Abstract
Background
Pseudorabies, also known as Aujeszky's disease, is caused by the pseudorabies virus (PRV) and has been recognized as a critical disease affecting the pig industry and a wide range of animals around the world, resulting in great economic losses each year. Shandong province, one of the most vital food animal-breeding regions in China, has a very dense pig population, within which pseudorabies infections were detected in recent years. The data, however, on PRV epidemiology and coinfection rates of PRV with other major swine diseases is sparse.
Objectives
This study aimed to investigate the PRV epidemiology in Shandong and analyze the current control measures.
Methods
In this study, a total number of 16,457 serum samples and 1,638 tissue samples, which were collected from 362 intensive pig farms (≥ 300 sows/farm) covered all cities in Shandong, were tested by performing enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR).
Results
Overall, 52.7% and 91.5% of the serum samples were positive for PRV-gE and -gB, respectively, based on ELISA results. In addition, 15.7% of the tissue samples were PCR positive for PRV. The coinfection rates of PRV with porcine circovirus type 2 (PCV2), porcine reproductive and respiratory syndrome virus, and classical swine fever virus were measured; coinfection with PCV2 was 35.0%, higher than those of the other two viruses. Macroscopic and microscopic lesions were observed in various tissues during histopathological examination.
Conclusions
The results demonstrate the PRV prevalence and its coinfection rates in Shandong province and indicate that pseudorabies is endemic in pig farms in this region. This study provides epidemiological data that can be useful in the prevention and control of pseudorabies in Shandong, China.
Keywords: Pseudorabies virus, veterinary epidemiology, coinfection, porcine circovirus
INTRODUCTION
Pseudorabies, also known as Aujeszky's disease, is caused by the pseudorabies virus (PRV). It is a member of the genus Varicellovirus of the subfamily Alphaherpesviridae within the family Herpesviridae. Although numerous species of mammals can be infected by PRV [1,2], pigs are the primary host, as well, they act as the only reservoir and latent carrier of PRV [3]. PRV-infected pigs commonly show a range of signs including respiratory disorders, encephalomyelitis, reproductive failure in sows, and growth retardation in piglets [1,4]. It was reported that PRV has been eradicated from domestic pigs in many western countries, which is a benefit of the control efforts and effective eradication programs of those countries. A gE-deleted vaccine has been of paramount importance in tackling PRV infection in these PRV-free countries, particularly when differentiating infected animals from vaccinated counterparts [5,6].
The first epizootic PRV infection in pigs was identified in the 1960s in China. From the 1990s to late 2011, Hungary-origin gpI-negative vaccine strain Bartha-K61 was adopted in most pig farms in China, notably contributing to the control of pseudorabies and lower level of morbidity and mortality in newborn piglets [7]. Although the gE-deleted vaccine is available for control and eradication for pseudorabies, a variant PRV has re-emerged and spread to most of the regions in China since 2011 [7,8]. Data on the epidemiology of PRV and its coinfection rate with other major swine diseases may be of great importance for the prevention and control of PRV, particularly in regions with dense pig populations.
Shandong is a coastal province located in the east of China that has massive pig farms and, overall, a large pig population. The total population of pigs and sows in Shandong in 2017 was estimated to be approximately 28 million and 3 million, respectively. However, there have been no representative investigations of PRV prevalence, or of its coinfection with other major swine viral diseases, conducted in large pig farms in Shandong. The goal of this study was to describe PRV prevalence and its coinfection rates by examining 16,457 serum samples and 1,638 tissue samples collected from 362 pig farms in Shandong. In the study, we assessed macroscopic lesions, undertook histopathological examination, determined gB and gE antibody levels, and calculated coinfection rates for PRV with other major swine viral diseases. Our results suggest that PRV is highly prevalent in Shandong province and may be considered a major threat to the pig breeding industry in China.
MATERIALS AND METHODS
Experimental protocols
Serum samples were collected from seventeen cities, including all of the major cities in Shandong province. The samples were categorized as follows: sow, boar, fatting pig, replacement pig, and piglets. Based on the sample sizes of the seropositive pigs in each investigated city, tissue samples were randomly selected from the seropositive pigs to determine the PRV-positive rate and the coinfection rates of PRV with porcine reproductive and respiratory syndrome virus (PRRSV), classical swine fever virus (CSFV), and porcine circovirus type 2 (PCV2) by performing reverse transcription polymerase chain reaction (RT-PCR).
