Summary
Burn injury has become a major source of mortality and morbidity in countries with low socioeconomic status. World energy consumption is mainly based on fossil fuels. This source of energy, if not properly handled, can be a source of major accident to lives and properties. The aim of this study is to highlight cases and the outcome of management of burns from cooking gas explosions in Lagos, Nigeria. The study involved all patients who sustained burns following cooking gas explosion within the study period. The parameters considered included demography, spread, anatomical locations and presence of inhalational injury, and outcome of management. A total of 347 patients were treated for burns during the study period, and 49 had burns from cooking gas explosion. Male to female ratio was 1.04:1. Patients between the ages of 21-40 years were the most affected. Extremities were involved in nearly all the patients. The presence of inhalational injury and larger burn surface area were found to be poor prognostic indices. Mortalities occurred within the first two weeks of injury. Cooking gas is becoming increasingly popular in Nigeria. Prevalence of burns from gas explosion is also on the increase. People are however not aware of its safe handling. More public enlightenment is required.
Keywords: burns, cooking gas, explosion, inhalational injury
Abstract
Les brûlures représentent une cause de morbidité et de mortalité considérables dans les pays à IDH faible. L’énergie consommée dans le monde est principalement d’origine fossile et son mésugeage est la cause d’accidents aux conséquences humaines et matérielles graves. Cette étude s’est penchée les caractéristiques et l’évolution de 49 patients (sur 347) hospitalisés dans le CTB de Lagos après explosion de réchaud à gaz. Nous avons relevé la démographie des patients, la surface et la localisation des brûlures, l’existence éventuelle d’une inhalation de fumées et le devenir. Le sex-ratio M/F était de 1,04/1, la tranche d’âge 21-40 ans était la plus fréquemment touchée. Les extrémités de presque tous les patients étaient brûlées. L’augmentation de la surface brûlée et la présence d’une inhalation de fumées étaient des facteurs de mauvais pronostic. En cas de décès, la mort survenait dans la première quinzaine. L’augmentation de la prévalence des brûlures lors d’une explosion de réchaud à gaz est parallèle à l’augmentation de leur utilisation, ce qui montre que des campagnes d’information sont nécessaires.
Introduction
Burn injury has been associated with high mortality and morbidity in low socioeconomic countries. While the incidence is reducing in the developed world, the same cannot be said of low-income countries. 1 Among the causes of burns, flame was noted to be the most common in our environment, with mishandling of petroleum products accounting for many of the cases.2
Crude oil was discovered in Nigeria in 1956 and commercial exploration began in 1958. Nigeria is one of the leading members of the Organization of Petroleum Exporting Countries (OPEC) and was once Africa’s largest producer of crude oil.
The products obtained from refining petroleum include automotive gas oil, premium motor spirit, black oil and gases. Use of the various products from the refinery has been on the increase and there is a corresponding increase in the greenhouse effect of combustion of these products. In 2016, the world conference on climate change in Paris France de-emphasized the use of most of these fossil products. In Nigeria, in order to reduce the greenhouse effects of these products, people are being discouraged from the use of wood and other forest degradation products, and use of natural products is being encouraged.
Natural gas is bottled and marketed as cooking gas in Nigeria. Cooking gas is gradually replacing domestic energy sources like firewood, coal and charcoal. Cooking gas is also known as liquefied petroleum gas and is a mixture of 70% butane and about 30% propane. It has a flash point of -156F (-104C) and exists in vaporized or gaseous form at room temperature. This makes it extremely combustible.3 It is supplied to homes through pipes and in pressurized cylinders. It is heavier than air, hence displaces air upwardly. This makes it easy to cause suffocation when it leaks out into a closed environment. It burns without smoke hence is environmentally friendly and does not deplete the ozone layer of the atmosphere. When supplied in cylinders, it is usually filled to about 80% to 85% of its capacity to allow for thermal expansion of the gas. It is colourless and odourless hence ethanethiol is usually added to give its characteristic odour for easy detection of gas leakage.
