Abstract
PURPOSE:
As teens in foster care prepare for emancipation, healthcare navigation is often overlooked as caseworkers address other social needs. This study examined the impact of healthcare education materials designed for foster youth, called ICare2CHECK. It was hypothesized that ICare2CHECK would increase non-urgent ambulatory healthcare use and decrease emergency/urgent care use.
METHODS:
Adolescents (N = 151; ages 16-22 years) were enrolled into ICare2CHECK and received health education materials at their baseline study visit. Surveys were repeated every three months to assess healthcare utilization. After 12 months of enrollment, healthcare data for all eligible youth and matched comparison youth (N=151) over the previous 24 months was extracted from the electronic health record (EHR; N = 302). EHR data was coded as counts of completed non-urgent ambulatory care encounters (i.e., primary and preventative care, specialty care), completed urgent or emergency encounters (i.e., urgent and emergency department visits, hospitalizations), completed foster care clinic visits, and total completed visits.
Results:
Healthcare use significantly decreased over time for both enrolled and comparison youth. Females, youth engaging in health risk behaviors, and those with a mental health or chronic condition diagnosis used significantly more healthcare. Receipt of educational materials, was associated with a smaller decline in healthcare use and non-urgent ambulatory care use, controlling for covariates. Self-reported use of educational materials was associated with increased utilization in the enrolled condition.
CONCLUSIONS:
Results suggest that ICare2CHECK is associated with increased engagement in healthcare generally, and non-urgent ambulatory care specifically (e.g., outpatient primary and specialty care).
Keywords: adolescent, foster care, health education, emancipation, healthcare utilization
INTRODUCTION
Young people emancipating from foster care face multiple health obstacles as adults. They experience higher rates of substance use, sexually transmitted infections, unintended pregnancy, injury, illness, and report disrupted health insurance coverage and poor access to healthcare following emancipation (1–7). Importantly, adolescents involved with child welfare have frequently experienced complex trauma and adversity, a significant predictor of poor health outcomes across the lifespan (8–10). Health concerns persist into early adulthood (2), motivating expanded foster care to age 21 (11) and eligibility for Medicaid until age 26 (12). While this is critical, experts and advocacy organizations have encouraged healthcare and child welfare systems to also develop targeted health education materials for young people emancipating from foster care (13), as it remains unclear whether expanded services and healthcare coverage alone is sufficient to alter young people’s engagement with healthcare systems and self-management of health (4, 14).
Educating young people about their health and navigating healthcare systems independently is important for all youth, in part because the transition from pediatric to adult care can be challenging (15–18). Healthcare transition and self-management education often occurs in the context of primary care, where best practice guidelines recommend that young people have conversations with their parents and primary care providers about accessing healthcare, engaging with health care systems, and managing their health independently (19). For adolescents in foster care there is reason to suspect that planning for the healthcare transition is overlooked (20). These young people do not have parents to assist them with navigating this transition, and the county or state representative acting as the in loco parentis typically focuses on other activities of daily living (e.g., budgeting and finance, school, work, transportation). Finally, while all young people in foster care are required to be seen for an annual physical and other healthcare services are recommended (21), research has demonstrated that foster youth frequently change healthcare providers, and are often disconnected from primary care (22, 23). As a result, young people emancipating from foster care may be less likely to experience coordinated transition and transfer to primary care providers (5, 14).
This study sought to investigate whether healthcare education materials developed in conjunction with young people support engagement with healthcare services in preparation for emancipation. It was hypothesized that delivery of high-quality, relevant educational materials would promote engagement with primary and specialty healthcare and would decrease reliance on emergency and urgent care.
METHODS
Participants
Adolescents in child protective services (CPS) custody for at least 12 months who were expected to emancipate due to a combination of age, case plan goal, and/or legal status were recruited to participate. All adolescents were in the custody of a single county child welfare agency that had extended foster care to age 21 years. Adolescents were considered eligible if they were aged 16 years or older, were without a diagnosis of cognitive disability or intelligence quotient (IQ) below 70, were English-speaking, and were residing in a family, group home, or independent living setting within a 1-hour driving distance of the academic medical center where the study was based. Adolescents younger than 16 years old, those with a cognitive disability or IQ below 70, youth who had been in protective custody for fewer than 12 months, and youth placed in inpatient treatment settings, nursing homes, juvenile detention, or who were reunited with family or adopted were considered ineligible to participate. All youth who participated in ICare2CHECK provided assent (if under age 18 years) or consent (if 18 years or older) to participate in the study. Of 436 youth who were determined eligible to participate in ICare2cHECK, 151 were recruited. Of the remaining 285 youth, 151 were matched based on gender, age, and race and ethnicity to serve as a comparison sample.