Serum sample collection and enzyme-linked immunosorbent assay (ELISA)
A total of 16,457 serum samples were collected from 17 geographically widespread cities in Shandong province, thereby covering the entire province. PRV-gE antibody levels were determined for all serum samples, and 4,034 samples were randomly selected to detect pseudorabies virus glycoprotein B (PRV-gB). Commercial ELISA kits (IDEXX Laboratories, USA) were used in accordance with the manufacturer’s instructions to differentiate the vaccine strain from the field strains.
Primer design and virus detection
A total of 1,638 lymph gland and brain samples from different pig farms were examined. Viral DNA or RNA was extracted from the samples by using commercial kits (Takara Biomedical Technology, China) in accordance with the manufacturer's instructions. Primers were designed for viral genome detection based on GenBank information (forward primer, 5′-TCCACTCGCAGCTCTTCT-3′; reverse primer, 5′-GCACGTCATCACGAAGGA-3′). Extracted DNA was used as a template to detect PRV and PCV2 by performing polymerase chain reaction (PCR). Extracted RNA was used to detect CSFV and PRRSV by using RT-PCR.
The following PCR cycle profile was applied: one cycle at 94°C for 5 min, 30 cycles at 94°C for 30 sec, 58 °C for 30 sec, and 72 °C for 50 sec, and a final extension at 72°C for 10 min. Cycling conditions for the one-step RT-PCR were as follows: 45°C for 25 min, 94°C for 5 min followed by 30 cycles of 94°C for 30 sec, 56°C for 30 sec, and 72°C for 50 sec, and a final extension at 72°C for 10 min. PCR products were subjected to electrophoresis on 1% agarose gels stained with ethidium bromide and were visualized with an ultraviolet light transilluminator.
Necropsy and histopathological examination
Clinical cases with typical pseudorabies symptoms were observed and dissected. Tissues were fixed in 10% phosphate-buffered formalin for 24 h and further processed for histological examination by following standard procedures. The tissue sections (4 µm) were investigated microscopically to detect histopathological lesions.
Statistical analysis
Positive rates of pseudorabies virus glycoprotein E (PRV-gE) and PRV were compared by sampling year and for different animal groups. If the 95% confidence interval (CI) of a variable was more or less than 1, it was considered an influencing factor. Differences were considered significant when the χ2 test p value was less 0.05.
Ethics approval and consent to participate
The protocol of this study was approved by the Ethic Committee on the animals of Shandong Agricultural University (SDAUA-2015-012).
RESULTS
Seroprevalence rate (SPR) of PRV-gB
Consistent with the results in previous studies in other regions of China [9,10,11,12], the immunization coverage for PRV was recorded as almost 100% in the investigated pig farms in Shandong province, which is reflected by the high seroprevalence rates (SPR) for PRV-gB presented in Table 1. Moreover, the high immunization coverage was reflected by the low S/N ratios, ranging from 0.17 to 0.32, observed in all of the investigated herds (data not shown). It is widely asserted that the PRV immunization density and antibody levels were considerably high in the region sampled, which is expected to provide effective prevention and control of PRV infections.
Table 1. SPR of PRV-gB in pigs in Shandong province from 2015 to 2018.
| Years | Sample numbers | PRV-gB-positive numbers | SPR |
|---|---|---|---|
| 2015 | 958 | 837 | 87.4% |
| 2016 | 1,564 | 1,453 | 92.9% |
| 2017 | 1,263 | 1,184 | 93.7% |
| 2018 | 249 | 218 | 87.6% |
| Total | 4,034 | 3,692 | 91.5% |
SPR = sero-prevalence rate, PRV-gB = pseudorabies virus glycoprotein B.
Seroprevalence rate of PRV-gE
However, as shown in Table 2, the average SPR of PRV-gE of pigs was 52.7% in the period between 2015 and 2018, ranging from 44.1% to 62.5% in different production phases but with the highest rate detected in piglets. The SPR in the piglet group was significantly higher than that in any other group (p < 0.05). The SPR of PRV-gE in the sow, fatting pigs, and young piglets groups showed similar trends with higher rates in 2016 and 2018 than in 2015 and 2017. However, the situation in boars differed, with the SPR PRV-gE peak (69.3%) occurring in 2017. The SPR of PRV-gE in replacement pigs fluctuated slightly, averaging 44.1% over the study period. Although the SPR for PRV-gE in replacement pigs was the highest in 2016, the difference was not significant.
