OBJECTIVES:
Hepatic encephalopathy (HE) is common in advanced cirrhosis and is characterized by marked neuropsychiatric abnormalities. However, despite its severity and effects on brain function, the impact of HE on psychological status of patients has not been adequately assessed. The aim of this study was to evaluate the effect of HE on psychological status of patients and their informal caregivers.
METHODS:
Fifteen patients with cirrhosis and episodic or persistent HE and their corresponding informal caregivers were included. Semistructured interviews were performed in patients and caregivers. Quality of life (QoL) was assessed by the short-form 36 in both patients and caregivers, and the Zarit burden score was measured in caregivers. The analysis of interviews was performed using qualitative methodology.
RESULTS:
HE causes a major psychological impact on patients with HE. The first episode of HE caused a very significant impact that was reported with deep feelings, mainly of fear, anger, misery, anxiety, and sorrow, which persisted with time. Symptoms causing more psychological impact on patients were impaired ability to walk and speak. All effects were associated with a marked impairment in QoL. The psychological impact was also marked in caregivers who had a major burden, as assessed by the Zarit score. Moreover, QoL, particularly the mental component score, was markedly impaired in caregivers in intensity similar to that of patients.
DISCUSSION:
HE has a profound psychological impact on patients and their informal caregivers, associated with a marked negative influence on QoL. The psychological effects of HE on patients and caregivers should be evaluated and treated.
Hepatic encephalopathy (HE) is very common in patients with advanced liver cirrhosis (1,2). The probability of developing the first episode of HE after diagnosis of uncomplicated cirrhosis ranges between 5% and 25% at 5 years of follow-up (1,3,4). Most importantly, the risk is much greater in patients who have already suffered from an episode of HE, reaching 40% at 1 year (5). Besides, HE is a prognostic indicator in patients with cirrhosis. In fact, HE has been found to be an independent predictive factor of mortality in many studies (1,2), and the survival rate after the first episode of HE is as low as 42% at 1 year (6). HE also represents a major cause of hospital admissions of patients with cirrhosis because of the recurrent nature of the condition (1,7–10). In the United States, HE accounted for approximately 110,000 hospitalizations every year during the period 2005–2009 (11). Finally, HE has a major impact on health-related quality of life (QoL) and socioeconomic status of patients with cirrhosis and represents a heavy burden for the caregivers (12).
Despite its high frequency and important clinical impact of HE on the natural history of cirrhosis, the possible negative effects of HE on psychological status of patients with cirrhosis have not been assessed. Specifically, the impact of the first and successive episodes of HE on patients' psychological status and the way patients and their caregivers see the progression of their disease and its effects on QoL have not been reported. This is particularly relevant considering that HE is a complication arising primarily from cerebral dysfunction compared with other complications of cirrhosis that are largely related to extracerebral organs. In this context, the current study was aimed at assessing the impact of HE on psychological status of patients with cirrhosis and their respective caregivers. All caregivers were informal caregivers, i.e., unpaid caregivers, mostly spouses or siblings.
PATIENTS AND METHODS
Patient population
Patients with cirrhosis and their respective informal caregivers who were seen at the Liver Unit of the Hospital Clínic in Barcelona were eligible for this study. The inclusion criteria were as follows: (i) diagnosis of cirrhosis based on either liver biopsy or standard clinical, laboratory, and ultrasonographic findings; (ii) age between 18 and 80 years; and (iii) a minimum of 2 bouts of episodic HE requiring hospital admission or visit to the emergency department or persistent HE, as defined by international guidelines (1). The exclusion criteria were as follows: (i) Wilson disease; (ii) neurodegenerative diseases; (iii) severe chronic extrahepatic diseases (cancer, dementia, chronic obstructive pulmonary diseases, heart failure, and chronic kidney disease requiring dialysis); and (iv) active drinking in patients with alcoholic cirrhosis at some point during the 12 months before inclusion in the study. If patients had more than one informal caregiver, the closest one was selected.
Study development
Semistructured interviews were performed in both patients and caregivers. These types of interviews were selected because they allow flexibility, facilitate empathy, enable the interview to explore new topics, and tend to produce rich data (13). Questions of the interviews are shown in Table 1, Supplementary Digital Content 2, http://links.lww.com/CTG/A253. Interviews were performed in a quiet room by an experienced nurse and were performed separately for patients and caregivers. All interviews were taped and were subsequently transcribed. Eighteen patients were recruited into the study. Recruitment ended when the research team noticed data saturation in the interviews performed.
