Abstract
Under the outbreak of COVID‐19, it was urgent to analyze the cases from clinical features and epidemiological factors, as well as understand the effectiveness of measures taken on disease prevent and control. A retrospective study was applied for descriptive analysis of clinical features and epidemiological factors of confirmed cases in four cities of Zhejiang. The Onset‐admission interval was calculated and plotted as well. The provincial measures regarding the response of COVID‐19 were summed up and sorted out. The distribution and sex and age were under normality distribution, and the age of 20 to 80 were all in risk of developing the disease. Clinical features of fever and cough were found mostly happen on patients. More than half of the patients had image changed on chest from reported data. The factor of closely contacted with confirmed cases was the most cause to the disease. The median onset‐admission interval was 6 days in Zhejiang province. As of the efficient health system, COVID‐19 had been successfully prevented and controlled in Zhejiang. Males and females were all vulnerable to COVID‐19. Preventing contact with confirmed cases could largely avoid the disease to happen. The government should take emergent and effective measures to prevent and treatment of the pandemic disease.
Keywords: clinical features, COVID‐19, epidemiological factor, provincial measures
1. INTRODUCTION
In December 2019, cases of pneumonia with unknown causes were reported in Wuhan, China. Epidemiological evidence suggested that most of these patients had visited the Huanan seafood market in Wuhan and Proved to be caused by SARS‐CoV‐2, which had not been found in humans before. 1 The infectious disease was officially named as COVID‐19 and this disease outbreak was declared as a Public Health Emergency of International Concern by World Health Organization (WHO) on 30 January 2020. 2 So far, more than 1 million cases of COVID‐19 have been confirmed globally. 3 In China, 83 597 confirmed cases have been reported and 78 145 patients have been cured to the date of 13 April 2020. 4
Analyzing of the genome of SARS‐CoV‐2 isolated from human airway epithelial cells, revealed that this new virus formed another clade within the subgenus sarbecovirus, Orthocoronavirinae subfamily. 5 Different from both SARS‐CoV and MERS‐CoV, SARS‐CoV‐2 is the seventh member of the family of coronaviruses that infect humans. 6 , 7 Some researchers have found that SARS‐CoV‐2 has a strong affinity to a human respiratory receptor and determined the phenomenon of human to human transmission in family homes and hospitals, which suggested a potential threat to the global public health. 8 Research found that the incubation period is 3 to 7 days in general, and days of 14 has been suggested as a quarantine period to ensure the absence of disease from healthy. 9 , 10 , 11
Zhejiang Province, ranked as the third place of COVID‐19 cumulative cases in China, has been suffering a lot for the disease. 12 Based on the official data, four cities had the most cases among a total of 11 cities in Zhejiang, which were Wenzhou, Hangzhou, Ningbo, and Taizhou, respectively. 3 , 12 Along with national actions against the disease, the Zhejiang government has also taken emergency measures to control the outbreak of disease, such as application of big data for monitoring the health status of citizens, 13 and development of nucleic acid detection kit for the early detection of COVID‐19 cases.
Since most of the studies were performed based on Wuhan or Hubei Province. Seldom information on novel coronavirus cases was known in other places of China. Therefore, it is necessary to explore the epidemiological and clinical characteristics of COVID‐19 patients in addition to related measures taken in non‐Hubei areas. 14 In this study, we performed a descriptive analysis of clinical characteristics and epidemiological factors of COVID‐19 patients and summed up the steps for disease control and treatment in Zhejiang province. These results may help us unravel the risk factors, characteristics as well as understand how could the epidemic be handled in Zhejiang, China.
2. METHODS
2.1. Data sources
A total of 889 confirmed cases were collected from the local health commission authority websites. The municipal government helped in procuring the accurate number of cases and reporting. The information of daily confirmed cases was collected from 27 January to 3 March in Hangzhou, Wenzhou, Ningbo, and Taizhou of Zhejiang province. The data included the date of onset, sex, age, clinical features, and exposure factors. Provincial measures had been summarized at the same time. All data for analysis were sorted up in excel as Supporting Information Appendix.