Procedures
Study staff communicated with CPS, who provided a letter of consent for all eligible participants. CPS provided study staff with a list of eligible youth that included case history, current placement status, and names of stakeholders including guardians ad litem and caseworkers. These individuals were contacted about the youths’ eligibility for the study and were given the opportunity to opt youth out of participating. Study staff reviewed child welfare and electronic health records (EHR) to confirm eligibility. Youth who were deemed eligible (N=365) were mailed a letter explaining the study with instructions to opt out of additional contact. Study staff then contacted participants by phone or in person while receiving medical care at the foster care clinic located at Cincinnati Children’s Hospital Medical Center (CCHMC). This study was approved and monitored by the Institutional Review Board at CCHMC.
More than half (N=204) of eligible youth were successfully contacted, and 154 provided initial verbal consent (if aged 18 years or older) or assent (if aged 16 or 17 years) to participate. Three participants were lost to enrollment due to changes in placement (n = 2) or incarceration (n = 1). Study staff scheduled in-person visits with youth in their homes or public locations (e.g., community centers, libraries, restaurants). During visits, participants (N=151) provided written informed assent or consent and completed surveys. In-person visits occurred at baseline, six months after baseline, and twelve months after baseline. Participants also completed brief phone surveys three and nine months after baseline. Participants were compensated for their time with a ClinCard valued at $15 plus a first aid kit and study materials for their first visit, $20 for the six month follow-up, and $20 for the twelve month follow-up.
Study staff received electronic health record (EHR) data from CCHMC for enrolled and comparison youth in the year prior to and during study participation. Extracted data included encounter date, encounter type (primary care, specialty care, emergency and urgent care, and hospitalizations), encounter diagnoses, flowsheet data, and laboratory screening results.
Materials
The ICareGuide is an analog tool designed to assist foster youth in navigating the healthcare system and maintaining connections to primary care. Design experts from the Live Well Collaborative engaged with foster youth and stakeholders to design the ICareGuide. Youth selected the format, organization, and styling of the information. The resulting pocket-sized guide included space to record personal health information such as medications, immunization records, and family medical history as well as provided information on accessing heathcare (including primary care doctors, dentists, and eye doctors), sexual and reproductive health, and managing medical emergencies. The guide included a chart listing various symptoms and guidance on appropriate level of health care (e.g., when to seek emergency care), instructions on how to apply for Medicaid, how to prepare for and arrange transportation to medical appointments, and why preventive healthcare is important. Information regarding prevention of pregnancy and sexually transmitted infections as well as emergency hotlines were included. During focus groups, many youth requested information regarding pediatric care for their own children, and this information was added. Youth also rejected a mental health or wellness section, so information on this topic, such as healthy relationships and mental health support hotlines, was spread throughout the guide.
The companion website, www.icare2check.org, was designed to provide information similar to that in the ICareGuide. Additional information not present in the ICareGuide included interactive features such as maps showing healthcare facility locations, a tool to assist youth in deciding what type of medical treatment (e.g., self-treatment, primary care, or emergency services) they need, links to healthcare knowledge games, and the transition readiness assessment questionnaire (24). Information geared toward caregivers of youth in foster care, such as how to talk to youth about sensitive subjects like mental and sexual health, was included on the site.
Measures
EHR data was coded as counts of completed non-urgent encounters (i.e., primary and preventative care, specialty care), missed encounters (i.e., scheduled but not completed or cancelled in less than 24 hours), completed urgent or emergency encounters (i.e., urgent and emergency department visits, hospitalizations), and mandated foster care clinic encounters. Mental health and chronic medical conditions were dichotomously coded from encounter diagnoses. Lifetime substance use (e.g., alcohol, tobacco, marijuana; yes/no) was coded from encounter diagnoses, laboratory results, and flowsheet data. Sexual risk behaviors (e.g., multiple partners, sexual debut before age 14, inconsistent use of barrier protection, diagnosis of sexually transmitted infections, pregnancy; yes/no) was coded from encounter diagnoses, laboratory results, and flowsheets. Demographic characteristics (age at baseline visit, minority status [yes/no], sex [male/female]) were also derived from the EHR.
At follow-up study visits, enrolled youth reported whether they still had their ICareGuide (yes/no) and had used their ICareGuide to complete any of the following tasks (yes/no): make a doctor’s appointment, arrange transportation to a medical appointment, make decisions about what type of healthcare to utilize, visit a free clinic, learn about sexual health, and deciding what to do in case of an emergency. At the final study visit, participants reported how helpful they believed the ICareGuide was (Not at all helpful, Not very helpful, Unsure, Somewhat helpful, Very helpful) and whether they planned to use their ICareGuide in the future (yes, no, unsure).
Self-reported healthcare utilization data for enrolled youth were derived from survey results. At baseline, participants reported the number of times they had seen primary care, specialty care, and emergency care providers in the past twelve months. At each subsequent visit, participants reported the number of times they had seen these providers since the previous study visit.
CPS provided number of placement changes, length of time in custody, legal status (planned permanent living arrangement, permanent custody, and temporary custody), and primary removal reason (neglect, physical/emotional/sexual abuse, child behavior problems).
Utilization of www.ICare2CHECK.org was evaluated using Google Analytics to track website traffic, locations of users, and page visits.