Demographic, clinical, and laboratory data were collected from all patients at the time of inclusion in the study. Psychometric and QoL evaluation was performed in all patients. Psychometric assessment was performed with the Psychometric Hepatic Encephalopathy Score, which includes a combination of several psychometric tests (14). Health-related QoL was evaluated using the Medical Outcomes Study Short-Form 36 (SF-36) self-administered questionnaire (15,16). The SF-36 is a generic standardized instrument including 36 items divided into 8 domains. It measures 4 domains in the area of physical health and 4 domains in the area of mental health. Two summary scores can be obtained, a physical component score (PCS) and a mental component score (MCS). The domains range from 0 to 100, whereas the summary scores for the PCS range from 8 to 73, and scores for the MCS range from 10 to 74. A higher score indicates a better QoL.
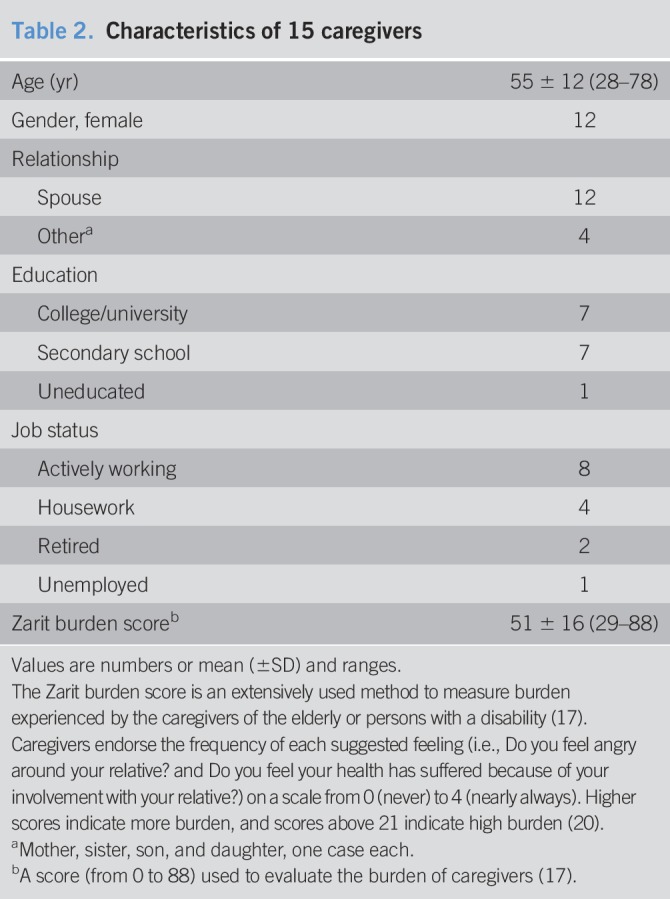
Demographic, family relationship, and educational information was collected from all caregivers. In addition, the Zarit Burden Interview was used to evaluate the burden of the caregivers (17). It consists of a caregiver self-report measure that contains 22 items. Each item is a statement that the caregiver is asked to endorse using a 5-point schedule. Response options range from 0 (never) to 4 (nearly always). A higher score up to 88 indicates heavier burden. QoL of caregivers was also assessed with the SF-36.
Analysis
The analysis of the interviews was performed using hermeneutic phenomenology (18). The transcribed interviews were analyzed by 2 researchers who are anthropologists (R.M. and N.F.). The data analysis consisted of 2 phases; in the first phase, the data were analyzed to obtain codes in an inductive manner. To stay as close as possible to the phenomenon described by the participants, coding was inductive and open, not yet classified or interpreted through the theoretical frameworks, and an unrestricted number of facets were expressed in preliminary code names. In the second phase, the relevant codes were grouped into categories, which were based on at least one code.
All patients and caregivers provided written informed consent to participate in the study. Patients and caregivers were informed before the interview about the purpose of the interview and that they could withdraw from the study at any time even after finishing the interview. To preserve patient confidentiality, all names were substituted by fictitious names. Moreover, only the involved researchers had access to the interview transcripts. The sample size was determined by data saturation of interviews. Saturation was defined when categories were well described and dimensionalized. Saturation is not dependent on the amount of data collected and analyzed but rather occurs when no significant new insights are emerging (i.e., additional interviews are not generating novel data necessary for fleshing out the categories that have already emerged) (19). However, a sample size calculation was also performed using changes in QoL data. Assuming a 25% reduction of the SF-36 values in the study population with respect to the normal population, with 80% power and alpha of 0.05, 15 patients were needed. The protocol was approved by the Institutional Review Board of the Hospital Clínic in Barcelona. Descriptive statistics was performed for all demographic, clinical, and laboratory variables. Data are expressed as mean and SD.