Table 2. Seroprevalence rate of PRV-gE among different pig herd types in Shandong province from 2015 to 2018.
| Years | Herds, No. (%) | PRV-gE | OR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| Piglets | Sows | Boars | Fatting pigs | Replacement pigs | ||||
| 2015 | 95/197 (48.2) | 505/1,109 (45.5) | 117/332 (35.2) | 47/123 (38.2) | 446/995 (44.8) | 1,210/2,756 (43.9) | 1 (ref.) | |
| 2016 | 929/1,387 (67.0) | 1,378/2,424 (56.8) | 212/442 (48.0) | 159/288 (55.2) | 231/492 (47.0) | 2,909/5,033 (57.8) | 1.750 | 1.592–1.922 |
| 2017 | 890/1,503 (59.2) | 1,194/2,534 (47.1) | 70/101 (69.3) | 92/225 (40.9) | 230/552 (41.7) | 2,476/4,915 (50.4) | 1.859 | 1.686–2.048 |
| 2018 | 767/1,202 (63.8) | 927/1,697 (54.6) | 69/171 (40.4) | 98/187 (52.4) | 211/496 (42.5) | 2,072/3,753 (55.2) | 1.575 | 1.426–1.739 |
| Total | 2,681/4,289 (62.5) | 4,004/7,764 (51.6) | 468/1,046 (44.7) | 396/823 (48.1) | 1,118/2,535 (44.1) | 8,667/16,457 (52.7) | ||
| OR | 1 (ref.) | 0.639 | 0.486 | 0.556 | 0.473 | |||
| 95% CI | 0.592–0.689 | 0.424–0.557 | 0.479–0.646 | 0.428–0.523 | ||||
PRV-gE = pseudorabies virus glycoprotein E; OR = odds ratio; CI = confidence interval.
PCR positive rate of PRV
Among the 1,638 tissue samples, 257 samples were PRV-positive. The PRV-positive rates are summarized by sample year in Table 3. The overall PRV-positive rate over the 2015-2018 study period averaged 15.7%, with the highest rate of 27.8% observed in 2016 (110/395); the PRV-positive rate averaged approximately 11.8% for the other three years (2015, 2017, and 2018). The PRV-positive rate for 2016 was significantly higher than those for the other years (p < 0.05).
Table 3. PRV-positive rate in pigs sampled in Shandong province from 2015 to 2018.
| Year | Sample numbers | Positive numbers | PRV-positive rate | OR | 95% CI |
|---|---|---|---|---|---|
| 2015 | 196 | 31 | 15.8% | 1 (ref.) | |
| 2016 | 395 | 110 | 27.8% | 2.054 | 1.320–3.197 |
| 2017 | 556 | 60 | 10.8% | 0.644 | 0.403–1.028 |
| 2018 | 491 | 56 | 11.4% | 0.685 | 0.427–1.101 |
| Total | 1,638 | 257 | 15.7% |
PRV = pseudorabies virus; OR = odds ratio; CI = confidence interval.
Coinfection
Coinfections of PRV with PRRSV, PCV2, or CSFV were detected in all of the PRV-positive samples tested via PCR. The coinfections varied among the areas tested (Table 4). In this study, 35.0% of the PRV-positive pigs were simultaneously coinfected by PCV2, followed by 12.1% coinfected by PRRSV and 5.8% coinfected by CSFV. The coinfection rates of PRV and PCV2 were over 40% in the Tai’an (28/67), Ji’ning (11/22), Liaocheng (10/20), and Zibo (3/5) areas.