RESULTS
Adolescents recruited into ICare2CHECK (N = 151) had a mean age of 18.08 years (SD = 1.36). Youth were African American (70.5%), non-Hispanic white (24.5%), or multi-racial or other racial and ethnic categories (5%); 54% of participants were female. Adolescents were in foster care for 1 to 14 years (M = 2.91, SD = 3.16); most had a legal status of planned permanent living arrangement (71.7%) or permanent custody (12%). Youth entered foster care primarily due to neglect (62%), physical abuse (5%), sexual abuse (3%), emotional abuse (3%), or child behavior problems (27%). The majority of adolescents (61%) participated in all 3 in-person data collection time points; 21% completed only 2 visits, and 17% completed only the baseline study visit. There were no significant differences in demographic characteristics or healthcare utilization between those who completed 2 or more study visits and those who were lost to follow-up (ps > .05). Youth enrolled in ICare2CHECK were slightly younger than comparison youth (t (300) = 4.06, p < .01), and used more healthcare in the year prior to enrollment (t (240) = −2.09, p = .03) because of more visits to the foster care clinic (t (300) = −4.22, p < .01); no differences in emergency and urgent care or non-urgent healthcare were identified (see Table 1). Youth enrolled in ICare2CHECK were also generally more impaired; they were more likely to have a chronic medical condition (χ2 (1) = 27.70, p < .01) or mental health diagnosis (χ2 (1) = 39.06, p < .01) than comparison youth and were more likely to engage in health risk behaviors (χ2 (1) = 9.11, p < .01 and χ2 (1) = 7.28, p < .01 for lifetime substance use and sexual risk taking, respectively).
Table 1.
Descriptive statistics for youth in ICare2CHECK enrolled and comparison samples.
| Comparison Sample | ICare2CHECK Enrolled Sample | Significant Group Difference | |||
|---|---|---|---|---|---|
| Variable | M/% | SD | M/% | SD | |
| Age (Year 1) | 18.72 | 1.39 | 18.08 | 1.36 | t (300) = 4.06** |
| Adolescent girls | 0.54 | 0.54 | ns | ||
| Racial/Ethnic minority | 0.75 | 0.75 | ns | ||
| Number of placements | 7.06 | 5.45 | 6.62 | 4.84 | ns |
| Length of time in care | 3.17 | 3.29 | 2.91 | 3.16 | ns |
| Legal Status | ns | ||||
| Temporary custody | 0.19 | 0.16 | |||
| Permanent custody | 0.20 | 0.12 | |||
| Planned permanent living arrangement | 0.61 | 0.72 | |||
| Primary Removal Reason | ns | ||||
| Neglect | 0.59 | 0.61 | |||
| Physical abuse | 0.12 | 0.04 | |||
| Sexual abuse | 0.04 | 0.03 | |||
| Child behavior problems | 0.19 | 0.28 | |||
| Parental substance use | 0.04 | 0.01 | |||
| Emotional abuse/neglect | 0.02 | 0.03 | |||
| Total Health Care Use | |||||
| Year 1 | 3.19 | 5.49 | 4.39 | 4.40 | t (240) = −2.09* |
| Year 2 | 0.75 | 1.75 | 2.60 | 4.07 | t ( 203) = −5.13** |
| Mandated Foster Care Visits | |||||
| Year 1 | 0.63 | 1.10 | 1.20 | 1.24 | t (300) = −4.22** |
| Year 2 | 0.15 | 0.47 | 0.40 | 0.75 | t (300) = −3.47** |
| Scheduled Visits | |||||
| Year 1 | 1.78 | 4.93 | 2.26 | 3.41 | ns |
| Year 2 | 0.42 | 1.27 | 1.61 | 3.47 | t (300) = 2.61** |
| Unscheduled Visits | |||||
| Year 1 | 0.78 | 1.51 | 0.93 | 1.59 | ns |
| Year 2 | 0.18 | 0.57 | 0.59 | 1.28 | t (300) = −3.60** |
| Lifetime substance use (y) | 0.34 | 0.52 | χ2 (1) = 9.11** | ||
| Current substance use (y) | 0.28 | 0.40 | ns | ||
| Lifetime sexual risk behavior (y) | 0.70 | 0.85 | χ2 (1) = 7.28** | ||
| Any chronic condition (y) | 0.09 | 0.35 | χ2 (1) = 27.70** | ||
| Any mental health diagnosis (y) | 0.26 | 0.63 | χ2 (1) = 39.06** | ||
Note: Age, race, ethnicity, number of placements, length of time in care, legal status, primary removal reason were determined based on child welfare report. Gender, healthcare use, lifetime substance use (i.e., ever endorsed tobacco, alcohol, marijuana, or illicit substance use, any encounter), current substance use (i.e., endorsed tobacco, alcohol, marijuana, or illicit substance use during an encounter over the past 12 months), lifetime sexual risk behavior (i.e., multiple partners, inconsistent condom use, sexually transmitted infection diagnosis), chronic condition diagnosis, and mental health diagnosis was based on electronic health record data.