RESULTS
Characteristics of the study population
Of the 18 patients included, 3 were subsequently excluded, 2 because they withdrew consent before the interview and one because of an emergent admission to hospital. Therefore, the study population consisted of 15 patients with cirrhosis and their respective informal caregivers. The main characteristics of patients and caregivers are shown in Tables 1 and 2. The median time elapsed between the first episode of HE and the interview was 24 months (range 2–72 months).
Table 1.
Characteristics of 15 patients with cirrhosis and HE included in the study
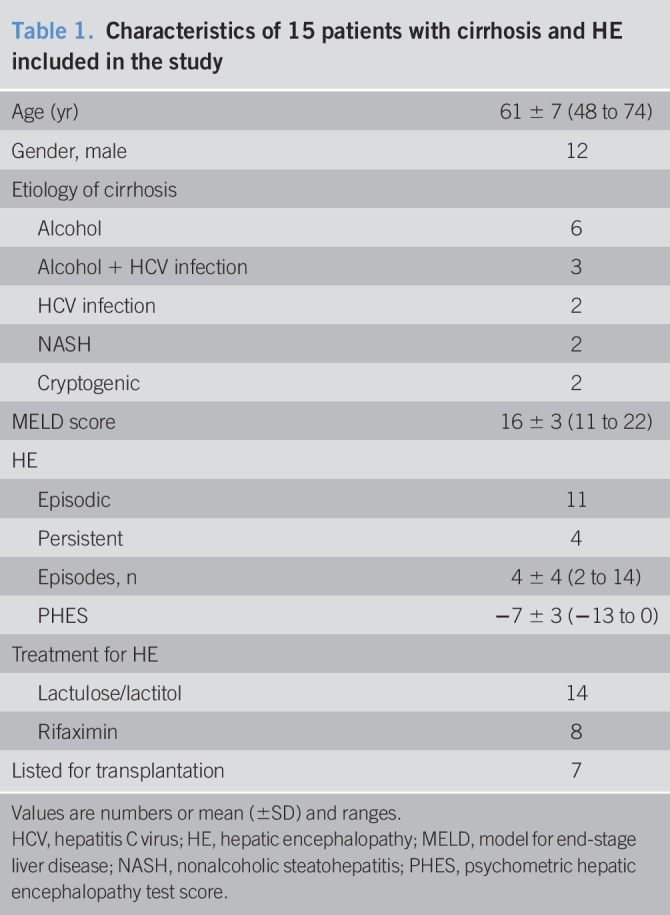
Table 2.
Characteristics of 15 caregivers
QoL of patients and caregivers and relationship with disease burden
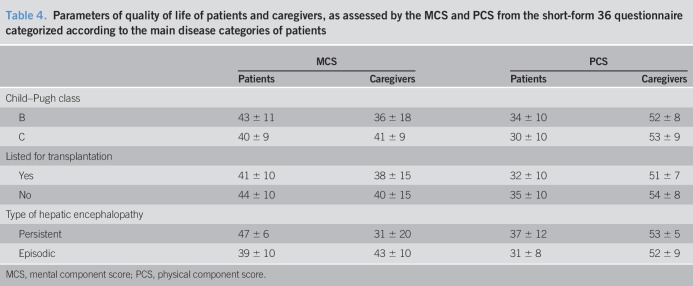
Both patients and caregivers had markedly impaired QoL indicators (Tables 3 and 4). Interestingly, values in caregivers were similar or only slightly higher than those of patients and markedly lower than those of a reference population.
Table 3.
