Abstract
The demand for telemedicine has been increasing over the past several years with the growth of technology and digital connectivity in our daily lives. With the impact of the global coronavirus disease 2019 pandemic, telemedicine implementation has become a necessity for many specialties because social distancing measures have greatly affected access to routine medical care. This article presents a detailed and systematic approach to conducting a hand physical examination during a video telemedicine encounter. Although the telemedicine physical examination has limitations, most components of the normal physical examination can be completed remotely with a systematic approach. We enumerate modifications to maximize examination remotely and present considerations for improved delivery of telemedicine care. These methods may be beneficial to providers incorporating telemedicine into their practice.
Key words: Coronavirus, COVID-19, Hand examination, Telehealth, Telemedicine
With the continued impact of the global coronavirus disease 2019 (COVID-19) pandemic, the application and expansion of telemedicine modalities have become prominent. Although telemedicine has been used successfully for many years for a variety of purposes, the inability to touch our patients physically has resulted in limited use of telemedicine for fields that rely heavily on physical examination. Thus, most data presented to date on the efficacy of telehealth as an alternative to office visits has largely focused on telemental health, telerehabilitation, and teledermatology.1 Because of the importance of the physical examination within hand surgery, applications of telemedicine have been limited. Telemedicine applications within hand surgery have largely focused on specific clinical situations, such as postoperative care for select patients, smartphone photography to monitor range of motion (ROM) for specific joints, and triage for tertiary referral.2, 3, 4, 5, 6 A randomized controlled trial examining comprehensive video-assisted orthopedic consultations demonstrated that physicians rated their ability to examine the patient as good or very good 98% of the time.7 Of note, the examination was completed with the help of a nurse trained in physical examination maneuvers. It was also shown that these visits provided adequate patient satisfaction and were cost-effective.8,9 Although there have been successful applications of telemedicine in specific settings, the ability to perform a comprehensive hand consultation and examination has not been evaluated. Because of the current demand for telemedicine visits, the purposes of this article and accompanying Video were to characterize the components of the hand examination that could and could not be performed remotely and to suggest adjustments to maximize the efficacy of the remote hand consultation and examination.
Feasibility of Telemedicine Hand Examination
The comprehensive hand examination in a traditional office visit typically involves inspection and palpation, vascular examination, sensory examination, and motor examination. The ideal position for examination is with the patient across from the provider, with the patient’s hands resting on a table. Complete inspection consists of observing how the patient holds the hands and assessing for visible signs of injury or trauma such as swelling, erythema, ecchymosis, and laceration. Inspection should include having the patient demonstrate the digital cascade through flexion and extension, paying close attention to deficits in ROM or malrotation. Palpation should assess for areas of localized tenderness, swelling, or masses. Areas of localized swelling or erythema should also be assessed for associated fluctuance and warmth. Vascular examination consists of a peripheral pulse examination, temperature, color assessment, and capillary refill. A proper sensory examination should consist of the ability to discern light touch, as well as 2-point discrimination in the relevant sensory distributions. A motor examination should begin with assessing for passive ROM across all joints in the hand and wrist. All extrinsic flexors, extrinsic extensors, and intrinsic muscles should be assessed with and without resistance. Finally, specialty tests should be performed, such as provocative tests for carpal tunnel, cubital tunnel, and de Quervain tenosynovitis, among others.
Using the normal in-person hand examination as a framework, we can systematically go through and assess each step or maneuver for feasibility during a remote, telemedicine encounter. Patient positioning is important during in-person examinations, equally so when remote. However, limitations in camera positioning poses challenges for both the patient and the provider. Ideal positioning would have a camera looking down on the patient’s hands, as if directly across from the provider. However, this cannot be independently achieved with all personal computers or smart devices. In addition, this camera angle prohibits eye contact with the patient, which could prove detrimental to communication during the examination. The use of a smart phone poses additional limitations as one hand may have to be used to hold the device. If a smartphone is the only option for a patient, the assistance of a family member or friend may be warranted for videotaping. Alternatively, patients can be instructed to secure the handheld device in a vertical position across themselves for the optimal perspective.
