Abstract
BACKGROUND/OBJECTIVES
The COVID‐19 pandemic has massively disrupted essential clinical research. Many regulatory organizations have rightfully advocated to temporarily halt enrollment and curtail all face‐to‐face interactions. Views and opinions of patients and their caregivers are seldom considered while making such decisions. The objective was to study older participantsʼ and their caregiversʼ perspectives to participate in ongoing clinical research during the COVID‐19 pandemic.
DESIGN
Cross‐sectional.
SETTING
VISN‐16/Geriatric Research, Education and Clinical Center (GRECC), Department of Veterans Affairs.
PARTICIPANTS
Older participants and their caregivers (N = 51) enrolled in ongoing clinical research studies.
MEASUREMENTS
Questions about perceptions of safety to attend research visit, the level of panic among the general public, and medical centerʼs preparedness in handling the pandemic. Other questions identified the source of pandemic information and the preference of a phone or in‐person visit.
RESULTS
Mean age was 69.3 (±9.4) years, 53% were male, 39% were caregivers, and 65% were Caucasian. Majority (78%) of the participants felt safe/very safe attending the scheduled research appointment; 63% felt that the extra screening made them feel safe/very safe; 82% felt that the medical center was prepared/very prepared for the pandemic. Participants split evenly on their preference for phone versus in‐person visits. Family members and television news media were the commonly used sources of pandemic information irrespective of their education. Perceptions were influenced by gender and source of information, not by age or education. Females perceived higher level of panic compared to males (P = .02). Those relying on news media felt safer compared to those that relied on family members (P = .008).
CONCLUSION
Even though informants felt that the medical center was prepared to handle the pandemic, only half the participants preferred the in‐person visit. Pandemic information was obtained from family members or the television news media. Knowing patientsʼ perspectives may help researchers be better prepared for future pandemics. J Am Geriatr Soc 68:E14–E18, 2020.
Keywords: patient perspectives, COVID‐19, pandemic
Pandemics unfortunately, are not infrequent events anymore. Even after controlling for disease surveillance, communications, geography, and host availability, the total number and diversity of outbreaks have increased significantly since 1980.1 Historically, low and middle income countries have borne the burden of infectious disease outbreaks, but more recently pandemics have exposed the lack of preparedness in well‐connected, economically‐stable, developed countries. Although patient‐centered research is critical during pandemics, each pandemic brings huge disruptions in essential clinical research.2 Coronavirus Disease (COVID‐19), with its asymptomatic transmission, symptoms mimicking those of influenza, and a human‐to‐human transmission rate of 4, has attained a pandemic state and exposed the vulnerability of our clinical research enterprise.3
Many national organizations such as the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), and the Office of Research and Development (ORD), have indicated research visits to be nonessential.4, 5 They have advocated, rightfully so, to temporarily halt study enrollment and curtail face‐to‐face interactions. As the principal investigators (PI) weigh in ethical principles, local/national guidance, staffing strain, and the risk involved to each participant to ultimately decide the course of action for their clinical trials, they seldom examine patientʼs and caregiverʼs views and opinions.6
Clinical research depends primarily on the willingness of research participants to volunteer. Hence, it is important to learn the factors that shape oneʼs willingness to participate in clinical research particularly during a pandemic. The general public is supportive of clinical research in general, and even during pandemics.7, 8 Gobat et al. (N = 6,804) reported that 82% of the participants considered that it was important to conduct medical research during epidemics.8 The authors concluded that greater knowledge about pandemics, trust in health professionals, and trust in the government predicted an increase in willingness to participate in research.8 Others report that participants sometimes rely on an instinctive decision‐making style, which may be enhanced during pandemics.2 Negative psychological effects of quarantine including post‐traumatic stress symptoms, confusion, and worry that their family members may contract COVID‐19, can influence oneʼs willingness to participate in clinical research.3, 9 Others emphasize the importance of research during pandemics and that participantsʼ age, prior involvement in research, and complexity of the proposed research study to be determinants of participatory decisions.7, 10, 11 The goal was to study the perspectives of the older patients and their caregivers to participate in ongoing clinical research during the COVID‐19 pandemic.
