Abstract
Background
The COVID‐19 pandemic has resulted in the implementation of rapidly changing protocols and guidelines related to the indications and perioperative precautions and protocols for tracheostomy. The purpose of this study was to evaluate current guidelines for tracheostomy during the COVID‐19 pandemic to provide a framework for health systems to prepare as the science evolves over the upcoming months and years.
Methods
Literature review was performed. Articles reporting clinical practice guidelines for tracheostomy in the context of COVID‐19 were included.
Results
A total of 13 tracheotomy guidelines were identified. Two were available via PubMed, five in society or organization websites, and six identified via health system websites or other sources. Five were from Otolaryngology‐Head and Neck Surgery specialties, six from Anesthesiology and one from Pulmonary/Critical Care. All (100%) studies recommended postponing elective OR cases in COVID‐19 positive patients, while seven recommended reducing team members to only essential staff and three recommended forming a designated tracheostomy team. Recommendations with supporting references are summarized in the article.
Conclusions
Tracheostomy guidelines during the COVID‐19 pandemic vary by physician groups and specialty, hospital systems, and supply‐chain/resource availability. This summary is provided as a point‐in‐time current state of the guidelines for tracheotomy management in April 2020 and is expected to change in coming weeks and months as the COVID‐19 pandemic, virus testing and antibody testing evolves.
Keywords: COVID‐19, coronavirus, recommendations, tracheotomy, tracheostomy
1. INTRODUCTION
The first cases of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), the virus causing coronavirus disease (COVID‐19), were first reported as only a few cases in rural China and has now grown into a global pandemic. While this virus does not appear to be as deadly as the coronavirus outbreak in 2003 known as SARS, it unfortunately has proven to be much more easily transmitted and infectious. SARS‐CoV‐2 has an incubation period of an estimated 4 days and a relatively slow onset of symptoms, allowing infected persons to unknowingly transmit the virus. 1 Newer evidence also suggests a significant percentage of carriers of the virus may remain asymptomatic, thus making transmission more difficult to contain. 2
Although most cases range from relatively asymptomatic to mild flu‐like symptoms and progress with anosmia, ageusia, fever and cough, approximately 20% to 30% of COVID‐19 patients require admission to the intensive care unit (ICU) for respiratory support. 3 This rapid influx of patients has challenged health care institutions, hospitals, and medical practitioners alike. In response, many guidelines for care of COVID‐19 patients continue to be updated by the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), hospitals, and individual societies from around the world.
Due to the spread of COVID‐19 through aerosol and fine droplets, medical personnel are in direct danger of occupational exposure while caring for these patients. This is especially true for aerosol‐generating airway procedures including upper aerodigestive tract endoscopy, intubation, and mucosal entry which can potentially expose everyone involved in these cases. 4 A report from the outbreak in Wuhan, China warns that otolaryngologists‐head and neck surgeons are exceptionally at risk, citing an event in which 14 medical personnel contracted COVID‐19 during an endoscopic pituitary surgery. 5 Additionally, studies in Italy have revealed that otolaryngologists‐head and neck surgeons are exposed to the greatest risk of infection while caring for COVID‐19 positive patients. 6 Therefore, the risk posed to otolaryngologists‐head and neck surgeons during many commonly performed surgeries cannot be understated. A statement from American Academy of Otolaryngology—Head and Neck Surgery “strongly recommends that all otolaryngologists‐head and neck surgeons provide only time‐sensitive or emergent care” in order to mitigate this risk. 7 Tracheostomies and tracheostomy care, however, may play a critical role in the management of COVID‐19 patients and the main indications are: prolonged intubation (due to risks for subglottic stenosis and laryngeal stenosis), and limiting use of resources such as ventilators and sedatives (which may be in short supply). While these interventions may be necessary to provide adequate care, they are also high‐risk procedures which demand special precautions be taken in order to mitigate occupational risk.
