Summary
The present study aims to document the epidemiologic features and outcomes of burn injuries in Southeastern Iran based on International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) guidelines. This retrospective cross-sectional study was carried out at Khatam-Al-Anbiya Hospital. Patient demographics, including burn injury data and outcome data were collected from medical records and analyzed through descriptive and analytical statistics using SPSS software. A total of 3,030 burn patients were included in this study. A total of 55% of the subjects were males. The largest age group included patients aged 15-44 (61%). The majority of burns were caused by flame (70.5%), and most of them were third-degree burns (73%). Mean affected total body surface area (TBSA) was 43.98%±30.75% in all subjects and 80.85%±21.41% in the deceased individuals. Most of the burns were accidental (66.2%), and 37% of them occurred in winter. Mean hospital stay was 4.49±4.67 days (within the range of 1–113 days). A quarter of all patients admitted to the hospital died (24.9%). The number of admitted patients, mean length of stay (LOS), and the mortality rate showed a decreasing trend from 2007 to 2016. In contrast, the total mortality rate was high. The significant predictors of mortality included being female, flame burns, longer LOS, a larger TBSA, burns of higher degrees, as well as burn complications. The documentation of burn data, based on ICD-10 directives, standardizes findings from burn injury analyses and leads to the comparability of data at different national and international levels.
Keywords: epidemiology, outcomes, burn injuries, burns, mortality, risk factors
Abstract
Cette étude rapporte l’épidémiologie et le devenir des patients brûlés dans le sud- est iranien, en utilisant la CIM 10. Elle a été conduite dans l’hôpital Khatam-Al-Anbiya. Les données démographiques ainsi que celles concernant la brûlure et le devenir des patients ont été analysées, en utilisant SSPS. Parmi les 3 030 patients, 55% étaient des hommes. La tranche d’âge la plus représentée (61%) était 15–44 ans. La majorité des brûlures, très souvent (73%) de 3ème degré étaient dues à une flamme (70,5%). La surface brûlée était globalement de 43,98+/30,75% (80,85+/-21,41% chez les patients décédés). Les brûlures étaient le plus souvent accidentelles (66,2% des cas), 37% d’entre elles survenant en hiver. La durée d’hospitalisation était de 4,49+/-4,67 jours (1-113), le quart (24,9%) des patients étant décédés. On observe une baisse du nombre de patients, de la durée de séjour et de la mortalité entre 2007 et 2016, cette dernière restant élevée. Les variables corrélées à la mortalité sont le sexe féminin, la brûlure par flamme, l’augmentation de la surface brûlée et de la durée de séjour, la profondeur de la brûlure et l’existence de complications. L’utilisation de la CIM 10 permet une standardisation des études épidémiologiques, ce qui les rend comparables entre elles.
Introduction
Burns are crippling injuries and are more common in developing as well as low- and middle-income countries,1 where more than 95% of severe burns occur.2 Burn injuries have serious consequences, such as negative impacts on mobility and growth of extremities,3 long-lasting psychological effects on patients,4 scar deformities, contracture deformities, and tissue defects,5 which may lead to disability. The World Health Organization (WHO) has reported that about 180,000 deaths occur annually due to burn injuries in low- and middle-income countries.6More than 100,000 people annually are burned in Iran.7-10 The mortality rate of burn patients in Iran has been estimated at about 10%.10,11
Furthermore, burn consequences are not limited to the physical health of patients but affect social, economic and physiological domains as well.12 In 2015, Karimi et al. reported that the average cost for each patient, each percent of burns, and one-day stay at hospital was US$ 2.810, US$ 162, and US$ 195, respectively.13 Burn consequences are more challenging in low- and middle-income countries.14
Burns are preventable, according to the WHO.6
Reports indicate the success of burn prevention programs in developed countries. The lack of a coherent and robust program for the prevention of burns is evident in developing countries.15 The epidemiology and outcome of burns are significantly influenced in different parts of the world by cultural factors, civilization and industrialization.16,17 In a national study, Sadeghian et al. found a significant decrease in the burn-related age-standardized mortality rate from 6.1 in 1990 to 1.7 per 100,000 individuals in 2015.18
However, based on past research, the incidence of burn injuries in Iran has had an increasing trend.19,20
Epidemiological studies are required in each region to design and implement effective preventive programs. 21 Furthermore, due to incomplete and inconsistent burn data in developing countries, they could not be comparable at national and international levels. Thus, there is a need to improve the quality of burn data and decrease the related ambiguity through data standardization.22
International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10), is the global standard for health information designed to enable the assessment of health parameters. 23 ICD-10 contains detailed data on burns, including the site, severity (degree), percentage, and cause of burn injuries, as well as the location of burn occurrence and the type of the victim’s activities.24 It is necessary to utilize this global standard to describe the data obtained from epidemiological studies on burns for the standardization and comparison of burn data. This study aims to document the epidemiologic characteristics and outcome of burn injuries in Southeastern Iran based on ICD-10 guidelines.
Methods
Data sources
Data for this retrospective cross-sectional study were obtained from the records of patients admitted to Khatam-Al-Anbiya Hospital affiliated to Zahedan University of Medical Sciences, Zahedan, Iran, from April 2007 to March 2016. Zahedan is the capital of Sistan and Baluchestan Province.25 Among other provinces of Iran, Sistan and Baluchestan ranks lowest in terms of development indicators; in addition, it is the least developed province in terms of health indicators. According to the Statistical Center of Iran, Sistan and Baluchestan Province had a population of 2,775,014 in 2016, with 1,401,931 and 1,373,083 men and women, respectively. In the same year, Zahedan had a population of 672,589, with 342,524 and 330,065 men and women, respectively. In addition, it has an area of 36,581 km2.26
Sargolzaie et al. found out that injuries had the highest mortality rate among other diseases in Zahedan.25 Khatam-Al-Anbiya Hospital is the only center for burn injuries in the city, which covers almost all other cities in the province.27
Study design and patient record selection
The complete records of inpatients from April 2007 to March 2016 were used. Burn patients’ records were selected according to ICD-10 categories for burns and corrosions codes (T20–T32). The study population consisted of the records of all inpatients with burn injuries in all age groups at the mentioned burn center. The total number of inpatients’ records with burn injuries in the Hospital was 3,047 for the aforementioned period, out of which 17 records were excluded because over 20% of the required data were incomplete. Sampling was not conducted, and all 3,030 records were reviewed for data collection.
Data collection
A predesigned checklist was used for data collection. The checklist included burn patients’ record number, age, gender, marital status, occupation, place of residence (urban or rural), type of insurance, education, referral method, pregnancy status, burn year, burn intent, burn site, burn percentage, burn severity (degree), location of burn occurrence, activity at the time of burn injuries, burn reason, external cause of burn, disposition, burn injury complications and comorbidity, as well as length of stay (LOS). To standardize data collection and presentation, ICD-10 volumes 1 and 2 were used for the categorization of burn patients’ age and activity, burn site, burn degree, extent of total body surface area (TBSA), location of burn occurrence, burn etiology, as well as burn intent. ICD-10 volume 1 classifies the site of burns and corrosions into 11 categories from T20 to T30. It also classifies TBSA into categories T31 and T32.28 The authors referred to the Medical Records Department of the Hospital and carefully reviewed all inpatient records on burn injuries. Next, they entered the data of the records in a pre-designed checklist.
