Abstract
Background Foveal attachment of the triangular fibrocartilaginous complex (TFCC) is essential for distal radioulnar joint stability. Controversy still exists as to which is the best treatment in case of foveal lesions. Actual arthroscopic techniques either require mini open steps or are complex and expensive. We present a simple all inside knotless repair, providing a strong bony fixation in the fovea.
Materials and Methods Through 3–4 and 6R portals, the ulnar fovea is debrided and a wire is passed percutaneously through the TFCC to place a mattress suture at its free end. It is then reattached to the fovea with an impacted anchor.
Retrospective Study Between 2013 and 2016, a cohort of 5 patients presenting with isolated Palmer 1B, EWAS 2 lesions of the TFCC were operated on with this technique. Clinical evaluation was based on a compared measurement of the grip strength, pain on a visual analogic scale (VAS), different ranges of motion, and distal radioulnar joint (DRUJ) stability. We also used functional scores: Mayo modified wrist score (MMWS), Quick disability arm, shoulder and hand (DASH), and patient-related wrist evaluation (PRWE). The average follow-up was 29.4 months (range 9–42 months).
Results On postoperative evaluation, pain was reduced by 5 points (range 1–9) and grip strength averaged 94% of the unaffected side. Range of motion averaged 92% on the unaffected side. DRUJ instability was slight in 4 patients and mild in 1 patient. MMWS was excellent for 1, good for 1, and satisfactory for 3 patients. Quick Dash averaged 17.68 (range 0–38.6) compared with preoperative average of 59.48 (range 45–77) with an amelioration of 43 (range 34–57).
PRWE averaged 20 (range 1–41.5) compared with preoperative average of 60.3 (range 33.5–76.5) with an amelioration of 41 (range 32–58). We reported no complications and particularly no lesions of the dorsal sensory branch of the ulnar nerve.
Conclusions We present a simple arthroscopic technique using a single suture anchor placed in the ulnar fovea. Repairs performed with this technique are simple and the results achieved seem to be similar to those obtained with conventional open or arthroscopic techniques, although further investigation with an increased number of patients and follow-up are required. It however became our first choice of treatment in European Wrist Arthroscopy Society (EWAS) 2 lesions of the TFCC.
Keywords: wrist arthroscopy, TFCC, foveal
Anatomical understanding of the triangular fibrocartilaginous complex (TFCC) was improved by the work of Nakamura et al. 1 The importance of the proximal component in distal radioulnar joint (DRUJ) stability is now broadly accepted. 2 3 4 5 Its lesion leads to instability of the DRUJ, resulting in ulnar-sided pain, reduced grip strength, and limitation of the pronosupination. 3 5
Traditional arthroscopic suturing have shown their shortcomings in providing DRUJ stability, failing to repair the foveal attachments of the TFCC. 6 7 8 Open repairs have shown good clinical results, although by the mean of extensive and difficult exposure of the DRUJ. 6 9
To solve this problem, several arthroscopic techniques have been described. 3 5 10 11 Most of these techniques either combine open and arthroscopic steps 3 or are complex and require expensive supplies. 11 We present a simplified all inside knotless arthroscopic foveal reattachment technique.
Materials and Methods
Patients
A review was conducted on a retrospective cohort who underwent arthroscopic TFCC foveal repair from January 2013 to December 2016. The surgical listing and medical linkage systems were queried to obtain all patients who underwent arthroscopic foveal TFCC repair surgery performed by the senior surgeon (DF). Operative reports were reviewed to determine the type of procedure, and the type of TFCC tear repaired was classified according to Palmer 12 and Atzei et al. 3
Regarding the patients, date of birth, age at surgery, arm dominance, side of injury, and comorbidities were determined. Work- and sport-related activities were also noted. Constitutional hyperlaxity was researched for through Beighton et al 13 criterions.