During the physical examination, inspection can be accomplished with minimal limitation. Adequate assessment for trauma and other signs of injury can be performed, as well as observation of the digital cascade. Palpation cannot be performed remotely, and thus detailed assessment for tenderness, as well as localization of any masses, is limited by remote examination. The vascular examination had limitations as well. Peripheral pulses and temperature cannot be properly assessed, whereas color and capillary refill can be reliable. It is not possible to conduct formal sensory examination with 2-point discrimination remotely. Most aspects of the motor examination can be accomplished remotely, aside from strength against resistance. Passive ROM can be performed with the use of the patient’s contralateral hand to demonstrate end ROM. With the use of graphical instruction or visual demonstration, motor function for each muscle group in the hand and wrist can be evaluated with the assistance of the patient’s opposite hand. Although the patient can perform these maneuvers independently, the provider is unable to make a quantitative strength assessment without providing resistance. Thus, distinguishing strength for grades 3, 4, and 5 of 5 is impossible. Certain special tests and provocative maneuvers can be consistently performed whereas others cannot. For example, Tinel or Durkan test cannot be performed for carpal tunnel. However, Phalen test can be performed independently to recreate the subjective symptoms of carpal tunnel. For cubital tunnel, Tinel test cannot be performed but the elbow flexion test serves as a good alternative. Others, such as Finklestein, Froment, triangular fibrocartilage complex (TFCC) load test, and Cozen tests all can be modified and performed independently in the remote setting. Table 1 lists limitations and reasonable alternatives for special hand tests.
Table 1.
Modified Examinations
| Examination | Feasibility for Telemedicine | Proposed Examination or Adjustments |
|---|---|---|
| Carpal tunnel | Phalen or reverse Phalen | |
| Tinel | Poor | |
| Durkan | Poor | |
| Phalen | Good | |
| Reverse Phalen | Good | |
| Cubital tunnel | Elbow flexion | |
| Tinel | Poor | |
| Elbow flexion | Good | |
| de Quervain | Modified Finklestein | |
| Finklestein | Variable | |
| Eichhoff | ||
| Trigger finger | Rely on inspection during digital flexion and triggering | |
| Palpation at A1 pulley | Poor | |
| Triggering of finger | Good | |
| Epicondylitis | Modified Cozen and golfer’s elbow test | |
| Cozen (lateral) | Poor | |
| Golfer’s elbow test (medial) | Poor | |
| Ulnar nerve palsy | Modified Froment | |
| Froment | Poor | |
| Wartenberg sign | Good | |
| TFCC tear | ||
| TFCC load test | Poor | Modified TFCC load test |
Comprehensive Telemedicine Hand Physical Examination
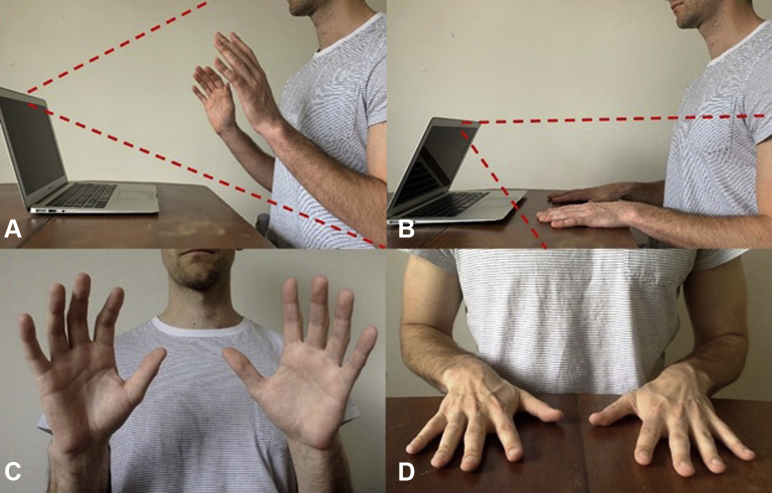
With the feasibility of each aspect of the physical examination in mind, we established our approach to the remote physical telemedicine encounter. In anticipation of the limitations of the remote examination, there should be an increased focus on taking a detailed and focused patient history. The first consideration when initiating the examination portion of the encounter is patient positioning. Most of the examination will be conducted with the patient facing the device’s camera, with the shoulders centered in the frame (Fig. 1A). This is most easily accomplished with the use of a personal laptop that allows for easy camera adjustment in the vertical axis.