Table 4. Number of PRV-positive samples and number of coinfected PRV-positive samples in different regions of Shandong province from 2015 to 2018.
| City | No. | PRV + PRRSV | PRV + PCV2 | PRV + CSFV |
|---|---|---|---|---|
| Tai'an | 67 | 8 | 28 | 5 |
| Linyi | 44 | 8 | 15 | 2 |
| Ji'ning | 22 | 4 | 11 | 1 |
| Liaocheng | 20 | 1 | 10 | 1 |
| Laiwu | 20 | 3 | 5 | 1 |
| Dongying | 17 | 1 | 4 | 0 |
| Binzhou | 15 | 1 | 3 | 2 |
| Zaozhuang | 11 | 1 | 3 | 1 |
| Ji'nan | 9 | 0 | 1 | 0 |
| Heze | 8 | 1 | 1 | 1 |
| Weifang | 6 | 1 | 2 | 0 |
| Dezhou | 5 | 0 | 2 | 1 |
| Zibo | 5 | 0 | 3 | 0 |
| Qingdao | 3 | 0 | 1 | 0 |
| Rizhao | 2 | 1 | 1 | 0 |
| Weihai | 2 | 1 | 0 | 0 |
| Yantai | 1 | 0 | 0 | 0 |
| Total | 257 | 31/257 (12.1%) | 90/257 (35.0%) | 15/257 (5.8%) |
PRRSV = porcine reproductive and respiratory syndrome virus; PCV2 = porcine circovirus type 2; CSFV = classic swine fever virus.
Clinical signs, gross lesions, and histopathological lesions
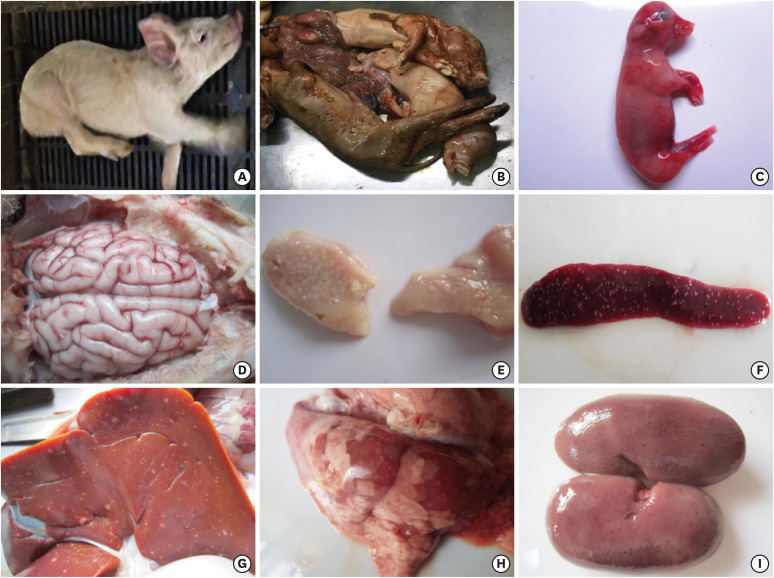
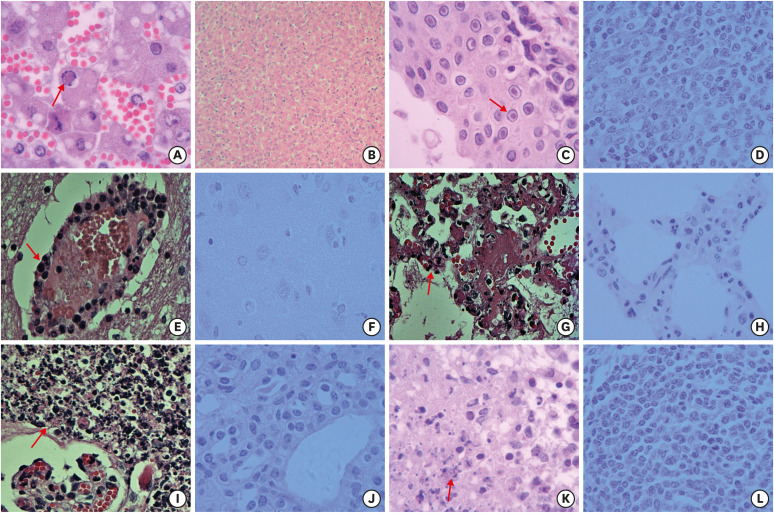
Although the sampled pigs had been previously immunized against PRV, typical pseudorabies cases were observed. Sick sows that were positive for PRV-gE in serum and shown to be PRV-positive by PCR detection (Supplementary Fig. 1) had symptoms that included reproductive disorders, premature birth, stillbirth, and mummified fetus. Infected piglets had typical neurological symptoms, like ataxia and limb paddling behavior. Meninges and brain showed congestion and hemorrhage, and there was an increase in cerebrospinal fluid. Also observed were parenchymatous organs, like liver and spleen, and lymph nodes had visible gray-white necrosis. In addition, lungs showed edema, hemorrhage, congestion, and even serous and cellulosic exudations. Examples of these conditions are shown in Figs. 1 and 2.