Inclusion criteria were: surgical treatment of isolated Palmer 1B lesion of the TFCC with both proximal and distal component of the foveal insertion lesion (EWAS 2) diagnosed by an arthro-computed tomography (CT) and/or magnetic resonance imaging (MRI) and confirmed during surgery with a minimal follow-up of 9 months.
Exclusion criteria were degenerative lesions of the TFCC (Palmer type 2), absence of foveal lesion, irreparable foveal lesions of the TFCC (EWAS 4), and arthritis of the radiocarpal or DRU joints. Isolated proximal component lesions (EWAS 3), requiring a different type of repair, were also excluded.
A total of five patients (three men and two women) were reviewed. The average age at surgery was 30.8 (range 25–41 years). Four patients were right-handed and 1 patient was left-handed. Dominant side was affected in three of the five patients.
The average follow-up was 29.4 months (range 9–42 months). All of the patients had a significant history of trauma before the onset of pain. The delay from injury to surgery averaged 7.4 months (range 1–14 months). All patients presented with ulnar wrist pain. Three patients presented with preoperative significative clinical and symptomatic instability of the DRUJ.
Operative Technique
An axillary block is administered and the patient is positioned supine with the affected arm on a hand table with a tourniquet inflated to 250 mm Hg. The wrist is suspended with the Whipple Wrist Traction Tower (Linvatec Company) with a 10-pound (4.5 kg) traction. The 3–4 portal is located with a 21-gauge needle, incised with a no. 15 blade, and bluntly dissected with a mosquito forceps. A 2.7 mm 30° arthroscope is inserted in this portal. The 6R portal is identified at the distal aspect of the TFCC with a needle and used as an instrumental portal along with a 6U outflow portal. It is very important to anticipate the course that will be required to access the fovea for the implantation of the anchor. The portal must therefore be more distal and ulnar than usual ( Fig. 1C ).
Fig. 1.

Foveal preparation: ulnar styloid process debridement with a radiofrequency device ( A ) and motorized burr, ( B ): arthroscopic view, and ( C ): operative view showing the direction required for the burr.
This technique does not require accessory portals. Midcarpal ulnar and radial (MCU and MCR) are only performed to assess scapholunate and lunotriquetral stability according to the associated lesions observed in the radiocarpal joint and preoperative assessment.
The TFCC is evaluated by three maneuvers: trampoline test, 7 hook test, 3 and Ghost sign 14 to confirm the proximal detachment of the TFCC. The repair is performed with the camera in the 3–4 portal and instruments in the 6R portal. Soft-tissue interpositions are debrided through the lesion of the TFCC using a radiofrequency device and an oscillating device (full radius shaver) to access the radial side of the ulnar styloid process ( Fig. 1A ). The ulnar foveal footprint, located in the middle of the radial side of the basis of the ulnar styloid, is abraded using a motorized burr ( Fig. 1B and C ).
The hole for the introduction of an impacted Anchor (Mini Pushlock, Arthrex, Naples, FL, USA) is created on the foveal footprint using a dedicated 2 mm manual drill ( Fig. 2A–C ). 20 to 30° flexion of the wrist allows for a better course of the instrument to reach the fovea ( Fig. 2A ). The impaction device must be in line with the ulna and care must be taken not to slip anteriorly.
Fig. 2.

Foveal hole drilling with the dedicated manual drill. ( A ) Operative view. ( B ) Arthroscopic view through 3–4 optical portal. ( C ) Artist drawing (Image courtesy: Massimiliano Crespi).