Results of different domains of the short-form 36 in patients and caregivers
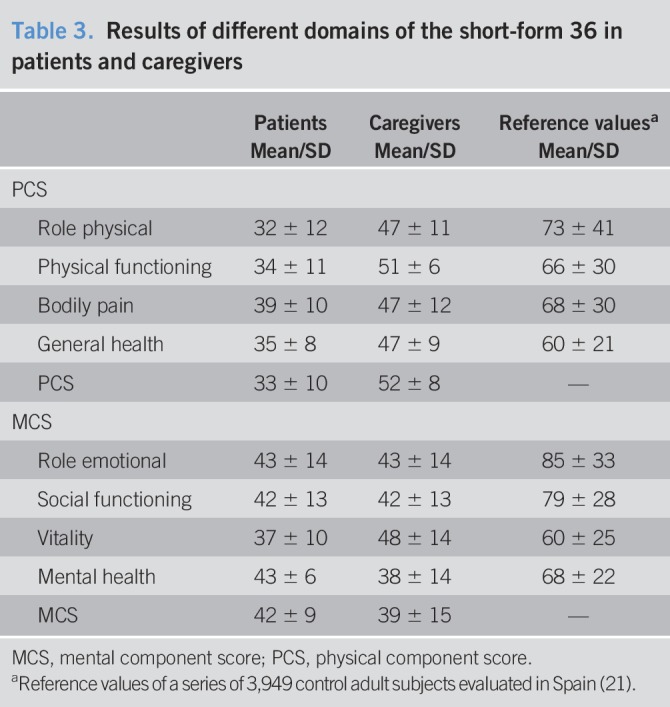
Table 4.
Parameters of quality of life of patients and caregivers, as assessed by the MCS and PCS from the short-form 36 questionnaire categorized according to the main disease categories of patients
Consistent with the impaired quality of life of caregivers, the average Zarit burden score was high, which indicates a heavy burden related to care (Table 2). The Zarit burden score had a significant direct correlation with several components of the SF-36, including role physical, general health, vitality, social functioning, and mental health (r > 0.50 for all; P < 0.05). By contrast, values of the Psychometric Hepatic Encephalopathy Score did not correlate with either the MCS or PCS of their corresponding caregivers.
Psychological burden of hepatic encephalopathy
Personal experience with the first episode of HE
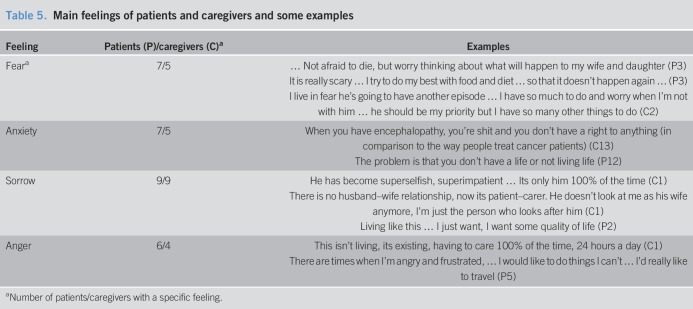
In general, the first episode was striking and totally unexpected. Single words most commonly used by patients and caregivers to explain the experience of the first bout of HE were misery, sorrow, trauma, disorientation, surprise, fear, anxiety, and lack of awareness (Table 5 and Figure 1, Supplementary Digital Content 1, http://links.lww.com/CTG/A252).
Table 5.
Main feelings of patients and caregivers and some examples
An interesting issue reported in several interviews was that most patients and caregivers had not received information from their physicians about HE and found the information on Internet. In fact, several caregivers complained about this lack of information, as reported in the following examples (code after verbatim represents patients [P] or caregivers [C] and their respective numbers).
“… at the beginning I thought it was Alzheimer's because some members of his family have got Alzheimer's. But, when symptoms were more severe, I looked on the internet ….” (C8)
“… I found the information online. Before I knew nothing, nobody explained it to me.” (C12)
Personal experience about clinical symptoms
Patients and caregivers reported their experiences about the symptoms of HE. Some examples are as follows:
“Yesterday, it started again with … the speech. I recognize it immediately with the speech; it seems that he is … drunk … and then the movement, because he is very slow, very slow with the movements, and then …. He gets very clumsy, much more clumsy.” (C1)
“I used to speak fluently, my speech was very fluent, … but now it is very hard to find the right words. It is very difficult.” (P1)
“… I would have prefer to have ascites, since it can be punctured. … I know … other complications like varices can be treated. One banding and the problem is solved. But …, the encephalopathy is very difficult to handle.” (P12)
“… I remember I was disoriented and talking very slowly. … I felt nervous, increasingly nervous and irritated.” (P2)
“I could not speak well … and had a complete disorientation. … I did not know what I was saying and where I was going ….” (P4)
“… very distressing. Because I wanted to move forward but my legs were going sideways … they were not listening to me ….” (P8)
“… there were moments in which he could not walk. He lost his balance … and all these things.” (P12)
Pharmacological treatment and diet
Comments were mainly related to the person who had the responsibility of adherence to the prescribed treatment and also with respect to the effects of laxatives and enemas. In male patients, the person responsible for taking care of treatment was the caregiver who was almost always a woman. In female patients, the same patient and not the caregiver was responsible for taking care of treatment. Although most patients stated the effectiveness of laxatives/enemas in treating or preventing the bouts of HE, several persons complained about the limitations that these treatments caused in their social life.