Statistical analysis
The collected data were entered into SPSS software and analyzed using descriptive (mean, frequency, and percentage) as well as analytical (a chi-square test, a one-way ANOVA, Spearman’s rho, and the Pearson correlation coefficient) statistics. Pvalue< 0.05 was considered significant.
Results
Study population
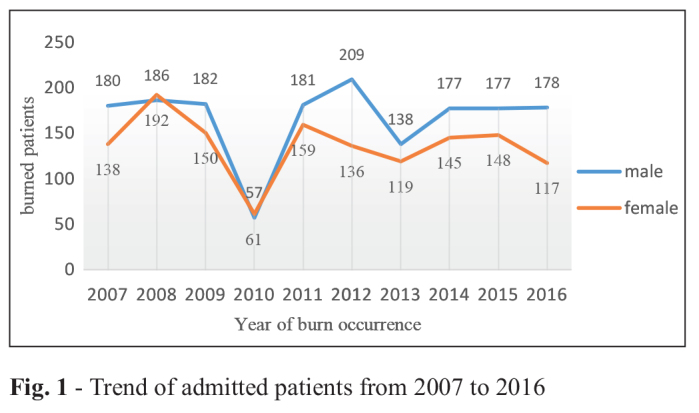
Although the number of patients with burn injuries showed a decreasing trend in both sexes in 2010, this decreasing trend has been insignificant over the past 10 years, and has been more prominent in women than in men. Furthermore, the mortality rate showed a decreasing trend from 26.45% in 2007 to 15.9% in 2016 (Fig. 1).
Fig. 1. Trend of admitted patients from 2007 to 2016.
Demographics
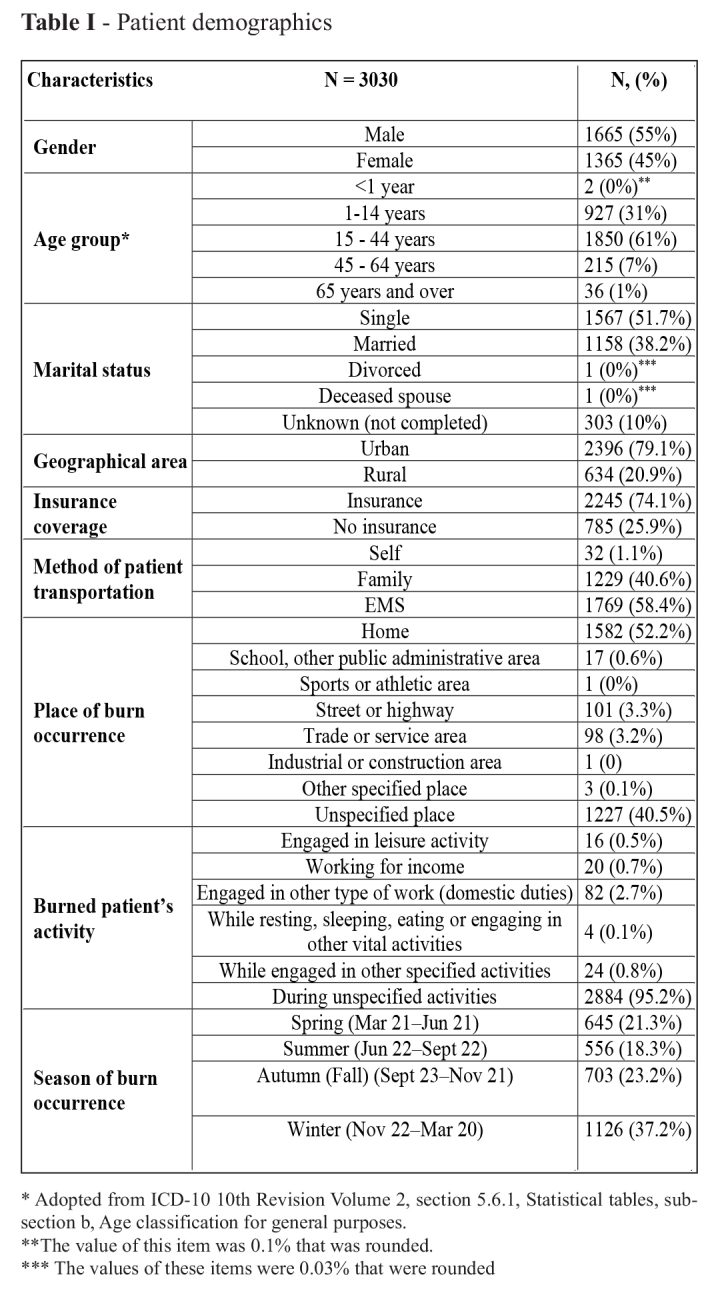
A total of 3,030 patients with burn injuries were admitted to Khatam-Al-Anbiya Hospital during the study period: 55% and 45% were male and female, respectively (male to female ratio 1.22:1). The patients had a median age of 21 years (interquartile range [ITQ] 9-30) and a mean ± standard deviation (SD) age of 22±15.38 years. Most of the patients were aged 15 to 44 years (61%). The age groups were adopted from WHO.24 About half of the patients were single (51.7%), more than 75% of them lived in urban areas, and the rest lived in rural areas. The most common method of patient transfer to the burn center was by ambulance (58.4%). The next common transfer methods were by the patient’s family members (40.6%) followed by being referred to the center (1.1%, n=32). About 75% of the patients were covered by a health insurance plan (74.1%). Over half of the burns occurred at home (52.2%), followed by unspecified places (40.5%). The burn patients’ activity had not been specified in most of the records (95.2%). The majority of the burns occurred in winter (37.2%). The employment status of 96.8% of the patients was unspecified, 30 patients (1%) were unemployed, 40 patients (1.3%) were employed, and 28 patients (0.9%) had at-home jobs. The education level of none of the patients was recorded in medical records. Out of 1,365 women, 74 individuals were pregnant, and 31 individuals (41.89%) died (Table I).
Table I. Patient demographics.