The majority of adolescents reported that the ICareGuide was somewhat (46%) or very helpful (42%), and 78% of participants who responded to surveys at the 12 month follow-up reported that they still had the guide (42% of all participants who received a guide at enrollment). The majority of youth (80%) reported using the ICareGuide at least once during the study, with sections discussing emergency care, reproductive health, and symptoms information most commonly endorsed. Figure 1 illustrates frequencies of use for ICareGuides by study participants, with consistent use reported across timeframes. The ICareSite was used less frequently by study participants, with 140 unique users locally accessing the site over the study period and a median frequency of 1 visit per local user.
Figure 1.
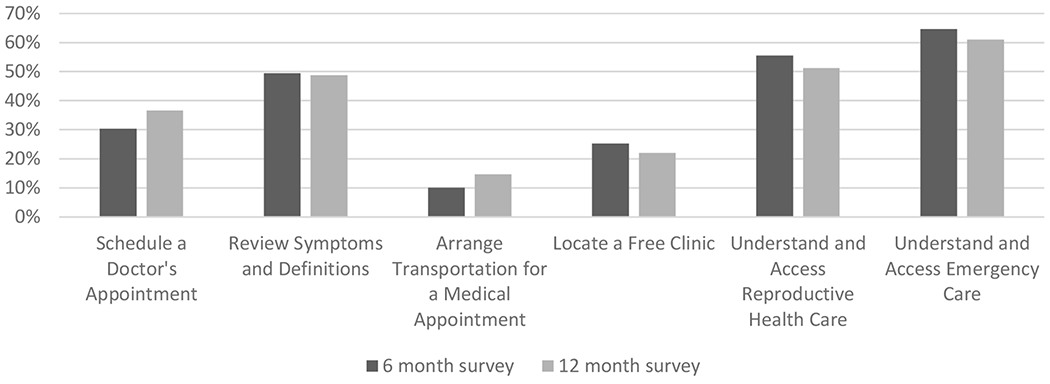
Percentage of participants endorsing use of the ICareGuide for specific health information at the 6 month and 12 month follow-up surveys.
Healthcare utilization significantly decreased for both enrolled and comparison youth in the year following study launch (t (150) = 5.65, p < .01 and t (150) = 5.13, p < .01, respectively). Similar patterns were observed for foster care clinic visits, non-urgent healthcare visits, and emergency and urgent care. Participant self-report of healthcare use was compared to EHR data from the same time-frame. Across all types of healthcare use, self-report data generally indicated higher healthcare use than EHR data. Specifically, for 12% of youth total healthcare use was higher in EHR data than self-report, 3% had agreement between data sources, and the remaining 85% reported more total healthcare use than was reflected in EHR data.
Multivariate Analyses
To account for existing group differences, generalized multivariate regression models were estimated predicting healthcare use in the year following study launch for enrolled and comparison youth. Healthcare use was non-normally distributed; both Poisson and negative binomial regression models with and without zero-inflation were estimated. A combination of residual variances and results from Vuong’s test (25) were used to determine the model that best fit count outcome data for total healthcare use, foster care clinic visits, non-urgent healthcare, and urgent and emergency visits. Analyses were completed using R version 3.5.3.
For total healthcare use, a negative binomial distribution without zero-inflation best fit the data (dispersion = 1.07, residual variance (590) = 597.72, Vuong’s z = −1.19, p = .11). Model results indicated a significant time by group interaction, such that after accounting for the significant effects of demographic characteristics, health risk behaviors, and diagnoses between the two groups, enrolled youth experienced a significantly smaller decrease in healthcare utilization than their peers in the comparison condition (Table 2, Figure 2).
Table 2.
Multivariate model results predicting total healthcare use, mandated use, scheduled visits, and unscheduled visits
| Total | Mandated | Scheduled | Unscheduled | |||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Intercept | 6.40** | 0.84 | 5.14** | 0.98 | 5.39** | 1.28 | −0.78 | 1.73 |
| Group | −0.06 | 0.15 | 0.29* | 0.14 | −0.08 | 0.23 | −0.43 | 0.22 |
| Time | −1.36** | 0.17 | −1.29** | 0.23 | −1.45** | 0.26 | −0.64 | 0.38 |
| Group*time | 0.87** | 0.21 | 0.33 | 0.28 | 1.13** | 0.33 | 0.27 | 0.42 |
| Age | −0.32** | 0.04 | −0.32** | 0.05 | −0.30** | 0.07 | −0.01 | 0.10 |
| Gender | 0.68** | 0.11 | 0.35** | 0.11 | 0.79** | 0.17 | 0.75** | 0.19 |
| Minority | −0.19 | 0.12 | 0.19 | 0.13 | −0.39* | 0.19 | −0.08 | 0.20 |
| Length of time in custody | −0.01 | 0.02 | −0.04* | 0.01 | 0.02 | 0.02 | −0.07* | 0.03 |
| Number of placements | 0.01 | 0.02 | 0.04** | 0.01 | −0.02 | 0.02 | 0.07* | 0.03 |
| Substance use | 0.71** | 0.12 | 0.49** | 0.11 | 0.65** | 0.19 | 0.25 | 0.19 |
| Sexual Risk | 0.00** | 0.00 | 0.01** | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Chronic conditions | 0.49** | 0.12 | −0.22 | 0.13 | 0.81** | 0.19 | 0.12 | 0.19 |
| Mental health diagnoses | 0.23* | 0.11 | −0.08 | 0.11 | 0.27 | 0.18 | 0.92** | 0.20 |
p < .01;
p < .05
Figure 2.