Fig. 1. Clinical signs and gross lesions observed in PRV-infected pigs. (A) Typical neurological symptom: infected pigs paddled their limbs; (B, C) Stillbirth: pregnant sow had a miscarriage; (D) Brain: meningeal congestion and bleeding; (E) Tonsil: ulcerative necrosis around crypts; (F) Spleen: dense grayish-white necrotic foci on the surface; (G) Liver: grayish-white necrotic foci of varying sizes on the surface; (H) Lung: interstitial pneumonia with grayish-white necrotic foci; (I) Kidney: needle-shaped hemorrhage and grayish-white necrotic foci on the surface.
Fig. 2. Histopathological lesions in the tissues of pseudorabies virus-infected pigs. (A) Liver: hepatic sinusoids congestion, hepatocyte degeneration, and necrosis, red-stained inclusion bodies in cell nucleus (H & E stain. Original magnification: ×1,000); (B) Liver (control) (H & E stain. Original magnification: × 200); (C) Tonsillar crypts: intranuclear red-stained inclusion bodies in epithelia (H & E stain. Original magnification: ×400); (D) Tonsillar crypts (control) (H & E stain. Original magnification: ×400); (E) Brain: cerebral vascular congestion, perivascular cuffs of lymphocytes (H & E stain. Original magnification: ×400); (F) Brain (control) (H & E stain. Original magnification: ×400); (G) Lung: necrotic inflammation of the pulmonary interstitium, necrosis, and disintegration of infiltrating lymphocytes in necrotic foci (H & E stain. Original magnification: ×400); (H) Lung (control) (H & E stain. Original magnification: ×400); (I) Kidney: necrotic inflammation of renal interstitium, necrosis, and disintegration of infiltrating lymphocytes in necrotic foci (H & E stain. Original magnification: ×400); (J) Kidney (control) (H & E stain. Original magnification: ×400); (K) Spleen: intranuclear red-stained inclusion bodies in epithelia, nuclear disintegration, and necrosis (H & E stain. Original magnification: ×400); (L) Spleen (control) (H & E stain. Original magnification: ×400).
H & E, hematoxylin and eosin.
DISCUSSION
Porcine pseudorabies has been considered one of the most critical and high-priority swine diseases in China and was listed in the “Mid- and Long-term Animal Disease Prevention and Control Program in China”, which targets the eradication of pseudorabies in pig farms in China by the end of 2020 [13,14]. The PRV eradication program was launched in 2011 and has been implemented in some pig farms, especially intensive farms, in Shandong province. Previous studies have shown that the positive rate of PRV-gE in swine farms of northern China have been greater than 50%, with some rates of up to 90% [9,14,15]. The present study is one of the first epidemiological investigations focusing on PRV seroprevalence and its coinfection rates with other major swine viral diseases in Shandong province. It can be speculated that the results presented herein may have a beneficial influence on undertaking PRV prevention and control at not only provincial and national levels but also at the international level.
Our results demonstrate that, regardless of a nearly full vaccination rate, a high proportion of the examined pigs were latently infected by PRV in the field, which is recognized as the most critical source of infection when a latent viral genome is reactivated [8,16]. It, therefore, can be safely concluded that although vaccination is by no means unimportant for PRV prevention and control, the currently available vaccines may not be providing sufficient protection against PRV infection. A previous study reported on some variant PRV strains were isolated in the study area [15]. Such variant viruses not only threaten the health of domestic pigs, but they may also cause bovine death through interspecies infection [17]. Thus, it is necessary to urgently undertake other forceful preventive measures, such as biosecurity strengthening, animal monitoring, virus identification, removal of latent carriers, and improvement of environmental hygiene [18,19].