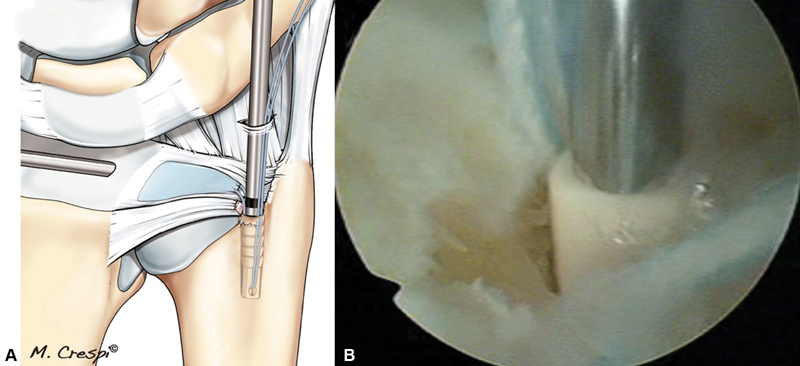
A 2/0 wire (Fiberwire, Arthrex, Naples, FL, USA) is mounted on an 18 Gauge needle. It is inserted percutaneously proximal to the 6R portal and passed through both the proximal and the distal layers of the TFCC, 2 to 3 mm from the free end, in a proximal-to-distal direction. The needle is turned to twist the wire, preventing its accidental removal while the needle is pulled out just proximally under the TFCC ( Fig. 3 ).
Fig. 3.

The wire mounted on an 18 Gauge needle is passed through the TFCC. ( A ) Artist drawing (Image courtesy: Massimiliano Crespi). ( B ) Operative view. Abbreviation: TFCC, triangular fibrocartilaginous complex.
The wire is retrieved and pulled out through the 6R portal. This operation is performed a second time, 4 to 5 mm dorsally. A horizontal mattress suture is then placed on the TFCC.
The two threads of the wire are passed through the aperture of the anchor ( Fig. 4 ).
Fig. 4.

A horizontal mattress suture is passed through the TFCC. The two threads are mounted onto the Pushlock device. ( A ) Artist drawing (Image courtesy: Massimiliano Crespi). ( B ) Operative view. Abbreviation: TFCC, triangular fibrocartilaginous complex.
The anchor is introduced through the 6R portal and advanced to the previously prepared hole on the foveal footprint. Tension is set on the suture by pulling on the two wire strands while impacting the anchor in the predrilled hole, thereby locking the suture and the articular disk in the foveal area ( Fig. 5 ). The driver of the anchor is removed and the suture tails are cut flush with the disk ( Fig. 6A ). Efficiency of the repair is tested using the trampoline ( Fig. 6B ) and hook tests, and by testing DRUJ stability and pronosupination range of motion.
Fig. 5.
Insertion of the Mini Pushlock. ( A ) Artist drawing (Image courtesy: Massimiliano Crespi). ( B ) Arthroscopic view through 3–4 optical portal.
Fig. 6.

Final result. ( A ) Artist drawing (Image courtesy: Massimiliano Crespi). ( B ) Arthroscopic view through 3–4 optical portal. Trampoline effect is restored. ( C ) Postoperative MRI showing the healing of the foveal insertion of the TFCC. Abbreviation: MRI, magnetic resonance imaging; TFCC, triangular fibrocartilaginous complex.
Rehabilitation Protocol
The wrist is immobilized in a brachioantebrachial splint in a neutral position for 3 weeks, relayed by a removable wrist splint for 3 more weeks. Digital range-of-motion exercises are initiated immediately. Range-of-motion and strengthening exercises of the forearm and wrist are initiated at 6 weeks. Manual activities and sports can be resumed at 2 months.
