Dear Editor, Since novel coronavirus disease 2019 (COVID‐19), caused by the SARS‐CoV‐2 virus, crossed the Chinese borders and became pandemic, Italy has rapidly become the country with the highest number of patient deaths as well as confirmed and/or hospitalized patients, after China.1 2 On 12 March 2020, Italy was declared a red zone and special protocols were enacted to limit the spread of the virus. Although COVID‐19 does not have an epidermotropism, cutaneous manifestations in patients positive for COVID‐19 have been reported;3 therefore, departments of dermatology are considered at high risk4 and, in order to minimize nosocomial virus spread were ordered to admit only patients needing urgent treatments or undergoing chronic immunosuppressive therapy. Hence, it is crucial to maintain phototherapy services for immunosuppressed dermatology patients who cannot access other treatments, especially during the COVID‐19 emergency.
From 24 February 2020, the Italian Society of Dermatology (SIDeMaST) has produced a series of vademecums2 to protect both healthcare professionals (HRs) and attending patients, and to manage certain patients in high‐risk categories, but no data are currently available on their real‐life application. We describe our real‐life experience and our phototherapy protocols before and during red‐zone declaration in the San Gallicano Dermatological Institute, a primary referral dermatological hospital in Rome, Italy.
Before 12 March 2020, we were treating 62 patients with vitiligo using narrowband ultraviolet B (NB‐UVB); we had 55 patients with psoriasis [45 treated with NB‐UVB, three with psoralen plus UVA (PUVA) and seven displaying palmoplantar psoriasis (treated with 308‐nm monochromatic excimer light)]; 10 patients with parapsoriasis/mycosis fungoides (three treated with PUVA and seven with NB‐UVB); five patients with atopic dermatitis (two treated with UVA1 and three with NB‐UVB); and two patients with localized scleroderma (treated with UVA1). To minimize SARS‐CoV‐2 exposure, a new internal protocol based on telemedicine, triage and treatment (‘3Ts’) was applied (Figure 1), as follows.
Figure 1.
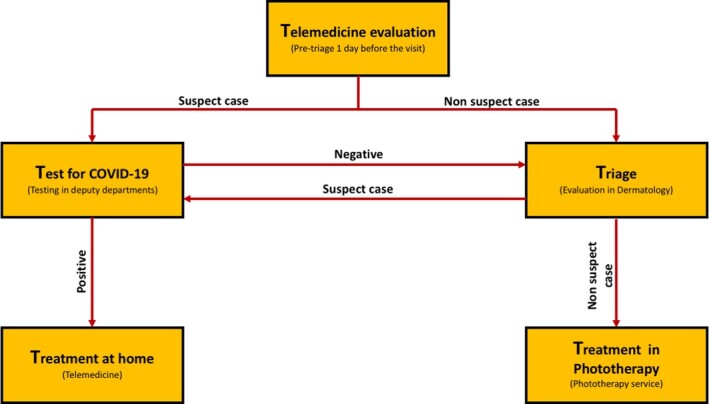
Telemedicine, triage, treatment (3T) protocol for admission to phototherapy.
Firstly, via telemedicine, patients due to attend the service the next day undergo a phone call pre‐triage in which HRs ask about presence of fever (temperature 37·5 °C/99·5 °F), sore throat, rhinorrhoea, cough, cold and flu‐like symptoms; contact with patients confirmed or in quarantine for COVID‐19; or recent trips (< 14 days) to other high‐risk countries.
Secondly, through triage, if patients pass the pre‐triage they are authorized to access the hospital where they undergo a secondary face‐to‐face triage verifying the pre‐triage COVID‐19 criteria.
Thirdly, patients undergo treatment: after preliminary physician examination, patients receive phototherapy (UVA1 or NB‐UVB) delivered only by ramps equipped with 13 Philips TL 01 NB‐UVB lamps (fitted with TL 100‐W fluorescent tubes; Philips, Amsterdam, the Netherlands), and not by booths, which are difficult to sanitize. Both HRs and dermatologists go into another room and communicate with the patient using a microphone and speaker system to minimize contact. Ramps and the entire treatment room are sanitized after each patient by cleaning all of the surfaces, including the floor up to 1 m from the lamps, with a hydroalcohol solution containing glutaraldeyde. HRs and physicians wash their hands and brush the subnail region after each patient. Any HRs in direct contact with patients wear the suggested personal protective equipment (mask model N95 with a FFP2 filter protecting, gloves and protective glasses).5 Patients are encouraged to wear the provided mask entering the phototherapy area and to remove it only during the treatment. Everyone is instructed to maintain a safety distance of 2–3 m.