Burn etiology
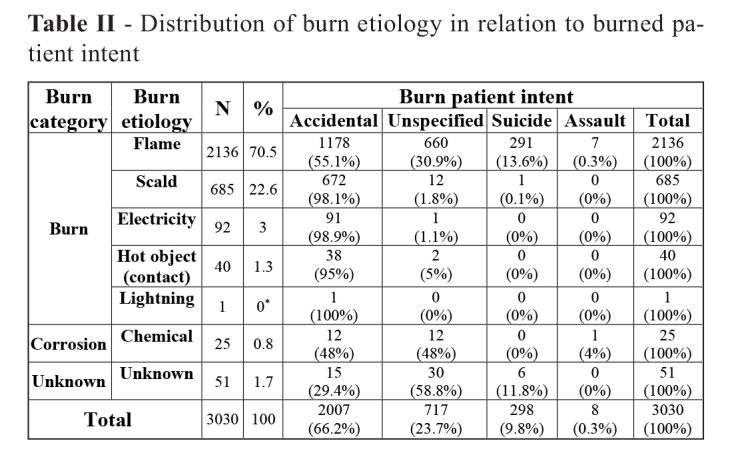
The most frequent burn etiology was flame, which occurred in 70.5% of the cases. It was followed by scald injuries in 22.6%, electrical burns in 3%, contact burns in 1.3%, unknown causes in 1.7%, chemical burns in 0.8%, as well as lightning burns in 0.03% of the cases. The most common burn intent was accidental, which was recorded for 66.2% of the patients, followed by unspecified intent in 23.7%, suicide in 9.8%, and assault in 0.3% of the cases (Table II).
Table II. Distribution of burn etiology in relation to burned patient intent.
Burn sites
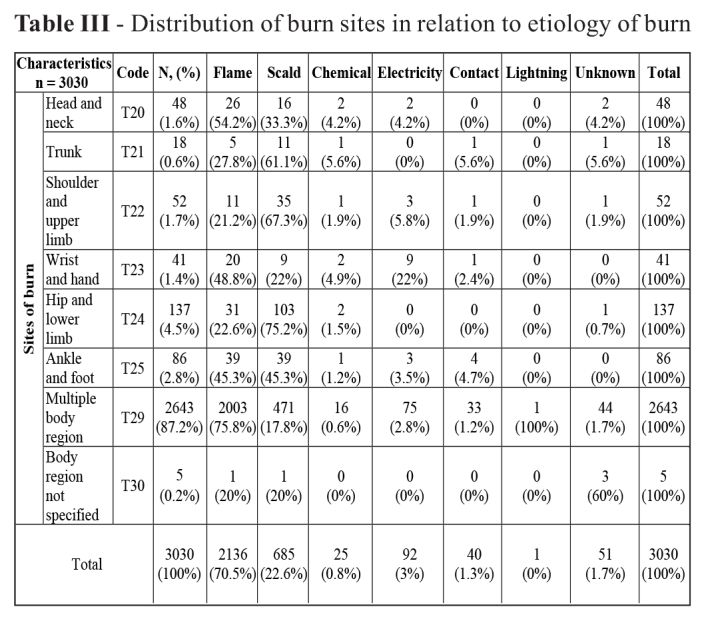
Most of the burns (87.2%) affected multiple body regions. The hip and the lower limb were the most common burn sites among others. Our findings showed that flame was a common burn etiology in the head, neck, wrists and hands. The trunk, shoulders, the upper limb, the hip and the lower limb were mainly burned by scald injuries. Electrical burns mainly occurred in the wrists and hands (Table III). Burn degree (severity)
Table III. Distribution of burn sites in relation to etiology of burn.
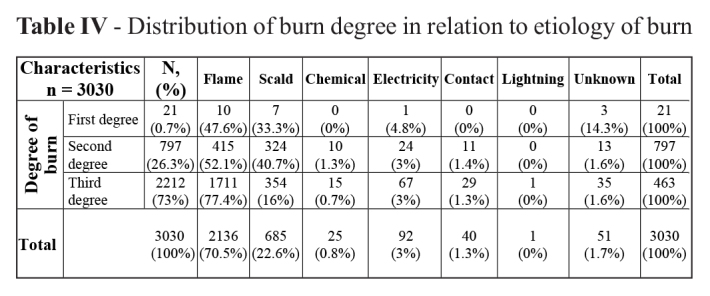
The majority of the patients had third-degree burns (73%), followed by second-degree (26.3%) and first-degree (0.7%) burns. Flame and scald burns were the most common causes in all burn degrees (Table IV).
Table IV. Distribution of burn degree in relation to etiology of burn.
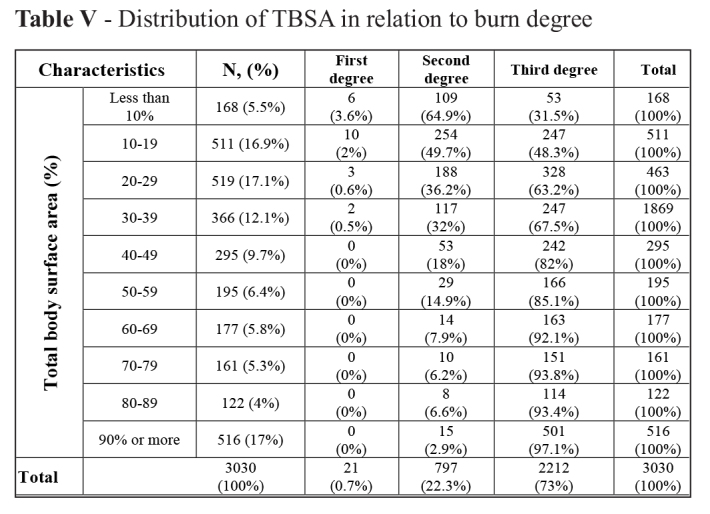
Total body surface area (TBSA)
ICD-10 TBSA subdivisions were applied in this study. The affected mean TBSA was 43.98%±30.75% (within the range of 2-100%). The highest TBSA frequency was related to the 10-19%, 20-29%, and ≥90% categories. There was a significant correlation between TBSA and burn degree (Pearson’s correlation coefficient = 0.421, P = 0.000), indicating that an increase in TBSA would be associated with an increase in burn degree (Table V).
Table V. Distribution of TBSA in relation to burn degree.
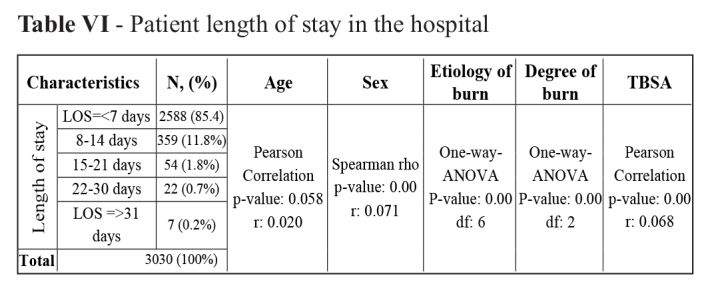
LOS
Hospital stay ranged from 1 to 113 days with a mean stay of 4.49±4.67 days. More than 75% of the patients had a hospital stay of 7 days or shorter (85.4%), and only 7 patients had a hospital stay of 30 days or longer (0.2%). The 15-44 years age group was the most common age group in all LOS categories. Patients with electrical burns had significantly longer LOS (p-value = 0.000). There was a significant positive correlation between burn degree and LOS because patients with higher burn degrees had longer LOS (p-value= 0.000). Pearson’s correlation coefficient showed a weak positive correlation between TBSA and LOS, indicating that patients with a higher TBSA had longer LOS. However, there was no correlation between age and LOS (p-value=0.058). Furthermore, a weak positive correlation was observed between sex and LOS as women had longer LOS than men (p-value= 0.000) (Table VI).