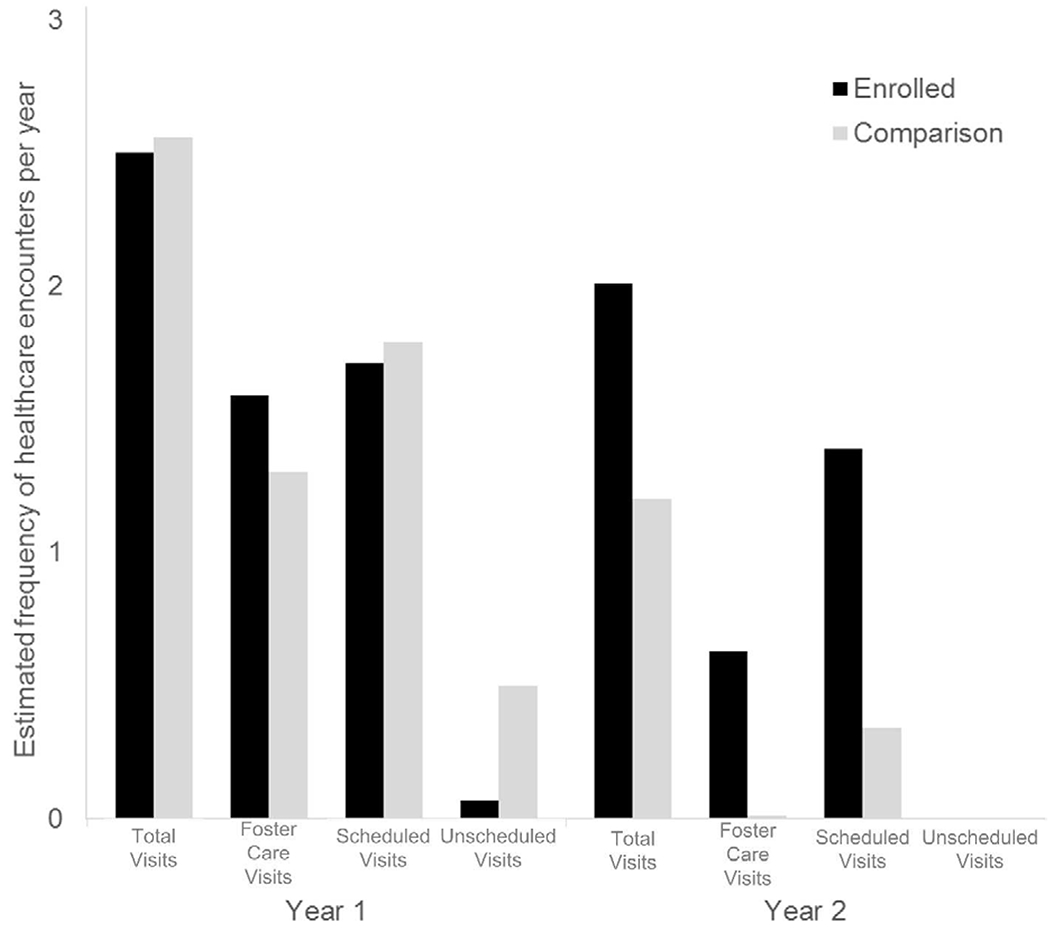
Estimated frequency of healthcare use captured in the electronic health record by encounter type for youth enrolled in ICare2CHECK and comparison youth.
For foster care visits, a Poisson distribution without zero-inflation best fit the data (residual variance (590) = 508.61, Vuong’s z = −1.61, p = .06). Model results indicated that after accounting for the significant effects of demographic characteristics, health risk behaviors, and diagnoses between the two groups, there was a significant decrease in foster care visits over time for both groups, with enrolled youth continuing to have foster care visits more frequently than their peers in the comparison condition.
For non-urgent healthcare visits, a negative binomial distribution without zero-inflation best fit the data (dispersion = 0.39, residual variance (590) = 469.51, Vuong’s z = 1.38, p = .08). Model results indicated a significant time by group interaction, such that after accounting for the significant effects of demographic characteristics, health risk behaviors, and diagnoses between the two groups, enrolled youth experienced a significantly smaller decrease non-urgent healthcare care than their peers in the comparison condition.
