Coronavirus disease 2019 (COVID‐19) is an infectious disease caused by a newly emerging coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). COVID‐19 has a very variable clinical picture, ranging from asymptomatic to SARS that can lead to death.
Our case, a 74‐year‐old female patient, presented with fever, moderate dyspnoea and leucocytosis (white blood cell count 21.6 × 109/l, neutrophils 16.8 × 109/l, lymphocytes 3.67 × 109/l). Reverse transcriptase‐polymerase chain reaction for SARS‐CoV‐2 was performed, which confirmed COVID‐19.
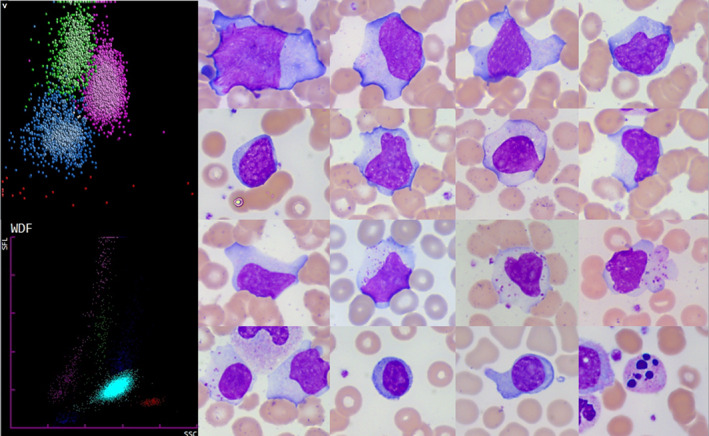
Peripheral blood film examination revealed a highly pleomorphic atypical lymphocyte population (right). Many cells were large (15–30 µm). The cytoplasm was sometimes granulated. Cytoplasmic basophilia was sometimes generalised and sometimes confined to the cytoplasmic margins. Some cells had one or more nucleoli and could have been mistaken for blast cells. Plasma cells and apoptotic cells were also present.
In 5–10% of full blood counts of our hospitalised patients suffering from COVID‐19 (all care sectors including intensive care), flags on our haematology analysers are present: ‘MO Blast’ for DXH800 (Beckman Coulter, top left) and ‘Blasts Abn/lympho?’ for XN10 (Sysmex, bottom left), requiring a blood film examination.
Cytology in COVID‐19 usually shows numerous neutrophils with either normal or decreased lymphocytes. This case illustrates the atypical lymphocytes that are often present. These cells morphologically mimic those of Epstein–Barr virus or cytomegalovirus infection, whereas plasma cells and plasmacytoid lymphocytes (present in some of our patients) are not usually a feature of these two infections.