The increased availability and use for domestic cooking purposes was not preceded by adequate public enlightenment on its safe handling procedures. This has resulted in an increase in the number of patients presenting at our centre with thermal burns resulting from domestic cooking gas explosion. The accidents are associated with high morbidity. In order to highlight the increasing danger associated with the use of cooking gas, we embarked on this study in which the characteristics of these injuries, risk factors involved, method and outcome of treatment were determined. It is hoped that the study will alert policy makers, safety officers and health planners to the need for designing and implementing ways of preventing these accidents.
Materials and methods
Study centre
This was a retrospective study of all patients admitted for burns due to cooking gas explosion between January 1st, 2016 and December 31st, 2017 to the Burns and Trauma (B and T) Centre of the Lagos State University Teaching Hospital (LASUTH), Ikeja-Lagos, Nigeria, where ethical clearance for the study was obtained. The Centre is located in Lagos, South-West Nigeria. It is a purposely-designed facility for burn care.
Patients
All consenting patients admitted for burn injury resulting from cooking gas explosions to the Burns Centre within the study period were recruited for the study. The records of the patients were retrieved from the Medical Record Department. The data collected was inclusive of demography, aetiology of burns, extent and depth of burns, presence of inhalational injury, morbidity, length of hospital stay, nature of valve and connecting conduit, complications and outcome of management.
Treatment protocol
Patients were received at the triage wing of the burn centre for assessment and commencement of management. History was documented and physical assessments were performed. The treatment protocol of the centre4,5 was undertaken in all patients, viz: the patients were reviewed by the burns specialist registrar at presentation into the emergency room (ER), who documented history and clinical findings and classified the injury as either minor burn or major burn. Burn surface area estimation was calculated using the Wallace Rule of Nine for adults and the Lund and Browder chart for children.6,7 Adults with less than 20% total body surface area (TBSA) and children less than 10% and with no inhalational injury or significant co-morbidity were categorized as minor burns: a higher TBSA with or without inhalational injury was regarded as a major burn. Patients with major burns were admitted to the burn ward while those with minor burns were treated in the ER and discharged for outpatient follow-up. Assessment of depth was clinically determined, and fluid resuscitation was done with Ringer’s Lactate using the Parkland formula. Urinary output was closely monitored to ensure adequate resuscitation.
Tetanus immune-prophylaxis was administered. Wound care included irrigation with normal saline, application of antibacterial agent and occlusive dressing. Microbial examination was done by taking wound biopsy for microscopy. All patients were commenced on prophylactic antibiotics from admission into the ER. Patients with suspected inhalational burns had arterial blood gasses (ABG) assessment and were admitted to the intensive care unit where 100% oxygen was administered via elective endotracheal intubation after being reviewed by the intensivist. Patients with deep dermal burns had wound excision and split thickness skin graft while areas with superficial burns were allowed to epithelise. Outcome was determined after the patient was discharged or died. The time of discharge occurred when over 95% of the wound had healed in the absence of significant morbidity. Clinical parameters were monitored until the final outcome.
Data collection and statistical analysis
Data were entered onto a proforma and manually entered into statistical package for social science (SPSS) version 20. The results for continuous variables were presented as Mean+SEM, while the results for discrete variables were presented as ratios, percentages and proportions. The confidence interval was 95% and significance level was p < 0.05. The data were further presented in descriptive format using tables and figures.
Exclusion criteria
Patients with burns from causes other than cooking gas were excluded from the study.
Results
Demography
A total of 347 patients were seen, admitted, and treated for burns from various causes in the unit over the study period. There were 224 (64.5%) males and 123 (35.5%) females, giving a female to male ratio of 1:1.8. Forty-nine (14.1%) patients had burn injury from cooking gas explosion: 25 were male (51%) and 24 (49%) female, with a female to male ratio (F: M) of 1: 1.04. Age of the victims ranged from 6 years to 68 years (mean ± SEM =31.51 ± 1.786) (Table I).
