acupuncture in the Iranian samples. Journal of Diabetes 2013;5(Suppl s1):70. [] [Google Scholar]
References to ongoing studies
Leung 2012 {published data only}
- Leung L, Neufeld T, Marin S. Effect of self‐administered auricular acupressure on smoking cessation‐‐a pilot study. BMC Complementary and Alternative Medicine 2012;12:11. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ashenden 1997
- Ashenden R, Silagy CA, Lodge M, Fowler G. A meta‐analysis of the effectiveness of acupuncture in smoking cessation. Drug and Alcohol Review 1997;16:33‐40. [DOI] [PubMed] [Google Scholar]
Brewington 1994
- Brewington V, Smith M, Lipton D. Acupuncture as a detoxification treatment: an analysis of controlled research. Journal of Substance Abuse and Treatment 1994;11(4):289‐307. [DOI] [PubMed] [Google Scholar]
Castera 2002
- Castera P, Nguyen J, Gerlier J‐L, Robert S. Is acupuncture beneficial in tobacco cessation, and is its effect specific? A meta‐analysis. [L'acupuncture est‐elle bénéfique dans la sevrage tabagigue, son action est‐elle spécifique? Une méta‐analyse]. Acupuncture & Moxibustion 2002;1(3‐4):76‐85. [Google Scholar]
Chae 2004
- Chae Y, Yang CH, Kwon YK, Kim MR, Pyun KH, Hahm DH. Acupuncture attenuates repeated nicotine‐induced behavioral sensitization and c‐Fos expression in the nucleus accumbens and striatum of the rat. Neuroscience Letters 2004;358(2):87‐90. [DOI] [PubMed] [Google Scholar]
Cheng 1980
- Cheng RS, Pomeranz B, Yu G. Electroacupuncture treatment of morphine‐dependent mice reduces signs of withdrawal, without showing cross‐tolerance. European Journal of Pharmacology 1980;68:477‐81. [DOI] [PubMed] [Google Scholar]
Cheng 2012
- Cheng H‐M, Chung Y‐C, Chen H‐H, Chang Y‐H, Yeh M‐L. Systematic review and meta‐analysis of the effects of acupoint stimulation on smoking cessation. The American journal of Chinese medicine 2012;40(3):429‐42. [DOI] [PubMed] [Google Scholar]
Choy 1978
- Choy YM, Tso WW, Fung KP, Leung KC, Tsang YF, Lee CY, et al. Suppression of narcotic withdrawals and plasma ACTH by auricular electroacupuncture. Biochemical and Biophysical Research Communications 1978;82:305‐9. [DOI] [PubMed] [Google Scholar]
Choy 1983
- Choy DS, Lutzker L, Meltzer L. Effective treatment for smoking cessation. American Journal of Medicine 1983;75:1033‐6. [DOI] [PubMed] [Google Scholar]
Clavel 1997
- Clavel‐Chapelon F, Paoletti C, Benhamou S. Smoking cessation rates 4 years after treatment by nicotine gum and acupuncture. Preventive Medicine 1997;26:25‐8. [DOI] [PubMed] [Google Scholar]
Clement‐Jones 1979
- Clement‐Jones V, McLoughlin L, Lowry PJ, Besser GM, Rees LH, Wen HL. Acupuncture in heroin addicts: changes in met‐enkephalin and beta‐endorphin in blood and cerebrospinal fluid. Lancet 1979;2:380‐3. [DOI] [PubMed] [Google Scholar]
Cummings 2009
- Cummings, M. Modellvorhaben Akupunktur ‐ a summary of the ART, ARC and GERAC trials. Acupuncture in Medicine 2009;27(1):26‐30. [DOI] [PubMed] [Google Scholar]
Fonnebo 2007
- Fonnebo V, Grimsgaard S, Walach H, Ritenbaugh C, Norheim AJ, MacPherson H, et al. Researching complementary and alternative treatments‐‐the gatekeepers are not at home. BMC medical research methodology 2007;7:7‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fuller 1982
- Fuller JA. Smoking withdrawal and acupuncture. Medical Journal of Australia 1982;1:28‐9. [DOI] [PubMed] [Google Scholar]
Han 1993
- Han JS, Zhang RL. Suppression of morphine abstinence syndrome by body electroacupuncture of different frequencies in rats. Drug and Alcohol Dependence 1993;31:169‐75. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analysis. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hui 2005
- Hui KK, Liu J, Marina O, Napadow V, Haselgrove C, Kwong KK, et al. The integrated response of the human cerebro‐cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. NeuroImage 2005;27(3):479‐96. [DOI] [PubMed] [Google Scholar]
Jiang 1994
- Jiang A, Cui M. Analysis of therapeutic effects of acupuncture on abstinence from smoking. Journal of Traditional Chinese Medicine 1994;14(1):56‐63. [PubMed] [Google Scholar]
Jobst 1995
- Jobst KA. A critical analysis of acupuncture in pulmonary disease: efficacy and safety of the acupuncture needle. Journal of Alternative and Complementary Medicine 1995;1(1):57‐85. [DOI] [PubMed] [Google Scholar]
Klawansky 1995
- Klawansky S, Yeung A, Berkey C, Shah N, Phan H, Chalmers TC. Meta‐analysis of randomized controlled trials of cranial electrostimulation. Journal of Nervous and Mental Disease 1995;183:478‐85. [DOI] [PubMed] [Google Scholar]
Law 1995
- Law M, Tang JL. An analysis of the effectiveness of interventions intended to help people stop smoking. Archives of Internal Medicine 1995;155:1933‐41. [PubMed] [Google Scholar]