2.2. Statistical analysis
We carried out a retrospective study on the epidemiological factors and clinical characteristics. Government steps were sorted out for disease prevention and control. Descriptive analysis was applied for the clinical characters of patients as well as epidemiological factors among cities. Two‐way histogram was made with frequencies of age by gender shown above and below the x axis. Pie charts were drawn for comparing exposure factors of getting COVID‐19. Onset‐admission interval was calculated from the date of symptoms onset and diagnosis. Time chart was made for measures on the response of COVID‐19 in Zhejiang. Categorical variables were described as frequency rates or percentage, and continuous variables were analyzed as either means with standard deviations or median with interquartile range (IQR) values. Skewness and kurtosis test was applied for checking the normality. EXCEL 2016 and STATA 14.0 were employed for analysis.
3. RESULTS
Table 1 showed the basic information of COVID‐19 cases in Hangzhou, Wenzhou, Ningbo, and Taizhou. In a total of 889 cases, 438 were male and 451 were female, with a variant sex proportion among each city. Wenzhou suffered the most from COVID‐19, ranked by Hangzhou, Ningbo, and Taizhou, respectively. The mean age in four cities was 47.82, with a standard deviation of 15.19. Patients within age 14 to 49 accounted for a larger proportion and were ranked by an age group of 50 to 64. The younger suffered the less to COVID‐19 in four cities.
Table 1.
Descriptive analysis for COVID‐19 cases of four major cities in Zhejiang Province
| Basic city information | Hangzhou (n = 154) | Wenzhou (n = 472) | Ningbo (n = 144) | Taizhou (n = 119) | Total (n = 889) |
|---|---|---|---|---|---|
| Sex‐No., % | |||||
| Male | 73 (47.40) | 249 (52.75) | 48 (33.33) | 68 (57.14) | 438 (49.27) |
| Female | 81 (52.60) | 223 (47.25) | 96 (66.67) | 51 (42.86) | 451 (50.73) |
| Age groups‐No., % | |||||
| 0‐14 | 7 (4.55) | 5 (1.06) | 3 (2.08) | 3 (2.52) | 18 (2.02) |
| 15‐49 | 77 (50.00) | 247 (52.33) | 54 (37.50) | 63 (52.94) | 441 (49.61) |
| 50‐64 | 55 (35.71) | 164 (34.75) | 53 (36.81) | 36 (30.25) | 308 (34.65) |
| ≥65 | 15 (9.74) | 56 (11.86) | 34 (23.61) | 17 (14.29) | 122 (13.72) |
| Age, mean ± SD | 46.05 ± 16.32 | 47.63 ± 14.35 | 51.24 ± 16.47 | 46.74 ± 14.88 | 47.82 ± 15.19 |
| Clinical symptoms on admission ‐No., % | |||||
| Fever | 114 (74.03) | 338 (71.61) | 103 (71.53) | 77 (64.71) | 632 (71.09) |
| Cough | 81 (52.60) | 233 (49.36) | 7 (4.86) | 40 (33.61) | 361 (40.61) |
| Sore throat | 24 (15.58) | 48 (10.17) | 2 (1.39) | 12 (10.08) | 86 (9.67) |
| Sputum production | 21 (13.64) | 51 (10.81) | NA | 13 (10.92) | 85 (9.56) |
| Shortness of breath | 7 (4.55) | 3 (0.64) | NA | 0 (0.00) | 10 (1.12) |
| Headache | 31 (20.13) | 30 (6.36) | NA | 11 (9.24) | 72 (8.10) |
| Fatigue | 23 (14.94) | 61 (12.92) | NA | 16 (13.45) | 100 (11.25) |
| Myalgia | 13 (8.44) | 27 (5.72) | NA | 8 (6.72) | 48 (5.40) |
| Diarrhea | 9 (5.84) | 10 (2.12) | 1 (0.69) | 4 (3.36) | 24 (2.70) |