Table I. Age distribution of burns patients from cooking gas explosions.

Aetiology of explosions
The causes of explosion were leakage of gas from the cylinder stopper in 31 (63.3%) patients, leakage in the connecting pipes in 10 (20.4%) patients and failure to switch off the knobs on the cylinders in 8 patients (16.3%).
Levels of education
The number of patients with primary education was five (10.2%), 26 (53.1%) patients had secondary school education and 18 (36.7%) had tertiary education.
Knowledge of safety precautions and cost of valve/conduit tubes
None of the patients had a formal education on the mode of operating cooking gas cylinders. Knowledge was passed on to them by neighbours or family members. The cylinders did not have any instructional label attached to them. Forty-three (87.8%) patients used the low-cost cylinder stopper and tubing systems.
Occupation
Twenty-four (49%) patients were private entrepreneurs, 11 (22.4%) were civil servants and 11 (22.4%) were students.
Time of presentation at burns and trauma centre
Ten (20.4%) patients presented within the first two hours of injury, 19 (38.8%) patients presented between 2-8 hours of injury, while 11 (22.5%) patients presented after 24 hours of injury (Fig. 1).
Fig. 1. A chart of frequency against interval between injury and presentation for definitive treatment.

Site of accidents
Thirty-two (65.3%) patients sustained the accident at home; seven (14.3%) patients were injured at the retail store where cooking gas was being sold, while 20.4% sustained the injury at their workplace/ office.
First aid measures
The first aid administered to these patients at the sites of injury included the application of motor oil and organic substances in 22 (44.9%) patients. These substances included eggs, raw pap, palm oil and vegetable oil. Twenty-two (44.9%) patients did not have any form of first aid at the site of the accident before presenting to the hospital. Five patients (10.2%) had copious water irrigation before presenting to health facilities.
Thirty-eight (77.6%) patients were commenced on intravenous fluid resuscitation before presenting to the Burns Unit. Thirty-six patients (73.5%) had intravenous antibiotics, and 79.6% had parenteral analgesic. The rest did not receive any form of treatment.
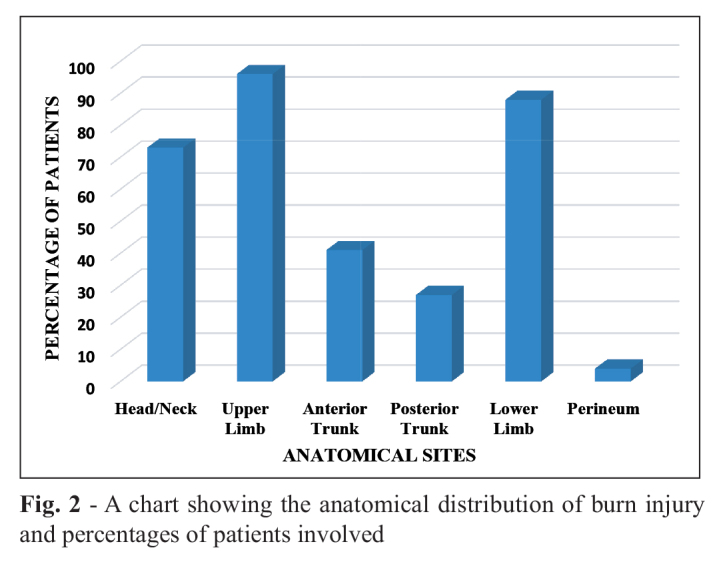
Anatomic distribution of burns
Thirty-six (73.5%) patients sustained burns to the head and neck and 45 (95.9%) patients to both upper extremities. The anterior trunk was more affected in 20 (40.8%) patients while 13 (26.5%) patients had burns on the posterior trunk. Lower limb was involved in 43 (87.8%) patients (Fig. 2).
