Abstract
Purpose
A minority of young, gay, bisexual and other men who have sex with men (YGBMSM) living with HIV in the United States achieve viral suppression, thus increasing the likelihood of viral transmission during condomless anal intercourse (CAI). The purpose of this study was to explore potential risk factors for CAI and serodiscordant CAI among YGBMSM with detectable viremia.
Methods
146 YGBMSM (age 16–24) with a detectable viremia enrolled into an mHealth adherence intervention. Baseline characteristics, stratified by any CAI and any serodiscordant CAI (past 3 months), were computed. Random Forests (RF) and regression methods were used to assess factors associated with each type of CAI. Adjusted prevalence rate ratios (aPRR) and 95% confidence intervals were calculated.
Results
Half (51.9%) reported engaging in CAI; 57.1% of those reported serodiscordant CAI (SD-CAI). There was strong agreement between the RF and regression methods. Significant risk factors of CAI included marijuana use (aPRR=1.97, 95% CI: 1.21 – 3.21), problematic substance use (aPRR=1.56, 95% CI: 1.11 – 2.20) and being in a committed relationship (aPRR=1.66, 95% CI: 1.21 – 2.27). Only 47% believed they were less likely to transmit HIV through CAI when virally suppressed.
Conclusion
High rates of CAI, including engagement in SD-CAI in a population of YGBMSM with detectable viral loads poses significant concerns for onward transmission. Individual, dyadic and structural predictors of CAI were associated with engagement in risk in this priority population. Addressing these factors in concert with ensuring viral suppression will be key to ending the epidemic among youth.
Keywords: viral load, sexual risk, condomless sex, adolescents, young adults, HIV
Introduction
Despite a slight decline in HIV incidence from 2010 to 2016, youth (aged 13 to 24) in the United States (US) still bear a disproportionate burden (1). In 2017, youth made up 21% of all new HIV diagnoses; 87% of those were among men, most (93%) of whom were young, gay, bisexual and other men who have sex with men (YGBMSM) (1). Youth experience worse outcomes along all stages of the care continuum, most significantly, having the lowest rates of viral suppression among all age groups (1). A review of US studies, conducted between 2000–2012, found that only 62% of youth (aged 13–29) with HIV engaged in medical care within 12 months of diagnosis. Of those in care, only 43% are retained in care over 1–3 years, and among those who initiated antiretroviral therapy (ART), only 51% achieved viral suppression to less than 400 copies/ml (2). In a national study of 467 youth (aged 13–24) in care, while 77% were virally suppressed at baseline, only 59% of those initially virally suppressed maintained suppression at all follow-up points over 12 months (3).
Many youth living with HIV (YLHIV) continue to engage in condomless sex after diagnosis, including a large proportion of youth with detectable viremia (4, 5). Among 200 YGBMSM (ages 16–24 years) living with HIV recruited from 14 clinical sites, 20.5–22.5% reported condomless anal intercourse (CAI) across partner serostatus (HIV-negative/status unknown or HIV-positive) and type of CAI (receptive or insertive) (6). Among 991 YGBMSM (aged 13–24 years) in a national clinic-based sample, 688 (69.4%) had detectable viremia and 458 (46.2%) reported CAI, with 310 (31.3%) reporting serodiscordant (SD-CAI) in the past 3 months (4). Those YGBMSM with detectable viremia were more likely than those who were virally suppressed to report CAI and SD-CAI (5). Incident sexually transmitted infections (STIs) are also associated with worse viral suppression among YLHIV (7).
While there has been limited research on correlates of CAI and SD-CAI among YGBMSM living with HIV with detectable viral loads (5, 8), data from the national clinic-based sample described above identified an association between problematic substance use, greater depressive symptoms, and receiving an HIV diagnosis in the past 6 months with engagement in CAI (5). Given the high HIV transmission rates attributable to CAI among persons who are aware of their status with unsuppressed viral loads (9), and the importance of addressing the HIV epidemic among YGBMSM, the current study aims to provide a more nuanced analysis of factors associated with CAI among virologically detectable YGBMSM using multiple variable selection methods.
METHODS
Design
From October 2015 to September 2016, 146 YGBMSM living with HIV (age 16–24) were recruited into a two-arm, randomized intervention trial, Epic Allies, to test the acceptability, impact, and long-term sustainability of the Epic Allies mobile phone application (app) intervention (10). Epic Allies is a theory-based mobile app that utilizes game mechanics and social networking features to improve engagement in care, ART uptake, adherence, and viral suppression (11). Study participants were required to have a detectable viral load, defined as a viral load greater that the lower limit of detection (LLD) for the assay used. Participants were recruited from four sites within the Adolescent Trials Network for HIV Interventions (ATN) system of care; University of South Florida (Tampa, FL), Montefiore (Bronx, NY), Stroger/CORE Center (Chicago, IL), and Tulane (New Orleans, LA). A fifth (non-ATN) site, UNC Chapel Hill (Chapel Hill, NC) was also included. Chart abstraction and medical record review was completed for viral load data. Participants completed computer-assisted self-interview (CASI) surveys at baseline (prior to randomization), 13, 26 and 39 weeks (10). Baseline data were used for the analyses described below.
Primary ethical review of the study was completed by UNC Institutional Review Board. The trial is registered with clinicaltrials.gov under protocol number: NCT02782130.
Measures
Sociodemographic items included gender, sexual identity, race/ethnicity, relationship status, education, employment status, income (past 30 days), homelessness (past 3 months) and incarceration (lifetime). Participants were classified as either new-to-care (initiation of HIV treatment within the past 12 months) or non-adherent to ART (first entered HIV care more than 12 months prior to the baseline visit).
Sexual Risk
Each participant was asked separately how many times in the past 3 months they had insertive and receptive CAI with HIV-positive, HIV-negative, and status unknown male partners. Serodiscordant CAI was defined as any CAI in which the partner(s) was HIV-negative or of unknown HIV status.
Mental Health
Depressive symptoms were assessed using the validated 20-item Center for Epidemiologic Studies Depression Scale (CES-D) with scores ranging from 0 to 60. A dichotomous variable was created using a cutoff score of ≥ 16 which suggests clinically relevant depressive symptoms (12). Generalized anxiety was measured using the validated 7-item Generalized Anxiety Disorder (GAD-7) scale (range 0–21) (13). A dichotomous variable was created using a cutoff of ≥ 10 which represents moderate to severe anxiety.
Substance Use
Patterns of substance use were established using items from the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) (14). Of interest to this study was lifetime use of alcohol, marijuana, cocaine, amphetamines or opioids and the frequency of alcohol and marijuana use in the last 3 months. ASSIST frequency categories were collapsed into two categories: irregular use (never, once or twice, monthly or weekly), and regular use (daily or almost daily). The 6-item Car, Relax, Alone, Forget, Friends, Trouble (CRAFFT), which measures consequences of alcohol and/or drug use among youth, was used to identify problematic substance use which was defined as endorsement of 2 or more of the 6 items (15).
Social Media Use
Participants were asked about their number of social media site accounts and past-month frequency of use. Frequency of account use was collapsed into categories of daily (once to several time per day), weekly (1 to 6 times per week), and less than weekly (less than once per week or not at all). Participants were also asked if they used the internet to search for sex partners in the last 3 months and frequency. Frequency was collapsed as described for social media.
HIV Transmission Beliefs
Attitudinal variables assessed participant beliefs regarding infectiousness and viral load (3 questions), serosorting (3 questions), and sexual positioning (1 question) using a 4-point response scale (1=strongly agree to 4=strongly disagree). An example of a viral load belief item is: “If my viral load is low or undetectable, I am less likely to infect another person with HIV if I have unprotected sex.” An example of a serosorting belief item is: “I am less concerned about using condoms with a partner who is also HIV positive.” One item: “I will have oral sex with a partner instead of either vaginal or anal sex in order to reduce the risk of infecting another person with HIV” assessed sexual positioning beliefs. All answers were dichotomized into agreement versus disagreement.