| Nausea | 3 (1.95) | 1 (0.0.21) | NA | 0 (0.00) | 4 (0.45) |
| Chill | 5 (3.25) | 32 (6.78) | NA | 10 (8.40) | 47 (5.29) |
| Asymptomatic infection | 4 (2.60) | 8 (1.69) | NA | 7 (5.88) | 19 (2.14) |
| Image change on chest | |||||
| Yes | 103 (66.88) | 18 (3.81) | 117 (81.25) | 7 (5.88) | 245 (27.56) |
| Unilateral infected | 68 (66.02) | NA | NA | 5 (71.43) | 73 (8.21) |
| Bilateral infected | 35 (33.98) | NA | NA | 2 (28.57) | 37 (4.16) |
| No | NA | NA | 16 (11.11) | NA | 16 (1.80) |
| Not report | 51 (33.12) | 454 (96.19) | 11 (7.64) | 112 (94.12) | 628 (70.64) |
| Exposure ‐No., % | |||||
| Traveled back from Wuhan city | 45 (29.22) | 150 (31.78) | 18 (12.50) | 45 (37.82) | 258 (29.02) |
| Traveled back from city outside of Wuhan | 21 (13.64) | 33 (6.99) | 19 (13.19) | 11 (9.24) | 84 (9.45) |
| Closely contacted with confirmed cases | 26 (16.88) | 190 (40.25) | 92 (63.89) | 52 (43.70) | 360 (40.49) |
| Unclear causes | 14 (9.09) | 46 (9.75) | 12 (8.33) | 7 (5.88) | 79 (8.89) |
| Interval from disease onset to diagnosis (Onset‐admission interval) | |||||
| 1‐3 | 29 (20.14) | 68 (14.62) | 46 (31.94) | 21 (18.75) | 164 (18.96) |
| 4‐6 | 60 (41.67) | 157 (33.76) | 37 (25.69) | 40 (35.71) | 294 (33.99) |
| 7‐9 | 23 (15.97) | 110 (23.66) | 33 (22.92) | 30 (26.79) | 196 (22.66) |
| >9 | 32 (22.22) | 130 (27.96) | 28 (19.44) | 21 (18.75) | 211 (24.39) |
| Days, median (IQR) | 6 (4‐9) | 7 (4‐10) | 5 (3‐9) | 6 (4‐9) | 6 (4‐9) |
Although the proportion of clinical symptoms differed from each city, symptoms such as fever, cough, and fatigue were commonly found among patients, and symptoms of sore throat, sputum production, headache, and chill were also co‐existing on patients. In addition, we noticed that asymptomatic infection cases made up a small proportion among cities, whom performed healthy even during the illness. Although the information of image change was partially lacking, still we could find among 60% to 80% patients had radiological changes in lungs, and 60% to 70% patients were unilateral infected compared with around 30% patients were bilateral infected. Under the exposure column, closely contacted with confirmed cases was the main cause of COVID‐19, followed by a exposure history in Wuhan city. Beyond those, factors like exposure history outside of Wuhan, shopping in the supermarket, taking transportation, and so on. were also considered risk factors to the disease. Median and interquartile range were calculated for onset‐admission interval, and most patients were in 5 to 7 interval days among the four cities.
Figure 1 illustrated a distribution of COVID‐19 cases by sex and age in Zhejiang. It was found that the frequency of age was different between male and female groups. The most frequent age among male patients was under 50, while age 35 and 52 had the largest numbers of patients in female group. The distribution was examined as normality through skewness and kurtosis test, with the most cases focused on the age from 20 to 80, and less cases were located between the age of 0 to10 as well as 90 to 100.
Figure 1.

