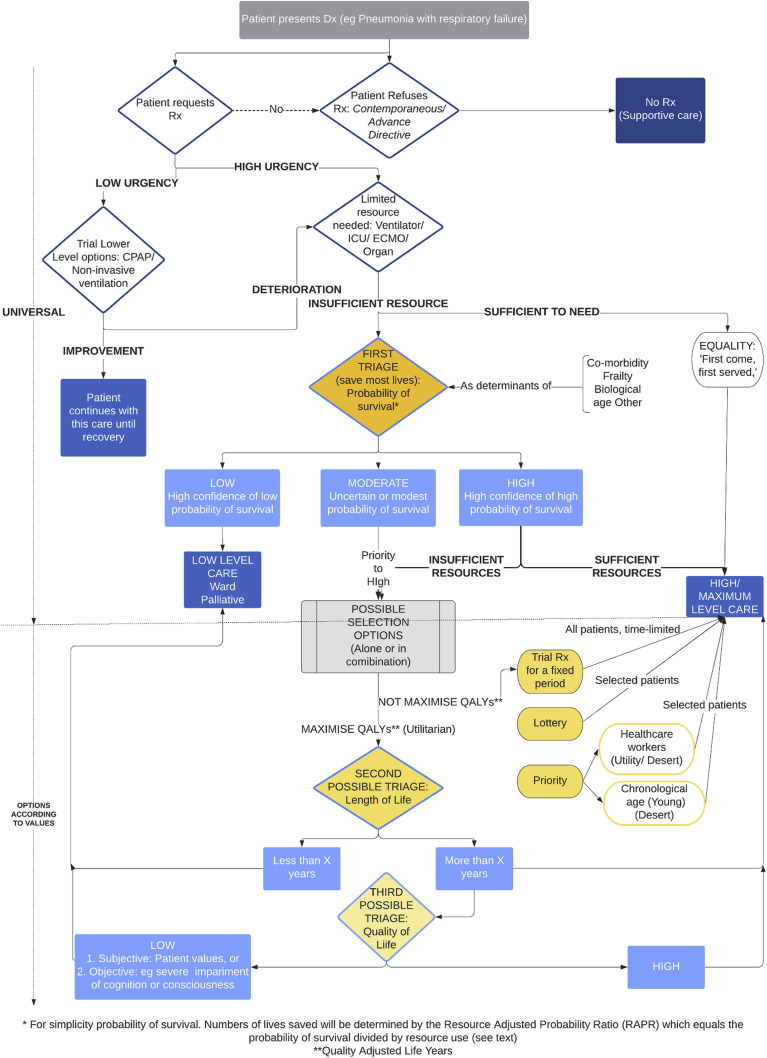
The burning ethical question raised by the coronavirus disease 2019 (COVID-19) pandemic is how to deal fairly and ethically with a large number of patients simultaneously becoming critically unwell. Across the world, in both developed and developing countries, health systems are grappling with the possibility or the reality that the demand for intensive medical care will outstrip availability. There is a need for ethical guidelines on how to allocate treatment, but such guidelines are potentially highly controversial.1 In this commentary, we set out a simple algorithm (Fig 1 ), including what we take to be the essential ethical principles that ought to guide resource allocation in any country or setting and optional elements that will vary between countries depending on the weight placed on different ethical values (Table 1 ).2, 3, 4, 5, 6, 7
Fig. 1.
An ethical algorithm for rationing life sustaining treatment.
Table 1.
Comparison of ventilator/intensive care allocation guidelines proposed or being applied in the setting of the COVID-19 pandemic. NICE, National Institute for Health and Care Excellence; QALY, quality adjusted life-years; QoL, quality of life; SIAARTI, Italian Society of Anesthesia Analgesia Resuscitation and Intensive Care; SOFA, Sequential Organ Failure Assessment.