Lewith 1995
- Lewith GT. The treatment of tobacco addiction. Complementary Therapies in Medicine 1995;3:142‐5. [Google Scholar]
Liang 2010
- Liang J, Ping XJ, Li YJ, Ma YY, Wu LZ, Han JS, et al. Morphine‐induced conditioned place preference in rats is inhibited by electroacupuncture at 2 Hz: role of enkephalin in the nucleus accumbens. Neuropharmacology 2010;58(1):233‐40. [DOI] [PubMed] [Google Scholar]
Lund 2009
- Lund I, Naslund J, Lundeberg T. Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: a physiologist's perspective. Chinese Medicine 2009;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lundeberg 2008
- Lundeberg T, Naslund J, Lund I, Thomas M. The Emperors sham ‐ wrong assumption that sham needling is sham. Acupuncture in Medicine 2008;26(4):239‐42. [DOI] [PubMed] [Google Scholar]
Ng 1975
- Ng LKY, Douthitt TC, Thoa NB, Albert CA. Modification of morphine‐withdrawal syndrome in rats following transauricular stimulation: an experimental paradigm for auricular acupuncture. Biological Psychiatry 1975;10:575‐80. [PubMed] [Google Scholar]
Patterson 1993
- Patterson MA, Patterson L, Flood NV, Winston JR, Paterson SI. Electrostimulation in drug and alcohol detoxification: significance of stimulation criteria in clinical success. Addiction Research 1993;1:130‐44. [Google Scholar]
Sakurai 2000
- Sakurai Y, Yamaguchi M, Abiko Y. Inhibitory effect of low‐level laser irradiation on LPS‐stimulated prostaglandin E2 production and cyclooxygenase‐2 in human gingival fibroblasts. Eur J Oral Sci 2000;108(1):29‐34. [DOI] [PubMed] [Google Scholar]
Schwartz 1988
- Schwartz JL. Evaluation of acupuncture as a treatment for smoking. American Journal of Acupuncture 1988;16:135‐42. [Google Scholar]
Smith 1988
- Smith, MO. An acupuncture programme for the treatment of drug‐addicted persons. Bulletin on Narcotics 1988;40(1):35‐41. [PubMed] [Google Scholar]
Tahiri 2012
- Tahiri M, Mottillo S, Joseph L, Pilote L, Eisenberg MJ. Alternative smoking cessation aids: a meta‐analysis of randomized controlled trials. American Journal of Medicine 2012;125(6):576‐84. [DOI] [PubMed] [Google Scholar]
Ter Riet 1990
- Ter Riet G, Kleijnen J, Knipschild P. A meta‐analysis of studies into the effect of acupuncture on addiction. Brirish Journal of General Practice 1990;40:379‐82. [PMC free article] [PubMed] [Google Scholar]
Vincent 1987
- Vincent CA, Richardson PH. Acupuncture for some common disorders: a review of evaluative research. Journal of the Royal College of General Practitioners 1987;37:77‐81. [PMC free article] [PubMed] [Google Scholar]
Wen 1973
- Wen HL, Cheung SYC. Treatment of drug addiction by acupuncture and electrical stimulation. Asian Medical Journal 1973;9:138‐41. [Google Scholar]
White 2001
- White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complementary Therapies in Medicine 2001;9(4):237‐45. [DOI] [PubMed] [Google Scholar]
White 2009
- White AR, Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupuncture in Medicine 2009;27(1):33‐5. [DOI] [PubMed] [Google Scholar]
Yoon 2004
- Yoon SS, Kwon YK, Kim MR, Shim I, Kim KJ, Lee MH, Lee YS, Golden GT, Yang CH. Acupuncture‐mediated inhibition of ethanol‐induced dopamine release in the rat nucleus accumbens through the GABA(B) receptor. Neuroscience Letters 2004;369(3):234‐8. [DOI] [PubMed] [Google Scholar]
Yoon 2010
- Yoon SS, Kim H, Choi KH, Lee BH, Lee YK, Lim SC, et al. Acupuncture suppresses morphine self‐administration through the GABA receptors. Brain Research Bulletin 2010;81(6):625‐30. [DOI] [PubMed] [Google Scholar]
Yoshimoto 2006
- Yoshimoto K, Fukuda F, Hori M, Kato B, Kato H, Hattori H, et al. Acupuncture stimulates the release of serotonin, but not dopamine, in the rat nucleus accumbens. Tohoku J Exp Med 2006;208(4):321‐6. [DOI] [PubMed] [Google Scholar]
Zhang 1992
- Zhang X. Acupuncture and moxibustion in smoking abstinence: a five year review with analysis of reports on the treatment of 15,866 cases. International Journal of Clinical Acupuncture 1992;3(2):149‐54. [Google Scholar]
References to other published versions of this review
White 1997
- White AR, Rampes H, Ernst E. Acupuncture for smoking cessation. Cochrane Database of Systematic Reviews 1997, Issue 1. [DOI: 10.1002/14651858.CD000009] [DOI] [Google Scholar]
White 2002
- White AR, Rampes H, Ernst E. Acupuncture for smoking cessation. Cochrane Database of Systematic Reviews 2002, Issue 2. [10.1002/14651858.CD000009.pub2] [DOI] [PubMed] [Google Scholar]
White 2011
- White AR, Rampes H, Liu JP, Stead LF, Campbell J. Acupuncture and related interventions for smoking cessation. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD000009.pub3] [DOI] [PubMed] [Google Scholar]