Distribution of gender and age from summing up COVID‐19 cases in four cities
Figure 2 further interpreted the components of exposure factors in four cities. We found the factor of intimate contact with confirmed cases took up for 39%, 39%, 64%, and 44% in Hangzhou, Wenzhou, Ningbo, and Taizhou, respectively, which was the leading cause of COVID‐19. A factor of exposure history in Wuhan was found also highly associated with the disease in each city. In Hangzhou, flight taken occupied 5% of its cases, showing that public transportation would contribute to the dissemination and transmission of the virus. In Wenzhou, we found a factor of shopping in Yintai market took up for 4% of its cases, pointing out accessed to a public occasion could be a risk factor of the disease transmission. In addition, a factor of got in touch with returnees from Wuhan was also identified as an epidemiological factor especially when patients were asymptomatic, without obvious clinical symptoms.
Figure 2.

Epidemiological analysis for COVID‐19 exposure in four major cities
Figure 3 summed up the date of onset and confirmed diagnosis for all cases. The x‐axis was the date and y‐axis represented the number of daily onset and confirmed cases. The figure showed that the earliest case occurred on 6th January, and the number of patients with symptoms culminated on 23rd January. However, there was a delay between the symptoms onset and diagnosis, for example, the diagnosis of first case was almost 20 days late behind symptoms onset. On 29th January, the number of daily confirmed cases reached a peak, which was close to 120. However, along with a following decreased trend, the number of daily confirmed cases raised again to 100 on 3rd February, and then descended as time went on. Starting from 23rd January, the provincial government launched a first level emergency response to this Public Health event.
Figure 3.

Date of onset and diagnosis from summed data in Zhejiang
Apart from the national measures, the local government has also taken some effective steps on the response of the outbreak of COVID‐19 (Figure 4). The provincial government quickly initiated a first‐level response to the major public health emergency on 23rd January. And other key measures have been taken subsequently, for instance, public gathering was prohibited and public transportation had been suspended. In addition, each city carried out relevant steps targeting on efficient controlling disease. As Wenzhou had more people exposed to epidemiological factors, the local government conducted a large‐scale screening for timely detection of potential cases. Likewise, Hangzhou distributed free medical masks to the public. More detailed information could be found in Figure 4.
Figure 4.
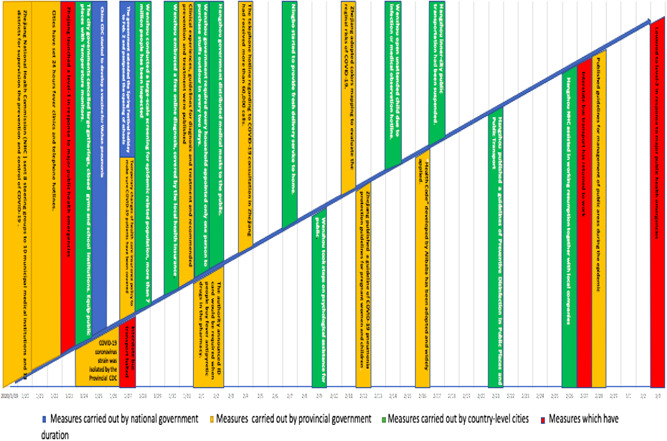
Measures have taken on prevention and control of COVID‐19
4. DISCUSSION
In December of 2019, Wuhan started the outbreak of COVID‐19. 15 Since then, the first case in Zhejiang was reported on 21st January. 12 Zhejiang, where is a province with large floating population, due to its specificity, the province soon ranked as the third place of cumulative confirmed cases in China. 3 , 12 In this study, we did a retrospective study analysis for the confirmed cases diagnosed from 27th January to 1st March. Detailed information like sex, exposure factors, clinical symptoms, date of onset and diagnosis as well as measures on response of the disease were sorted up, which contributed on understanding the characteristics and development of COVID‐19 cases outside of Wuhan.