The COVID‐19 pandemic has resulted in the implementation of rapidly changing protocols and guidelines related to the indications and perioperative precautions and protocols for tracheotomy. Tracheotomy, resource and supply chain concerns, and aerosolization of virus has resulted in this procedure receiving widespread attention and new guidelines. As this procedure is often performed by otolaryngologist‐head and neck surgeons, general surgeons, critical care physicians and exposure risks to operating rooms, ventilators, ICUs, nurses, respiratory therapists among others, hospitals have developed rapidly evolving protocols (Figure 1). The purpose of this study was to evaluate current guidelines for tracheostomy during the COVID‐19 pandemic to provide a framework for health systems to prepare as the science evolves over the upcoming months and years.
FIGURE 1.
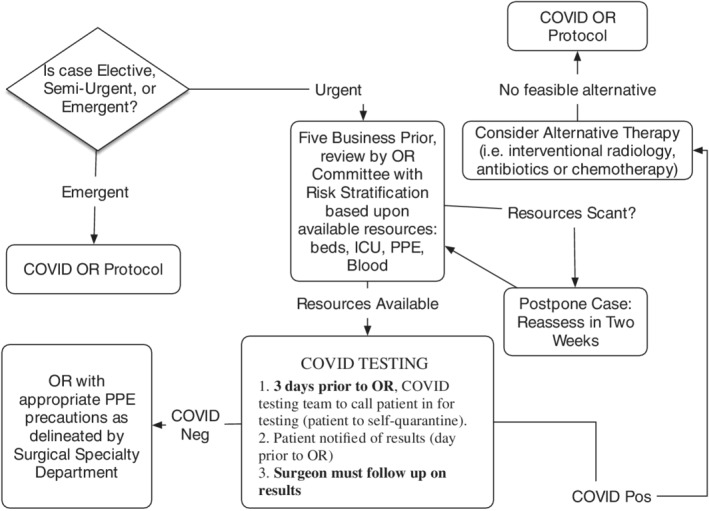
Flow diagram for operating room cases
The purpose of this study was to evaluate the current practice guidelines and recommendations in regards to COVID‐19 as they pertain to tracheostomy and provide a collective summary of recommendations. Individual or institutional‐specific guidelines have been published from groups around the world to guide medical personnel during aerosol‐generating procedures, such as a tracheostomy. It is essential that all those potentially involved are aware of these guidelines and implement them when appropriate.
2. METHODS
2.1. Literature review and evidence collection
A literature review was performed searching for all published English‐language literature reporting on clinical practice guidelines pertaining to tracheostomy in the context of COVID‐19. A search strategy was employed with the following search strings: “covid OR covid‐19 OR coronavirus” with “tracheostomy OR tracheotomy OR tracheostomy change” in the last 5 years. Gray literature (literature that is not commercially published) was identified by searching the websites of governmental health agencies, professional associations, and other medical societies. Google search engine was used to search for additional information. These searches were supplemented by references of relevant individual articles. Results were limited to articles in the English language. After the completed search, a total list of records was obtained, and duplicates removed. A final list of full text articles was then compiled, and one author independently screened each article.
3. DISCUSSION
A total of 13 tracheotomy guidelines were identified (Table 1). Two were available via PubMed, five in society or organization websites, and six identified via health system websites or other sources. Five were from Otolaryngology‐Head and Neck Surgery specialties, six from Anesthesiology and one from Pulmonary/Critical Care.
TABLE 1.