“… I think there should be other medications that could prevent these encephalopathies ….” (C1)
“You are always afraid …, I am always afraid of not eating this … not eating that. You control the protein … if I feel little confuse … I run to a colon cleanse/rectal laxative.” (P1)
Feelings and emotions
Patients and caregivers expressed a number of feelings and emotions that are summarized in Table 5 and Table 2, Supplementary Digital Content 3, http://links.lww.com/CTG/A254. An example of the feelings of caregivers is as follows:
“I am angrier, because I have a lot of work at home with him. Sometimes, I think I should prioritize myself; then … I think I would have to do better with him.” (C2)
“He has become superegoistic, superimpatient … he wants to absorb you 100%. And I tell you that he does not care anything more than him, nothing more than him … Once I have loved him, now I don't know! … Our situation … matrimonial … has changed a lot, that is, we have weakened a lot. He does not speak, he does not smile. It has changed a lot!” (C1)
Limitations of daily life and coping with the disease
Patients were more dependent on the presence of a caregiver, whereas caregivers were generally convinced that patients should be almost always under close surveillance. However, some patients said that they still could do some of their regular activities.
“… it seems that I'm 88 years old and I'm like a baby that needs to be cleaned up … I don't want to live like this …, I prefer what the physician on duty told me once, we will stop and do not go far … but, … I want a little QoL, you know, I'm not saying to live like a 20-year old, but I would like to be able to go out. This (HE) has happened to me not 1, 2, or 5 times, … many times more.” (P2)
“… I'm not afraid and have no problem in doing it, I drive my motorcycle and I'm not afraid of doing it ….” (P4)
Finally, some caregivers and patients even see the situation in a positive way, considering their previous life experiences:
Our relationship as a couple has not been affected. In fact, it's better than before (laughs), it's better than before. Because at least, I say that before I had a teenager, a rebellious teenager and very bad and now I have a … a child, I have a better child and I am much better. I prefer a child than a rebellious teenager, and then we get along and my daughter too ….” “I'm calmer even though it is more tied. Because it does not give me problems, it does not give me discussions.” (C10)
“… I am not sad, even now I am more alive, happier, I don't care about the disease …, I have it, then I have to endure.” (P10)
“There is no relationship between husband and wife. I feel like a mother, a sergeant, a policeman, a nurse, …. I'm just rounding the whole day! All of this affects a lot, … that will surely go worse!” (C4)
DISCUSSION
The clinical manifestations of HE, either covert or overt, have been well studied and are extensively described in guidelines and reviews (1,2). However, there is very limited information on the psychological effects that HE may have on patients. The findings of the current study clearly demonstrate that HE produces a major psychological impact not only on patients with cirrhosis but also on their main caregivers. HE influences markedly the way patients and caregivers cope with cirrhosis, causes a major limitation in their regular activities, and has a striking emotional impact, altogether being associated with a marked impairment in QoL.
The current study is unique in that it represents to the best of our knowledge the first study evaluating the psychological effects of HE as assessed by qualitative methodology based on interviews of patients and their main caregivers. One of the main findings of this study is that the first episode of HE has a major impact on patients and their families, probably because of the profound alteration of cognitive function. The main terms used to explain the feelings that patients and caregivers had after the first episode of HE were fear, anger, anxiety, and sorrow. These feelings persisted during a long period even if HE did not recur and affected their lives ever since. Importantly, fear had multiple components, including fear of death, having another episode of HE, being left alone at home, going out, and so forth. Another interesting finding was that the 2 manifestations of HE episodes that were more consistently repeated by patients and caregivers were difficulty to speak and move. By contrast, agitation and irritation, which are frequently considered the main components of HE by physicians, were mentioned less frequently in the interviews by both patients and caregivers. It cannot be excluded, however, that this could be due at least in part to a deliberate elimination of these signs by caregivers in an intention to “protect” patients from symptoms related to bad behavior. Moreover, patients clearly stated that they preferred to have other complications of cirrhosis, such as large ascites or gastrointestinal bleeding, than HE. Another important aspect that appeared repeatedly in relation to the first episode of HE was that it was completely unexpected. Moreover, most patients were not informed about the possible development of neurological complications of cirrhosis and consequently were not educated on what to do if they developed symptoms of HE. Therefore, education of patients and caregivers on the potential development of HE should be implemented to improve their knowledge about the disease.