For urgent and emergency care visits, a zero-inflated negative binomial distribution best fit the data (Vuong’s z = 3.65, p < .01). Results indicated that there were no significant changes in urgent or emergency care visits with time or by group after accounting for covariates.
Additional Poisson regression models estimated associations between self-reported healthcare utilization and self- use of the ICareGuide for enrolled young people. Those findings (Table 3) indicated that young people who reported using the ICareGuide more frequently also reported higher healthcare utilization across types of use (i.e., primary, specialty, urgent, emergency care) after accounting for covariates.
Table 3.
Multivariate Poisson regression analyses predicting self-reported healthcare utilization over a 12-month period, predicted by self-reported frequency of ICareGuide use among those in the enrolled condition (n = 151)
| Primary Care | Specialty Care | Urgent Care | Emergency Care | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE |
| Intercept | −0.40 | 0.77 | −4.80** | 1.28 | 10.17** | 2.66 | 3.16 | 2.25 |
| ICareGuide use | 0.03** | 0.01 | 0.03* | 0.02 | 0.10** | 0.02 | 0.05* | 0.02 |
| Age | 0.09* | 0.04 | 0.24** | 0.07 | −0.58** | 0.15 | −0.16 | 0.12 |
| Gender | 0.22* | 0.11 | 0.74** | 0.20 | 0.03 | 0.27 | −0.06 | 0.26 |
| Minority status | 0.04 | 0.13 | 0.12 | 0.25 | −0.92** | 0.26 | −1.03** | 0.25 |
| Substance use | −0.03 | 0.10 | 0.40* | 0.17 | 0.17 | 0.25 | 0.02 | 0.24 |
| Sexual risk behavior | 0.15 | 0.11 | −0.28 | 0.19 | −0.17 | 0.28 | 0.13 | 0.28 |
| Chronic condition | −0.08 | 0.16 | −1.48** | 0.46 | 0.45 | 0.40 | −0.62 | 0.52 |
| Mental Health diagnosis | −0.07 | 0.11 | 0.26 | 0.19 | −0.77** | 0.28 | −0.27 | 0.26 |
p < .05;
p < .01
DISCUSSION
This study evaluated the impact of healthcare education materials on healthcare utilization using EHR data from a pediatric medical center and participant self-report. The ICareGuide had high acceptance, with the majority of youth retaining the guide over the study period. Healthcare utilization declined with age; however, the decline was less severe for total and non-urgent healthcare visits for enrolled youth based on EHR data, and frequency of ICareGuide use was associated with increased self-reported healthcare utilization. Contrary to our hypothesis, there were no significant differences in emergency and urgent care use for those who did and did not receive the ICareGuide. It is possible that the ICareGuide had no impact on emergency and urgent care use; however, youth who received the ICareGuide had more chronic conditions than the comparison sample. As a result, it remains unclear whether ICareGuide use was ineffective, or whether youth in the intervention condition required more emergency and urgent care than the comparison sample due to their disease burden. These preliminary findings suggest that the ICareGuide may be beneficial for assisting young people with accessing healthcare during the transition out of foster care.
Given normative expectation that young people will decrease engagement in pediatric healthcare services in young adulthood, it is not surprising that all adolescents experienced declines in healthcare utilization over the two years of this study. At the freestanding children’s hospital where this study took place, adolescent primary care and foster care clinic services continue to age 21. However, age ranges for other specialties vary, consistent with the landscape of healthcare and the transition between pediatric and adult services nationally (19). This could, in part, explain why healthcare use decreased generally, and why there were no differences observed in emergency healthcare utilization for enrolled and comparison youth. Consistent with this explanation, self-reported healthcare use (across all types) increased as self-reported use of the ICareGuide increased. Research evaluating the impact of the ICareGuide objectively and across multiple healthcare settings is warranted.
Supporting access to non-urgent healthcare may be particularly beneficial as foster youth prepare for independence and self-management of healthcare services. Adolescents in foster care are known to have more acute and chronic health concerns than their peers (13, 26, 27), which may have life-long impact. Connections with outpatient primary and specialty services support access to preventative healthcare services known to confer life-long benefit (28, 29). For that reason, it may be particularly beneficial for adolescents preparing for emancipation to engage with non-urgent healthcare systems, including primary care and medical homes, to receive healthcare transition planning services in preparation for independence in self-management (30).
Our research team initially expected that young people would desire a technology-based platform for ICareGuides; however, young people reported that they desired a durable analog solution that they could carry with them, without relying on technology. Consistent with other studies (31), youth participating on our design team faced challenges with technology maintenance rather than access. They requested a discrete, pocket-sized guide that they could write in, keep organized, and that was durably bound and laminated to protect from damage. The integration of foster youth into the design of the ICareGuide may have contributed to the majority of young people retaining their guide after 12 months. The ICareSite was designed as a companion, with similar information and some technology-based benefits (e.g., maps updated by location) to supplement and provide support in the event that youth lost or misplaced the ICareGuide. It was therefore no surprise that results indicate young people in ICare2CHECK used the ICareGuide more frequently, while the ICareSite was accessed less often. The desire to have an analog version of the ICareGuide may change as technology maintenance improves; future research studying this more closely is needed.