Figure 1.
Patient and laptop positioning A with view centered on shoulders and B with palms flat on table with C, D corresponding views from the provider’s perspective.
Inspection and palpation
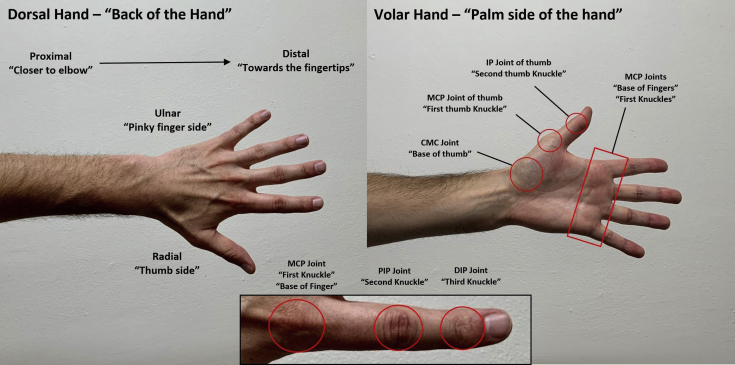
Begin with inspecting the dorsal and volar aspects of the hand and wrist by having the patient hold the hands up and go through the range of full pronation and supination. Pay specific attention to deformities such as swan’s neck, mallet, or boutonniere, or signs of Dupuytren disease or arthritis. Ask the patient to make a series of fists by flexing and extending all digits. This should be performed with the patient’s hands in full pronation with palms facing the camera, as well as in a neutral position with the palms perpendicular to the camera. This allows for complete visualization of the digital cascade. The entirety of the forearm, elbow, and upper arm to the shoulder should be visualized as well. Expanding the scope of inspection may improve the accuracy of the examination and provide additional clues that may complement the limitations of the telemedicine encounter. Because palpation cannot be accomplished remotely, we propose that graphical depictions of relevant surface anatomy and anatomical orientation using layman’s terms be given to the patient to aid in this portion of the examination (Fig. 2). The provider should move systematically through each area of interest, showing the patient where to press. Although this can be variable in accuracy and success, it can help the patient communicate more effectively and localize areas of tenderness or masses to the provider.
Figure 2.
Graphical depiction of relevant surface anatomy and anatomical orientation for patient review before and during telemedicine encounter. This identifies basic anatomical vocabulary and orientation with corresponding layman’s terms in quotations marks. CMC, carpometacarpal; DIP, distal interphalangeal; IP, interphalangeal; MCP, metacarpophalangeal; PIP, proximal interphalangeal.
Neurovascular evaluation
The vascular portion of the examination is performed by assessing for abnormalities in color and having the patient perform the capillary refill test with the fingernail near the camera. Despite limitations in the sensory examination, subjective numbness or paresthesias can be further explored independently with the use of a paper clip. Providing pictorial depictions of relevant sensory distributions can aid the patient in a subjective comparison of sensory function.