Fig. 2. A chart showing the anatomical distribution of burn injury and percentages of patients involved.
Depth of injury
Burn injuries to the head and neck were mostly superficial partial thickness burn. Other parts of the body sustained mixed thickness injury. Twenty-six (53%) patients with lower extremity burns had deep partial thickness degree burns.
Total burn surface area (TBSA)
The total extent of burn injury ranged from 12-81% TBSA. The TBSA of injury involving the head and neck ranged between 1 to 9%, upper extremities between 2% to 18%, 5% to 18% for the anterior trunk and 1% to 12% for the posterior trunk. The lower limb had TBSA ranging from 4% to 34% (Fig. 3). Thirty-three (67% ) patients sustained burn injury with total surface area of 21% to 50%.
Fig. 3. Distribution pattern of total burn surface area among the patients.

Inhalational injury
Among the thirty-six (73.5%) patients who sustained burns to the head and neck region, 20 (56%) had clinical features suggestive of inhalational injury. All the patients had elective endotracheal intubation.
Blood transfusion services
Sixteen (32.7%) patients out of all those that sustained injury from gas explosion had blood transfusion. Six (12.2%) patients were transfused with 3 units of blood each and ten (20.4%) patients had 2 units of blood transfused.
All patients who received blood transfusion had TBSA greater than 30%. Four (8.2%) patients each had two units of blood transfused within the first three weeks of admission due to low haemoglobin. Among those who had surgery, six (12.2%) patients each had two units transfused, while another six (12.2%) patients had three units of blood transfused during the process of wound excision and skin grafting between the second and third week of admission.
Length of hospital stay (LOS)
The minimum duration of hospitalization was 3 days and the maximum was 86 days (Mean±SEM = 26.2±3.2). Three patients were discharged from the triage area after initial treatment for outpatient management because they had minor burns.
Surgical procedures
Thirty-two (65.3%) patients with deep partial thickness burns and full thickness burn were treated with burn wound excision and split thickness skin grafting. Eleven (22.4%) patients had peripheral venous cut down and eight (16.3%) patients had central venous catheter placement.
Complications and mortality
The overall mortality for all cases that were seen and treated during the study period was 78 (22.5%). Out of these, eight patients (10.3%) sustained injury from cooking gas explosion, representing a case fatality of 16.3%, while the case fatality from the other causes of burns combined was 23.5%. Three patients died within the first week of being burned, while the remaining five patients died in the second week of injury. Among the mortalities, 75% of the patients had inhalational injury and they all had a TBSA of 47% to 81%.
A logistic regression analysis was conducted to predict the factors responsible for mortality recorded among the patients. The variables used included depth of burns, TBSA, presence of inhalational injury, age of patients, gender, duration before presentation and level of education. The “non-model” without the predictors has 83.7% predictive accuracy, which later increases to 95.9% in the test model, which is a better predictive power compared to the “non-model”.
A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between mortality and survival (Chi square = 32.406, p = 0.000 with df = 6). Nagelkerke’s R2 = 0.821 (normal value = 0 – 1.0) indicated a strong relationship between prediction and grouping, i.e. 82.1% between predictors and prediction.
The Wald’s criterion demonstrated that inhalation injury and TBSA made a significant contribution to the prediction (p = 0.036 and 0.031 respectively).
The odds ratios were highest for these two parameters, 18 and 6.7 respectively, meaning mortality will most likely increase by 18 and 6.7 times in the presence of inhalational injury and larger TBSA respectively compared to other predictive factors (Table II).
Table II. Logistic regression: variables associated with mortalities.