Postoperative Evaluation
Patients were reviewed by the junior author (GK). Exertional wrist pain was assessed using the visual analog scale (VAS). The range of motion for both upper extremities was measured with standard goniometers. Wrist extension, flexion, radial and ulnar deviation, and forearm rotation were measured. Grip strength was evaluated with the Jamar dynamometer (Sammons–Weston, Bolingbrook, IL). The results were reported as percentages of the normal side. Each measurement was performed 3 times and the average value was noted. DRUJ stability was evaluated by a passive anteroposterior translation in neutral position, full supination, and full pronation. It was graded as “slight” when inferior to 5 mm, “mild” when between 5 and 10 mm, and severe when greater than 10 mm. 8 Functional outcome was evaluated with the Modified Mayo wrist score, 15 Quick disability arm, shoulder and hand (DASH), 16 and patient-related wrist evaluation (PRWE). 17 Satisfaction was evaluated both by a visual scale and by subjective evaluation in 4 grades: very satisfied/satisfied/mildly satisfied/unsatisfied. We also evaluated the subjective wrist value derived from the subjective shoulder value described by Gilbart and Gerber. 18 It is defined as a patient's subjective wrist assessment expressed as a percentage of an entirely normal wrist, which would score 100%.
Delay to return to work and sports were evaluated, including evaluation of the level (same/lesser/none).
Complications
Specific complications such as dorsal sensory branches of the ulnar nerve (DSBUN) lesions were researched for.
Results
At follow-up, pain VAS evaluation averaged 0.4 (range 0–1) compared with preoperative pain which averaged 6.75 (range 2–9). Preoperative to postoperative diminution of pain was 5 (range 1–9). Regarding the range of motion, wrist extension/flexion averaged 133°, range 125 to 145, which was 92% of the unaffected side. Pronation/supination averaged 170° and ranged from 160 to 180°, which was 98% of the unaffected side. Grip strength averaged 36 kg and ranged from 20 to 59 kg, which was 94% of the unaffected side.
DRUJ stability examination showed slight instability in four patients and mild in one patient. None of the patients presented with severe instability. One patient had hyperlaxity according to Beighton et al. 13 According to the Mayo wrist score, one patient had an excellent result, one patient had a good result, and three had satisfactory results. Quick Dash averaged 17.68 (range 0–38.6) compared with preoperative average of 59.48 (range 45–77) with an amelioration of 43 (range 34–57). PRWE averaged 20 (range 1–41.5) compared with preoperative average of 60.3 (range 33.5–76.5) with an amelioration of 41 (range 32–58). Subjective wrist value averaged 78 (range 60–95) compared with preoperative average of 35 (range 20–60) with an amelioration of 47.5 (range 30–65). Patient satisfaction averaged 8.2 (range 5–10). Two patients were very satisfied, two satisfied, one mildly satisfied, and no patient was unsatisfied. Return to work was possible in all patients with the same position, with a mean delay of 54 days (range 26–92). Sports and leisure activities were resumed at an average of 20 weeks (range 9–31) at the same level for three patients and at a lesser level for two patients. None of the patients could not resume their usual activities.
No complications were reported, including no lesion of the DSBUN.
Discussion
Both painless rotational stability and full range of motion of the DRUJ are critical in functional capacity of the upper limb. 6 The role of the foveal insertion of the TFCC in DRUJ stability was shown by several studies 2 6 19 20 since its description by Nakamura et al. 1 Haugstvedt et al 21 have shown in a biomechanical study that the foveal insertion of the TFCC has a greater importance in DRUJ stability than any other insertion sites. Classic arthroscopic techniques failed to diagnose or to reconstruct this structure, leading to unsatisfactory results 2 7 9 Boquet et al 2 considered that some of their unsatisfactory results may be caused by undiagnosed EWAS 2 (repairable complete foveal tear) or EWAS 3 (repairable proximal tear) which would have needed a foveal repair. Estrella et al, 22 Chou et al, 10 and Anderson et al 23 have showed that poor results in peripheral TFCC repair were explained by a persistent DRUJ instability, which was caused by a lesion of the proximal component of the TFCC. Atzei et al 3 have found proximal TFCC lesions (EWAS stage 2 or 3) in up to 70% of the reparable lesions of the TFCC. Anderson et al 23 found that more than 40% of their TFCC repair needed immediate or eventual DRUJ reconstruction.
To solve this difficult problem, techniques of foveal reattachment were described with promising results though through extensile approaches. 6 9 24 Chou et al 10 described a mini-invasive technique using a foveal anchor which provided excellent (three cases) or good (five cases) results according to the Mayo wrist score.