Included studies
| Author/source | Title | Year |
|---|---|---|
| American Academy of Otolaryngology—Head and Neck Surgery | Otolaryngologists and the COVID‐19 Pandemic | 2020 |
| Parker et al | Tracheotomy recommendations during the COVID‐19 Pandemic | 2020 |
| National Tracheostomy Safety Project | NTSP considerations for tracheostomy in the COVID‐19 outbreak | 2020 |
| American Society of Anesthesiologists | COVID‐19 Resources for Anesthesiologists | 2020 |
| Anaesthesiologists WFoSo | Coronavirus—guidance for anesthesia and perioperative care providers | 2020 |
| Brewster et al | Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group | 2020 |
| Kong et al | Infographic for Principles of Airway Management in COVID‐19 | 2020 |
| Harrison et al | Guidance for surgical tracheostomy and tracheostomy tube change during the COVID‐19 Pandemic | 2020 |
| Wax et al | Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019‐nCoV) patients | 2020 |
| Chen et al | Perioperative Management of Patients Infected with the Novel Coronavirus: Recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists | 2020 |
| Respiratory Care Committee of Chinese Thoracic Society | Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia | 2020 |
| Zucco et al | Perioperative Considerations for the 2019 Novel Coronavirus (COVID‐19) Anesthesiology Patient Safety Foundation | 2020 |
| Wei et al | Safe tracheostomy for patients with severe acute respiratory syndrome | 2020 |
Tracheostomies are a common surgical procedure performed by otolaryngologists‐head and neck surgeons and other specialties in both the emergent and elective setting. In the COVID‐19 population, special consideration must be given in evaluating the urgency and indications for performing tracheostomy. If possible, delaying tracheostomy until patients clear the virus should be the primary recommendation. Additionally, there may be some expanding indications in the COVID‐19 patient population. As COVID‐19 patients wean off the ventilator, some may be at high risk for requiring noninvasive ventilation or reintubation. Both instances have been noted to be aerosol‐generating events and should be avoided when possible. Ventilation using a tracheostomy may aide in weaning off of the ventilator and allow for decreased sedation, however it is important to highlight that after tracheostomy, there is significant risk of aerosolization when the patient coughs or is suctioned, which puts staff at risk. 8 Discussion between intensive care and otolaryngology teams should take place as well as discussion regarding percutaneous vs open tracheostomy. The main motivators for performing tracheostomy will likely be resource‐based, such as availability of ventilators, ICU beds and sedative constraints, rather than patient‐based factors. In patients testing positive for COVID‐19, this summary of recommendations serves as a guideline along with institutional protocols.
3.1. Elective tracheostomy in COVID‐19 positive patients
3.1.1. General precautions
COVID‐19 positive patients should postpone elective cases until testing negative, if possible.9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Two tests 48 hours apart, depending on test method, may be necessary due to the false negative rate of testing.
If resources allow, test all tracheostomy patients for COVID‐19 within 48 hours prior to surgery.9, 10, 13, 15, 17, 18
Allow adequate time for education and rehearsal with staff prior to donning necessary PPE, as N95 masks can make communication difficult. This will ensure all involved parties are adequately informed and operate smoothly.9, 10, 12, 13, 14, 15, 17, 18
Tracheostomy should be avoided in patients with respiratory instability. 8
Mechanical ventilator parameters should be carefully considered. Many institutions recommend >21 days of ventilation with lower ventilator settings (40%‐50% FiO2, PEEP <12. In addition, the severity of the patients overall illness must be taken into account. Patient should be without bleeding diathesis or the need for vasopressive agents.
Airborne precautions should be followed by all team members that are present.9, 10, 11, 12, 13, 14, 15, 16, 17, 18
3.1.2. Location
The operation should be performed in an ICU room or operating room, preferably with negative pressure and a HEPA filtration system. ICU may be preferable to operating room, even given negative aspects of limited surgical access due to ICU bed, as it decreased the risks inherent in transport of the patient (eg, need to disconnect circuit for transfer, increased risk of disconnection, manual ventilation, etc.). Consider positioning the patient closer to the surgeon prior to beginning the procedure.9, 11, 13, 14, 16, 17, 18
If necessary to move the patient, care should be taken when transporting the patient to the operating room. Designate a team member to remain clear of contact with the patient and interact with the environment.
3.1.3. Personnel
Reduce team members to only essential staff. Consider one surgeon, one anesthesiologist, and one surgical staff member. Additional team members may remain on standby outside of the room.9, 10, 12, 13, 14, 15, 17
Procedure should be performed by the most experienced staff to maximize safety and efficiency. Trainees only to be present if attending physician is not available.9, 10, 12, 13, 14, 15, 16
Consider forming a “designated tracheostomy team” to limit inexperienced staff during COVID‐19 positive procedures, as well as including an infection control nurse (or designated individual) to ensure all team members comply with infection control processes to limit transmission to other team members.9, 13, 17
3.1.4. Equipment
All personnel should be equipped with the proper PPE, including an N95 mask or purified air purifying respirator (PAPR) device, eye goggles, transparent full‐face shield, gown, and double gloves.9, 10, 11, 12, 13, 14, 15, 16, 17, 18
PPE equipment should be readily available in the area where COVID‐19 positive patients are managed.9, 10, 11, 12, 13, 14, 15, 16, 17, 18
Surgical tracheotomy tray. 19
Viral filter is recommended, or at minimum a heat and moisture exchanger (HME) device.9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Avoid disconnecting HME; if necessary, disconnect distal to HME.