It is not uncommon for pigs to be concurrently infected with more than one pathogen under the current intensive swine breeding system. Previous studies have reported that pigs can be coinfected by PRV and a wide range of other pathogens, such as PRRSV, CSFV, PCV2, Streptococcus spp., etc. In this study, 35.0% of the PRV-positive pigs were coinfected by PCV2. It has been reported that PCV2 may significantly influence the reproductive performance of gilts and multiparous sows [20,21]. A possible explanation for the high incidence of coinfections is that presence of a latent PRV infection may weaken a pig's immune system, resulting in increased susceptibility to other pathogens. Our findings reveal a high frequency of coinfection of PRV and PCV2 in Shandong province, China.
CONCLUSIONS
The results of this study clearly demonstrate that PRV is endemic at high levels in pig farms in Shandong province and PRV infection is widespread throughout the province. The currently available vaccines appear to provide only limited protection against PRV infection. A majority of the PRV-infected pigs in Shandong province were shown to be coinfected, with most of those infected with PCV2. This high incidence of coinfection should be considered crucial during the design of programs for pseudorabies control and PRV eradication.
Footnotes
Funding: This study is supported from Shandong “Double Tops” Program, National Key Research and Development Program of China, Grant/Award Number: 2017YFD0500600.
Conflict of Interest: The authors have no conflicts of interest to declare.
- Conceptualization: Ma Z, Han Z.
- Data curation: Ma Z, Han Z.
- Formal analysis: Ma Z, Han Z.
- Funding acquisition: Liu S.
- Investigation: Ma Z, Han Z, Meng F, Wang H, Cao L, Li Y, Jiao Q.
- Methodology: Ma Z, Liu M.
- Writing - original draft: Ma Z, Han Z.
- Writing - review & editing: Liu S, Liu M.
SUPPLEMENTARY MATERIAL
Results obtained from polymerase chain reaction assays used to detect the presence of pseudorabies virus.
References
- 1.Mettenleiter TC. Aujeszky's disease (pseudorabies) virus: the virus and molecular pathogenesis--state of the art, June 1999. Vet Res. 2000;31(1):99–115. doi: 10.1051/vetres:2000110. [DOI] [PubMed] [Google Scholar]
- 2.Pomeranz LE, Reynolds AE, Hengartner CJ. Molecular biology of pseudorabies virus: impact on neurovirology and veterinary medicine. Microbiol Mol Biol Rev. 2005;69(3):462–500. doi: 10.1128/MMBR.69.3.462-500.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crandell RA. Pseudorabies (Aujeszky's disease) Vet Clin North Am Large Anim Pract. 1982;4(2):321–331. doi: 10.1016/s0196-9846(17)30108-8. [DOI] [PubMed] [Google Scholar]
- 4.Rziha HJ, Mettenleiter TC, Ohlinger V, Wittmann G. Herpesvirus (pseudorabies virus) latency in swine: occurrence and physical state of viral DNA in neural tissues. Virology. 1986;155(2):600–613. doi: 10.1016/0042-6822(86)90220-5. [DOI] [PubMed] [Google Scholar]
- 5.Müller T, Hahn EC, Tottewitz F, Kramer M, Klupp BG, Mettenleiter TC, Freuling C. Pseudorabies virus in wild swine: a global perspective. Arch Virol. 2011;156(10):1691–1705. doi: 10.1007/s00705-011-1080-2. [DOI] [PubMed] [Google Scholar]
- 6.Smith G. Preferential sexual transmission of pseudorabies virus in feral swine populations may not account for observed seroprevalence in the USA. Prev Vet Med. 2012;103(2-3):145–156. doi: 10.1016/j.prevetmed.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tong W, Li G, Liang C, Liu F, Tian Q, Cao Y, Li L, Zheng X, Zheng H, Tong G. A live, attenuated pseudorabies virus strain JS-2012 deleted for gE/gI protects against both classical and emerging strains. Antiviral Res. 2016;130:110–117. doi: 10.1016/j.antiviral.