Stigma
HIV Stigma was measured using an abbreviated (10-item) scale designed for YLHIV (16) with a 5-point Likert response (1= strongly disagree to 5= strongly agree). An example item includes: “I have lost friends by telling them I have HIV.” HIV stigma was analyzed continuously (score range 10–50) with higher scores indicating more stigma.
Internalized homophobia was assessed using the Internalized Homophobia Scale-Revised (HIS-R) (17). The 5-item scale uses a 5-point Likert response (1= strongly disagree to 5= strongly agree). An example item includes, “I feel that being gay/bisexual is a personal shortcoming for me.” The upper two categories (4 and 5) were combined due to sparsity.
Perceived homophobia was quantified using the binary answer (1= agree, 2= disagree) to the question, “In the last 12 months, I have perceived a rise in homophobia/transphobia”.
Statistical Analysis
Descriptive statistics, stratified by the binary CAI behaviors of any CAI and any SD-CAI were computed, with frequency counts and percentages used for categorical variables and medians with interquartile ranges used for continuous variables. For continuous covariates, either previously validated, clinically meaningful ranges were used for values as transformed categorical variables (e.g. depression and anxiety scores), or the data were fitted via loess curves and regression fit statistics to determine if other forms of the variable, such as quadratic, log transformation, or meaningful cut offs improved the fit of the regressions.
Random Forests (RF) methods were used to determine which of the chosen covariates were most important in predicting each type of CAI behavior (18). RF is a non-parametric, data-driven analysis that can be used for prediction, ranking variables and for variable selection, without having to make a priori assumptions about the structure of data or the relationship between the response (dependent) and predictor (independent) variables (19). Individual regression trees are constructed via binary splits in numeric predictor variables. The dataset is split into subsets that are increasingly homogeneous with regard to the response variable to form regression “trees.” The process is repeated recursively until a stopping criterion is met. To construct trees, bootstrap samples of the original data are taken repeatedly and conditional inference trees produced for each subset, in a process called bagging. A random subset of predictor variables is taken repeatedly so that one or a few variables are not able to dominate all trees. Results are summarized over all trees to provide overall inference. We used 500 trees in the bagging process, sub-selected 5 variables at a time for our regression trees, and specified nodes with fewer than five observations as a stopping criterion (18).
The relevance of each of the predictor variables in the RF was summarized by calculating the variable permutation accuracy importance (18). Any variable that had a permutation importance score greater than the absolute value of the lowest score was considered to be “important” in predicting CAI. Positive values exceeding this range are more likely to indicate a non-arbitrary level of importance in predicting the outcome (18). Each variable’s importance generated from the RF was then summarized graphically with corresponding permutation scores to provide a visual “ranking” of importance within the regression tree models. Because RF is primarily designed to optimize prediction, we computed measures of predictive accuracy by calculating the area under the curve (AUC) for each set of variables on each outcome. All RF methods were performed using the party package in R version 3.4.1 (20).
To complement the RF analysis, parametric adjusted Modified Poisson regressions were used to identify associations and to quantify the magnitude and direction of adjusted effects for each covariate on each outcome. First, regressions were run separately for each covariate that was included in RF and each regression adjusted for study site in order to ascertain a list of covariates that independently predicted CAI outcomes. Second, in order to estimate a more valid prevalence rate ratio (PRR), regressions were again run separately for each covariate of interest and adjusted for known predictors of CAI (age, ethnicity, and relationship status). All regression analyses were performed using SAS software version 9.4.
RESULTS
Sample Characteristics
Descriptive statistics stratified by CAI and SD-CAI are presented in Table 1. At baseline, 134 (91.8%) participants provided CAI information (University of South Florida (n=25), Montefiore (n=29), Stroger/CORE Center (n=21), Tulane (n=24) and UNC Chapel Hill (n=35). The sample was primarily male (94%) and gay-identified (76%). Most participants (82%) were African American; 19% identified as Hispanic or Latino. Less than half (37%) reported being in a committed relationship and 81% had at least a high school/GED level education. A majority of participants were currently employed (67%) and reported making less than $12,000/year (73%). A quarter of the sample (28%) reported homelessness for one night or more in the last 90 days and a similar number (27%) reported having ever been incarcerated.
Table 1.
Sample characteristics of YGBMSM1 (n=134) overall and by differences in sexual risk behavior.
| Type of CAI Behavior | |||||
|---|---|---|---|---|---|
| Total (N=134) | Any CAI2 | Serodiscordant CAI | |||
| Variable | No (N=64) | Yes (N=70) | No (N=94) | Yes (N=40) | |
| Demographics | |||||
| Age, Median (IQR) | 22 (20, 23) | 21 (20, 23) | 22 (20, 23) | 22.0 (20, 23) | 22 (20, 23) |
| Current Gender Identity | |||||
| Male | 126 (94%) | 59 (92%) | 67 (96%) | 89 (95%) | 37 (93%) |
| Female, transgender female, other | 8 (6%) | 5 (8%) | 3 (4%) | 5 (5%) | 3 (7%) |
| Sexual Identity | |||||
| Gay | 102 (76%) | 45 (70%) | 57 (81%) | 70 (74%) | 32 (80%) |