Closed suction system. If patient is not mechanically ventilated, tracheostomy hub should be connected to a closed system identical to those used when a patient is connected to a mechanical ventilator.9, 10, 11, 13, 14, 15, 16, 17, 18
3.1.5. Intraoperative techniques
Limit use of suction and electric cautery. 19
Establish complete paralysis using neuromuscular blockade to prevent coughing and aerosol dispersion.4, 7, 8, 13, 17, 18
Maintain adequate pre‐oxygenation (100%) for 5 minutes10, 12, 13, 14, 16, 17 prior to tracheotomy.
After tracheostomy placement, connect patient to ventilator with viral filter10, 11, 12, 13, 14, 16, 17, 18 and confirm end tidal CO2 and tidal volumes.
Check for proper inflation and monitor any evidence of cuff leaks.8, 9, 11, 15
Suture the tube to the skin and strap separately. 19
After removing endotracheal tube, place facemask on patient to protect against dispersion should the patient cough. 18
Doffing of PPE and disposal of tools according to institutional protocol.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19
3.2. Emergency tracheostomy in COVID‐19 positive or unknown patient
The risk of emergent airway should be balanced with situation‐specific prognostic factors that may indicate a low likelihood of favorable patient outcome.
In the event of an airway emergency in which endotracheal intubation is unable to be achieved and a tracheostomy is indicated, the guidelines above should be followed as much as possible.
An emphasis should be placed on safety of medical personnel through the proper use of PPE. Review and implementation of these guidelines can limit confusion and unnecessary occupational exposure to staff.9, 15, 19
3.3. Tracheostomy management in COVID‐19 positive patients
3.3.1. General precautions
Patient management should comply with all institutional guidelines for patients with COVID‐19 who require oxygenation/hospitalization. 9
Encourage the patient to perform as much of the cleaning and care as possible. 9
Staff caring for this patient set should be properly educated on COVID‐19 airway management (such as using closed suctioning, cannula care), as these are high‐risk (to staff) scenario.9, 15
PPE and airborne/droplet precautions should be followed according to institutional protocol.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19
Tracheostomy change procedures should be delayed until patient no longer tests positive and cuffed tracheostomy tube left in place with cuff inflated until that time.8, 9, 15
3.3.2. Ventilated patients
3.3.3. Nonventilated patients
Cuffed, nonfenestrated tracheostomy tubes should be used and remain inflated to limit aerosol generation.9, 10, 12, 14, 15, 19
Viral filter is recommended, or at minimum (HME) device should be placed on the tracheostomy tube.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19
A simple facemask should be placed on the patient.9, 11, 17, 18
Any suctioning should be done using a closed system.9, 10, 11, 12, 13, 14, 15, 16, 18, 19
Should supplemental oxygenation be needed, a closed T‐piece is preferable due to its protection against droplet spread. 9
4. LIMITATIONS
This study evaluated the current practice guidelines and recommendations for tracheostomy during the SARS‐CoV‐2 outbreak to provide a collective summary for otolaryngologists‐head and neck surgeons in this difficult time. However, we acknowledge the inherent limitations of this study. Although we included all published literature to date, this was limited only to those published before March 31st, 2020. As more is learned about SARS‐CoV‐2 and more data becomes available, it is possible that the guidelines may change or be altered as a result. Still, this is the most up‐to‐date collection of clinical guidelines for tracheostomy with respect to the SARS‐CoV‐2 outbreak available at this time. Further studies are needed to determine the efficacy of these guidelines, and in order to establish recommendations for similar viral epidemics in the future.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Heyd CP, Desiato VM, Nguyen SA, et al. Tracheostomy protocols during COVID‐19 pandemic. Head & Neck. 2020;42:1297–1302. 10.1002/hed.26192