Discussion
Flame burn is a major cause of hospital admission in Nigeria.8 Among the causes of flame burns, petroleum products are the most common cause of burns in Nigeria. The male and female ratio was nearly equal in this study. A review of the literature did not show many studies involving the incidence of explosion from butane cooking gas as causes of morbidity and mortality in patients with flame burns. Nnabuko et al. reported 7.5% burns from cooking gas explosions among the study population in the Eastern part of Nigeria.9 The 14.1% incidence in this study was higher than the value recorded in the eastern part of the country. This may be due to the higher population density and the cosmopolitan nature of Lagos compared to Enugu. It may also be due to an increasing awareness regarding the use of cooking gas instead of wood and charcoal among the population. The ability of gas to spread from source of leakage to the surroundings makes it likely to affect anybody within the vicinity of a gas explosion.
The number of males with burns is nearly double the number of females among all the patients admitted for burns during the study period. This predominance of males is most likely due to the fact that males tend to be more adventurous and are involved in more risky jobs and activities, hence predisposing them to accidents, including burns. This is in tandem with findings in other studies.10,11 There was however a nearly equal male to female ratio among patients who suffered burns from cooking gas explosion because females are usually more involved in household food preparation using cooking gas, hence this increased incidence compared to other causes of flame burns. This may also be the reason for the involvement of children in the accident, who sometimes follow their mother to the kitchen.
Richards et al.12 reported nine cases of camp gas explosion in 1999 at the Odstock Centre for Burns, Plastic and Maxillo-facial Surgery, Salisbury District General Hospital. The explosions were due to failure of the valve mechanism. This is in tandem with our study in which the explosions were mostly due to valve leakages and the use of low cost connecting tubes, which are most likely to have lower quality rubber tubing for the conduit systems. Inspection of the commonly used cylinders in the study environment during the study period showed there is no instruction provided on the cylinders to help educate the masses on the precautions to be taken to prevent such incidents, and most of the patients do not have any prior knowledge of safety precautions.
The extremities were most affected in this study; this may be due to the fact that the limbs are not usually covered by clothing, exposing these regions to the lethal effect of the explosion. The statistically significant factors determining mortality as seen in this study were presence of inhalational injury and total body surface area involved. This is similar to findings from previous studies. Smith et al.13 at the North Carolina University found that the mortalities recorded among 1447 burn patients that were studied over five and half years depends on the presence of inhalational injury, total burnt surface area and advancing age of patients. Other studies also arrived at similar conclusions.14-16
Though the patients were electively ventilated, the combination of inhalational injury and larger burn surface area in these patients still resulted in mortalities.
In this study the risk factors responsible for the explosion were the use of poor-quality valves and tubing systems, as most patients were victim of an explosion that resulted from a leakage from the tubes and valves. Another risk factor identified was level of education of the patients. Most of the patients had primary and/or secondary school education. Individuals in the higher economic class will mostly have domestic help doing the cooking. These domestic helpers are from the low socioeconomic class and often with a low level of educational achievement, consequently they may have poor knowledge of the safe use of cooking gas cylinders.
Domestic cooking gas consists of a storage cylinder, the tubing system and the burner. Since its first production in the 1820s, it has been improved to reduce accidental explosions.17 The ignition system has been modified over the years. Some use matchsticks for ignition. There is usually a massive explosion associated with this if the gas leaks prior to ignition. A pilot system has also been devised, in which there is a tiny streak of continuously burning flame called the pilot flame, which burns out once the knob is turned on. The disadvantage of this is that it continuously consumes the fuel even when not in use. It has the advantage of total independence of outside light source.
Nowadays, manufacturers install safety valves known as flame failure devices in the knobs of cooking gas cylinders. This automatically cuts off gas supply during accidental explosion. An auto recognition ignition system has also been devised. The burner automatically re-ignites if the flame is put out while the gas is still on. This helps to prevent continuous leakage of the gas into the environment. In Nigeria there is no law regulating the provision of cooking gas to consumers. Most of the vendors are located at the side of the road with the gas-filled cylinders displayed in the open by the roadside, exposing multiple individuals to the risk of explosion.
Conclusion
Cooking gas explosion is an increasingly common cause of domestic burns. It is more common among the low socio-economic class. Awareness of domestic cooking gas as cause of burns, either formal or informal, has been very low.