| Bisexual | 26 (19%) | 14 (22%) | 12 (17%) | 18 (19%) | 8 (20%) |
| Other | 6 (4%) | 5 (8%) | 1 (1%) | 6 (6%) | 0 (0%) |
| Hispanic/Latino | 26 (19%) | 9 (14%) | 17 (24%) | 12 (13%) | 14 (35%) |
| Racial Identification | |||||
| White | 8 (6%) | 4 (7%) | 4 (6%) | 6 (7%) | 2 (6%) |
| African American/Black | 102 (82%) | 52 (85%) | 50 (79%) | 76 (84%) | 26 (79%) |
| Other | 14 (11%) | 5 (8%) | 9 (14%) | 9 (10%) | 5 (15%) |
| In a committed relationship | 50 (37%) | 15 (23%) | 35 (50%) | 35 (37%) | 15 (38%) |
| Highest Education | |||||
| < 12th grade | 25 (19%) | 14 (22%) | 11 (16%) | 20 (21%) | 5 (13%) |
| Completed high school/GED, some technical/college | 97 (72%) | 46 (72%) | 51 (73%) | 67 (71%) | 30 (75%) |
| College/technical degree or more | 12 (9%) | 4 (6%) | 8 (11%) | 7 (7%) | 5 (13%) |
| Economic | |||||
| Currently employed | 90 (67%) | 44 (69%) | 46 (66%) | 62 (66%) | 28 (70%) |
| Approximate yearly income | |||||
| < $11,999 | 98 (73%) | 46 (72%) | 52 (74%) | 70 (74%) | 28 (70%) |
| $12,000+ | 23 (17%) | 9 (14%) | 14 (20%) | 14 (15%) | 9 (23%) |
| Don’t know/Refuse | 13 (10%) | 9 (14%) | 4 (6%) | 10 (11%) | 3 (8%) |
| Life Stressors | |||||
| Homeless for one night or more (3 mo.) | 38 (28%) | 17 (27%) | 21 (30%) | 27 (29%) | 11 (28%) |
| Ever incarcerated | 36 (27%) | 17 (27%) | 19 (27%) | 29 (31%) | 7 (18%) |
|
Male Sex partners Median (IQR) |
1.0 (1.0, 3.0) | 0 (0.0, 1.0) | 2.0 (1.0, 4.0) | 1.0 (0.0, 2.0) | 3.0 (1.5, 5.0) |
| Social Media Use | |||||
| Number of social media accounts | |||||
| None | 9 (7%) | 5 (8%) | 4 (6%) | 7 (7%) | 2 (5%) |
| 1 to 3 | 48 (36%) | 24 (38%) | 24 (34%) | 37 (39%) | 11 (28%) |
| 4 to 6 | 66 (49%) | 31 (48%) | 35 (50%) | 43 (46%) | 23 (58%) |
| 7 to 9 | 11 (8%) | 4 (6%) | 7 (10%) | 7 (7%) | 4 (10%) |
| Frequency of visit to social media accounts (3 mo.) | |||||
| Less than weekly | 11 (8%) | 7 (11%) | 4 (6%) | 9 (10%) | 2 (5%) |
| Weekly | 12 (9%) | 3 (5%) | 9 (13%) | 7 (7%) | 5 (13%) |
| Daily | 111 (83%) | 54 (84%) | 57 (81%) | 78 (83%) | 33 (83%) |
| Used internet to search for a sex partner (3 mo.) | 55 (41%) | 19 (30%) | 36 (51%) | 30 (32%) | 25 (63%) |
| How often looked online for sex partner | |||||
| Less than weekly | 104 (78%) | 54 (84%) | 50 (72%) | 79 (84%) | 25 (64%) |
| Weekly | 15 (11%) | 6 (9%) | 9 (13%) | 9 (10%) | 6 (15%) |
| Daily | 14 (11%) | 4 (6%) | 10 (14%) | 6 (6%) | 8 (21%) |
| Mental Health | |||||
| Depressive symptoms | 76 (57%) | 36 (56%) | 40 (57%) | 50 (53%) | 26 (65%) |
| Moderate/Severe Anxiety | 38 (28%) | 15 (23%) | 23 (33%) | 25 (27%) | 13 (33%) |
| Substance Use | |||||
| Problematic substance use | 69 (52%) | 24 (39%) | 45 (64%) | 38 (41%) | 31 (78%) |
| Ever used alcohol | 116 (87%) | 52 (83%) | 64 (91%) | 80 (86%) | 36 (90%) |
| Alcohol daily/almost daily | 9 (7%) | 4 (6%) | 5 (7%) | 6 (6%) | 3 (8%) |
| Ever used marijuana | 97 (73%) | 38 (60%) | 59 (84%) | 63 (68%) | 34 (85%) |
| Marijuana daily/almost daily | 46 (35%) | 19 (30%) | 27 (39%) | 33 (35%) | 13 (33%) |
| Ever used Cocaine/ Amphetamines/Opioids | 23 (17%) | 7 (11%) | 16 (23%) | 14 (15%) | 9 (23%) |
| HIV Health and Medication Adherence | |||||
| Non-adherent | 68 (51%) | 34 (53%) | 34 (49%) | 50 (53%) | 18 (45%) |
| New-to-care | 66 (49%) | 30 (47%) | 36 (51%) | 44 (47%) | 22 (55%) |
| HIV Transmission Beliefs | |||||
| If VL3 is low/undetectable I’m less likely to infect someone w/ HIV | 62 (48%) | 25 (41%) | 37 (54%) | 40 (44%) | 22 (56%) |
| I practice safer sex less often because new medical treatments for HIV/AIDS have come along | 55 (42%) | 23 (38%) | 32 (46%) | 40 (44%) | 15 (38%) |
| I am less concerned about using condoms w/ a partner who is also HIV+ | 31 (24%) | 10 (16%) | 21 (30%) | 22 (24%) | 9 (23%) |
| I am more concerned about using condoms with HIV− or unknown status partners when VL is detectable | 92 (71%) | 43 (70%) | 49 (71%) | 62 (68%) | 30 (77%) |
| A partner who doesn’t seem interested in using condoms is probably also HIV+ | 53 (41%) | 20 (33%) | 33 (48%) | 37 (41%) | 16 (41%) |
| I look for other HIV+ people to have sex with | 26 (20%) | 7 (11%) | 19 (28%) | 19 (21%) | 7 (18%) |
| I will have oral sex w/ /partner to reduce risk of infecting someone | 40 (31 %) | 16 (26%) | 24 (35%) | 25 (27%) | 15 (39%) |
| Stigma | |||||
| HIV Stigma Median (IQR) | 21 (16.0, 28.0) | 20 (14, 27) | 22 (17, 28) | 20 (14, 25) | 23 (18, 30) |
| Internalized Homophobia Scale | |||||
| 1 | 54 (40%) | 28 (44%) | 26 (37%) | 42 (45%) | 12 (30%) |
| 2 | 29 (22%) | 11 (17%) | 18 (26%) | 17 (18%) | 12 (30%) |
| 3 | 33 (25%) | 21 (33%) | 12 (17%) | 27 (29%) | 6 (15%) |
| 4 or 5 | 18 (13%) | 4 (6%) | 14 (20%) | 8 (9%) | 10 (25%) |
| Perceived a rise in homophobia/transphobia (12 mo.) | 46 (34%) | 17 (27%) | 29 (41%) | 25 (27%) | 21 (53%) |
Young gay, bisexual or other men who have sex with men
Condomless anal intercourse
Viral load
Participants reported a high level of depressive symptoms, with 57% meeting the criteria for being at risk of depression. Fewer participants met criteria for moderate to severe anxiety (28%). More than half of the sample (52%) screened positive for problematic substance use. Few (7%) reported daily alcohol use, while a third (35%) reported daily marijuana use.
Standardized Cronbach’s alpha computed on scales used in analysis sample indicate a sufficient level of reliability for the CES-D (α=0.891), GAD (α=0.938), CRAFFT (α= 0.778), Felt Stigma (α= 0.866), and internalized homophobia (α=0.906).
Condomless Anal Intercourse
Participants reported a median of 1.0 (IQR 1.0, 3.0) male sex partner in the past 3 months. Half (52.2%, n=70) of the participants reported engaging in any type of CAI in the last 3 months; of those 71.4% reported any insertive CAI and 90.0% any receptive CAI. Of those reporting any CAI, 57.1% (n=40) reported having CAI with someone whose HIV status was either negative or unknown. Of those who had SD-CAI, 60% reported insertive and 85% reported receptive CAI.