| First level triage | Second level principles (tie break or supplementary) | |||||
|---|---|---|---|---|---|---|
| Pandemic allocation guidelines | Probability of survival | Duration of therapy required | Life-years/quality | Reciprocity (priority to health workers or young) | Equal share – fixed duration (time-limited trial) | Equal chance (lottery or first-come, first-served) |
| SIAARTI (Italy),2 Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances | ✓ Comorbidities, functional status, age (no specific cut off) |
× | ✓ | × | ✓ ICU trial (daily re-evaluation) |
× |
| NICE (UK)3 COVID-19 rapid guideline: critical care in adults |
✓ Frailty (not applied to younger people, stable long-term disabilities, learning disabilities and autism), Comorbidities, Severity of acute illness |
× | × | × | Review of treatment suggested | × |
| University of Pittsburgh (US)4 Allocation of scarce critical care resources during a public health emergency |
✓ SOFA scores, comorbidities |
× | × | ✓ Both |
Periodic reassessment | × |
| Daugherty and colleagues (US)5 Too many patients … a framework to guide statewide allocation of scarce mechanical ventilation during disasters |
✓ Likelihood of short-term survival (SOFA scores), likelihood of long-term survival (severe comorbidities) |
× | × | ✓ Life-cycle preference for young Pregnant women |
× | ✓ After other principles |
| Emanuel and colleagues (international)6 Fair allocation of scarce medical resources in the time of COVID-19 |
✓ | × | ✓ Life-years only in comparing patients whose likelihood of survival is similar No evaluation of QoL or QALY |
✓ Priority to health care workers when other factors similar; Youngest first when it aligns with maximising benefits |
✓ | ✓ No first-come first-served; Random selection among patients with similar prognosis |
| New York State Task Force on Life and the Law, New York State Department of Health7 Ventilator allocation guidelines |
✓ Likelihood of short-term survival (SOFA scores) |
× | × | ✓ Young age may be considered as a tie-breaking criterion in limited circumstances |
✓ Review at 48 and 120 h |
✓ Lottery after other principles |
Support patient autonomy
When a competent patient presents with a diagnosis (e.g. viral pneumonia), they should be provided with the facts about the available treatments and given the opportunity to express their personal wishes, priorities, and values. Requests may not be able to be accommodated, but competent refusals must be respected. Refusal can be contemporaneous, or through a valid advance directive or legally appointed surrogate if they are incompetent. Where possible, patient values should be elicited about what quality of life they would judge acceptable after intensive medical treatment.
Assess urgency, delay non-urgent treatment
If clinical need is non-urgent, a trial of lower levels of care (e.g. CPAP, noninvasive ventilation) should be instituted to reduce demand on critical care. A treatment escalation plan should be in place in case they subsequently deteriorate.
Consider availability of resource
The resource (CPAP, ventilator, ICU care, extracorporeal membrane oxygenation [ECMO], organ support) is either sufficient for the needs of all relevant patients or it is not. If it is sufficient, then a principle of equal treatment for equal need applies. In intensive care, this principle will often take the form of ‘first come, first served’, allocating preferentially to those arriving first for medical attention.
If there are insufficient resources, one solution would be to increase availability. Where this is not possible (or has already occurred, and resources are still insufficient), ‘first come, first served’ would mean that patients with poor prognosis, requiring long periods of treatment be treated at the expense of patients arriving later with much better prognosis. This will inevitably mean a reduction in the number of lives saved. It would also be unfair because when someone happens to fall ill (earlier or later) would decide allocation. According to the principle of temporal neutrality,8 when a harm occurs should not make a moral difference. In a separate paper,1 we discuss a number of other shortcomings of ‘first come, first served’ when there are limited resources.
First level allocation: save the most lives
The first ethical principle for allocation aims to maximise the numbers of lives saved. This is a basic principle endorsed by triage in settings of overwhelming medical need (e.g. disaster, battlefields, or pandemics). It is supported by both popular intuition and multiple ethical theories, as we now show.
Imagine you are manning the sole coastguard boat on duty. Two boats have overturned some distance from each other. There are five people in one life raft due north and, some 50 miles away due south, another person is on a separate life raft. A storm is brewing and it is likely that you will only be able to get to one life raft before the storm overturns them and the sailors drown. Which direction should you go?
Several years ago, when we asked a random sample of the public, 98% of respondents (88/90) elected to save five drowning people rather than one person; only 2% elected to toss a coin to decide.9
According to utilitarianism, resources should be distributed to bring about the most good: the greatest good to the greatest number. But non-utilitarian theories can also recognise the importance of this principle. According to a contractualist approach, the right distribution is the one we would choose from behind a ‘veil of ignorance’, that is if we did not know who we would be in society. From behind the veil, rational self-interest requires that you choose the policy that gives you the greatest chance of surviving.
We should save more lives rather than fewer, other things being equal. We can call this the moral requirement to save the greatest number. It should be a universal requirement of rationing.
In practice, saving the greatest number logically entails saving those patients with a higher probability of surviving. Imagine one group, A, has a 90% chance of surviving with treatment, and another group, B, has a 10% chance. For every 10 people treated in group A, 9 will survive, but only one will survive from B.
Saving the greatest number also requires estimating patients' duration of treatment and other resource use, as longer duration of therapy means fewer patients can be treated. Imagine patients in group A take 1 week to recover and patients in B take 2 weeks. We can save two patients in group A for every one patient in B. Group A patients, like those with higher probability of survival, should have priority.