Although open or mini-open repairs have shown good clinical results, arthroscopic treatment improves surgical accuracy through optical magnification and respecting the extensor retinaculum, 3 particularly the extensor carpi ulnaris tendon sheath. 25 Arthroscopy also reduces some complications such as DSBUN lesions. Anderson et al 23 reported an increased rate of postoperative superficial ulnar nerve pain in the open group (14 out of 39 patients) compared with the arthroscopic group (8 out of 36 patients) with no statistical difference in clinical outcome between the two groups. Mathoulin and Atzei 26 reported stiffness and pronosupination limitation in open repairs to justify their use of arthroscopy. These elements may contribute to the better outcomes provided by arthroscopic treatment of TFCC lesions. 23
In 18 patients with a mean follow-up of 18 months, Atzei et al 3 showed a statistically significative improvement in grip strength (from 73 to 90% of the contralateral side) and pain changes (VAS decreased from 8.3 to 1.2) after arthroscopically assisted foveal repair. The repair was performed using a direct foveal (DF) portal and a 2 to 2.5 cm skin incision between the 6U and the DF portals. Through this incision, they inserted an anchor in the fovea. whose wires were passed through the TFCC under arthroscopic control. and sutures were tied to assure TFCC compression against the distal ulna. Modified Mayo wrist score was good or excellent in 94% of the patients and 83% resumed their previous work and recreational activities. Fourteen of the 18 patients had EWAS 2 lesions. They reported 4 transient neurapraxia of the DSBUN which recovered spontaneously in 3 to 4 months. Mathoulin and Atzei 26 in their retrospective study of 72 TFCC lesions found 29 foveal lesions, 18 EWAS 2, and 11 EWAS 3. EWAS 2 lesions were treated by a technique similar to the one described by Atzei et al 3 using an incision between the 6U and the DF portal. With a mean 12-months (range 6–26 months) follow-up, they found a good recovery in both mobility and strength when compared with the opposite unarmed side. Regarding EWAS 2 lesions, they showed recovery of the range of motion in flexion extension and grip strength recovery identical to the unaffected side. However, in two cases, limitation of radial inclination and pronosupination occurred. Arthroscopic control was performed in four patients with a healthy aspect and negative testing of the TFCC.
Nakamura et al 4 described a transulnar procedure to perform the reattachment of the TFCC on the fovea. This technique required a targeting device to drill two parallel holes between the ulnar cortex and the ulnar half of the TFCC. Wires were introduced in the tunnels through a shuttle relay technique and were tied on the ulnar cortex to perform the TFCC reattachment. They treated 24 foveal lesions with a 3.5-year follow-up (range 12–60 months). Fifteen of the 24 patients described a complete pain relief. Severe pain remained in two cases and pain recurred at 8 to 12 months after the surgery in four cases. DRUJ instability disappeared in 17 cases, and seven others presented with moderate to severe instability. The final clinical results obtained were 13 excellent, 3 good, 4 fair, and 4 poor. Delay between trauma and treatment was identified as related to a poor outcome.
Iwasaki and Minami 27 also described a transosseous technique with only one ulnar tunnel, with fixation of the TFCC being secured by a suture on the ulnar periosteum around the hole. They did not present clinical results but reported MRI images of attachment of the TFCC to the distal entry site of the tunnel at 12 weeks postoperatively.
In the technique described by Park et al, 5 a 2 cm long longitudinal skin incision was required on the lateral aspect of the ulna and a specially designed targeting device was used to create the transosseous tunnel with a 4 mm cannulated drill. The suture was then secured by two anchors proximally to the bone tunnel. This technique was performed in 16 patients with a 31.1-month follow-up (range 2–42 months). The range of forearm pronosupination and grip strength improved significantly. Pain decreased from 3.7 to 0.8 ( p = 0.001). The mean modified Mayo wrist score significantly improved after surgery from 61.8 to 83.4 ( p = 0.001). The quick DASH score improved from 35.0 to 9.9 ( p = 0.001). No surgery-related complications, such as ulnar styloid fracture, infection, and nerve injury, occurred.