Following ICare2CHECK, CPS has sustained access to ICareGuides for youth in their custody. Young people are provided a guide when they turn 16 and caseworkers and healthcare providers completing exams at the foster care clinic assist young people with completing the guide. It takes approximately 15 minutes to discuss the ICareGuide with young people. The burden introduced by providing ICareGuides to young people is low, with high perceived value for CPS. The ICareGuide has additionally been adapted for dissemination with youth with juvenile justice involvement (32).
While this study holds significant potential to improve healthcare education for young people in foster care, limitations must be considered. A randomized control trial would definitively demonstrate the impact of ICareGuides on healthcare utilization outcomes for adolescents in foster care. Foster youth enrolled in ICare2CHECK were significantly more likely to have a chronic condition or mental health diagnosis than comparison youth, which may have promoted engagement with the healthcare system, biasing findings. Additionally, healthcare utilization was objectively measured within a single healthcare system, and young people were accessing healthcare services outside of our pediatric healthcare system. Replication of this study in a community where health information exchanges or Medicaid billings data are available would be ideal. Finally, healthcare utilization, while important, is not a perfect proxy for health status – the ultimate indicator of adolescent and young adult wellbeing. Studies examining young people’s reports of their health status, quality of life, disease management, missed days from school or work, or other indicators of health (e.g., disease-specific indicators such as Hemoglobin A1c or asthma control) in a longitudinal manner would be ideal to establish that ICare2CHECK improved health outcomes for young people.
Despite these limitations, this study makes an important contribution in that it provides preliminary evidence that a low-impact intervention may improve healthcare utilization in a population of foster youth who are preparing for emancipation. This is a highly vulnerable group of young people (2, 33) with known health risks in foster care (34, 35) and following emancipation (1, 2, 6, 36). Materials that support conversations and share information to improve healthcare utilization, such as the ICareGuide, may be beneficial in addressing health needs and closing the disparities these young people face in healthcare access and health status in adulthood.
IMPLICATIONS AND CONTRIBUTIONS.
This study evaluated novel healthcare education materials specifically designed for emancipating foster youth. Findings indicate that young people benefit from receiving ICare2CHECK materials, particularly for maintaining engagement with non-urgent ambulatory care. ICare2CHECK may ease the transition to self-management of healthcare for adolescents in foster care.
Acknowledgments:
This study is based on data from an observational study where clinical trials registration was not required. The findings reported in this manuscript have not been previously published or presented at any conference proceedings. The project described was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number 5UL1TR001425-02, the CareSource Foundation, the Cincinnati Children’s Hospital Medical Center Research Foundation, and the National Institute of Drug Abuse, under Award Number 1 K01 DA041620-01A1. All authors declare that they have no conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA or the National Institutes of Health.
Abbreviations:
- IQ
Intelligence quotient
- CPS
Child Protective Services
- CCHMC
Cincinnati Children’s Hospital Medical Center
- EHR
Electronic Health Record
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Courtney ME, Dworsky AL, Brown A, et al. Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 26. 2011. [Google Scholar]
- [2].Ahrens KR, Garrison MM, Courtney ME. Health outcomes in young adults from foster care and economically diverse backgrounds. Pediatrics 2014;134:1067–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ahrens KR, Richardson LP, Courtney ME, et al. Laboratory-diagnosed sexually transmitted infections in former foster youth compared with peers. Pediatrics 2010;126:e97–e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dworsky A, Ahrens K, Courtney M. Health insurance coverage and use of family planning services among current and former foster youth: implications of the health care reform law. Journal of Health Politics, Policy, and Law 2013;38:421–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Dworsky A, Courtney M. Addressing the mental health service needs of foster youth during the transition to adulthood: how big is the problem and what can states do? Journal of Adolescent Health 2009;44:1–2. [DOI] [PubMed] [Google Scholar]
- [6].Dworsky A, Courtney ME. The risk of teenage pregnancy among transitioning foster youth: Implications for extending state care beyond age 18. Children and Youth Services Review 2010;32:1351–1356. [Google Scholar]
- [7].Kushel MB, Yen IH, Gee L, et al. Homelessness and health care access after emancipation: results from the Midwest Evaluation of Adult Functioning of Former Foster Youth. Archives of Pediatrics and Adolescent Medicine 2007;161:986–993. [DOI] [PubMed] [Google Scholar]