Predictors of any CAI behavior
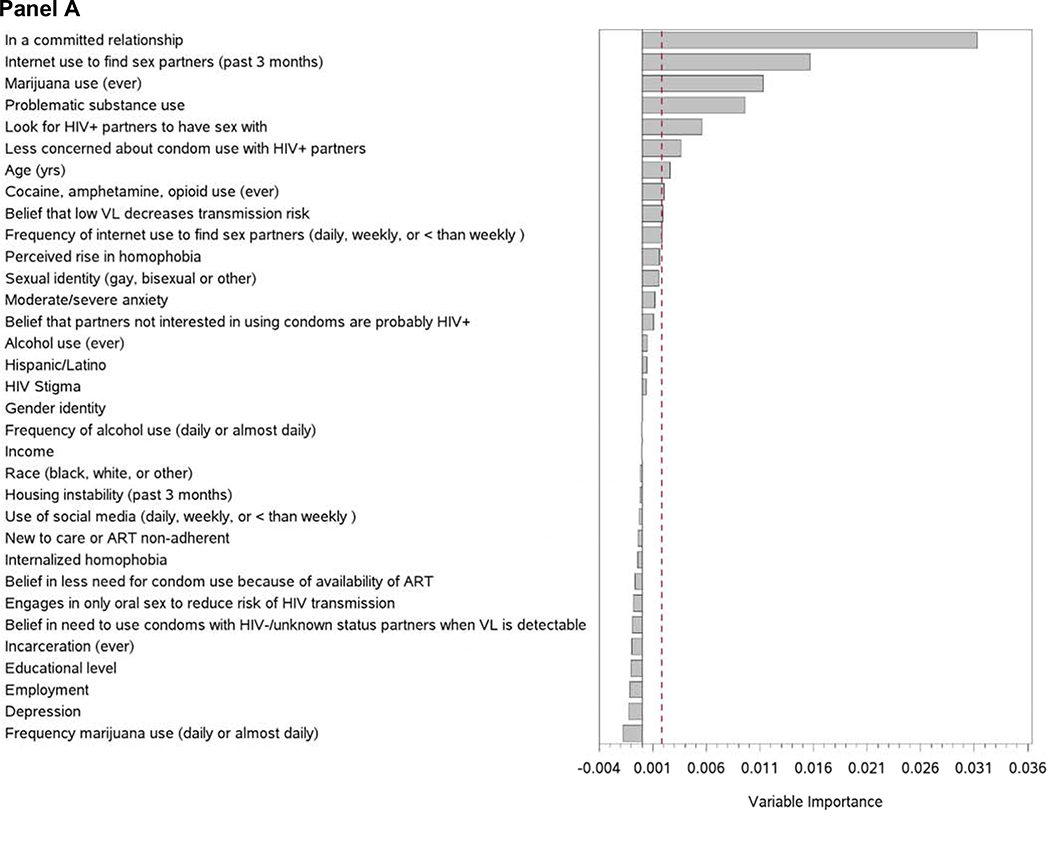
There was strong agreement between the RF and regression methods. Nearly all variables found to be important in predicting CAI using RF methods were also identified in regression analysis. Analysis of AUC, revealed an excellent level of discrimination for models of any CAI (AUC=0.82, 95% CI: 0.76 – 0.89), acceptable discrimination for insertive (AUC=0.71, 95% CI: 0.64 – 0.78) and receptive CAI (AUC=0.79, 95% CI: 0.72 – 0.86), and less discriminatory for serodiscordant CAI (AUC=0.65, 95% CI: 0.58 – 0.72) (Supplemental Table 1). Relationship status was the most important predictor of engaging in any CAI according to the variable selection process using RF methods (Figure 1, Panel A), with those in a committed relationship being more likely to have any CAI (Adjusted PRR=1.66, 95% CI: 1.21 – 2.27) (Supplemental Table 2). Substance use was an important RF predictor (Table 2) with those reporting ever having used marijuana almost twice as likely (PRR=1.97, 95% CI: 1.21 – 3.21) and those with problematic substance use more likely (PRR=1.56, 95%CI: 1.11 – 2.20) to report engaging in any CAI. Those who looked for sex partners online were also more likely to report any CAI (PRR=1.77, 95% CI: 1.28 – 2.47). Individuals engaging in CAI were also more likely to have reported looking for other HIV-positive individuals to have sex with (PRR=1.63; 95% CI: 1.21 – 2.19). In the crude regression analysis, individuals engaging in any CAI were less concerned about safety with HIV-positive partners, and changed very little when adjustment was made for known risk factors of CAI (PRR=1.36; 95%CI: 0.98 – 1.87). Belief that a low viral load decreased the risk of infecting a partner was an important predictor of any CAI in the RF analysis; however, there was not strong evidence for this association from the regression analysis.
Figure 1.
Random Forest Variable Importance for Predictors of Any CAI (Panel A) and Serodiscordant CAI (Panel B). Dotted line at absolute value of minimum variable importance score.
Table 2.
Characteristics associated with prevalence of any CAI and any serodiscordant CAI among YGBMSM
| Type of CAI Behavior | |||||
|---|---|---|---|---|---|
| Any CAI | Serodiscordant CAI | ||||
| Variable | Level | Estimate (95% CI) | P-value | Estimate (95% CI) | P-value |
| Demographics | |||||
| Age (years) | - | 1.08 (1.00,1.18) | .065 | 1.08 (0.94,1.25) | .256 |
| Current Gender Identity (ref: Male) |
Female, trans female | 0.55 (0.18,1.71) | .304 | 0.94 (0.30,2.95) | .922 |
| Other | 0.88 (0.15,5.14) | .889 | 1.55 (0.22,10.7) | .657 | |
| Sexual Identity (ref: Gay) |
Bisexual | 0.27 (0.05,1.50) | .134 | ||
| Other | 0.86 (0.56,1.33) | .499 | |||
| Hispanic/Latino | Yes | 1.24 (0.87,1.77) | .227 | 2.07 (1.23,3.49) | .006 |
| Racial Identification (ref: White) |
African American/Black | 1.20 (0.56,2.59) | .637 | 1.32 (0.33,5.29) | .691 |
| Other | 0.83 (0.41,1.67) | .593 | 0.85 (0.23,3.06) | .801 | |
| In a committed relationship | Yes | 1.61 (1.18,2.20) | .003 | 0.94 (0.55,1.61) | .832 |
| Highest Education (ref: < 12th grade) |
Completed high school/GED, some technical/college | 1.17 (0.73,1.89) | .510 | 1.47 (0.62,3.45) | .382 |
| College/technical degree or more | 1.55 (0.85,2.81) | .152 | 2.10 (0.76,5.81) | .152 | |
| Economic | |||||
| Currently employed | Yes | 1.17 (0.73,1.89) | .510 | 1.47 (0.62,3.45) | .382 |
| Yearly income (ref: <$11,999) |
$12,000+ | 1.15 (0.78,1.69) | .474 | 1.38 (0.78,2.44) | .269 |
| Don’t know/Refuse | 0.57 (0.24,1.35) | .199 | 0.78 (0.27,2.22) | .637 | |
| Life Stressors | |||||
| Homeless for one night or more (3 mo.) | Yes | 1.11 (0.78,1.57) | .559 | 0.99 (0.55,1.78) | .965 |
| Ever been incarcerated? | Yes | 1.06 (0.73,1.53) | .755 | 0.58 (0.28,1.20) | .143 |
| Social Media Use | |||||