Motor examination
For the motor examination, begin by having the patient demonstrate passive ROM using the contralateral hand to demonstrate end range of flexion and extension of all digits and both wrists. Explore any deficits in greater detail by having the patient provide closer visualization so the provider can obtain a more accurate estimate of ROM of each joint. For active motor function, the provider should demonstrate each maneuver beforehand to help with patient compliance. Begin with the extrinsic flexors. Ideal visualization for the provider is achieved with the patient’s hands in a neutral position, with the palms perpendicular to the camera or slightly pronated. Assess the flexor pollicis longus by having the patient block the metacarpophalangeal (MCP) joint of the thumb and flex through the interphalangeal joint. Assess the flexor digitorum profundus of each digit by having the patient block the proximal interphalangeal joint and flexing through the distal interphalangeal joint. Assess the flexor digitorum superficialis by blocking flexion of adjacent digits before flexing through the digit of interest. Ideal assessment of the extrinsic extensors involves a change in camera angle. If possible, instruct the patient to lower the camera so that the palms can rest flat on the table in view of the camera (Fig. 1B). Assess the abductor pollicis longus and extensor pollicis brevis by having the patient extend and abduct the thumb away from the hand. Assess the extensor pollicis longus by having the patient lift the thumb off the table. Assess the extensor digitorum communis for each digit by independently extending and lifting it off the table, making sure that MCP joints are in extension. Have the patient make a fist and assess the extensor carpi radialis brevis and longus by demonstrating extension and radial deviation of the wrist, and the extensor carpi ulnaris by ulnar deviation of the wrist. Next, evaluate the function of the intrinsic muscles of the hand. Have the patient demonstrate MCP flexion and proximal interphalangeal joint extension to evaluate the function of the lumbrical muscles. Have the patient abduct, adduct, and then cross the fingers to evaluate interosseous muscle function, paying close attention for Wartenberg sign. Finally, have the patient demonstrate opposition of the thumb and little finger to evaluate the intrinsic thenar and hypothenar muscles.
Special tests
The physical examination should conclude by using any special tests or provocative maneuvers that are warranted based on the patient’s history and physical examination thus far. In brief, special tests that can be reliably performed include Phalen test, elbow flexion test, and modified versions of Finklestein, Froment, Cozen, and TFCC load test.
To perform the Phalen test, have the patient oppose the dorsal aspect of each hand to achieve complete and forced flexion of both wrists. Have the patient hold this position for 30 to 60 seconds and assess for the presence of symptoms in the median nerve distribution.
The elbow flexion test is performed by having the patient hold the elbow in full flexion for 1 minute to assess for the presence of symptoms in the ulnar distribution.
A modified Finklestein test can be performed independently by ulnarly deviating the wrist and using the contralateral hand to flex the thumb into the palm to assess for pain along the extensor pollicis brevis–abductor pollicis longus tendons. A modified test for Froment sign for ulnar nerve palsy can be performed with the patient holding both ends of a piece of paper.
A modified test for Cozen sign for lateral epicondylitis can be performed with the patient’s forearm and palm flat on the table. Have the patient make a fist, extend the wrist to elevate fist off the table, and use the contralateral hand to provide resistance to wrist extension. A modified golfer’s elbow test can be performed in a similar fashion with wrist flexion.
A modified TFCC load test can be performed with the patient loading the little finger with the contralateral hand. Figure 3 demonstrates modified examination maneuvers. Although these tests ideally should be performed in their unmodified form by a trained provider for proper interpretation, we believe that these modifications are adequate and reliable for the purposes of a telehealth encounter when in-person visitation is not possible.
Figure 3.
Demonstrations of modified special examination maneuvers. Modified Froment showing A negative and B positive signs. Modified tests for C, D medial and E, F lateral epicondylitis. Patient positioning for G modified TFCC load test and H modified Finklestein test.
Special considerations and patient selection
To maximize the usefulness of any telemedicine visit, it is vital for radiographic studies and other advanced diagnostic testing such as EMG results to be available for review. Special attention should be paid on the days leading up to a telemedicine visit to contact patients and provide them with instructions regarding how to make imaging and test results available to their provider for timely review. In addition, if radiographic studies are necessary for a visit but have not been completed, these should be ordered in advance. Because of the limitations of the remote patient encounter, access to all diagnostic studies is even more important. Because of the limitations of the remote physical examination, it may be helpful and a more efficient use of time and resources to give scheduling preference to patients who have diagnostic studies ready for review for telemedicine visits.