Table VI. Patient length of stay in the hospital.
Outcomes
Less than half of the patients were discharged with some improvement (39.2%), 30% of the patients left the hospital against medical advice (LAMA), and 11 of them were transferred to burn centers in other cities. In total, 756 deaths occurred in 3,030 patients, indicating a mortality rate of 25%. Among them, 15% and 10% of the patients were female and male, respectively (female to male death ratio 1.5:1). The highest rate of death was in the 14-44 years age group. Furthermore, flame was the most common cause of burns leading to death. The most common burn intent in death cases was accidental (41.1%), followed by unspecified intent (31.1%) and suicide (27.5%). Only two burn patients died due to homicide (0.3%).
Mortality
Out of 756 deceased patients, 83.2% had a hospital stay of 7 days or less, 13.8% stayed there for 8-14 days, 1.7% stayed for 15-21 days, 1.2% stayed for 22-30 days, and only one patient (0.1%) had a hospital stay of 31 days or more. Additionally, the extent of burns in over half (56.7%) of the deceased patients was 90% or higher. The mean and standard deviation of age, LOS and TBSA among patients who died from burns was 22±14.64 years (within the range of less than 1 year and 74 years), 4.99±5.65 days (within the range of 1-113 days), and 80.85%±21.41% (within the range of 9-100%), respectively. In addition, there was a significant negative correlation between mortality rate and LOS (r = -0.121, p-value = 0.000), as the deceased patients had shorter LOS than the ones who survived (Table VII).
Table VII. Distribution of deceased patients in relation to age, sex, LOS, burn degree, TBSA, etiology and intent.
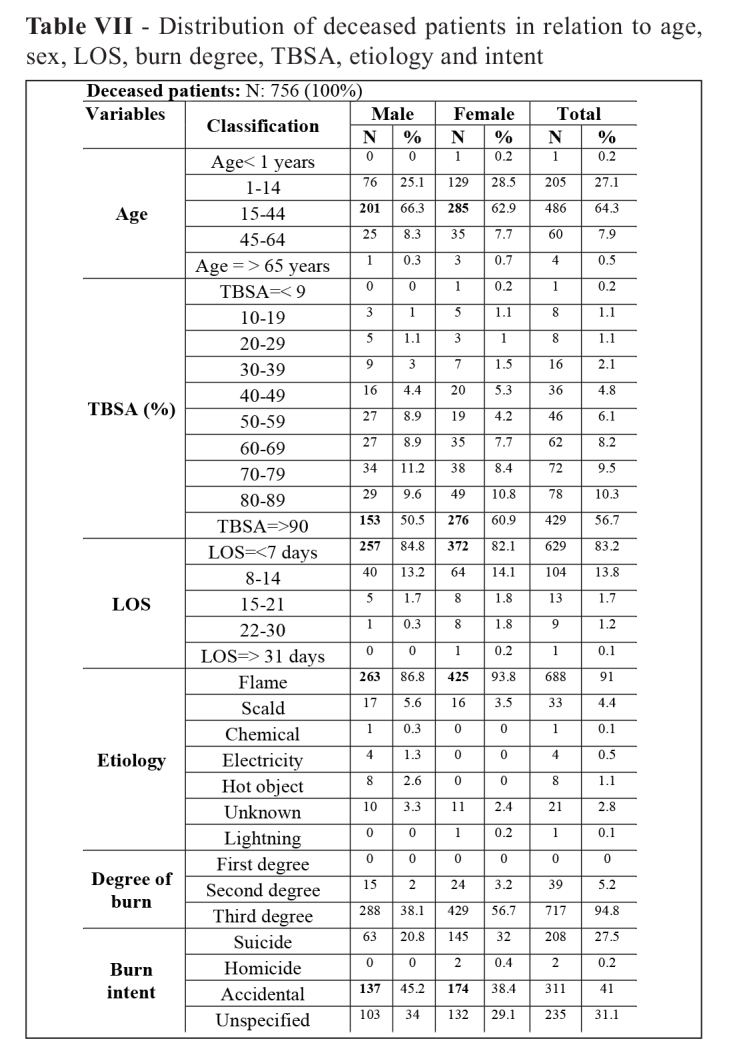
About 25% of all 3,030 burn patients admitted to the center died (female to male ratio 1.49:1). Out of the total 756 deceased patients, 486 patients (64.3%) were aged 15-44 years. More than half of the patients had a TBSA of 90% or more (56.7%). There was a significant positive correlation between mortality rate and TBSA in the deceased patients (r = 0.402, p-value = 0.000), as a higher TBSA led to death more frequently than a lower TBSA. Most of the deceased patients had a hospital stay of 7 days or less. Flame was the most common burn etiology among the deceased patients (91%). The chi-square test revealed that mortality rate increased significantly in burn patients with a flame etiology (pvalue = 0.000). Moreover, accidental burns were the most common burn intent in the deceased patients (41%). The chi-square test showed a significant correlation between mortality rate and burn intent (pvalue = 0.000). Sixty-nine percent of the deceased patients had second- and third-degree burns. A significant correlation was found between mortality rate and burn degree (r = 0.192, p-value = 0.000), as an increase in burn degree increased mortality rate.
Complications and comorbidities
Infection was the most common complication of burn injuries in burn patients (n=183, 6%), followed by renal disease (n=20, 0.7%), respiratory poisoning (n=17, 0.6%), bedsores (0.5%), convulsions (n=14, 0.5%), cardiovascular disease (n=13, 0.4%), and abortion (n=6, 0.2%).
Out of 363 comorbidities reported with burns, addiction (n=142), cardiovascular disease (n=58), neurological disease (n=51), diabetes mellitus (n=30), hyperlipidemia (n=19), mental disorders (n=17), respiratory disease (n=17), hyperthyroidism (n=4), diseases of the blood and blood-forming organs (n=13), digestive diseases (n=6), genitourinary disease (n=2), malignancies (n=2), and infectious disease (n=2) were the most common comorbidities, respectively.
Discussion
A total of 3,047 patients with burn injuries were admitted to Khatam-Al-Anbiya Hospital from 2007 to 2016. To the best of our knowledge, the present study is the largest regional epidemiological study of burn patients in Zahedan. This retrospective study aimed to characterize the trend, etiology, site, severity, TBSA, intent, time and outcome of burn patients admitted to Khatam-Al-Anbiya Hospital so as to provide epidemiologic data for future planning, policy-making and injury prevention measures.