| Number of social media accounts (ref: none) |
1–3 | 1.17 (0.53,2.58) | .696 | 1.03 (0.27,3.92) | .962 |
| 4–6 | 1.23 (0.57,2.65) | .595 | 1.58 (0.45,5.53) | .478 | |
| 7–9 | 1.45 (0.59,3.54) | .420 | 1.57 (0.34,7.27) | .561 | |
| Frequency of visit to social media accounts (in last month) (ref: less than weekly) |
Weekly | 2.10 (0.92,4.83) | .079 | 2.28 (0.56,9.24) | .248 |
| Daily | 1.43 (0.64,3.15) | .381 | 1.60 (0.45,5.66) | .465 | |
| Used internet to search for a sex partner (3 mo)? | Yes | 1.49 (1.08,2.06) | .016 | 2.30 (1.35,3.91) | .002 |
| Frequency going online for sex partners (past month)? (ref: less than weekly) |
Weekly | 1.23 (0.78,1.96) | .375 | 1.62 (0.79,3.30) | .186 |
| Daily | 1.39 (0.93,2.08) | .106 | 2.16 (1.20,3.90) | .011 | |
| Mental Health | |||||
| Depressed | Yes | 2.10 (0.92,4.83) | .079 | 2.28 (0.56,9.24) | .248 |
| Moderate/Severe Anxiety | Yes | 1.43 (0.64,3.15) | .381 | 1.60 (0.45,5.66) | .465 |
| Substance Use | |||||
| Problematic Substance Use | Yes | 1.60 (1.12,2.29) | .009 | 3.13 (1.62,6.07) | .001 |
| Ever used alcohol | Yes | 1.51 (0.80,2.85) | .202 | 1.23 (0.52,2.93) | .636 |
| Alcohol daily/almost daily | Yes | 1.27 (0.68,2.40) | .452 | 1.43 (0.52,3.95) | .488 |
| Ever used marijuana | Yes | 1.92 (1.16,3.18) | .011 | 2.00 (0.92,4.35) | .081 |
| Marijuana daily/almost daily | Yes | 1.15 (0.83,1.58) | .395 | 0.86 (0.50,1.50) | .597 |
| Ever used Cocaine/Amphetamines/Opioids | Yes | 1.46 (1.03,2.07) | .035 | 1.42 (0.76,2.65) | .269 |
| HIV Health and Medication Adherence | |||||
| New-to-care vs. Non-adherent | New-to-care | 1.21 (0.87,1.70) | .257 | 1.54 (0.89,2.67) | .123 |
| HIV Transmission Beliefs | |||||
| If VL is low/undetectable I’m less likely to infect someone w/ HIV | Yes | 1.22 (0.89,1.69) | .219 | 1.33 (0.78,2.27) | .296 |
| I practice safer sex less often because new medical treatments for HIV/AIDS have come along | Yes | 1.18 (0.86,1.62) | .314 | 0.85 (0.50,1.43) | .533 |
| I am less concerned about using condoms w/ a partner who is also HIV+ | Yes | 1.38 (1.00,1.91) | .047 | 0.96 (0.50,1.84) | .899 |
| I am more concerned about using condoms with HIV− or unknown status partners when VL is detectable | Yes | 1.03 (0.73,1.46) | .865 | 1.40 (0.75,2.64) | .293 |
| A partner who doesn’t seem interested in using condoms is probably also HIV+ | Yes | 1.33 (0.97,1.83) | .078 | 0.98 (0.58,1.66) | .953 |
| I look for other HIV+ people to have sex with | Yes | 1.55 (1.14,2.10) | .005 | 0.91 (0.46,1.83) | .796 |
| I will have oral sex w/ /partner to reduce risk of infecting someone | Yes | 1.16 (0.83,1.62) | .386 | 1.37 (0.79,2.39) | .257 |
| Stigma | |||||
| Internalized Homophobia | 2 | 1.27 (0.83,1.92) | .269 | 1.77 (0.91,3.45) | .093 |
| 3 | 0.77 (0.46,1.30) | .327 | 0.83 (0.35,1.98) | .679 | |
| 4+ | 1.55 (1.06,2.27) | .023 | 2.34 (1.21,4.51) | .012 | |
| Rise in homophobia/transphobia (12mo). | Agree | 1.28 (0.93,1.76) | .135 | 1.96 (1.16,3.33) | .012 |
| HIV Stigma (Range: 0–50) | -- | 1.01 (0.99,1.03) | .447 | 1.03 (1.00,1.06) | .048 |
All regressions adjusted for study site
Estimates found “important” by Random Forests analysis in bold
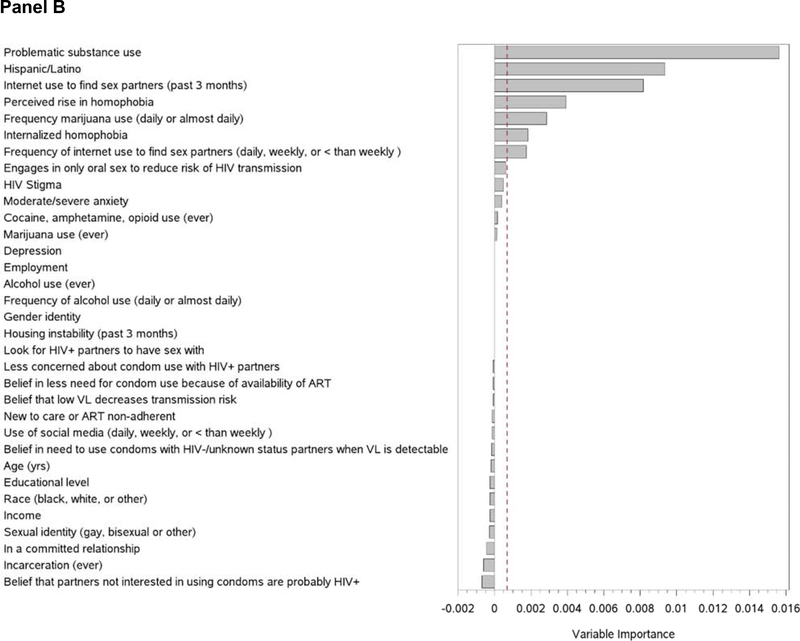
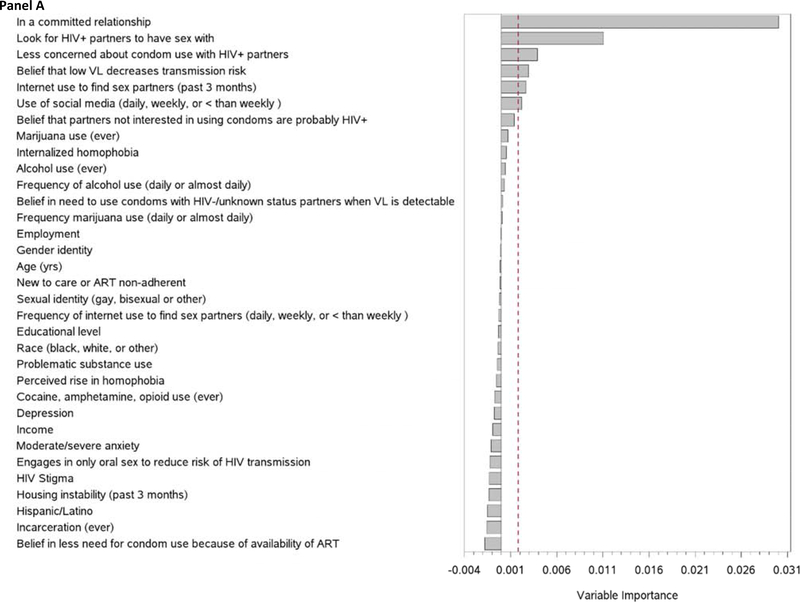
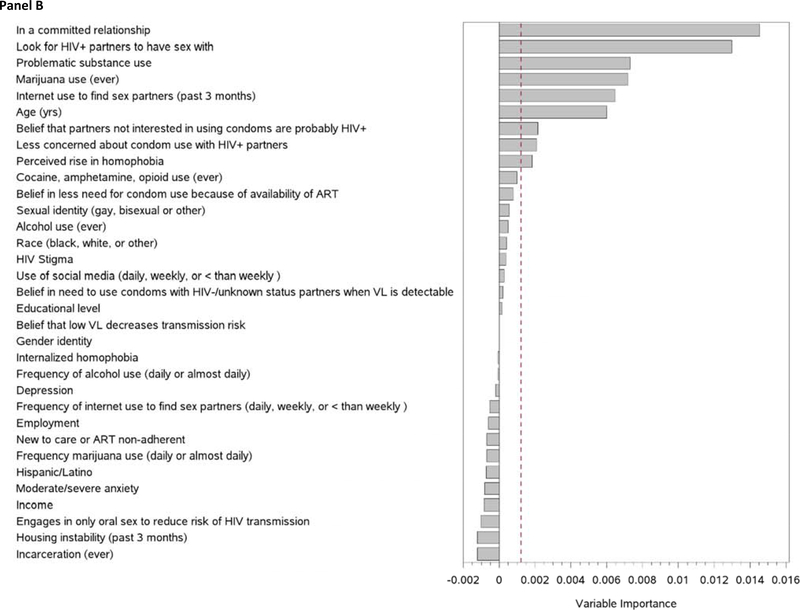
Predictors of Insertive and Receptive CAI
Both insertive and receptive CAI were most strongly associated with relationship status (Table 3, Figure 2, panels A and B), with the effect of being in a committed relationship more pronounced for insertive CAI (PRR=2.20, 95% CI: 1.40 – 3.47) versus receptive CAI (PRR=1.59, 95% CI: 1.12 – 2.26) (Supplemental Table 3). Problematic substance use (PRR=1.54, 95% CI: 1.05 – 2.28) and ever using marijuana (PRR 1.90, 95% CI: 1.11 – 3.26) were associated with higher prevalence of receptive, but not insertive CAI.
Table 3.