As mentioned, several studies outlined and validated appropriate use for telemedicine for specific types of patient encounters.2, 3, 4, 5 Several recent studies commented on smartphone photography as a reliable alternative to goniometry, the reference standard for measuring joint ROM. This has been shown to be effective for measuring ROM in the elbow, wrist, and fingers, especially in the setting of contracture. For patients for whom it is known that an assessment of ROM for a particular joint will be a necessary component of the physical examination, instructions can be provided regarding how to photograph themselves accurately. Another specific patient encounter that was validated in the telemedicine setting is postoperative care for carpal tunnel release. As described by Tofte et al,2 patients provided with instructions about removing surgical dressing and sutures, photographing the incision, and performing a basic neuromuscular examination were able to complete an effective 10- to 14-day postoperative visit remotely. However, suture removal proved to be the most difficult aspect.2 With this in mind, we believe that postoperative visits for minor hand surgery such as carpal tunnel release or trigger finger release can be readily managed through a telemedicine visit, especially if absorbable sutures were used. Many other postoperative visits can likely be managed remotely but should be evaluated on a case by case basis to determine the level of care and individual patient demands.
Thought should also be given to specific patient encounters that are not appropriate to be conducted via telemedicine. Clearly, any injuries that require manipulation, such as displaced fractures or dislocations, or other specialized care such as pin removal or cast removal or application, cannot be conducted remotely. In addition, patients for whom it is known with relative certainty that an injection needs to be administered, such as recurrent trigger finger or carpometacarpal arthritis, would benefit little from a telemedicine visit.
A more complicated issue to tackle is the surgical decision-making process and informed consent. It has been shown that telemedicine encounters are not inferior to in-person encounters for patient comprehension during informed consent.10 However, there is uncertainty whether reliable risk and benefit assessment can be conveyed remotely. For patients with a previous in-person encounter with documented appropriateness for surgical intervention, surgical decision-making and informed consent can proceed without issue. We also think that conditions with well-defined radiographic criteria for surgery are appropriate for surgical decision-making and informed consent via a remote visit. In these cases, the risks and benefits of intervention versus nonintervention, such as persistent deformity, posttraumatic arthritis, and recurrent joint instability, can be reliably assessed from certain radiographic studies and do not depend on physical examination. In cases in which indications for surgery are more complex and have not been discussed in previous detail, an adequate risk and benefit assessment might not be possible in a remote setting. In such cases, patient comprehension of risks and benefits may require in-depth demonstration, patient education, or understanding of the patient’s own physical examination findings, which may necessitate in-person consultation. Thus, we advise providers to exercise caution before obtaining consent for surgery in these situations.
Providers should also be aware of technology access and digital literacy limitations of their patients. According the American Consumer Survey Reports conducted in 2016, 89% of households in the United States had a personal computer or smart device in their home and 81% had access to broadband Internet.11 Higher rates of access to technology included younger householders and those located in metropolitan areas. Lower rates of access to computers or smart devices were ones making less than $25,000/y and those aged greater than 65 years, with access rates of 71.7% and 74.8%, respectively. Digital literacy is also an important factor to consider. Data from the US Department of Education demonstrated that digital literacy is associated with level of education and age.12 Digital literacy rates were 59% for individuals with less than a high school education and 72% for individuals aged 55 to 65 years. This is compared with a rate of 84% for all individuals aged 16 to 65 years. For practical purposes, when scheduling a telemedicine appointment, it is vital to know the devices to which the patient has access, if the patient is able to use them properly, and, if not, whether anyone in the household is able to assist before the start of an encounter. A previsit contact with the patient establishing technological aptitude can be beneficial to the success of the telehealth encounter. This communication may be accomplished by the person scheduling the visit, a medical assistant, or a physician extender.
Patient confidentiality should always be protected and telemedicine practices must comply with Health Insurance Portability and Accountability Act of 1996 (HIPAA) rules and regulations. Thus, patient health data and video conferencing security are important considerations when initiating telemedicine encounters.13 Although many commonly employed video conferencing platforms are safe and appropriate for use in this setting, proper compliance requires entering a HIPAA business associates agreement with a technology vendor to ensure data security.14 With the declaration of a national health emergency from COVID-19, the Office for Civil Rights at the Department of Health and Human Services announced that to access a greater number of patients and limit risk for infection, it will not impose penalties for video-chatting noncompliance with HIPAA.15 This provision lasts for the duration of the national health emergency and applies to the use of telemedicine for any reason, not just illness relating to COVID-19. Thus, lack of a business associates agreement should not prohibit providers from using telemedicine, but providers should be sure to establish proper compliance if they wish to continue telemedicine practices outside the national health emergency provision.