These two factors affecting number saved can be combined in the concept of a Resource Adjusted Probability Ratio (RAPR).
The concept captures that patients who have higher probabilities of survival and are expected to recover quickly (freeing up the resources for others) should have highest priority. Length of stay is a good proxy for resource use. For example if a patient has a 50% chance of survival and the predicted length of stay is 10 days, whereas the average length of stay is 5 days, the RAPR is 25%.
Different patient factors may predict prognosis; for example biological age, frailty, and comorbidity may reduce the RAPR in patients with COVID-19 respiratory failure. Any factor that reduces probability of survival or increases resource use is relevant at this stage. This is the ethical justification for recent National Institute for Health and Care Excellence (NICE) guidance to consider not providing intensive care to patients with high frailty scores.3 Would this be discriminatory?
It would be discriminatory to include criteria in allocation that are not ethically relevant (e.g. race, sexuality, religion, or political beliefs). However, it is not discrimination to use patient characteristics to estimate prognosis unless a characteristic is used to systematically disadvantage a group. For example age per se (without consideration of prognosis) would be ageist and arguably unlawful discrimination under the Equality Act 2010.10 However, using probability of survival is an ethically defensible criterion.
Based on the RAPR, patients could be classified into three categories. Those whom clinicians are confident have a high probability of survival (and low resource use) should receive the life-sustaining treatment (LST). For example this might be approximately >80% survival, but the absolute threshold will be relative to the numbers of patients needing the LST resource and the availability of the resource at a time. In cases of extreme scarcity, it may be that only those with >90% chance of survival can be treated, whereas in health systems with greater resources relative to demand, the threshold could be lower. The figure may vary over time as the resource availability may change.
Those in the low probability survival group (and high resource use) would usually be given lower levels of care such as ward care or palliative care. Again, the actual figure used to indicate low priority will be relative to resource availability. It might apply to those with <10% survival but it could reach as low as <5% in conditions of relative abundance.
We recognise that there are significant error margins around any figure. Prognostic uncertainty is one of the major problems of a decision-making process for resource allocation,11 but still we must reduce it to a minimum and then we should tolerate the residual uncertainty.
Second level allocation – selection of which patients to save
The first level of allocation aims at saving the greatest number. High RAPR patients should receive the resource. However, there may be more high RAPR patients than there are ventilators. In this case, a different allocation procedure will be needed for this group. Or there may be sufficient ventilators for this group but a large second group of moderate RAPR patients who may not be able to all receive treatment. Principles will be needed to select from this moderate group.
There are several possible policy options. Any or all of these could be used and will be used in different jurisdictions depending on the ethics (including values) and laws of that society. All are potentially ethically defensible.
-
1.
Lottery. A simple lottery or ‘first come, first served’ could be used for this group, or a selection of the group. (As high-priority patients have already been selected for treatment, and low priority selected against treatment, such a lottery would have less impact on overall survival.)
-
2.
Second triage. This could involve either, or both, or sequential assessment of predicted length and quality of life. Utilitarians consider both the expected increase in length and quality of life to be relevant. For example one could set a minimum of 5 years expected of life after treatment as a threshold. This could be used to decide amongst moderate prognosis candidates. Quality of life could also be considered. For example, those with severe impairments of cognition or consciousness (such as late dementia) would not be candidates on this criterion. This may or may not be lawful depending on the legal jurisdiction.10 This option will maximise the quality adjusted life-years (QALY), a standard metric of evaluating the effectiveness of health interventions and used in other areas for resource allocation and decisions about distributive justice.
-
3.
Priority. Priority could be accorded on utilitarian or desert-based grounds to health care workers who have contracted COVID-19 in the course of their work. Priority could also be accorded to younger patients just because they have enjoyed less life, that is, on grounds of desert. For example, the Pittsburgh guidelines recommend the following age categories: 12–40, 41–60, 61–75, and older than 75 yr.4
-
4.
Trial of treatment. Some consideration of equality of opportunity could be afforded to those with uncertain or moderate chances of survival by offering a fixed-term trial of treatment followed by withdrawal. This would address consideration of excessive resource use and still give poorer prognosis patients a chance.
Some of these features (e.g. age) have already contributed to an assessment of probability of survival in the first stage of allocation. In this second phase, they operate more directly. For example, age might be used to prioritise some patients on the basis of desert. That is, even if probability of survival were the same, this would give weight to younger people based on desert considerations. Desert is related to fairness. If you commit a crime, you deserve punishment. If you have had less cake (life), you deserve more. Similarly, a severe cognitive impairment might reduce probability of survival (and be included in the universal assessment) or it might be used as an optional criterion of allocation. Severe cognitive impairment would also affect the ability to appreciate the benefits of a successful treatment.