METHODS
This study was developed to capture older patient and caregiver perspectives regarding participation in clinical research during the COVID‐19 pandemic. Five questions with 5‐point Likert scales were used to quantitatively evaluate participant perspectives. These questions included participantsʼ perception of safety to attend the visit, the level of panic among the general public, medical centerʼs preparedness in handling the pandemic, the safety associated with the extra screening at the entrance and if they would recommend others to attend their medical appointments. Two additional questions identified the source of information about the pandemic and the participants preferences of whether to attend in‐person or via a phone visit. While responding to the source of information they were encouraged to pick the most commonly used resource if they had relied on more than one source.
Interviews were conducted from March 4, 2020 to March 18, 2020 before the ORD released the guidance to temporarily halt all in‐person research visits unless such a halt would be detrimental to the participants. Veterans and their caregivers (N = 51) that were enrolled in several ongoing clinical research studies at the VISN16 Little Rock Geriatric Research, Education and Clinical Center (GRECC) were interviewed either during their in‐person visit or via phone if they had canceled/postponed the visit. They were all participants from ongoing geriatric clinical research studies pertaining to mild cognitive impairment, and major neurocognitive disorder with and without behavioral problems.
Statistical Analysis
Descriptive statistics were obtained that included frequencies, percentages, means, standard deviations, medians, and 25th and 75th percentiles for demographic and/or general perception variables, as appropriate. A two‐independent‐sample t‐test or a Wilcoxon rank‐sum test was performed to compare certain groups with respect to each of five perception variables. While analyzing the information source variable, only the group relying on a family member and the group relying on TV as the source were compared due to the small numbers of respondents relying on other modalities. Also, a chi‐square test was performed to test for an association between a binary education variable (high school or less and greater than high school) and the information source variable (family member and TV). A 5% significance level was used. SAS Enterprise Guide 7.15 (SAS Institute, Cary, NC) was utilized to perform the statistical analyses.
RESULTS
A total of 51 Veterans/caregivers were interviewed that were scheduled for ongoing clinical research studies over a period of 2 weeks surrounding increased surveillance for COVID‐19. Of these, 31 were Veterans while 20 were caregivers. Mean age was 69.3 (±9.4) years, 53% were male, 39% were caregivers, and 65% were Caucasian (Table 1). Mean education was 12.8 (±2.3) years. Majority (78%) of the participants felt safe/very safe attending the scheduled research appointment (40 reported feeling safe ≥4 on a Likert scale of 1‐5); 66% felt that the extra screening made them feel safe/very safe; 82% felt that the medical center was prepared/very prepared for the pandemic (Figure 1). Although the majority responded that the general public was panicked/very panicked about the pandemic (86%), they reported that they would likely/very likely recommend others to keep their medical appointments (82%) (Figure 1).
Table 1.
Demographics and Descriptive Statistics for Perception Variables (N = 51)
| Variable | ||
|---|---|---|
| Categorical variables | n | % |
| Age | ||
| ≤65 years | 18 | 35.3 |
| >65 years | 33 | 64.7 |
| Gender (male) | 27 | 52.9 |
| Participants (participants only) | 31 | 60.8 |
| Race | ||
| Caucasian | 33 | 64.7 |
| African American | 18 | 35.3 |
| Education | ||
| ≤High school | 31 | 60.8 |
| >High school | 20 | 39.2 |
| Perception variables (N = 51) | Mean | SD |
| How safe do you feel in coming for this research visit? | 4.3 | 1.1 |
| What do you think of the preparedness of the VA in handling COVID 19? | 4.3 | 0.9 |
| How safe did the extra screening at the entrance make you feel?a | 4.1 | 1.0 |
| How likely are you to recommend others to keep their medical appointments? | 4.2 | 0.9 |
| How panicked do you think the general public is about COVID 19? | 4.5 | 0.8 |
There was one missing value for this variable.
Figure 1.