There is limited information on burden that HE causes to patients and families. We are aware of only one qualitative study analyzing the effects of HE on patients with cirrhosis (22). The analysis identified 4 different thematic groups: multiple losses (memory, physical and communicative abilities, control, and identity), anxiety, dependency on others, and social isolation. However, the study included only 8 patients and did not analyze the effect of HE on their caregivers and did not correlate it with QoL or disease burden. Our results extend these previous findings by indicating that HE has a major impact on QoL of patients and represents a huge burden for caregivers. Hence, patients with HE had values of MCS and PCS of the SF-36 QoL questionnaire that were among the lowest reported in patients with decompensated cirrhosis (16,23,24). Moreover, and most importantly, the main caregivers of patients with HE had high Zarit burden scores, indicative of a major burden related to the care of patients with HE. Only 2 studies have been reported analyzing the effects of HE on caregivers (25,26). Bajaj et al. (25) reported the existence of a high burden in the caregivers of patients with HE, but a comparison of values between this study and the current study cannot be made because the latter study used the shortest form of the Zarit score, made of 12 questions, whereas in the current study, the longer form of 22 questions was used. Most importantly, values of the Zarit burden score in our series of caregivers were similar to those reported for caregivers of patients with Alzheimer disease, which indicates that the burden for caregivers of patients with HE compares similarly to that of caregivers of patients with dementia (27). Finally, this severe burden was associated with a marked impairment in the QoL scores of caregivers. In fact, values of MCS of caregivers were similar to those of patients and particularly lower for caregivers of patients with persistent HE (Table 3). Furthermore, values of MCS and PCS of caregivers were markedly lower compared with those of the general population of similar sex and age (21). Finally, another study provided qualitative information on experiences of caregivers of patients with HE and showed that despite an initial shock, caregivers demonstrated marked acceptability and responsibility of care (26). Overall, these findings indicate that caregivers of patients with HE suffer from tremendous impairment of their QoL.
We believe that the findings of the current study are clinically relevant and may help improve the current approach to the overall management of patients with HE. First, the current findings call for better education of patients with cirrhosis and their families on clinical manifestations, particularly HE, evolution, and outcomes of the disease. In this regard, we propose the implementation of educational programs for patients with cirrhosis and their relatives led by nurses with expertise in the management of patients with chronic liver diseases (28). Second, the major psychological impact that HE has on patients and their caregivers suggests that the multidisciplinary team dealing with patients with cirrhosis should include a psychologist to address the emotional issues related to the disease and particularly to HE. Psychologists are usually part of multidisciplinary teams for liver transplantation. However, our results suggest that psychological support should not be restricted to patients' candidates or in the waitlist for transplantation and should also be used in patients not candidates to transplant. Finally, and most importantly, special attention should be placed on caregivers of patients with HE in a way similar to that provided to caregivers of patients with dementia or other major chronic debilitating conditions (29).
The current study is unique in that it analyzes information from individual interviews to capture the psychological effects of HE together with data of QoL and burden of disease. However, the study has also some limitations that should be mentioned. First, the number of patients included appears small but is adequately powered. Studies using qualitative methodology include a lower number of patients than those using quantitative methodology. Moreover, recruitment of patients in the current study was canceled when saturation of data was noticed (19). Second, only patients with overt HE were included. Therefore, the findings may not apply to patients with exclusively covert HE. Evaluation of the psychological impact of covert HE should be assessed in future studies. Finally, the findings with respect to the feelings related to the first episode of HE may be altered because of recall bias because the median time elapsed between the first episode of HE and the interview was relatively long in some of the patients included.
In conclusion, the results of the current study indicate that HE has a major psychological impact on patients and their informal caregivers, which is associated with a profound negative influence on their quality of lives. Physicians, nurses, nurse practitioners, and physician assistants dealing with patients with cirrhosis should be aware of these effects of HE on both patients and caregivers and apply measures to counteract their negative consequences.