Quality of life is a hugely contested concept. Broadly, it can be construed subjectively or objectively. Both concepts are ethically defensible and different societies will accept different standards. A subjective assessment is determined by the patient themselves. An objective assessment might include: absence of suffering, happiness, minimal cognitive capacity, full consciousness, capacity to engage in meaningful human relationships.12
It will be up to particular societies to decide whether quality of life should be included or what standard should be employed.
Utilitarianism favours Second Triage and Priority (on grounds of utility, not desert). Egalitarians favour Lottery. Trial of Treatment gives some consideration to both equality and utility.13
Decision-making
Decision-making should be the clinician's ultimate responsibility, in consultation with patients, their families, and colleagues. They will be best-placed to know the facts around patient numbers, need, urgency, resource availability, prognosis, including likely survival and future level of function.
However, decision-making should be informed by the ethical principles and values proposed in this algorithm. At a minimum, every reviewed proposal for allocation of ventilators in the pandemic should include prioritisation of chance of survival. Differences between countries in their chosen approach to allocation (Table 1) are inevitable, and will reflect the ethical choices of particular societies. However, these values must be made explicit and decisions not left to personal values, conscience, intuition, religion, or idiosyncrasy. Algorithmic ethics makes these values and their relationship explicit. How these values are applied will depend on the facts. But we should as a society agree on the ethical values and their relationship. As events such as the COVID-19 pandemic befall us, our values and choices play a significant role in determining who lives and who dies.
Authors' contributions
Conception and drafting of the algorithm: JS
Conception of the table: DW
Writing of the first draft of the manuscript: DW, JS
Elaboration of arguments and addition of clinical detail: DW, MV
Development of arguments and construction of a comparative table: LC
All authors revised the document for critical intellectual input and approved the final version
Declarations of interest
JS reports grants from Wellcome Trust and Uehiro Foundation on Ethics and Education. The other authors report no other conflicts.
Funding
JS and DW received support from the Uehiro Foundation on Ethics and Education, and the Wellcome Trust via the Wellcome Centre for Ethics and Humanties (WT203132) and JS from the Wellcome Trust via the Responsibility and Healthcare project (WT104848). Through his involvement with the Murdoch Children's Research Institute, JS was supported by the Victorian Government's Operational Infrastructure Support Program.
References
- 1.Craxì L, Vergano M, Wilkinson D, Savulescu J. Rationing in a pandemic: lessons from Italy. Asian Bioethics Review (forthcoming). [DOI] [PMC free article] [PubMed]
- 2.Vergano M., Bertolini G., Giannini A. SIAARTI recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances. Minerva Anestesiol. 2020;86:469–472. doi: 10.23736/S0375-9393.20.14619-4. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health Care Excellence COVID-19 rapid guideline: critical care in adults 2020. https://www.nice.org.uk/guidance/ng159/resources/covid19-rapid-guideline-critical-care-pdf-66141848681413 Available at: [PubMed]
- 4.White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA, doi:10.1001/jama.2020.5046. [DOI] [PubMed]
- 5.Daugherty Biddison E.L., Faden R., Gwon H.S. Too many patients a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155:848–854. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 6.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 7.New York State Task Force on Life and the Law and New York State Department of Health . 2015. Ventilator allocation guidelines.https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf Available at: [Google Scholar]
- 8.Savulescu J., Goold I. Freezing eggs for lifestyle reasons. Am J Bioeth. 2008;8:32–35. doi: 10.1080/15265160802248492. [DOI] [PubMed] [Google Scholar]
- 9.Arora C., Savulescu J., Maslen H., Selgelid M., Wilkinson D. The intensive care lifeboat: a survey of lay attitudes to rationing dilemmas in neonatal intensive care. BMC Med Ethics. 2016;17:69–77. doi: 10.1186/s12910-016-0152-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Savulescu J., Cameron J., Wilkinson D. Equality or utility? Ethics and law of rationing ventilators. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han P.K., Klein W.M., Arora N.K. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making. 2011;31:828–838. doi: 10.1177/0272989X11393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilkinson D., Savulescu J. Elsevier; Oxford: 2018. Ethics, conflict and medical treatment for children: from disagreement to dissensus. [PubMed] [Google Scholar]
- 13.Wilkinson D., Savulescu J. Cost-equivalence and pluralism in publicly-funded health-care systems. Health Care Anal. 2018;26:287–309. doi: 10.1007/s10728-016-0337-z. [DOI] [PMC free article] [PubMed] [Google Scholar]