Burn injury prevalence and trend
The Statistical Center of Iran estimated the population of Sistan and Baluchestan Province and Zahedan city to be 2,775,014 and 672,589, respectively in 2016. Over a 10-year period, the prevalence rate of burn injuries in the mentioned populations was 1.09 and 4.5 per 1,000 persons in Sistan and Baluchestan Province and Zahedan city, respectively. Despite the slight decrease in burn injuries in some years over the 10-year period, there have been no significant changes in the burn injury trend over this period in this center, and burn injuries have posed serious threats to the health of this community. LOS was shorter in 2016 than in previous years; however, the study showed that the mortality rate decreased slightly over the 10-year period. These findings indicate the need for more effective burn prevention and treatment procedures.
Sex
The male-to-female burn ratio was 1.22:1 in this study, being consistent with Li et al., Jin et al., Iqbal et al., Soltan et al., Danesh et al. and Sharma et al.16,29-33 In addition, the female-to-male ratio was 1.49:1 in the deceased patients, being similar to Sharma et al. and Queiroz et al.33,34 The Spearman’s rho test showed a weak positive correlation between sex and mortality rate (r = 0.053, p-value = 0.000), indicating a higher mortality rate in women than in men. According to our findings, being female was a predictor of mortality. Moreover, women had longer LOS than men (p-value = 0.000). Death occurred in 10.6% (145/1365) and 3.8% (63/1665) of female burn patients and male burn patients, respectively, with suicide intent. These findings indicate that women had a higher tendency to commit suicide than men. Suicide attempts in women could be due to poor cultural and socioeconomic status, uncertainties about solving individual and family problems, and their easy access to flammable materials at home. Panjeshahin et al.35 and Ansari Moghaddam et al.27 reported similar results.
Age
Most of the burn victims were in the most productive age group of 15-44 years (61%), followed by the age groups of 1-14 years (31%) and 45-64 years (7%). Only 36 victims (1%) were in the 65 years and above age group. Out of 756 deaths, 64.3% were in the 15-44 years age group, followed by the 1-14 years (27.1%) and 45-64 years (7.9%) age group. Only 4 (0.5%) and 1 (0.2%) deceased patients were in the 65 years or more and less than one year age group, respectively. Despite the fact that mortality rate is expected to be higher in older people and children, the results of this study showed that the highest mortality rate was in the 15-44 years age group. Moreover, the Pearson’s correlation test showed that age had no significant effects on mortality rate in the deceased patients (r = 0.023, p-value = 0.100), which was consistent with Danesh et al. and Queiroz et al.32,34, but different from Iqbal et al.16 The findings could be explained by the age distribution of the population in Sistan and Baluchestan Province based on the 2016 census in Iran, according to which almost half of the province population (n=1,342,592, 48.38%) was aged 14-44 years.26
Burn site
The upper extremity has been introduced as the most common burn site in the literature.30,36 Our findings showed that the most common anatomical regions affected in burn victims were multiple regions (87.2%) followed by the hip and the lower limb (4.5%), ankles and feet (2.8%), shoulders and the upper limb (1.7%), the head and neck (1.6%), as well as the trunk (0.6%). These findings were similar to Page et al., Yoon et al., and Ortiz-Prado et al.36-38 but differed from Jin et al., Gilbert et al., and Li et al.30,39,40 The majority of the deceased patients were burned in multiple body regions (99.5%). In addition, only three deceased patients had burn injuries in the hip and the lower limb (0.4%), and one patient had burn injuries in the shoulder and the upper limb (0.1%). People’s flammable clothes in this province could explain the reason for burns in the hip and the lower limb. Therefore, burns affecting more than two regions at the same time caused more deaths.
Etiology
More than 2,850,000 people die from burns in low- and middle-income countries every year.41 In the present study, flame was the most frequent cause of burn injuries, accounting for 70.5% of all burn injuries, which was similar to Karimi et al., Wang et al., Ortiz-Prado et al., Kumar et al., and Ringo and Chilonga,13,21,38,41,42 but different from Soltan et al., Al-Shaqsi et al., and Hosseini et al.31,43,44 Moreover, it was found in this study that the majority of the deceased patients (91%) were burned with flame. The results indicate a correlation between mortality rate and flame burns. Easy access to various sources of flame at home or at work and the use of unsafe kerosene heaters could explain the high frequency. Although flame and scald burns were the most frequent burns in both men and women, chemical and electrical burns affected men more than women. This is due to the fact that men are more exposed to chemicals and electricity than women through occupational exposure, which makes it more likely for them to be affected by these burn etiologies.
TBSA
According to the study results, about 95% of the admitted patients had burn injuries on more than 10% of their TBSA. These findings are consistent with the results of Iqbal et al. and Al-Shaqsi et al.16,43 The highest frequency of affected TBSA was seen in the 20-29%, 90% or more, and 10-19% categories, respectively. In addition, 56.7% of the deceased patients had burn injuries on more than 90% of their TBSA. According to past research, a TBSA of over 20% is connected with a mortality rate of about 10%, which increases exponentially with an increase in TBSA.43,45 This study also revealed a positive correlation between mortality rate and a higher TBSA because an increase in TBSA increased the mortality rate.
Burn degrees
Most of the patients had third-degree burns (73%) followed by second-degree burns (26.3%). First-degree burns only accounted for 0.7% of all burns. These findings were consistent with those of the majority of other studies carried out in developing and developed countries,21,37,40,46 but different from some others.42,47-49 The majority of burns of any degree occurred by flame. Furthermore, thirddegree burns were the most common burns in the deceased patients (94.8%) while second-degree burns were observed as well (5.2%). Moreover, there was a significant correlation between mortality rate and burn degree, for higher burn degrees were associated with higher mortality rates.
Burn intent
According to past research, burn injuries are responsible for 22% of all suicide attempts and 17% of suicide deaths in Iran.50 This study showed that the majority of the burns were accidental in nature (66.2%), while suicide (9.8%), homicide, and unspecified intent were observed as well. Accidental burns were the most common intent in deaths caused by burning (41%), followed by unspecified burns (31.1%), suicide burns (27.5) and homicide burns. These findings were consistent with those of other studies.51 In addition, this study revealed that about 70% of all suicide attempts by victims resulted in death. Family and marital conflicts as well as domestic violence against women are the major contributing factors for suicide in Iran.16 The findings of this study indicated that the suicide attempt rate was over two times higher in women than in men (203 women versus 95 men), and that 71% and 66% of the women and men died from suicide attempts, respectively.