Patients suspected of COVID‐19 infection are tested. In confirmed cases, patients can receive a prescription after undergoing a teledermatological evaluation from home via Skype. Patients with a negative test result can undergo triage in dermatology.
As this protocol does not permit us to perform the same number of visits normally given, we were forced to assign priorities based on disease morbidity, severity and risk or erythroderma (dermatological emergency). Thus, for patients with vitiligo we decided to interrupt NB‐UVB and switch them to self‐application of tacrolimus ointment (0·1% for lesions located in resistant sites and 0·03% for sensitive areas, including eyelids) plus systemic antioxidants to continue melanocyte stimulation previously triggered by phototherapy. For patients with psoriasis we opted to maintain NB‐UVB only in patients with Psoriasis Area and Severity Index (PASI) > 10 or in patients with rupioid psoriasis. Conversely, patients with PASI < 10 were switched to topical corticosteroids and, if highly keratotic we added a keratolytic agent. Owing to the well‐known immunosuppressive effects of PUVA,6 all patients undergoing this treatment were shifted to NB‐UVB with or without retinoids. Patients with poorly infiltrated but generalized parapsoriasis and mycoses fungoides continue NB‐UVB. In atopic dermatitis, only patients with Eczema Area and Severity Index > 10 or ScORing Atopic Dermatitis > 30 continue phototherapy and do not switch to topical corticosteroids; in particular, patients undergoing UVA1 were switched to NB‐UVB in order to decrease the number of visits (five vs. three), and also because UVA1 beds are difficult to sanitize efficiently. All patients with scleroderma undergoing UVA1 were switched to topical corticosteroids. After these decisions only 38 patients will continue NB‐UVB (31 with psoriasis, 10 with parapsoriasis/mycosis fungoides and three with atopic dermatitis).
In conclusion, during the COVID‐19 emergency, we believe that phototherapy represents an important resource for treating immunosuppressed at‐risk dermatology patients. HRs and dermatologists should carefully follow COVID‐19 preventive recommendations.
Acknowledgments
we thank Professor Thomas McCormick for the editing and suggestions.
Contributor Information
A. Pacifico, S. Gallicano Dermatological Institute IRCCS Rome Italy
M. Ardigò, S. Gallicano Dermatological Institute IRCCS Rome Italy
P. Frascione, S. Gallicano Dermatological Institute IRCCS Rome Italy
G. Damiani, Clinical Dermatology IRCCS Istituto Ortopedico Galeazzi Milan Italy Young Dermatologists Italian Network Centro Studi GISED Bergamo Italy.
A. Morrone, S. Gallicano Dermatological Institute IRCCS Rome Italy
References
- Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; 323:1545–6. [DOI] [PubMed] [Google Scholar]
- Società Italiana di Dermatologia (SIDeMaST). I vademecum di SIDeMaST nell'emergenza Coronavirus. Available at: https://www.sidemast.org/blog/tag/corona-virus (last accessed 1 May 2020).
- Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020; 34:e212–3. [DOI] [PubMed] [Google Scholar]
- Tao J, Song Z, Yang L et al. Emergency management for preventing and controlling nosocomial infection of the 2019 novel coronavirus: implications for the dermatology department. Br J Dermatol 2020; 182:1477–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan Y, Chen H, Chen L et al. Consensus of Chinese experts on protection of skin and mucous membrane barrier for healthcare workers fighting against coronavirus disease 2019. Dermatol Ther 2020; 10.1111/dth.13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich SE, Alcalay J, Applegate LA, Kripke ML. Immunosuppression in phototherapy. Ciba Found Symp 1989; 146:131–9. [DOI] [PubMed] [Google Scholar]