CONFLICTS OF INTEREST
Guarantor of the article: Núria Fabrellas, PhD.Specific author contributions: Núria Fabrellas, PhD, and Rebeca Moreira, BSN, contributed equally to this work. Conceived and designed the study: N.F. and R.M. Patient identification and data collection, including subject's assessment and blood tests: R.M., M. Carol, M. Cervera, G.P., M.P., A.J., E.P., C.S., I.G., E.S. Interview transcriptions: N.F., E.V., M.S., R.S., and R.M. Analysis of data: N.F., R.M., C.S., and E.S. Wrote the first draft of the paper: N.F., R.M., and P.G. Critical revision of data and manuscript revision: N.F., R.M., M. Carol, M. Cervera, G.P., M.P., E.V., M.S., R.S., A.J., E.P., C.S., I.G., E.S., P.S.K., P.G.
Financial support: Supported by grants awarded to N.F. (2014PREUI_UB), School of Nursing, Faculty of Medicine and Health Sciences of the University of Barcelona and P.G. (PI16/00043), N.F. (PI18/01330) both grants integrated in the Plan Nacional Investigación cientifíca, Desarrollo e Innovación Tecnológica (I + D + I) and cofunded by Instituto Carlos III (ISCIII)-Subdirección General de Evaluación and the European Regional Development Fund. P.G. is a recipient of an Institució Catalana d'Investigació i Estudis Avançats (ICREA) Academia Award. Also supported by a grant from Agencia de Gestió d'Ajuts Universitaris i de Recerca (AGAUR_SGR 01281).The funding sources had no role in the study design; collection, analysis, and interpretation of data; or writing of the report or decision to submit the paper.
Potential competing interest: None to report.
Study Highlights.
WHAT IS KNOWN
✓ HE is a common and severe complication of patients with advanced cirrhosis characterized by the development of neuropsychiatric manifestations.
✓ HE is associated with a marked impairment in QoL of patients, but input on caregivers is less known.
WHAT IS NEW HERE
✓ HE causes a major psychological impact on patients with HE, which parallels the psychological impact on informal caregivers that affects negatively their QoL.
✓ The first episode of HE was completely unexpected as most patients were not aware about the possible development of neurological complications of cirrhosis.
✓ Physicians and nurses caring for patients with HE should be aware of these negative psychological influences of HE on both patients and caregivers and apply measures to counteract them. Education about HE should also be performed.
TRANSLATIONAL IMPACT
✓ The correlation of the findings with quality of life parameters of both patients and caregivers and burden of disease. The care professionals, Doctors, Nurses and other health care providers should take measures to counteract the psychological burden an influence of the disease.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank all the faculty (physicians and nurses) of the Liver Unit of the Hospital Clinic in Barcelona for their support in this study. We also are very pleased with Roser Poblet and Nicki vanBerckel for their help. Finally, we would like to thank the patients and their families for their generosity to share their fears, feelings, and so forth, for this investigation.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A252, http://links.lww.com/CTG/A253, http://links.lww.com/CTG/A254
REFERENCES
- 1.American Association for the Study of Liver Diseases, European Association for the Study of the Liver. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J Hepatol 2014;61:642–59. [DOI] [PubMed] [Google Scholar]
- 2.Patidar KR, Bajaj JS. Covert and overt hepatic encephalopathy: Diagnosis and management. Clin Gastroenterol Hepatol 2015;13:2048–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: Natural history and prognostic factors. Hepatology 1987;7:122–8. [DOI] [PubMed] [Google Scholar]
- 4.Benvegnù L, Gios M, Boccato S, et al. Natural history of compensated viral cirrhosis: A prospective study on the incidence and hierarchy of major complications. Gut 2004;53:744–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma BC, Sharma P, Agrawal A, et al. Secondary prophylaxis of hepatic encephalopathy: An open-label randomized controlled trial of lactulose vs. placebo. Gastroenterology 2009;137:885–91. [DOI] [PubMed] [Google Scholar]
- 6.Bustamante J, Rimola A, Ventura PJ, et al. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol 1999;30:890–5. [DOI] [PubMed] [Google Scholar]