Geissler 11 described an all inside knotless technique using Mini-Pushlock which decreases potential soft-tissue irritation and intra-articular maneuvers and provides a very strong suture by repairing the TFCC directly back to the bone. This technique requires 14 steps, making it less reproductible and difficult to teach. It also requires a distal accessory 6R portal.
The technique described in this article repairs both superficial and deep layers. 11 Using a knotless procedure, as did Geissler 11 it is however simpler. It requires fewer operative steps and few supplies: one 18 Gauge needle, one impacted anchor, and its dedicated drill. Only two portals are needed, compared with other techniques requiring DRUJ portals, either volar ulnar or direct foveal, 3 accessory portals, 11 or even mini-open steps. 3 10 26 Indeed limited approaches were recommended 3 8 to prevent damages of the DSBUN. These lesions were related either to the direct foveal approach or the knots performed. In this technique, neither of these elements were required which may explain the absence of DSBUN symptoms.
Although the number of patients was not sufficient for a statistical analysis and the follow-up was relatively short, this technique seems promising and would require further study.
Conclusion
We present a simple arthroscopic technique using a single-suture anchor placed in the ulnar fovea. Repairs performed in this fashion are simple and results achieved seems to be similar to those obtained with conventional open or arthroscopically assisted techniques, although further investigation with an increased number of patients and follow-up are required. It however became our first choice of treatment in EWAS 2 lesions of the TFCC.
Footnotes
Conflict of Interest D. F. reports grants from ARTHREX Company during the course of the study and grants from KERIMEDICAL outside the submitted work. G. C. reports grants from Arthrex during the course of the study and grants from Kerimedical outside the submitted work. G. K. declares that he received fellowship support from Arthrex for another research work. P. U. declares that he has no competing interest.
References
- 1.Nakamura T, Yabe Y, Horiuchi Y. Functional anatomy of the triangular fibrocartilage complex. J Hand Surg [Br] 1996;21(05):581–586. doi: 10.1016/s0266-7681(96)80135-5. [DOI] [PubMed] [Google Scholar]
- 2.Boquet J, Lefebvre B, Van Innis F. Évaluation clinique rétrospective des traitements arthroscopiques des lésions du complexe triangulaire du poignet. Chir Main. 2012;31(02):91–96. doi: 10.1016/j.main.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Atzei A, Rizzo A, Luchetti R, Fairplay T. Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg. 2008;12(04):226–235. doi: 10.1097/BTH.0b013e3181901b1. [DOI] [PubMed] [Google Scholar]
- 4.Nakamura T, Sato K, Okazaki M, Toyama Y, Ikegami H. Repair of foveal detachment of the triangular fibrocartilage complex: open and arthroscopic transosseous techniques. Hand Clin. 2011;27(03):281–290. doi: 10.1016/j.hcl.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Park J H, Kim D, Park J W. Arthroscopic one-tunnel transosseous foveal repair for triangular fibrocartilage complex (TFCC) peripheral tear. Arch Orthop Trauma Surg. 2018;138(01):131–138. doi: 10.1007/s00402-017-2835-3. [DOI] [PubMed] [Google Scholar]
- 6.Kleinman W B. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007;32(07):1086–1106. doi: 10.1016/j.jhsa.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 7.Hermansdorfer J D, Kleinman W B. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16(02):340–346. doi: 10.1016/s0363-5023(10)80123-6. [DOI] [PubMed] [Google Scholar]
- 8.Atzei A. New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol. 2009;34(05):582–591. doi: 10.1177/1753193409100120. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Elias M, Smith D E, Llusá M. Surgical approach to the triangular fibrocartilage complex. Tech Hand Up Extrem Surg. 2003;7(04):134–140. doi: 10.1097/00130911-200312000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Chou K H, Sarris I K, Sotereanos D G. Suture anchor repair of ulnar-sided triangular fibrocartilage complex tears. J Hand Surg [Br] 2003;28(06):546–550. doi: 10.1016/s0266-7681(03)00173-6. [DOI] [PubMed] [Google Scholar]
- 11.Geissler W B. Arthroscopic knotless peripheral ulnar-sided TFCC repair. J Wrist Surg. 2015;4(02):143–147. doi: 10.1055/s-0035-1549278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(04):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 13.Beighton P, Solomon L, Soskolne C L. Articular mobility in an African population. Ann Rheum Dis. 1973;32(05):413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fontès D.Therapeutic interest of wrist arthroscopy - from a series of 280 casesPresented at: 6th Congress of IFSSH;1995723–728.