LOS
According to the results of this study, the value of LOS is associated with sex, burn etiology, burn degree and TBSA. LOS increased with an increase in burn degree from first-degree to second- and third-degree burns (2.93±2.16 days, 3.36±3.67 days, and 4.91±4.92 days, respectively) (p = 0.00), which was similar to Gilbert et al.,39 in which it was observed that an increase in LOS led to a range of superficial to full-thickness burns. Electrical burns were associated with significantly longer LOS than other burn etiologies (p=0.00); in other words, the mean LOS values of flame, scald, chemical and electrical burns were 4.74±5.01, 3.53±2.82, 2.48±1.61, and 6.47±6.19 days, respectively. The mean LOS was 4.22 days and 5.43 days in TBSA<50% and in TBSA>50%, respectively, indicating a significant correlation between LOS and TBSA (p= 0.00). Moreover, the mean LOS was longer for women than men (4.17±3.66 days and 4.88±5.63 days, respectively), indicating a significant correlation between LOS and sex (p = 0.00). The majority of the deaths (83.2%) occurred during the first week of admission.
Time
The incidence of burns peaked in winter (Nov 22-Mar 20) (Table I), which is the coldest period in Southeastern Iran. This finding was similar to that of Kumar et al. and Brooks and McGwin,41,52 but different from that of Wang et al., Li et al., Jin et al., Koushyar et al., and Aldana and Navarrete.21,29,30,53,54 Moreover, 37% of the patients died in winter, 23.9% in spring, 20.2% in autumn, and 18.5% in summer. Heating water on a stove and spending more time indoors increases the possibility of burns in cold seasons. Thus, winter was associated with an increase in mortality rate (p = 0.01).
Mortality and complications
The male mortality rate was 21.61 and 88.46 cases per 100,000 men among burn patients in Sistan and Baluchestan Province as well as Zahedan city, respectively. In the same vein, the female mortality rate was 32.99 and 137.24 cases per 100,000 women among burn patients in Sistan and Bluchestan Province as well as in Zahedan city, respectively. In total, 756 deaths occurred in 3,030 patients, accounting for a mortality rate of 24.9%, being similar to Koushyar et al.53 but higher than some previous studies carried out in Iran13,27,32,55,56 and other countries.16,57,58 Moreover, the rate obtained in this study was lower than that obtained in studies designed for assessing patients admitted to intensive care units (ICU).34,59 The lack of a specialized burn center and unfavorable health indices in the province could be the causes of the high burn-related mortality rates. In total, 785 (25.9%) patients were covered by no health insurance plan, out of whom 278 patients (35.4%) left against medical advice (LAMA) and 254 (32.4%) died. The results showed that most of the patients who were covered by no insurance plan had to leave the hospital because of the financial costs of burn injuries. Karimi et al.13 reported that 31% of burn patients were covered by no insurance plan, which was consistent with the present study.
Out of the entire 268 reported complications, infections (n=183, 6%), renal disease (n=20, 0.7%), respiratory poisoning (n=17, 0.6%), bedsores (0.5%), convulsions (n=14, 0.5%), cardiovascular disease (n=13, 0.4%) and abortion (n=6, 0.2%) were the most frequent ones. Burn complications were positively correlated with mortality (p=0.00), but no correlation was found among comorbidities at the time of admission and mortality.
Limitations
The incompleteness of data in patient records, especially data on the place of burn occurrence, as well as the burn patients’ activity, occupation and educational level was the most important limitation of this study.
Conclusion
The present study examined some important information about the burn trend over a 10-year period, as well as etiology, severity, time, intent, TBSA and the affected groups. Hospital admission and the death trend decreased from 2007 to 2016. The highest rates of burn admission and burn deaths were observed in adolescents and young adults. The majority of the burn victims were males (55%) in contrast to females (45%), but the mortality rate was higher in females than in males (60% vs 40%). Accidental burns (41%) were the most common intent in the deceased patients, followed by suicide and homicide. Multiple sites (87.2%) and flame (70.5%) were the most common sites and etiology of burns, respectively. Fiftyseven percent of the deceased patients had a TBSA of 90% or more. Most of the admitted and deceased patients had a LOS of 7 days or less. Third-degree burns were the most common burns in all patients and in the deceased ones. In addition, infection and addiction were the most common complication and comorbidity reported, respectively.
The total mortality rate was high (25%) in this study. Being female, flame burns, longer LOS, larger TBSAs, burns of higher degree and burn complications were the significant predictors of mortality. Documenting the epidemiological and outcome data of burns based on ICD-10 guidelines standardizes findings from burn injury analyses and makes the comparability of the data possible at different national and international levels. In addition, improving health indicators, planning for reducing family conflicts and violence against women, as well as teaching the method of properly using heating equipment and dealing with fire, especially at home, could possibly reduce the casualties and devastating consequences of burn injuries.
Acknowledgments
Funding.This work was supported by the Vice Chancellor for Research and Technology of Zahedan University of Medical Sciences [Grant No. IR.ZAUMS.REC.1397.264].
Competing interest.The authors have no conflict of interest to disclose. All authors read and approved the final version of the manuscript.
Acknowledgement.The authors wish to thank the Vice Chancellor for Research and Technology of Zahedan University of Medical Sciences for supporting the project. They are also thankful to the hospital authorities of Khatam-Al-Anbia Hospital and in particular the head of the medical records department for their cooperation in data collection.