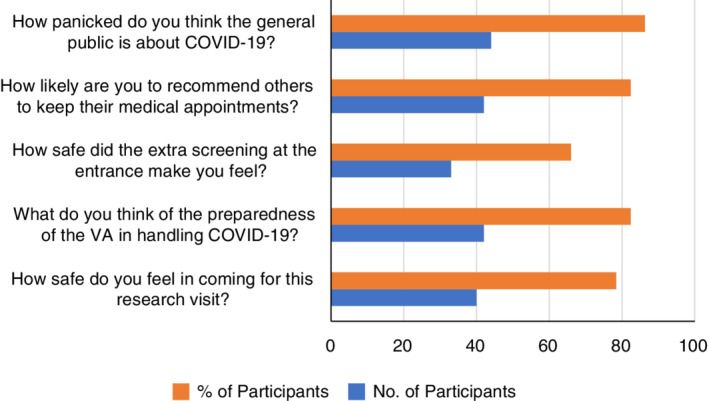
Frequencies and percentages associated with responses of ≥4 for 5 perception variables where 5 was the highest response on a 5‐point Likert scale of 1 to 5 (N = 51).
Phone visit was not deemed appropriate for four participants as they received daily intervention as part of the ongoing study. The remaining participants split evenly on their preference for phone versus in‐person visits (Table 2). Although several sources were sought out by the participants for information about the pandemic, family members (n = 24) and TV (n = 16) were the most commonly used modalities by this cohort. Veterans Affairs (VA) media or Facebook was used third most commonly by the respondents (10.2%). Two people had signed up for the CDC newsletter, and two others were not following news about the pandemic at all. There was no association between the binary education variable (high school or less and greater than high school) and the information source variable (considering only the family member group and the TV group) (P = .6847).
Table 2.
Respondent Characteristics and Perception about COVID‐19 Pandemica
| Perception variable | Safety | Preparedness | Screeningb | Recommendation | Panic |
|---|---|---|---|---|---|
| Age | |||||
| ≤65 (n = 18) | 5.0 (4.0, 5.0) | 4.4 (0.6) | 4.3 (0.8) | 4.5 (0.6) | 4.7 (0.6) |
| >65 (n = 33) | 5.0 (3.0, 5.0) | 4.2 (1.1) | 4.0 (1.1) | 4.1 (1.0) | 4.3 (0.9) |
| Gender | |||||
| Male (n = 27) | 4.4 (1.1) | 4.4 (0.9) | 4.1 (1.1) | 4.2 (1.0) | 4.2 (0.9) |
| Female (n = 24) | 4.1 (1.2) | 4.1 (0.9) | 4.1 (0.9) | 4.3 (0.9) | 4.8 (0.7)e |
| Education | |||||
| ≤High school (n = 31) | 4.3 (1.2) | 4.2 (0.9) | 4.1 (1.0) | 4.2 (0.9) | 4.5 (0.8) |
| >High school (n = 20) | 4.3 (1.2) | 4.3 (1.0) | 4.1 (1.1) | 4.3 (1.0) | 4.4 (0.9) |
| Participant/caregiver | |||||
| Participant (n = 31) | 4.3 (1.2) | 4.3 (0.9) | 4.0 (1.1) | 4.2 (0.9) | 4.4 (0.8) |
| Caregiver (n = 20) | 4.2 (1.2) | 4.3 (1.0) | 4.3 (1.0) | 4.4 (1.0) | 4.7 (0.8) |
| Phone visit preferencec | |||||
| Yes (n = 23) | 3.7 (1.4) | 3.7 (1.1) | 3.8 (1.1) | 3.7 (1.1) | 4.8 (0.4) |
| No (n = 23) | 4.7 (0.6)f | 4.7 (0.5)f | 4.3 (1.0) | 4.6 (0.6)f | 4.1 (1.0)f |
| Information sourced | |||||
| Family member (n = 24) | 3.9 (1.4) | 4.0 (1.2) | 4.1 (1.1) | 4.0 (1.1) | 4.5 (0.8) |
| TV (n = 16) | 4.8 (0.5)f | 4.6 (0.6)e | 4.2 (1.0) | 4.6 (0.7) | 4.6 (0.7) |
The summary statistics are given as mean (standard deviation), except for safety with respect to age where median is reported along with 25th and 75th percentiles. In that instance, a Wilcoxon rank‐sum test was utilized.
There was one missing value for this variable.
Only “Yes” and “No” responses were analyzed. There were four “N/A" responses and one missing value.
Only “Family Member” and “TV” responses were analyzed. There were nine responses other than “Family Member” and “TV” and two missing values.