- [8].Turner RJ, Thomas CS, Brown TH. Childhood adversity and adult health: Evaluating intervening mechanisms. Soc Sci Med 2016;156:114–124. [DOI] [PubMed] [Google Scholar]
- [9].Shonkoff JP, Garner AS, Siegel BS, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129:e232–e246. [DOI] [PubMed] [Google Scholar]
- [10].Slopen N, Non A, Williams DR, et al. Childhood adversity, adult neighborhood context, and cumulative biological risk for chronic diseases in adulthood. Psychosom Med 2014;76:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].P.L. 110-351. Fostering Connections to Success and Increasing Adoptions Act of 2008. 2008. [Google Scholar]
- [12].Patient Protection and Affordable Care Act PLN-, §2702, 124 Stat. 119, 318-319 Patient Protection and Affordable Care Act, Pub. L. No. 111-148, §2702, 124 Stat. 119, 318–319. 2010. [Google Scholar]
- [13].Council On Foster Care A, Kinship C, Committee On Early C. Health care of youth aging out of foster care. Pediatrics 2012;130:1170–1173. [DOI] [PubMed] [Google Scholar]
- [14].Lopez P, Allen PJ. Addressing the health needs of adolescents transitioning out of foster care. Pediatr Nurs 2007;33:345–355. [PubMed] [Google Scholar]
- [15].Crowley R, Wolfe I, Lock K, et al. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548–553. [DOI] [PubMed] [Google Scholar]
- [16].Blum RWM, Garell D, Hodgman CH, et al. Transition from child-centered to adult health care systems for adolescents with chronic conditions: A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health 1993;14:570–576. [DOI] [PubMed] [Google Scholar]
- [17].Okumura MJ, Hersh AO, Hilton JF, et al. Change in health status and access to care in young adults with special health care needs: results from the 2007 national survey of adult transition and health. J Adolesc Health 2013;52:413–418. [DOI] [PubMed] [Google Scholar]
- [18].Cuomo C, Rome ES. Translation of the six core elements of healthcare transition: A primary care approach. Journal of Adolescent Health 2017;60:S77–S78. [Google Scholar]
- [19].Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2011;128:182–200. [DOI] [PubMed] [Google Scholar]
- [20].Yen IH, Hammond WP, Kushel MB. From homeless to hopeless and healthless?: the health impacts of housing challenges among former foster care youth transitioning to adulthood in California. Issues Compr Pediatr Nurs 2009;32:77–93. [DOI] [PubMed] [Google Scholar]
- [21].Council On Foster C, Adoption, Kinship C, et al. Health Care Issues for Children and Adolescents in Foster Care and Kinship Care. Pediatrics 2015;136:e1131–1140. [DOI] [PubMed] [Google Scholar]
- [22].Greiner MV, Beal SJ. Developing a Health Care System for Children in Foster Care. Health promotion practice 2017:1524839917730045. [DOI] [PubMed] [Google Scholar]
- [23].Greiner MV, Ross J, Brown CM, et al. Foster caregivers’ perspectives on the medical challenges of children placed in their care: implications for pediatricians caring for children in foster care. Clin Pediatr (Phila) 2015;54:853–861. [DOI] [PubMed] [Google Scholar]
- [24].Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ—Transition Readiness Assessment Questionnaire. J Pediatr Psychol 2011;36:160–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Neelon B, O’Malley AJ, Smith VA. Modeling zero-modified count and semicontinuous data in health services research Part 1: background and overview. Stat Med 2016;35:5070–5093. [DOI] [PubMed] [Google Scholar]
- [26].Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics 2000;106:909–918. [PubMed] [Google Scholar]
- [27].Boonstra HD. Teen pregnancy among young women in foster care: A primer. Guttmacher Policy Review 2011;14:8–19. [Google Scholar]
- [28].Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank quarterly 2005;83:457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Cooley WC, McAllister JW, Kuhlthau P. Improved outcomes associated with medical home implementation in pediatric primary care. peds; 2009; 2009. 124. [DOI] [PubMed] [Google Scholar]
- [30].White PH, Cooley WC, Pediatrics Aao, et al. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2018;142:e20182587. [DOI] [PubMed] [Google Scholar]
- [31].Gonzales A. The contemporary US digital divide: from initial access to technology maintenance. Information, Communication & Society 2016;19:234–248. [Google Scholar]
- [32].Coates C, Meisman A, Gordon C, et al. 112. Evaluation of A Health Education Module About Accessing Community Based Healthcare Services For Youth In A Juvenile Detention Facility. Journal of Adolescent Health 2019;64:S58–S59. [Google Scholar]
- [33].Turney K, Wildeman C. Mental and physical health of children in foster care. Pediatrics 2016;138:e20161118. [DOI] [PubMed] [Google Scholar]
- [34].Szilagyi MA, Rosen DS, Rubin D, et al. Health care issues for children and adolescents in foster care and kinship care. Pediatrics 2015;136:e1142–e1166. [DOI] [PubMed] [Google Scholar]
- [35].Beal SJ, Nause K, Crosby I, et al. Understanding health risks for adolescents in protective custody. The journal of applied research on children: informing policy for children at risk 2018;9. [PMC free article] [PubMed] [Google Scholar]
- [36].Ahrens KR, McCarty C, Simoni J, et al. Psychosocial pathways to sexually transmitted infection risk among youth transitioning out of foster care: evidence from a longitudinal cohort study. J Adolesc Health 2013;53:478–485. [DOI] [PMC free article] [PubMed] [Google Scholar]