Production of high-quality tubing systems and valve mechanisms is essential to burn prevention. Explosion from cooking gas can occur in outdoor places, including at local retail points, hence the need for adequate and proper education for vendors.
Acknowledgments
Conflict of interest.The Authors have no conflict of interest to declare.
References
- 1.Forjuoh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Sanni OA. Adulterated kerosene burn disaster: the Nigerian experience. Ann Burns Fire Disasters. 2005;18:40–44. [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer H. Automotive Handbook. 4th ed. Robert Bosch GmbH: Stuttgart; 1996. pp. 238–239. [Google Scholar]
- 4.Fadeyibi IO, Ibrahim NA, Mustafa IA, Ugburo AO. Practice of first aid in burn related injuries in a developing country burns. Burns. 2015;41(6):1322–1332. doi: 10.1016/j.burns.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Fadeyibi IO, Mustapha IA, Ibrahim NA, Faduyile FI. Characteristics of paediatric burns seen at a tertiary centre in a low income country: a five year (2004-2008) study. Burns. 2011;37(3):528–534. doi: 10.1016/j.burns.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Hettiaratchy S, Papini R. ABC of burns: initial management of a major burn: II–assessment and resuscitation. BMJ. 2004;329:101–103. doi: 10.1136/bmj.329.7457.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pham TN, Gibran NS, Heimbach DM. Total Burn Care. 3rd ed. Saunders Elsevier; 2007. Evaluation of the burn wound: management decisions; pp. 81–85. [Google Scholar]
- 8.Olaitan PB, Olaitan JO. Burns and scalds - epidemiology and prevention. Nigerian J. Medicine. 2005;14:9–16. doi: 10.4314/njm.v14i1.37128. [DOI] [PubMed] [Google Scholar]
- 9.Nnabuko RE, Ogbonnaya IS, Otene CI, Ogbonna U. Burn injuries in Enugu, Nigeria - aetiology and prevention. A six-year retrospective review (January 2000 - December 2005). Ann Burns Fire Disasters. 2009;22(1):40–43. [PMC free article] [PubMed] [Google Scholar]
- 10.Blom L, Klingberg A, Laflamme L, Wallis L, Hasselberg M. Gender differences in burns: a study from emergency centres in the Western Cape, South Africa. Burns. 2016;42(7):1600–1608. doi: 10.1016/j.burns.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Fadeyibi IO, Jewo PI, Opoola P, Babalola OS, Ademiluyi SA. Burns and fire disaster from leaking petroleum pipes in Lagos, Nigeria: an 8-year experience. Burns. 2011;36(1):145–152. doi: 10.1016/j.burns.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Richards AM, Shakespeare PG. Portable camping stoves continue to cause burns. BMJ. 1999;318(7183):604. doi: 10.1136/bmj.318.7183.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith DL, Cairns DA, Ramadan F, Dalston JS. Effect of inhalation injury, burn size, and age on mortality: a study of 1447 consecutive burn patients. J Trauma. 1994;37:655–659. doi: 10.1097/00005373-199410000-00021. [DOI] [PubMed] [Google Scholar]
- 14.El-Helbawy RH, Ghareeb FM. Inhalation injury as a prognostic factor for mortality in burn patients. Ann Burns Fire Disasters. 2011;24(2):82–88. [PMC free article] [PubMed] [Google Scholar]
- 15.Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med. 2013;21:31. doi: 10.1186/1757-7241-21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Endorf FW, Gamelli RL. Inhalation injury, pulmonary perturbations, and fluid resuscitation. J Burn Care Res. 2007;28(1):80–83. doi: 10.1097/BCR.0B013E31802C889F. [DOI] [PubMed] [Google Scholar]
- 17.Snodgrass ME. Encyclopedia of Kitchen History. XX. Routledge; 2004. p. 428. [Google Scholar]