Characteristics associated with prevalence of insertive and receptive CAI among YGBMSM
| Any Insertive CAI | Any Receptive CAI | ||||
|---|---|---|---|---|---|
| Variable | Level | Estimate (95% CI) | P-value | Estimate (95% CI) | P-value |
| Demographics | |||||
| Age | 1.03 (0.92,1.14) | .636 | 1.11 (1.01,1.22) | .035 | |
| Current Gender Identity (ref: Male) |
Female, trans female | 0.95 (0.16,5.74) | .957 | ||
| Other | 0.60 (0.19,1.84) | .369 | |||
| Sexual Identity (ref: Gay) |
Bisexual | 0.96 (0.54,1.70) | .880 | 0.79 (0.47,1.31) | .360 |
| Other | 0.37 (0.07,2.15) | .270 | 0.28 (0.05,1.58) | .150 | |
| Hispanic/Latino | Yes | 0.98 (0.56,1.72) | .938 | 1.18 (0.78,1.78) | .425 |
| Racial Identification (ref: White) | African American/Black | 0.52 (0.20,1.38) | .188 | 1.15 (0.53,2.49) | .722 |
| Other | 0.57 (0.28,1.15) | .116 | 0.67 (0.33,1.35) | .262 | |
| In a committed relationship | Yes | 2.19 (1.39,3.44) | .001 | 1.55 (1.09,2.19) | .014 |
| Highest Education (ref: <12th grade) |
Completed high school/GED, some technical/college | 0.96 (0.54,1.72) | .898 | 1.10 (0.66,1.83) | .716 |
| College/technical degree or more | 1.19 (0.53,2.71) | .673 | 1.69 (0.90,3.17) | .099 | |
| Economic | |||||
| Currently employed | Yes | 0.81 (0.52,1.25) | .341 | 0.85 (0.59,1.22) | .375 |
| Yearly income (ref: <$11,999) |
$12,000+ | 0.95 (0.52,1.73) | .864 | 0.87 (0.53,1.45) | .602 |
| Don’t know/Refuse | 0.80 (0.33,1.95) | .628 | 0.60 (0.25,1.42) | .242 | |
| Life Stressors | |||||
| Homeless for one night or more (3 mo)? | Yes | 0.87 (0.52,1.46) | .595 | 1.12 (0.76,1.64) | .574 |
| Ever been incarcerated? | Yes | 1.03 (0.61,1.74) | .913 | 1.25 (0.85,1.83) | .251 |
| Social Media Use | |||||
| Number of social media accounts (ref: none) |
1–3 | 0.93 (0.41,2.07) | .850 | 1.41 (0.53,3.70) | .490 |
| 4–6 | 0.84 (0.38,1.85) | .668 | 1.44 (0.56,3.72) | .448 | |
| 7–9 | 0.79 (0.26,2.36) | .674 | 1.87 (0.65,5.42) | .249 | |
| Frequency of visit to social media accounts (in last month) (ref: less than weekly) |
Weekly | 2.14 (0.94,4.87) | .070 | 2.48 (0.89,6.87) | .081 |
| Daily | 0.95 (0.42,2.14) | .906 | 1.72 (0.66,4.51) | .268 | |
| Used internet to search for a sex partner (3 mo.)? | Yes | 1.22 (0.78,1.90) | .381 | 1.53 (1.07,2.19) | .021 |
| Frequency going online for sex partners (past month)? (ref: less than weekly) |
Weekly | 1.34 (0.72,2.50) | .351 | 1.21 (0.73,2.00) | .463 |
| Daily | 1.16 (0.61,2.20) | .656 | 1.37 (0.87,2.15) | .173 | |
| Mental Health | |||||
| Depressed | Yes | 0.98 (0.63,1.53) | .935 | 0.93 (0.64,1.34) | .690 |
| Moderate/Severe Anxiety | Yes | 1.15 (0.72,1.85) | .556 | 1.26 (0.88,1.80) | .212 |
| Substance Use | |||||
| Problematic Substance Use | Yes | 1.31 (0.82,2.07) | .257 | 1.54 (1.05,2.28) | .028 |
| Ever used alcohol | Yes | 1.60 (0.67,3.86) | .291 | 1.62 (0.80,3.28) | .183 |
| Alcohol daily/almost daily | Yes | 0.33 (0.05,2.06) | .235 | 1.47 (0.78,2.77) | .239 |
| Ever used marijuana | Yes | 1.45 (0.82,2.57) | .196 | 1.90 (1.11,3.26) | .020 |
| Marijuana daily/almost daily | Yes | 1.01 (0.64,1.59) | .977 | 1.27 (0.90,1.80) | .167 |
| Ever used Cocaine/ Amphetamines/Opioids | Yes | 0.91 (0.49,1.67) | .749 | 1.54 (1.04,2.28) | .031 |
| HIV Health and Medication Adherence | |||||
| New-to-care vs. Non-adherent | New-to-care | 1.31 (0.82,2.07) | .257 | 1.54 (1.05,2.28) | .028 |
| HIV Transmission Beliefs | |||||
| If VL is low/undetectable I’m less likely to infect someone w/ HIV | Yes | 1.53 (0.96,2.41) | .071 | 1.19 (0.83,1.70) | .353 |
| I practice safer sex less often because new medical treatments for HIV/AIDS have come along | Yes | 1.06 (0.68,1.66) | .789 | 1.36 (0.95,1.94) | .090 |
| I am less concerned about using condoms w/ a partner who is also HIV+ | Yes | 1.71 (1.10,2.64) | .017 | 1.42 (1.00,2.03) | .052 |
| I am more concerned about using condoms with HIV− or unknown status partners when VL is detectable | Yes | 0.96 (0.60,1.53) | .861 | 1.03 (0.70,1.51) | .891 |
| A partner who doesn’t seem interested in using condoms is probably also HIV+ | Yes | 1.59 (1.02,2.49) | .041 | 1.43 (1.00,2.03) | .048 |
| I look for other HIV+ people to have sex with | Yes | 2.00 (1.33,3.01) | .001 | 1.82 (1.32,2.52) | .000 |
| I will have oral sex w/ /partner to reduce risk of infecting someone | Yes | 1.33 (0.84,2.10) | .220 | 1.18 (0.82,1.70) | .375 |
| Stigma | |||||
| Internalized Homophobia | 2 | 0.97 (0.54,1.75) | .917 | 1.47 (0.94,2.30) | .094 |
| 3 | 0.81 (0.43,1.50) | .499 | 0.75 (0.41,1.36) | .339 | |
| 4+ | 1.23 (0.68,2.22) | .489 | 1.67 (1.10,2.55) | .017 | |
| Rise in homophobia/transphobia (12mo). | Agree | 1.11 (0.70,1.75) | .657 | 1.26 (0.88,1.80) | .209 |
| HIV Stigma (Range: 0–50) | -- | 1.01 (0.99,1.04) | .279 | 1.00 (0.98,1.02) | .938 |
All regressions adjusted for study site
Estimates found “important” by Random Forests analysis in bold
Figure 2.
Random Forest Variable Importance for Predictors of Any Insertive Condomless Anal Intercourse (CAI) (Panel A) and Receptive CAI (Panel B). Dotted line represents absolute value of minimum variable importance score
HIV transmission beliefs were associated with both insertive and receptive CAI behavior, including looking for other HIV-positive persons to have sex with (PRR=2.17, 95% CI: 1.44 – 3.26; insertive and PRR=1.94, 95% CI 1.42 – 2.65; receptive) and less concern about using condoms with HIV-positive partners (PRR=1.60, 95% CI: 1.02 – 2.52; insertive and PRR=1.41, 95% CI 0.98 – 2.02; receptive). Finding sex partners online was positively associated with receptive (PRR=1.59, 95% CI: 1.02 – 2.48) and insertive CAI (PRR=1.79, 95% CI: 1.25 – 2.56).