- 7.Berman K, Tandra S, Forssell K, et al. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol 2011;9: 254–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajaj JS. Liver capsule: Hepatic encephalopathy. Hepatology 2015;62:955. [DOI] [PubMed] [Google Scholar]
- 9.Graupera I, Solà E, Fabrellas N, et al. Urine monocyte chemoattractant protein-1 is an independent predictive factor of hospital readmission and survival in cirrhosis. PLoS One 2016;30(6):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cordoba J, Ventura-Cots M, Simón-Talero M, et al. Study Investigators of EASL-CLIF Consortium. Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J Hepatol 2014;60:275–81. [DOI] [PubMed] [Google Scholar]
- 11.Stepanova M, Mishra A, Venkatesan C, et al. In-hospital mortality and economic burden associated with hepatic encephalopathy in the United States from 2005 to 2009. Clin Gastroenterol Hepatol 2012;10:1034–41. [DOI] [PubMed] [Google Scholar]
- 12.Montagnese S, Bajaj JS. Impact of hepatic encephalopathy in cirrhosis on quality-of-life issues. Drugs 2019;79(Suppl 1):11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith JA. Semi-structured interviewing and qualitative analysis. In: Smith JA, Harre R, Langenhove LV, (eds). Rethinking Methods in Psychology. Sage: London, 1995, pp 9–26. [Google Scholar]
- 14.Weissenborn K, Ennen JC, Schomerus H, et al. Neuropsychological characterization of hepatic encephalopathy. J Hepatol 2001;34:768–73. [DOI] [PubMed] [Google Scholar]
- 15.Warw JE, Kosinski M, Dewey JE. How to Score Version 2 of the SF-36 Health Survey. Quality Incorporated: Lincoln, United Kingdom: 2000. [Google Scholar]
- 16.Orr JG, Homer T, Ternent L, et al. Health related QoL in people with advanced chronic liver disease. J Hepatol 2014;61:1158–65. [DOI] [PubMed] [Google Scholar]
- 17.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980;20:649–55. [DOI] [PubMed] [Google Scholar]
- 18.Laverty SM. Hermeneutic phenomenology and phenomenology: A comparison of historical and methodological considerations. Intern J Qual Meth 2003;2:21–35. [Google Scholar]
- 19.Foley G, Timonen V. Using grounded theory method to capture and analyze health care experiences. Health Serv Res 2015;50:1195–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan S, Kellner S, Gutierrez J, et al. The experience of essential tremor caregivers: Burden and its correlates. Front Neurol 2017;8:396–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.López-García E, Banegas JR, Graciani Pérez-Regadera A, et al. Population-based reference values for the Spanish version of the SF-36 Health Survey in the elderly. Med Clin 2003;120:568–73. [DOI] [PubMed] [Google Scholar]
- 22.Ladegaard Groenkjaer L, Hoppe T, Norlyk A, et al. Overt hepatic encephalopathy experienced by individuals with cirrhosis: A qualitative interview study. Gastroenterol Nurs 2017;41:468–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moscucci F, Nardelli S, Pentassuglio I, et al. Previous overt hepatic encephalopathy rather than minimal hepatic encephalopathy impairs health-related QoL in cirrhotic patients. Liver Inter 2011;31:1505–10. [DOI] [PubMed] [Google Scholar]
- 24.Solà E, Watson H, Graupera I, et al. Factors related to QoL in patients with cirrhosis and ascites: Relevance of serum sodium concentration and leg edema. J Hepatol 2012;57:1199–206. [DOI] [PubMed] [Google Scholar]
- 25.Bajaj JS, Wade JB, Gibson DP, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol 2011;106:1646–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Künzler-Heule P, Beckmann S, Mahrer-Imhof R, et al. Being an informal caregiver for a relative with liver cirrhosis and overt hepatic encephalopathy: A phenomenological study. J Clin Nurs 2016;25:17–8. [DOI] [PubMed] [Google Scholar]
- 27.Reed C, Belger M, Scott Andrews J, et al. Factors associated with long-term impact on informal caregivers during Alzheimer's disease dementia progression: 36-month results from GERAS. Int Psychogeriatr 2019;28:1–11. [DOI] [PubMed] [Google Scholar]
- 28.Fabrellas N, Carol M, Torrabadella F, et al. Nursing care of patients with chronic liver diseases: Time for action. J Adv Nurs 2018;74:498–500. [DOI] [PubMed] [Google Scholar]
- 29.Griffin JM, Meis LA, Greer N, et al. Effectiveness of caregiver interventions on patient outcomes in adults with dementia or Alzheimer's disease: A systematic review. Gerontol Ger Med 2015;1:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.