References
- 1.Atiyeh B, Masellis A, Conte C. Optimizing 1 burn treatment in developing low-and middle-income countries with limited health care resources (part 1). Ann Burns Fire Disasters. 2009;22:121–129. [PMC free article] [PubMed] [Google Scholar]
- 2.Tian H, Wang L, Xie W, Shen C. Epidemiologic and clinical characteristics of severe burn patients: results of a retrospective multicenter study in China, 2011–2015. Burns Trauma. 2018;6:14. doi: 10.1186/s41038-018-0118-z. doi: 10.1186/s41038-018-0118-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shakirov BM. Some different treatment of sandal burns of the hand in children. Int J Burns Trauma. 2017;7:120–123. [PMC free article] [PubMed] [Google Scholar]
- 4.Abdelhafiz A, Makboul M, Azab H, Khalifa H. The impact of antidepressant drugs on the psychological status of the hospitalized burn patients. Indian J Burns. 2015;23:43–49. doi: 10.4103/0971-653X.171648. [Google Scholar]
- 5.Grishkevich VM, Grishkevich M. Postburn scar contracture: formation, anatomy and classification. Adv Plast Reconstr Surg. 2016;1:18–24. [Google Scholar]
- 6.World Health Organization (WHO) Burns. 2018 Available from: https://www.who.int/newsroom/fact-sheets/detail/burns . [Google Scholar]
- 7.Dahmardehei M, Alinejad F, Ansari F, Bahramian M, Barati M. Effect of sticky mat usage in control of nosocomial infection in Motahary Burn Hospital. Iran J Microbiol. 2016;8:210–213. [PMC free article] [PubMed] [Google Scholar]
- 8.Karimi H, Motevalian SA, Momeni M. Epidemiology of outpatient burns in Iran: An update. Ann Burns Fire Disasters. 2014;27:115–120. [PMC free article] [PubMed] [Google Scholar]
- 9.Seyed-Forootan K, Karimi H, Motevalian S, Momeni M. LA50 in burn injuries. Ann Burns Fire Disasters. 2016;29:14–17. [PMC free article] [PubMed] [Google Scholar]
- 10.Shahmiri SS, Kolahdouzan M, Omrani A, Khazaei M. Determinants of mortality and the lethal area 50 index (LA50) in burn patients admitted to a large burn center; a single center experience. Bull Emerg Trauma. 2017;5:184–189. [PMC free article] [PubMed] [Google Scholar]
- 11.Mobayen M, Farzan R, Dadashi A, Rimaz S, Aghebati R. Effect of early grafting on improvement of lethal area index (LA50) in burn patients: a 7-year investigation in a burn referral centre in the North of Iran. Ann Burns Fire Disasters. 2017;30:189–192. [PMC free article] [PubMed] [Google Scholar]
- 12.Upadhyaya DN, Khanna V. Analyzing the socio-economic cost of burn care. Indian J Burns. 2012;20:53–54. [Google Scholar]
- 13.Karimi H, Motevalian S, Momeni M, Ghadarjani M. Financial burden of burn injuries in Iran: a report from the burn registry program. Ann Burns Fire Disasters. 2015;28:310–314. [PMC free article] [PubMed] [Google Scholar]
- 14.Nasoori A, Hoomand R. Maggot debridement therapy for an electrical burn injury with instructions for the use of Lucilia sericata larvae. J Wound Care. 2017;26:734–741. doi: 10.12968/jowc.2017.26.12.734. doi: 10.12968/jowc.2017.26.12.734. [DOI] [PubMed] [Google Scholar]
- 15.Stokes M, Johnson W. Burns in the Third World: an unmet need. Ann Burns Fire Disasters. 2017;30:243–246. [PMC free article] [PubMed] [Google Scholar]
- 16.Iqbal T, Saaiq M, Ali Z. Epidemiology and outcome of burns: Early experience at the country’s first national burns Centre. Burns. 2013;39:358–362. doi: 10.1016/j.burns.2012.07.011. doi: 10.1016/j.burns.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Rastegar Lari a, Alaghehbandan R. Epidemiological study of self-inflicted burns in Tehran, Iran. J Burn Care Rehabil. 2003;24:15–20. doi: 10.1097/00004630-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Sadeghian F, Moghaddam SS, Saadat S, Niloofar P. The trend of burn mortality in Iran - a study of fire, heat and hot substance-related fatal injuries from 1990 to 2015. Burns. 2018;45:228–240. doi: 10.1016/j.burns.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Aghajani MH, Haddadi M, Saadat S. Epidemiological pattern of injuries in Iran; a nationwide review of seven million emergency department admissions. Emerg (Tehran) 2017;5:e10. [PMC free article] [PubMed] [Google Scholar]
- 20.Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P. Recent trends in burn epidemiology worldwide: a systematic review. Burns. 2017;43:249–257. doi: 10.1016/j.burns.2016.08.013. doi: http://dx.doi.org/10.1016/j.burns.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang KA, Sun Y, Wu GS, Wang YR, Xia ZF. Epidemiology and outcome analysis of hand burns: a 5-year retrospective review of 378 cases in a burn center in Eastern China. Burns. 2015;41:1550–1555. doi: 10.1016/j.burns.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Martina NR, Wardhana A. Mortality analysis of adult burn patients. Jur Plast Rekons. 2013;2:96–100. doi: https://doi.org/10.14228/jpr.v2i2.155. [Google Scholar]
- 23.International Advisory Group for the Revision of ICD‐10 Mental Behavioural Disorders. A conceptual framework for the revision of the ICD‐10 classification of mental and behavioural disorders. World Psychiatr. 2011;10:86–92. doi: 10.1002/j.2051-5545.2011.tb00022.x. doi: 10.1002/j.2051-5545.2011.tb00022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO. Geneva: 2016. World Health Organization: International statistical classification of diseases and related health problems, 10th Revision. [Google Scholar]
- 25.Sargolzaie N, Kiani M, Salari M, Khosravi M. Top ten causes of death and life expectancy in Zahedan (South-East Iran) in 2014. Global J Health Sci. 2017;9:135–144. [Google Scholar]
- 26.Statistical Center of Iran: Detailed results of the Population and Housing Census - 2016 Tehran, Iran: Statistical Center of Iran, 2018. Available from: https://www.amar.org.ir/english/Population-and-Housing-Censuses. [Google Scholar]
- 27.Ansari-Moghaddam A, Baghbanian A, Dogoonchi M, Chooban B. Epidemiology of burn injuries in South-Eastern Iran: a retrospective study. Pak Med Assoc. 2013;63:1476–1481. [PubMed] [Google Scholar]
- 28.WHO. Geneva: 2016. World Health Organization: International statistical classification of diseases and related health problems, 10th Revision. [Google Scholar]
- 29.Li H, Yao Z, Tan J, Zhou J. Epidemiology and outcome analysis of 6325 burn patients: a five-year retrospective study in a major burn center in Southwest China. Sci Rep. 2017;7:460–466. doi: 10.1038/srep46066. doi: 10.1038/srep46066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jin R, Wu P, Ho JK, Wang X, Han C. Five-year epidemiology of liquefied petroleum gas-related burns. Burns. 217;44:210–217. doi: 10.1016/j.burns.2017.05.011. doi: 10.1016/j.burns.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 31.Soltan Dallal MM, Sharifi Yazdi MK, Rahimiforoushani A, Akhoondinasab MR. Epidemiology, etiology and outcomes of burn patients in a Referral Burn Hospital, Tehran. Tehran Univ Med J (TUMJ) 2016;74:344–349. [Google Scholar]