Predictors of Serodiscordant CAI
Similar to CAI, almost all predictors found to be important using RF methods were also identified in regression analysis. Variables strongly associated with SD-CAI, according to RF analysis (Figure 1, panel B), include problematic substance use (PRR=3.10, 95%CI: 1.63 – 5.87), and searching for sex partners online in the last 3 months (PRR=2.47, 95% CI: 1.46 – 4.18) with the rate of SD-CAI higher in those who searched for sex partners daily compared to those who searched less than weekly (PRR=2.19, 95% CI: 1.23 – 3.90). Hispanic/Latino ethnicity (PRR=2.06, 95% CI: 1.23 – 3.43), a perceived rise in homophobia (PRR=1.83, 95% CI: 1.09 – 3.06), and higher level of internalized homophobia (score of ≥ 4 vs 1) (PRR=2.50, 95% CI: 1.27 – 4.95) were also associated with a greater likelihood of SD-CAI.
DISCUSSION
A majority of virally non-suppressed YGBMSM enrolled in an mHealth treatment adherence intervention reported engaging in CAI in the last 3 months with being in a committed relationship, engaging in substance use and seeking sex online emerging as important predictors. While this echoes prior work (5), RF methods allowed for the elucidation of the relative importance of these variables, while accounting for their interdependency, in a way that is more difficult to demonstrate with standard regression modeling. Our findings can inform the development of more tailored risk reduction interventions for YGBMSM living with HIV.
Youth who reported being in a committed relationship were more likely to report CAI, aligning with prior studies among diverse MSM (21, 22) and affirming the likelihood that a significant proportion of HIV transmissions occur within the context of primary sexual relationships, particularly among YGBMSM (23). A desire to express intimacy, love and trust and to form an emotional connection are all motivating factors for CAI within relationships, however, most work to-date has focused on HIV-negative MSM (24, 25). An important next step for understanding relationship dynamics among youth would include a deeper investigation into the emotional context in which YGBMSM living with HIV make decisions about condom use and the role of primary partner turnover, partner concurrency and sexual agreements (26). Additional work could explore relationship longevity, communication, and sexual decision-making among YGBMSM living with HIV in order to create developmentally appropriate interventions, including consideration for couples-based approaches (27).
Rates of problematic substance use were high and associated with engagement in both CAI and SD-CAI; findings that have been well-described previously (21, 28–30). For some youth, substance use may be a way to cope with the stress of living with a stigmatized illness (including both HIV as well as comorbid mental health conditions) or as a way to lower inhibitions with regard to engagement in sex with another male partner (30). Substance use can also negatively impact ART adherence (31); thus, multifaceted interventions that address the type and frequency of substances that impact YGBMSM living with HIV is critical to limit the potential for onward transmission.
Higher internalized homophobia scores were associated with more than twice the prevalence of SD-CAI. While prior studies find mixed effects of the association between internalized homophobia and engagement in sexual risk behaviors among MSM (32, 33), among a large sample of black YGBMSM, those with greater internalized homophobia were less likely to discuss prevention with sex partners and disclose same sex sexual behavior to health care providers, and more likely to report receptive CAI (34). Future interventions to address internalized homophobia might adopt a resilience lens given findings that YGBMSM with more gay-affirming attitudes may be more likely to engage in protective health behaviors (35).
Depression and anxiety were prevalent in this sample, though not associated with sexual risk. Past studies, primarily focused on older MSM, report inconsistent findings of this association (36, 37), likely indicative of the complex relationship between psychosocial factors, cognitive appraisal processes, and risk (38). Notably, Cook et al. did find an independent association of depressive symptoms and sexual risk behavior, including both CAI and SD-CAI, in a large sample of YGBMSM living with HIV (39). While our cross-sectional study could not explore pathways from depression to engagement in risk, high prevalence supports interventions aimed at addressing mental health co-morbidities among YGBMSM living with HIV.
Youth enrolled in this study after the publication of seminal results documenting the beneficial individual and population effects of HIV treatment as prevention (TasP)(40) and approval of pre-exposure prophylaxis (PrEP) (41). Thus, our analysis provides a contemporary understanding of how messages regarding transmission are impacting engagement in risk. While less than half of participants endorsed the belief that they were less likely to infect another person through CAI if they had a low or undetectable VL, this was an important predictor of CAI in the RF analysis. Further, serosorting behaviors, specifically looking for other persons living with HIV to have sex with, was more likely to be reported by YGBMSM engaging in CAI (any, insertive and receptive). It is not known if participants had detectable viremia at the time of engaging in CAI or were even aware of their viral load results, but future work should explore if there exists any cognitive dissonance between how messages of protection are being received and their translation into behaviors among YGBMSM. While HIV transmission is not an issue among those with only positive partners, risks for acquisition of other STIs persists. In one study among adults living with HIV, participants with STIs were significantly more likely to have detectable viral loads and less likely to know their viral load than those who did not have an STI (42).
Overall, only 70% of participants were more concerned with using condoms with HIV negative/unknown status partners when their viral load was detectable. As TasP messaging appears to impact engagement in CAI (6), future qualitative work must take into account how youth are understanding and adapting their behaviors in the context of these scientific advances. Additional social and structural drivers of condom use and sexual risk including serostatus disclosure, social support and sexual network characteristics that impact both adherence and CAI among YGBMSM should be explored (39, 43, 44).
Use of geospatial apps and online sites to find sex partners was common in this study and among YGBMSM in general (45). While those who looked for sex partners online in the past 3 months were more likely to report any CAI, this finding should be interpreted cautiously given that other venues for meeting sex partners were not assessed. The stronger association between more frequent online partner searching and SD-CAI is similar to findings among an online sample of MSM (46). As such, continued development of online interventions, including consideration of delivery through sex seeking apps, is warranted.
The results of this research should be considered in light of its methodological limitations. The statistical methods were exploratory and not meant to provide confirmatory evidence of causal associations. The large number of null hypothesis tests performed make our results prone to Type I error, and thus, inference on any specific result should be interpreted with caution. All data analyzed were cross-sectional, and, therefore, interpretation of estimated prevalence ratios as risk ratios are subject to temporal bias, as well as point prevalence complement ratio bias. Specifically, all CAI outcomes were common (>20%) in most exposure strata, making the estimated prevalence ratio a conservative estimate of the risk ratio. Furthermore, like many randomized trials, our study sample was a convenience sample and our findings may not be generalizable to the broader YGBMSM population. Despite these limitations, many of our results align with previous findings and predictors of CAI, a positive sign of the external validity of our results. In addition, using two distinct methods of ascertaining risk factors and having those methods largely agree is a strong indication of internal validity.
Conclusion
High rates of CAI, including engagement in SD-CAI in a population of YGBMSM with detectable viral loads poses significant concerns for onward HIV transmission. Using multiple methods - both non-parametric (RF) and parametric (modified Poisson regression) approaches - to determine the most important predictors of CAI provides a more nuanced understanding of the multiple psychosocial individual and structural factors that are associated with engagement in risk in this priority population. Addressing these factors in concert with ensuring viral suppression will be key to ending the epidemic among youth in the US.
Supplementary Material
Implications and Contribution.
Findings indicate that half of all virally non-suppressed young, gay, bisexual and other men who have sex with men (YGBMSM) enrolled in an adherence intervention reported engaging in condomless anal intercourse (CAI) in the last 3 months. Predictors of CAI included individual, dyadic and structural level variables. This suggests the need for multifaceted interventions for YGBMSM living with HIV to stem onward transmission.
Acknowledgements
This paper was presented as a poster at the 2018 International AIDS Society Conference. Amsterdam, Netherlands, July 23–27, 2018.
This work was supported by the National Institutes of Health [grant number: R44 MH102096-02]
Footnotes
Disclosures:
No authors have conflicts of interest to report
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Centers for Disease Control and Prevention. HIV Among Youth. Available at: https://www.cdc.gov/hiv/group/age/youth/index.html Last accessed: August 14, 2019.