Table 1 presented a descriptive analysis of novel coronavirus pneumonia cases from four major cities in Zhejiang. Our study found males and females were all vulnerable to the disease, indicating gender may not be a risk factor of developing the disease. The infected patients could be found at all ages, and most patients were found at the age of 20 to 80. Research showed the infection of COVID‐19 is self‐limited, people whom could recover in a strong immune system. 16 And the younger would be in a lower likelihood of infection because of a faster immune response mechanism. 17 Elder population were in a higher risk to be infected owning to lack of knowledge of disease prevention or having chronic conditions. 18 , 19 Cough and fatigue were mostly found among patients, which were consistent with the findings of Shi et al and Wu et al 20 , 21 It is also important to carry out differential diagnosis from patients with common cold, especially when they had epidemiological exposure history. 22 We noticed that asymptomatic infection took up a small proportion among patients, although it varied from each city. The discrimination of asymptomatic patients was mostly from imaging screening in light of epidemiological exposure history. 23 , 24 As the asymptomatic did not present any clinical signs or symptoms but still excrete coronavirus and could become a source of infection, 25 , 26 it is necessary to detect the inapparent infection from population and prevent the disease from further spread.
Due to the unreported information on image change, the proportion for radiology “Changed” and “Unchanged” varied a lot between each city. Since chest CT could identify the early phrase of the disease infection, it has been recommended as one of major evidence for COVID‐19 diagnosis and public health surveillance. 27 Yang et al 28 has proved chest CT could be used to quickly assess patients with severity of the novel coronavirus. Research found the disease is mainly transmitted through respiratory tract and interpersonal contact. 10 , 22 Since closely contact with confirmed cases was the leading cause to COVID‐19 in Zhejiang Province, it is of great importance to quarantine the population with epidemiological exposure to prevent disease transmission. 29 , 30 In the meanwhile, public space as well as transportation could be closed or suspended for the spread of infectious disease. In this study, pregnant cases have not been found, however, we still need to pay attention to this special group, relevant guidelines should be made for the management of this group. 31
The day of onset‐admission interval was shorter than the initially reported cases in Wuhan, 9 while was a bit longer than days in Shanghai. 32 This indictor was supposed to reflect the effectiveness and capacity of public health emergency system, and it is regarded as a better health system with a shorter interval for admission. 33 As of the quick response to the COVID‐19 treatment, the local government has provided the effective detecting device such as the kit for reverse transcription polymerase chain reaction as well as taken strictly measures to control the disease, which shortened the diagnostic time significantly. 12 We found in Figure 3, the epidemic curve of symptoms onset peaked around 26th January and declined along with time. It is because the outbreak of COVID‐19 was around the spring festival period, as a growing number of people returned from Wuhan for celebrating the Chinese new year, cases occurred much more between 19th January to 3rd February.
Since the outbreak of COVID‐19, the local government has taken emergency measures to efficient control and treatment of disease. The only one death case and high recovery rate suggested the local health system was efficient and effective. The government was the earliest to set the first level response to this public health emergency in China after interpersonal transmission identified. 4 , 12 Moreover, other epidemic prevention measures have been implemented, for example, provincial government officially announced the daily confirmed and suspected cases, stopped all interprovincial roads transportation as well as promptly launched on a epidemic collection system, ensuring population health information were under surveillance. 34 , 35 Also, hospitals adopted a centralized treatment for COVID‐19 patients and integrated the research into clinics. 36 At the same time, local business also played a significant role in this event. For instance, the Alibaba company has developed a program of Health Code, collecting the data of personal information, traveling history, epidemic contact history and clinical symptoms. 37 The risk of disease was presented by different colors in Health Code. The green color meant a healthy status, in which persons were allowed to freely walk around in the city, the yellow represented a medium risk, indicating people should have been quarantined at home or clinics for 7 days, and the red suggested a higher risk of having COVID‐19, for people should be centralized quarantined for 14 days. By using the digital technology, the Health Code supported the government on the control of further spread of the disease.