- 32.Danesh HA, Javanbakht S, Nourallahzadeh M, Bakhshani NM. Epidemiology and mortality of burn injuries in Eastern Iran since 2009: an analysis of 2115 cases. Int J High Risk Behav Addict. 2019;8:e66232. doi: 10.5812/ijhrba.66232. [Google Scholar]
- 33.Sharma NP, Duke JM, Lama BB, Thapa B. Descriptive epidemiology of unintentional burn injuries admitted to a tertiarylevel government hospital in Nepal. Asia Pac J Public Health. 2015;27:551–560. doi: 10.1177/1010539515585386. doi: 10.1177/1010539515585386. [DOI] [PubMed] [Google Scholar]
- 34.Queiroz LFT, Anami EH, Zampar EF, Tanita MT. Epidemiology and outcome analysis of burn patients admitted to an Intensive Care Unit in a University Hospital. Burns. 2016;42:655–662. doi: 10.1016/j.burns.2015.08.002. doi: http://dx.doi.org/10.1016/j.burns.2015.08.002 . [DOI] [PubMed] [Google Scholar]
- 35.Panjeshahin M-R, Lari AR, Talei A-R, Shamsnia J, Alaghehbandan R. Epidemiology and mortality of burns in the South West of Iran. Burns. 2001;27:219–226. doi: 10.1016/s0305-4179(00)00106-6. doi: https://doi.org/10.1016/S0305-4179(00)00106-6 . [DOI] [PubMed] [Google Scholar]
- 36.Page F, Hamnett N, D’Asta F, Jeffery S. Epidemiology of U.K. military burns 2008-2013. J Burn Care Res. 2017;38:e269–e276. doi: 10.1097/BCR.0000000000000370. doi: 10.1097/BCR.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 37.Yoon C, Cho YS, Park S, Chung SP, Choi YH. Epidemiology of burns caused by moxibustion in Korea. Burns. 2016;42:1588–1592. doi: 10.1016/j.burns.2016.04.015. doi: 10.1016/j.burns.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 38.Ortiz-Prado E, Armijos L, Iturralde AL. A population-based study of the epidemiology of acute adult burns in Ecuador from 2005 to 2014. Burns. 2015;41:582–589. doi: 10.1016/j.burns.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 39.Gilbert AD, Rajha E, El Khuri C, Bou Chebl R. Epidemiology of burn patients presenting to a tertiary hospital emergency department in Lebanon. Burns. 2017 doi: 10.1016/j.burns.2017.06.015. doi: 10.1016/j.burns.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 40.Li H, Wang S, Tan J, Zhou J. Epidemiology of pediatric burns in southwest China from 2011 to 2015. Burns. 2017;43:1306–1317. doi: 10.1016/j.burns.2017.03.004. doi:http://dx.doi.org/10.1016/j.burns.2017.03.004 . [DOI] [PubMed] [Google Scholar]
- 41.Kumar S, Ali W, Verma AK, Pandey A, Rathore S. Epidemiology and mortality of burns in the Lucknow Region, India - a 5 year study. Burns. 2013;39:1599–1605. doi: 10.1016/j.burns.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 42.Ringo Y, Chilonga Y. Burns at KCMC: epidemiology, presentation, management and treatment outcome. Burns. 2014;40:1024–1029. doi: 10.1016/j.burns.2013.10.019. doi:http://dx.doi.org/10.1016/j.burns.2013.10.019 . [DOI] [PubMed] [Google Scholar]
- 43.Al-Shaqsi S, Al-Kashmiri A, Al-Bulushi T. Epidemiology of burns undergoing hospitalization to the National Burns Unit in the Sultanate of Oman: a 25-year review. Burns. 2013;39:1606–1611. doi: 10.1016/j.burns.2013.04.012. doi: 10.1016/j.burns.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 44.Hosseini S, Rashtchi V, Kamali K, Moghimi M. Epidemiology and outcome of 2,590 burned patients in Northwest Iran. Ann Burns Fire Disasters. 2017;30:85–90. [PMC free article] [PubMed] [Google Scholar]
- 45.Ho W-s, Ying S. An epidemiological study of 1063 hospitalized burn patients in a tertiary burns centre in Hong Kong. Burns. 2017;30:85–90. doi: 10.1016/s0305-4179(00)00095-4. [DOI] [PubMed] [Google Scholar]
- 46.Belba MK, Petrela EY, Belba AG. Epidemiology and outcome analysis of sepsis and organ dysfunction/failure after burns. Burns. 2017;43:1335–1347. doi: 10.1016/j.burns.2017.02.017. doi: 10.1016/j.burns.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 47.Forjuoh SN. Burns in low-and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 48.Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns. 2011;37:1087–1100. doi: 10.1016/j.burns.2011.06.005. doi:https://doi.org/10.1016/j.burns.2011.06.005 . [DOI] [PubMed] [Google Scholar]
- 49.Khandarmaa T-O, Harun-Or-Rashid M, Sakamoto J. Risk factors of burns among children in Mongolia. Burns. 2012;38:751–757. doi: 10.1016/j.burns.2011.11.006. doi:https://doi.org/10.1016/j.burns.2011.11.006 . [DOI] [PubMed] [Google Scholar]
- 50.Saadat M, Bahaoddini A, Mohabatkar H, Noemani K. High incidence of suicide by burning in Masjid-i-Sulaiman (southwest of Iran), a polluted area with natural sour gas leakage. Burns. 2004;30:829–832. doi: 10.1016/j.burns.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 51.Batra AK. Burn mortality: recent trends and sociocultural determinants in rural India. Burns. 2003;29:270–275. doi: 10.1016/s0305-4179(02)00306-6. doi:https://doi.org/10.1016/S0305-4179(02)00306-6 . [DOI] [PubMed] [Google Scholar]
- 52.Brooks RD, McGwin G. The epidemiology of emergency department-treated burn injuries associated with portable heaters in the United States, 2003-2013. J Burn Care Res. 2017;38:e306–e310. doi: 10.1097/BCR.0000000000000376. doi: 10.1097/BCR.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 53.Koushyar H, Amouzgar MH, Taghi SM. The epidemiology of burns in Mashhad Imam Reza Burn Center (MIRBC). Horizon of Medical Sciences. 2004;10:43–50. [Google Scholar]
- 54.Aldana MCDR, Navarrete N. Epidemiology of a decade of pediatric fatal burns in Colombia, South America. Burns. 2015;41:1587–1592. doi: 10.1016/j.burns.2015.05.005. doi: 10.1016/j.burns.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 55.Amir Alavi S, Mobayen M, Tolouei M, Noursalehi I. Epidemiology and outcome of burn injuries in burn patients in Guilan province, Iran. Qom Univ Med Sci J. 2013;7:35–41. [Google Scholar]
- 56.Emami SA, Motevalian SA, Momeni M, Karimi H. The epidemiology of geriatric burns in Iran: a national burn registry-based study. Burns. 2016;42:1128–1132. doi: 10.1016/j.burns.2016.03.011. doi: http://dx.doi.org/10.1016/j.burns.2016.03.011 . [DOI] [PubMed] [Google Scholar]
- 57.Mason SA, Nathens AB, Byrne JP, Gonzalez A. Trends in the epidemiology of major burn injury among hospitalized patients: a population-based analysis. J Trauma Acute Care Surg. 2017;83:867–874. doi: 10.1097/TA.0000000000001586. doi: 10.1097/TA.0000000000001586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hwee J, Song C, Tan KC, Tan BK, Chong SJ. The trends of burns epidemiology in a tropical regional burns centre. Burns. 2016;42:682–686. doi: 10.1016/j.burns.2015.10.019. doi: 10.1016/j.burns.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 59.Hashmi M, Kamal R. Management of patients in a dedicated burns intensive care unit (BICU) in a developing country. Burns. 2013;39:493–500. doi: 10.1016/j.burns.2012.07.027. doi: https://doi.org/10.1016/j.burns.2012.07.027 . [DOI] [PubMed] [Google Scholar]