- [2].Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS 2014;28:128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lally MA, van den Berg JJ, Westfall AO, et al. HIV Continuum of Care for Youth in the United States. J Acquir Immune Defic Syndr 2018;77:110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kahana SY, Jenkins RA, Bruce D, et al. Structural Determinants of Antiretroviral Therapy Use, HIV Care Attendance, and Viral Suppression among Adolescents and Young Adults Living with HIV. PLoS One 2016;11:e0151106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wilson PA, Kahana SY, Fernandez MI, et al. Sexual Risk Behavior Among Virologically Detectable Human Immunodeficiency Virus-Infected Young Men Who Have Sex With Men. JAMA Pediatr 2016;170:125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bruce D, Harper GW, Suleta K, et al. Sexual risk behavior and risk reduction beliefs among HIV-positive young men who have sex with men. AIDS Behav 2013;17:1515–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Camacho-Gonzalez AF, Chernoff MC, Williams PL, et al. Sexually Transmitted Infections in Youth With Controlled and Uncontrolled Human Immunodeficiency Virus Infection. J Pediatric Infect Dis Soc 2017;6:e22–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bruce D, Bauermeister JA, Kahana SY, et al. Correlates of Serodiscordant Condomless Anal Intercourse Among Virologically Detectable HIV-Positive Young Men Who Have Sex with Men. AIDS Behav 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hall HI, Holtgrave DR, Tang T, et al. HIV transmission in the United States: considerations of viral load, risk behavior, and health disparities. AIDS Behav 2013;17:1632–1636. [DOI] [PubMed] [Google Scholar]
- [10].LeGrand S, Muessig KE, Platt A, et al. Epic Allies, a Gamified Mobile Phone App to Improve Engagement in Care, Antiretroviral Uptake, and Adherence Among Young Men Who Have Sex With Men and Young Transgender Women Who Have Sex With Men: Protocol for a Randomized Controlled Trial. JMIR Res Protoc 2018;7:e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].LeGrand S, Muessig KE, McNulty T, et al. Epic Allies: Development of a Gaming App to Improve Antiretroviral Therapy Adherence Among Young HIV-Positive Men Who Have Sex With Men. JMIR Serious Games 2016;4:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Gonzalez P, Nunez A, Merz E, et al. Measurement properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): Findings from HCHS/SOL. Psychol Assess 2017;29:372–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Swinson RP. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evid Based Med 2006;11:184. [DOI] [PubMed] [Google Scholar]
- [14].Group WAW. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction 2002;97:1183–1194. [DOI] [PubMed] [Google Scholar]
- [15].Rumpf HJ, Wohlert T, Freyer-Adam J, et al. Screening questionnaires for problem drinking in adolescents: performance of AUDIT, AUDIT-C, CRAFFT and POSIT. Eur Addict Res 2013;19:121–127. [DOI] [PubMed] [Google Scholar]
- [16].Wright K, Naar-King S, Lam P, et al. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health 2007;40:96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Journal of Counseling Psychology 2009;56:32. [Google Scholar]
- [18].Strobl C, Malley J, Tutz G. An introduction to recursive partitioning: rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol Methods 2009;14:323–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Machado G, Mendoza MR, Corbellini LG. What variables are important in predicting bovine viral diarrhea virus? A random forest approach. Vet Res 2015;46:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hothorn T, Hornik K, Strobl C, et al. Party: A laboratory for recursive partytioning. 2010.
- [21].Mustanski BS, Newcomb ME, Du Bois SN, et al. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res 2011;48:218–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Stueve A, O’Donnell L, Duran R, et al. Being high and taking sexual risks: findings from a multisite survey of urban young men who have sex with men. AIDS Educ Prev 2002;14:482–495. [DOI] [PubMed] [Google Scholar]
- [23].Sullivan PS, Salazar L, Buchbinder S, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS 2009;23:1153–1162. [DOI] [PubMed] [Google Scholar]
- [24].Rosenberger JG, Herbenick D, Novak DS, et al. What’s love got to do with it? Examinations of emotional perceptions and sexual behaviors among gay and bisexual men in the United States. Arch Sex Behav 2014;43:119–128. [DOI] [PubMed] [Google Scholar]
- [25].Starks TJ, Gamarel KE, Johnson MO. Relationship characteristics and HIV transmission risk in same-sex male couples in HIV serodiscordant relationships. Arch Sex Behav 2014;43:139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Goldenberg T, Finneran C, Andes KL, et al. ‘Sometimes people let love conquer them’: how love, intimacy, and trust in relationships between men who have sex with men influence perceptions of sexual risk and sexual decision-making. Cult Health Sex 2015;17:607–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Jiwatram-Negron T, El-Bassel N. Systematic review of couple-based HIV intervention and prevention studies: advantages, gaps, and future directions. AIDS Behav 2014;18:1864–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bruce D, Harper GW, Fernandez MI, et al. Heavy Marijuana Use among Gay and Bisexual Male Emerging Adults Living with Hiv/Aids. J HIV AIDS Soc Serv 2013;12:26–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Bruce D, Kahana S, Harper GW, et al. Alcohol use predicts sexual risk behavior with HIV-negative or partners of unknown status among young HIV-positive men who have sex with men. AIDS Care 2013;25:559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].VanDevanter N, Duncan A, Burrell-Piggott T, et al. The influence of substance use, social sexual environment, psychosocial factors, and partner characteristics on high-risk sexual behavior among young Black and Latino men who have sex with men living with HIV: A qualitative study. AIDS Patient Care STDS 2011;25:113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].White JM, Gordon JR, Mimiaga MJ. The Role of Substance Use and Mental Health Problems in Medication Adherence Among HIV-Infected MSM. LGBT Health 2014;1:319–322. [DOI] [PubMed] [Google Scholar]
- [32].Mizuno Y, Borkowf C, Millett GA, et al. Homophobia and racism experienced by Latino men who have sex with men in the United States: correlates of exposure and associations with HIV risk behaviors. AIDS Behav 2012;16:724–735. [DOI] [PubMed] [Google Scholar]
- [33].Johnson MO, Carrico AW, Chesney MA, et al. Internalized heterosexism among HIV-positive, gay-identified men: implications for HIV prevention and care. J Consult Clin Psychol 2008;76:829–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Crosby RA, Salazar LF, Mena L, et al. Associations Between Internalized Homophobia and Sexual Risk Behaviors Among Young Black Men Who Have Sex With Men. Sex Transm Dis 2016;43:656–660. [DOI] [PubMed] [Google Scholar]
- [35].Hussen SA, Harper GW, Rodgers CRR, et al. Cognitive and Behavioral Resilience Among Young Gay and Bisexual Men Living with HIV. LGBT Health 2017;4:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Mustanski B The influence of state and trait affect on HIV risk behaviors: a daily diary study of MSM. Health Psychol 2007;26:618–626. [DOI] [PubMed] [Google Scholar]
- [37].Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS 2006;20:731–739. [DOI] [PubMed] [Google Scholar]
- [38].Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav 2011;15:1171–1179. [DOI] [PubMed] [Google Scholar]
- [39].Cook SH, Valera P, Wilson PA, et al. HIV status disclosure, depressive symptoms, and sexual risk behavior among HIV-positive young men who have sex with men. J Behav Med 2015;38:507–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N Engl J Med 2016;375:830–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Holmes D FDA paves the way for pre-exposure HIV prophylaxis. Lancet 2012;380:325. [DOI] [PubMed] [Google Scholar]
- [42].Kalichman SC, Eaton L, Cherry C. Sexually transmitted infections and infectiousness beliefs among people living with HIV/AIDS: implications for HIV treatment as prevention. HIV Med 2010;11:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].O’Connell AA, Reed SJ, Serovich JA. The efficacy of serostatus disclosure for HIV Transmission risk reduction. AIDS Behav 2015;19:283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Imahashi M, Fujimoto K, Kuhns LM, et al. Network overlap and knowledge of a partner’s HIV status among young men who have sex with men. AIDS Care 2019;31:1533–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Holloway IW, Rice E, Gibbs J, et al. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav 2014;18:285–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Cruess DG, Burnham KE, Finitsis DJ, et al. Online Partner Seeking and Sexual Risk Among HIV+ Gay and Bisexual Men: A Dialectical Perspective. Arch Sex Behav 2017;46:1079–1087. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.