4.1. Strength and weakness
It was the first time to describe the public available cases of COVID‐19 and local government measures in Zhejiang, China. The distribution of cases by sex, age, clinical features, exposure factors, and onset‐admission interval were analyzed and relevant measures in facing COVID‐19 were sorted for providing guidance of successful prevention and control. However, as other cities had much less cases and were lack of detailed information on patients, only Hangzhou, Wenzhou, Ningbo and Taizhou were selected to be analyzed, though the information of clinical features and image change in above cities were partly lost. Since the data was collected from public websites, the accuracy could not be completely ensured, either the results of analysis could not fully represent the whole patients in Zhejiang province yet.
5. CONCLUSION
Males and females were all vulnerable to COVID‐19, and the disease occurred at all age groups. Preventing contact with confirmed cases could largely avoid the disease happen. On account of the effective health system, the COVID‐19 has been successfully controlled under the joints of government and local businesses.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
GW and WC collected the data and together developed the draft. GW and XJ carried out data analysis and made the figures. XJ translated all collected data into English. Y‐PC helped to understand the clinical knowledge and revise the draft. All authors read and approved the final draft.
Supporting information
Supplementary information
ACKNOWLEDGMENTS
The authors thank all the people who made contribution on the disease control and treatment. The authors are very proud of these heroes.
Wang G, Chen W, Jin X, Chen Y‐P. Description of COVID‐19 cases along with the measures taken on prevention and control in Zhejiang, China. J Med Virol. 2020;92:1948–1955. 10.1002/jmv.25906
Guan Wang and Wenhu Chen are co‐first authors of the article.
REFERENCES
- 1. World Health Organization . Clinical management of severe acute respiratory infection when Novel coronavirus (2019‐nCoV) infection is suspected: interim guidance. https://www.who.int/publications‐detail/clinical‐management‐of‐severe‐acute‐respiratory‐infection‐when‐novel‐coronavirus‐(ncov)‐infection‐is‐suspected. Accessed January on 11, 2020.
- 2. World Health Organization . Naming the coronavirus disease (COVID‐19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/technical‐guidance/naming‐the‐coronavirus‐disease‐(covid‐2019)‐and‐the‐virus‐that‐causes‐it
- 3. DXY , COVID‐19, Global Pandemic Real‐time Report. 2020. https://ncov.dxy.cn/ncovh5/view/en_pneumonia?from=dxy&source=&link=&share=. Accessed April 6, 2020.
- 4. National Health Commission of the People's Republic of China . 2020. http://www.nhc.gov.cn. Accessed April 6, 2020. [DOI] [PMC free article] [PubMed]
- 5. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet. 2020;395(10224):565‐574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chan JFW, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person‐to‐person transmission: a study of a family cluster. The Lancet. 2020;395(10223):514‐523. 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523‐534. 10.1038/nrmicro.2016.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. He X, Zhang L, Ran Q, et al. Integrative bioinformatics analysis provides insight into the molecular mechanisms of 2019‐nCoV. MedRxiv. 2020. 10.1101/2020.02.03.20020206 [DOI] [Google Scholar]
- 9. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199‐1207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020;382:1708–1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS‐Cov‐2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Health Commission of Zhejiang Province . [Published online on April 6, 2020]. http://www.zjwjw.gov.cn/col/col1202101/index.html
- 13. Zhejiang launched a Health code to prevent and control the &hyphen‐qj4;epidemic. 2020. http://www.blueskyinfo.com.cn/wjwApp/webinfo/infoDetail.do?infoIds=E3BE035E1EEA087FC952B932BF6EAAAF9B8DA800D742DC5B8B596B3046E5FBCB49DF8A7DD3C89C7B. Accessed April 6, 2020.
- 14. Linton NM, Kobayashi T, Yang Y, et al. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020;9(2):538. 10.3390/jcm9020538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang G, Jin X. The progress of 2019 novel coronavirus event in China. J Med Virol. 2020;92:468‐472. 10.1002/jmv.25705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The World Health Organization . Health topic, coronavirus disease (COVID‐19) outbreak. Statement. 2020. http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/statements/statement‐older‐people‐are‐at‐highest‐risk‐from‐covid‐19,‐but‐all‐must‐act‐to‐prevent‐community‐spread. Accessed April 6, 2020.