P value <.05.
P value <.01.
Some perception about the pandemic appears to be influenced by gender and the source of information but not by age or educational status. There was a significant difference between males and females regarding the mean perceived level of panic in the general public (P = .02) with the mean perceived level of panic being higher among females (4.8 vs 4.2) (Table 2). Also, there was a significant difference between those who rely on TV compared to those who rely on family members for information about the pandemic in terms of mean perceived level of safety in coming for a research visit (p = .008) with those relying on TV feel safer (4.8 vs 3.9) to come for their in‐person visit. Additionally, there was a significant difference between those who preferred an in‐person visit and those that preferred a phone visit with respect to the mean perceived level of safety in coming for a research visit (P = .003) with those preferring an in‐person visit feeling safer (4.7 vs 3.7), mean perceived level of preparedness of the medical center in handling COVID‐19 (P = .001) with those preferring an in‐person visit perceiving a higher level of preparedness (4.7 vs 3.7), mean likelihood level of recommending others to keep their medical appointments (P = .002) with the likelihood level being higher among those preferring an in‐person visit (4.6 vs 3.7), and mean perceived level of panic in the general public about COVID‐19 (P = .005) with those preferring an in‐person visit perceiving a lower level of panic (4.1 vs 4.8). No statistically significant differences were found between the Veterans and the caregivers.
DISCUSSION
We present perspectives of participants and their caregivers from ongoing psychogeriatric clinical research trials. Majority of the participants felt safe to attend the scheduled appointments, that the Medical Center was well‐prepared for the pandemic, and that the extra screening made them feel safer. Interestingly, participants felt safe to come‐in for their appointments despite endorsing high levels of panic the general public had about the pandemic. Although these results of willingness to participate are in keeping other research studies conducted during pandemics, they could change vastly as the COVID‐19 pandemic peaks.8, 10
Half the participants preferred to have their visit over the telephone. Telephone visits keep people at home, and are effective ways to meet medical care during the pandemics, and thus, prevent overwhelming of the healthcare system.12 Even though the Department of Veterans Affairs has been a leader in providing telehealth, the research enterprise trails the clinical use of these platforms. Veterans in general, have embraced telehealth and reported to be extremely satisfied with such care.13 The lower number of participants preferring phone visits could be a cohort effect as other studies have found that older patients may not embrace change to telehealth.14 On the other hand, the preference for telephone visits in this cohort may have been driven by fear of the contagion given the age of the sample.
In our study, family members were sought out as the most common source for information regarding the pandemic followed by news media. Those who got information from family members perceived being less safe to attend their appointments and that the medical center was less prepared for the pandemic than those that relied on TV for news. Similar results were found during the influenza pandemic of 2009–10, where a negative effect was seen on vaccine uptake among those that used family and friends as a main resource.15 In a RAND study, respondents rated CDC and news reports as the most influential source of information during the influenza pandemic. However, in the same study those who reported friends and family to be their most influential information source had higher vaccination rate than the news report category.16 In our study, females perceived higher panic in the general public. Other studies have found some association between females and perception of risk of influenza infection during the H1N1 pandemic.17
Strengths of the study include the inclusion of both the participants and the caregivers, and also collecting the perceptions from those who attended or not attended their research visits. A convenience sample was appropriate as the aim of this study was to generate hypothesis to provide transferable but not generalizable data, however all participants were part of ongoing geriatric studies.18 Limitations of the study include that data was collected at a single site, small sample size, and that a responder bias cannot be ruled out. Ethnicity distribution in this cohort was reflective of the patient population. The small sample size could explain, in portion, the lack of association of education and age on perception of threat by the virus, the choice of information source or preference of visits, hence the results need to be interpreted with caution.
CONCLUSIONS
Most informants felt that the medical center was prepared to handle the pandemic and that the extra screening made them feel safer. Most common sources of information regarding the pandemic were either the family members or the television news media irrespective of educational status. Perceptions about the pandemic were influenced by gender and the source of information. Knowing patientsʼ and caregiverʼs perspectives may help researchers be better prepared for future pandemics. Two such measures could be investing in ways to send timely and accurate messages to patients and their caregivers and offering more telehealth options during pandemics.