REFERENCES
- 1. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lai CC, Liu YH, Wang CY, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2): facts and myths. J Microbiol Immunol Infect = Wei mian yu gan ran za zhi. 2020. 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020. 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tran K, Cimon K, Severn M, Pessoa‐Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Patel ZM, Hwang PH, Nayak JV, Dodd R, Sajjadi H, Jackler RK. Precautions for endoscopic transnasal skull base surgery during the COVID‐19 pandemic. 2020. https://neurosurgery.directory/2020/04/03/precautions-for-endoscopic-transnasal-skull-base-surgery-during-the-covid-19-pandemic/. [DOI] [PMC free article] [PubMed]
- 6. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020. https://onlinelibrary.wiley.com/doi/pdf/10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Otolaryngologists and the COVID‐19 Pandemic. American Academy of Otolaryngology—Head and Neck Surgery. 2020. https://www.entnet.org/content/otolaryngologists-and-covid-19-pandemic. [DOI] [PubMed]
- 8. Parker NP, Fritz MA, Rapoport SK, et al. Tracheotomy recommendations during the COVID‐19 pandemic. Am Acad Otolaryngol—Head Neck Surg. 2020. https://www.entnet.org/content/tracheotomy-recommendations-during-covid-19-pandemic. [Google Scholar]
- 9.NTSP Considerations for Tracheostomy in the COVID‐19 Outbreak. National Tracheostomy Safety Project. 2020. https://d3n8a8pro7vhmx.cloudfront.net/gtc/pages/1/attachments/original/1584713595/NTSP-COVID-19-tracheostomy-guidance-20-Mar-2020.pdf?1584713595
- 10.COVID‐19 Resources for Anesthesiologists. American Society of Anesthesiologists. 2020. https://www.asahq.org/about-asa/governance-and-committees/asa-committees/committee-on-occupational-health/coronavirus
- 11. Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia. Zhonghua jie he he hu xi za zhi = Zhonghua jiehe he huxi zazhi = Chin J Tuberc Respir Dis. 2020;17:E020 10.3760/cma.j.issn.1001-0939.2020.0020 [DOI] [PubMed] [Google Scholar]
- 12. Anaesthesiologists WFoSo . Coronavirus—Guidance for Anaesthesia and Perioperative Care Providers 2020. https://www.wfsahq.org/latest-news/latestnews/943-coronavirus-staying-safe. [Google Scholar]
- 13. Brewster NCC DJ, Do TBT, Fraser K, et al. Consensus statement: safe airway society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. Med J Aust. 2020. https://www.mja.com.au/journal/2020/consensus-statement-safe-airway-society-principles-airway-management-and-tracheal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kong DoAaIC‐TCUoH . Infographic for Principles of Airway Management in COVID‐19. 2020. https://www.aic.cuhk.edu.hk/covid19/.
- 15. Laura Harrison JR, Winter S. Guidance for Surgical Tracheostomy and Tracheostomy Tube Change during the COVID‐19 Pandemic. ENT UK. 2020. https://www.entuk.org/tracheostomy-guidance-during-covid-19-pandemic.
- 16. Liana Zucco NL, Ketchandji D, Aziz M, Ramachandran SK. Perioperative Considerations for the 2019 Novel Coronavirus (COVID‐19) Anesthesiology Patient Safety Foundation. 2020. https://www.apsf.org/news-updates/perioperative-considerations-for-the-2019-novel-coronavirus-covid-19/.
- 17. Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019‐nCoV) patients. Can J Anesth/J Can d'anesth. 2020;67:568‐576. 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen X, Liu Y, Gong Y, Guo X, Zuo M, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the joint task force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020. 10.1097/ALN.0000000000003301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wei WI, Tuen HH, Ng RWM, Lam LK. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope. 2003;113(10):1777‐1779. 10.1097/00005537-200310000-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]