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 8.An TQ, Peng JM, Tian ZJ, Zhao HY, Li N, Liu YM, Chen JZ, Leng CL, Sun Y, Chang D, Tong GZ. Pseudorabies virus variant in Bartha-K61-vaccinated pigs, China, 2012. Emerg Infect Dis. 2013;19(11):1749–1755. doi: 10.3201/eid1911.130177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu R, Bai C, Sun J, Chang S, Zhang X. Emergence of virulent pseudorabies virus infection in northern China. J Vet Sci. 2013;14(3):363–365. doi: 10.4142/jvs.2013.14.3.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y, Qiao S, Li X, Xie W, Guo J, Li Q, Liu X, Hou J, Xu Y, Wang L, Guo C, Zhang G. Molecular epidemiology of outbreak-associated pseudorabies virus (PRV) strains in central China. Virus Genes. 2015;50(3):401–409. doi: 10.1007/s11262-015-1190-0. [DOI] [PubMed] [Google Scholar]
- 11.Song C, Gao L, Bai W, Zha X, Yin G, Shu X. Molecular epidemiology of pseudorabies virus in Yunnan and the sequence analysis of its gD gene. Virus Genes. 2017;53(3):392–399. doi: 10.1007/s11262-017-1429-z. [DOI] [PubMed] [Google Scholar]
- 12.Xia L, Sun Q, Wang J, Chen Q, Liu P, Shen C, Sun J, Tu Y, Shen S, Zhu J, Zhao H, Wang Q, Li B, Tao J, Soares Magalhaes RJ, Yan Y, Cai C. Epidemiology of pseudorabies in intensive pig farms in Shanghai, China: Herd-level prevalence and risk factors. Prev Vet Med. 2018;159:51–56. doi: 10.1016/j.prevetmed.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Sun Y, Luo Y, Wang CH, Yuan J, Li N, Song K, Qiu HJ. Control of swine pseudorabies in China: opportunities and limitations. Vet Microbiol. 2016;183:119–124. doi: 10.1016/j.vetmic.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Hu D, Lv L, Zhang Z, Xiao Y, Liu S. Seroprevalence and associated risk factors of pseudorabies in Shandong province of China. J Vet Sci. 2016;17(3):361–368. doi: 10.4142/jvs.2016.17.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gu J, Hu D, Peng T, Wang Y, Ma Z, Liu Z, Meng F, Shang Y, Liu S, Xiao Y. Epidemiological investigation of pseudorabies in Shandong Province from 2013 to 2016. Transbound Emerg Dis. 2018;65(3):890–898. doi: 10.1111/tbed.12827. [DOI] [PubMed] [Google Scholar]
- 16.Sabó A. Analysis of reactivation of latent pseudorabies virus infection in tonsils and Gasserian ganglia of pigs. Acta Virol. 1985;29(5):393–402. [PubMed] [Google Scholar]
- 17.Cheng Z, Kong Z, Liu P, Fu Z, Zhang J, Liu M, Shang Y. Natural infection of a variant pseudorabies virus leads to bovine death in China. Transbound Emerg Dis. 2020;67(2):518–522. doi: 10.1111/tbed.13427. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, Zhang S, Xu Q, Wu J, Zhai X, Li S, Wang J, Ni J, Yuan L, Song X, Zhao B, Zhou Z, Wang C, Yang L. Investigation on pseudorabies prevalence in Chinese swine breeding farms in 2013–2016. Trop Anim Health Prod. 2018;50(6):1279–1285. doi: 10.1007/s11250-018-1555-1. [DOI] [PubMed] [Google Scholar]
- 19.Liu M, Kemper N, Volkmann N, Schulz J. Resistance of enterococcus spp. in dust from farm animal houses: a retrospective study. Front Microbiol. 2018;9:3074. doi: 10.3389/fmicb.2018.03074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mak CK, Yang C, Jeng CR, Pang VF, Yeh KS. Reproductive failure associated with coinfection of porcine circovirus type 2 and porcine reproductive and respiratory syndrome virus. Can Vet J. 2018;59(5):525–530. [PMC free article] [PubMed] [Google Scholar]
- 21.Dias AS, Gerber PF, Araújo AS, Auler PA, Gallinari GC, Lobato ZI. Lack of antibody protection against Porcine circovirus 2 and Porcine parvovirus in naturally infected dams and their offspring. Res Vet Sci. 2013;94(2):341–345. doi: 10.1016/j.rvsc.2012.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results obtained from polymerase chain reaction assays used to detect the presence of pseudorabies virus.