Conclusion
Although limitations exist for hand surgery telemedicine visits, especially as they pertain to aspects of the physical examination, we believe that with thoughtful consideration of examination maneuvers and appropriate patient selection, a significant amount of patient encounters can be effectively conducted remotely. Feasibility has been shown for several specific applications of telemedicine within hand surgery, but broader applications of telemedicine have not been fully evaluated. Currently, with the global COVID-19 pandemic and widespread stay-at-home orders, providers have been faced with growing pressure to evaluate patients from a distance. Subsequent studies should be performed to validate the broader application of telemedicine in hand surgery, but efforts should be made now to continue to meet the current needs of our patients.
Footnotes
Declaration of interests: Dr Rivlin is associated with or financially involved with Dimension Orthotics, LLC. No benefits in any form have been received or will be received by the other authors related directly or indirectly to the subject of this article.
Supplementary Data
References
- 1.Shigekawa E., Fix M., Corbett G., Roby D.H., Coffman J. The current state of telehealth evidence: a rapid review. Health Aff (Millwood) 2018;37(12):1975–1982. doi: 10.1377/hlthaff.2018.05132. [DOI] [PubMed] [Google Scholar]
- 2.Tofte J.N., Anthony C.A., Polgreen P.M., et al. Postoperative care via smartphone following carpal tunnel release. J Telemed Telecare. 2020;26(4):223–231. doi: 10.1177/1357633X18807606. [DOI] [PubMed] [Google Scholar]
- 3.Zhao JZ, Blazar PE, Mora AN, Earp BE. Range of motion measurements of the fingers via smartphone photography [published online ahead of print January 28, 2019]. Hand (N Y). 10.1177/1558944718820955. [DOI] [PMC free article] [PubMed]
- 4.Wagner E.R., Conti Mica M., Shin A.Y. Smartphone photography utilized to measure wrist range of motion. J Hand Surg Eur Vol. 2018;43(2):187–192. doi: 10.1177/1753193417729140. [DOI] [PubMed] [Google Scholar]
- 5.Meislin M.A., Wagner E.R., Shin A.Y. A comparison of elbow range of motion measurements: smartphone-based digital photography versus goniometric measurements. J Hand Surg Am. 2016;41(4) doi: 10.1016/j.jhsa.2016.01.006. 510.e1–515.e1. [DOI] [PubMed] [Google Scholar]
- 6.Tripod M., Tait M., Bracey J., Sexton K., Beck W., Wyrick T.O. The use of telemedicine decreases unnecessary hand trauma transfers. Hand (N Y) 2020;15(3):422–427. doi: 10.1177/1558944718810877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16(1):483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25(8):451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 9.Buvik A., Bergmo T.S., Bugge E., Smaabrekke A., Wilsgaard T., Olsen J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2) doi: 10.2196/11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bobb M.R., Van Heukelom P.G., Faine B.A., et al. Telemedicine provides noninferior research informed consent for remote study enrollment: a randomized controlled trial. Acad Emerg Med. 2016;23(7):759–765. doi: 10.1111/acem.12966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan C. Computer and Internet use in the United States: 2016. American Community Survey Reports: US Census Bureau. 2017;ACS-39. Available at: https://www.census.gov/content/dam/Census/library/publications/2018/acs/ACS-39.pdf. Accessed May 22, 2020.
- 12.Mamedova S, Pawlowski E. A Description of U.S. Adults Who Are Not Digitally Literate. Statistics In Brief: US Department of Education. 2018 May; NCES 2018-161.
- 13.Naam N.H., Sanbar S. Advanced technology and confidentiality in hand surgery. J Hand Surg Am. 2015;40(1):182–187. doi: 10.1016/j.jhsa.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services Health Insurance Portability and Accountability Act of 1996 (HIPAA) [Internet] https://www.hhs.gov/hipaa/for-professionals/index.html Available at:
- 15.Office for Civil Rights, US Department of Health and Human Services Notification of enforcement discretion for telehealth [Internet] https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.