- 17. Beusekom MV Children's COVID‐19 risks unique, Chinese studies find. 2020. http://www.cidrap.umn.edu/news‐perspective/2020/03/childrens‐covid‐19‐risks‐unique‐chinese‐studies‐find. Accessed April 6, 2020.
- 18. Centers for Disease Control and Prevention . Coronavirus Disease 2019 (COVID‐19) https://www.cdc.gov/coronavirus/2019‐ncov/specific‐groups/high‐risk‐complications.html. Accessed April 6, 2020.
- 19. Mary AEZ. Predisposition to Infection in the elderly. US Pharm. 2011;36(8):28‐31. https://www.uspharmacist.com/article/predisposition‐to‐infection‐in‐the‐elderly [Google Scholar]
- 20. Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID‐19 penumonia in Wuhan, China: a descriptive study. The lancet infectious disease. 2020;20:425‐434. 10.1016/S1473-3099(20)30086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China. JAMA. 2020;323(13):1239–1242. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 22. National Administration of Traditional Chinese Medicine . Diagnosis and treatment of novel coronavirus infected pneumonia (The seventh edition). http://www.satcm.gov.cn. Accessed April 6, 2020.
- 23. Health Commission of Wenzhou . COVID‐19 data. http://wjw.wenzhou.gov.cn. Accessed April 6, 2020.
- 24. Health Commission of Wenzhou . COVID‐19 data. http://wsjkw.zjtz.gov.cn/index.php. Accessed April 6, 2020.
- 25. Hu ZL, Song C, Xu CJ, et al. Clinical characteristics of 24 asymptomatic infections with COVID‐19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63(5):706–711. 10.1101/2020.02.20.20025619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID‐19. JAMA. 2020;323:1406. 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zu ZY, Jiang MD, Xu PP, et al. Coronavirus disease 2019 (COVID‐19): a perspective from China. Radiology. 2020:200490. 10.1148/radiol.2020200490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang R, Li X, Liu H, et al. Chest CT severity score: an imaging tool for assessing severe COVID‐19. Radiology. 2020;2. 10.1148/ryct.2020200047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han Y, Yang H. The transmission and diagnosis of 2019 novel coronavirus infection disease (COVID‐19): a Chinese perspective. J Med Virol. 2020. 10.1002/jmv.25749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liu Y, Gayle AA, Smith AM, et al. The reproductive number of COVID‐19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2):1–4. 10.1093/jtm/taaa021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sahu KK, Mishra AK, Lal A. A Twin challenge to handle: COVID‐19 with pregnancy. J Med Virol. 2020. 10.1002/jmv.25784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lu H, Ai J, Zhang W, et al. A descriptive study of the impact of disease control and prevention on the epidemics dynamics and clinical features of SARS‐CoV‐2 outbreak in Shanghai, lessons learned for metropolis epidemics prevention. Medrxiv. 2020. 10.1101/2020.02.19.20025031 [DOI] [Google Scholar]
- 33. Norrving B Oxford Textbook of Stroke and Cerebrovascular Disease. 2014. https://oxfordmedicine.com/view/10.1093/med/9780199641208.001.0001/med‐9780199641208. Accessed April 6, 2020.
- 34. The Tencent . How can Zhejiang achieve for 0 death in COVID‐19? 2020. https://xw.qq.com/cmsid/20200220A0N11L00?f=newdc. Accessed April 6, 2020.
- 35. The People's Governzament of Zhejiang Province. http://www.zj.gov.cn/. Accessed April 6, 2020.
- 36. The Sohu news . What experiences could learn from Zhejiang? 2020. https://www.sohu.com/a/373593778_115433. Accessed April 6, 2020.
- 37. The Sina News . What is Health Code? 2020. https://tech.sina.com.cn/roll/2020‐02‐23/doc‐iimxyqvz5108537.shtml. Accessed April 6, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information