ACKNOWLEDGMENTS
Conflict of Interest
There are no financial conflicts of interest or personal conflict of interest relevant to the submitted manuscript for any authors.
Author Contributions
All authors have contributed significantly to the paper and approve the final version. Detailed author contributions are as follows: Prasad Padala: conceptualization, recruiting and conducting the study, interpreting data analysis and manuscript preparation; Kalpana Padala: conceptualization, interpreting data analysis and critical review of the manuscript; Heath Gauss: data analysis and critical review of the manuscript; Ashlyn Jendro: interpreting data analysis and critical review of the manuscript; Lillian Orr: review of the manuscript; Christopher Parkes: recruiting and conducting the study; Kim Dean: interpreting data analysis and critical review of the manuscript; Kerrie Wilson: interpreting data analysis and critical review of the manuscript.
Sponsorʼs Role
Dr. Prasad Padala is supported by grants from the Department of Veterans Affairs, and the National Institute of Health. Dr. Kalpana Padala is supported by grants from the Department of Veterans Affairs, and the National Institute of Health.
The sponsor has no role in the design, methods, subject recruitment, data collections, analysis or preparation of paper.
Prior presentations: None.
REFERENCES
- 1. Smith KF, Goldberg M, Rosenthal S, et al. Global rise in human infectious disease outbreaks. J R Soc Interface. 2014;11(101):20140950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gobat NH, Gal M, Butler CC, et al. Talking to the people that really matter about their participation in pandemic clinical research: a qualitative study in four European countries. Health Expect. 2018;21(1):387‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5). pii: E1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention. COVID19. 2020. https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed March 17, 2020.
- 5.National Institutes of Health. COVID19 guidance. 2020. https://grants.nih.gov/grants/natural_disasters/corona-virus.htm. Accessed March 17, 2020.
- 6. Padala PR, Jendro AM, Padala KP. Conducting clinical research during the COVID‐19 pandemic: investigator and participant perspectives. JMIR Public Health Surveill. 2020;6(2):e18887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elliott LK, Bami H, Gelkopf MJ, Yee RC, Feldman BM, Goh YI. Patient and caregiver engagement in research: factors that influence co‐enrollment in research. Pediatr Rheumatol Online J. 2019;17(1):85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gobat N, Butler CC, Mollison J, et al. What the public think about participation in medical research during an influenza pandemic: an international cross‐sectional survey. Public Health. 2019;177:80‐94. [DOI] [PubMed] [Google Scholar]
- 9. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rojek AM, Horby PW. Modernising epidemic science: enabling patient‐centred research during epidemics. BMC Med. 2016;14(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lurie N, Manolio T, Patterson AP, Collins F, Frieden T. Research as a part of public health emergency response. N Engl J Med. 2013;368(13):1251‐1255. [DOI] [PubMed] [Google Scholar]
- 12. North F, Varkey P, Bartel GA, Cox DL, Jensen PL, Stroebel RJ. Can an office practice telephonic response meet the needs of a pandemic? Telemed J E Health. 2010;16(10):1012‐1016. [DOI] [PubMed] [Google Scholar]
- 13. Young LB, Foster L, Silander A, Wakefield BJ. Home telehealth: patient satisfaction, program functions, and challenges for the care coordinator. J Gerontol Nurs. 2011;37(11):38‐46. [DOI] [PubMed] [Google Scholar]
- 14. Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Walter D, Bohmer M, Reiter S, Krause G, Wichmann O. Risk perception and information‐seeking behaviour during the 2009/10 influenza A(H1N1)pdm09 pandemic in Germany. Euro Surveill. 2012;17(13):20131. [PubMed] [Google Scholar]
- 16. Maurer J, Uscher‐Pines L, Harris KM. Perceived seriousness of seasonal and A(H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among U.S. adults: does the source of information matter? Prev Med. 2010;51(2):185‐187. [DOI] [PubMed] [Google Scholar]
- 17. Gidengil CA, Parker AM, Zikmund‐Fisher BJ. Trends in risk perceptions and vaccination intentions: a longitudinal study of the first year of the H1N1 pandemic. Am J Public Health. 2012;102(4):672‐679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]