- 15.Cooney W P, Bussey R, Dobyns J H, Linscheid R L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 16.Dubert T, Voche P, Dumontier C, Dinh A. Le questionnaire DASH. Adaptation française d'un outil d'évaluation international. Chir Main. 2001;20(04):294–302. doi: 10.1016/s1297-3203(01)00049-x. [DOI] [PubMed] [Google Scholar]
- 17.MacDermid J C, Turgeon T, Richards R S, Beadle M, Roth J H. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(08):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Gilbart M K, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(06):717–721. doi: 10.1016/j.jse.2007.02.123. [DOI] [PubMed] [Google Scholar]
- 19.Gaumet G, Fontes D, Wavreille G, Limousin M. La pathologie ligamentaire du poignet. À propos de 32 lésions du complexe fibro-cartilagineux triangulaire du carpe (TFCC). Intérêt pronostique des lésions luno-triquetrales associées. Chir Main. 2012;31(06):298–305. doi: 10.1016/j.main.2012.10.160. [DOI] [PubMed] [Google Scholar]
- 20.Stuart P R, Berger R A, Linscheid R L, An K-N. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am. 2000;25(04):689–699. doi: 10.1053/jhsu.2000.9418. [DOI] [PubMed] [Google Scholar]
- 21.Haugstvedt J-R, Berger R A, Nakamura T, Neale P, Berglund L, An K-N. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am. 2006;31(03):445–451. doi: 10.1016/j.jhsa.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Estrella E P, Hung L-K, Ho P-C, Tse W L.Arthroscopic repair of triangular fibrocartilage complex tears Arthroscopy 20072307729–737., 737.e1 [DOI] [PubMed] [Google Scholar]
- 23.Anderson M L, Larson A N, Moran S L, Cooney W P, Amrami K K, Berger R A. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33(05):675–682. doi: 10.1016/j.jhsa.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 24.Bain G I, Pourgiezis N, Roth J H. Surgical approaches to the distal radioulnar joint. Tech Hand Up Extrem Surg. 2007;11(01):51–56. doi: 10.1097/bth.0b013e318033bdae. [DOI] [PubMed] [Google Scholar]
- 25.Fontès D. Traitement arthroscopique des lésions traumatiques récentes et chroniques du complexe triangulaire du poignet. Chir Main. 2006;25 01:S178–S186. [PubMed] [Google Scholar]
- 26.Mathoulin C, Atzei A. Réparation du ligament triangulaire (TFCC) : rapport d'une série de 72 cas suivant une nouvelle classification. E-Mem Acad Natl Chir. 2010;9(01):21–27. [Google Scholar]
- 27.Iwasaki N, Minami A. Arthroscopically assisted reattachment of avulsed triangular fibrocartilage complex to the fovea of the ulnar head. J Hand Surg Am. 2009;34(07):1323–1326. doi: 10.1016/j.jhsa.2009.02.026. [DOI] [PubMed] [Google Scholar]


