Summary
Healthcare workers are at risk of infection during the severe acute respiratory syndrome coronavirus‐2 pandemic. International guidance suggests direct droplet transmission is likely and airborne transmission occurs only with aerosol‐generating procedures. Recommendations determining infection control measures to ensure healthcare worker safety follow these presumptions. Three mechanisms have been described for the production of smaller sized respiratory particles (‘aerosols’) that, if inhaled, can deposit in the distal airways. These include: laryngeal activity such as talking and coughing; high velocity gas flow; and cyclical opening and closure of terminal airways. Sneezing and coughing are effective aerosol generators, but all forms of expiration produce particles across a range of sizes. The 5‐μm diameter threshold used to differentiate droplet from airborne is an over‐simplification of multiple complex, poorly understood biological and physical variables. The evidence defining aerosol‐generating procedures comes largely from low‐quality case and cohort studies where the exact mode of transmission is unknown as aerosol production was never quantified. We propose that transmission is associated with time in proximity to severe acute respiratory syndrome coronavirus‐1 patients with respiratory symptoms, rather than the procedures per se. There is no proven relation between any aerosol‐generating procedure with airborne viral content with the exception of bronchoscopy and suctioning. The mechanism for severe acute respiratory syndrome coronavirus‐2 transmission is unknown but the evidence suggestive of airborne spread is growing. We speculate that infected patients who cough, have high work of breathing, increased closing capacity and altered respiratory tract lining fluid will be significant producers of pathogenic aerosols. We suggest several aerosol‐generating procedures may in fact result in less pathogen aerosolisation than a dyspnoeic and coughing patient. Healthcare workers should appraise the current evidence regarding transmission and apply this to the local infection prevalence. Measures to mitigate airborne transmission should be employed at times of risk. However, the mechanisms and risk factors for transmission are largely unconfirmed. Whilst awaiting robust evidence, a precautionary approach should be considered to assure healthcare worker safety.
Keywords: aerosol, airborne, COVID‐19, SARS‐CoV‐2, transmission
Introduction
Severe acute respiratory syndrome (SARS) coronavirus‐2 (SARS‐CoV‐2) continues to cause an international health crisis through coronavirus disease 2019 (COVID‐19). The safety of healthcare workers is a global priority to prevent collapse of healthcare systems and transmission from hospital to the community. Due to frequent close contact with infected patients, healthcare workers are at high risk. Healthcare workers made up over 20% of all cases during the previous SARS‐CoV‐1 epidemic 1, 2, 3, 4, 5, 6. At the start of April 2020, over one million people had been confirmed infected with SARS‐CoV‐2. A healthcare worker infection rate as high as in the SARS‐CoV‐1 epidemic would involve enormous numbers of healthcare workers.
Current personal protective equipment (PPE) and infection control guidelines from the World Health Organization (WHO) are based on the assumption that the primary mechanism of transmission is direct and indirect droplet spread 7. Direct droplet spread is said to occur when respiratory particles greater than 5 μm in diameter make contact with the mucosal surface of a recipient. Indirect spread occurs when a fomite or an intermediate surface is touched, usually by a hand, which then contacts mucosal surfaces. The faeco‐oral route is also possible, with viral content noted in stools 8.
Airborne spread is thought to occur when respiratory particles less than 5 μm in diameter are inhaled and deposited in the lungs. These particles have been described interchangeably as aerosols, droplet nuclei, airborne and small particles. The WHO advises that airborne transmission can occur, but only when aerosol generating procedures (AGP) are performed 7. The WHO‐defined AGPs partly include: positive pressure ventilation; tracheal intubation; airway suctioning; nebuliser treatment; and bronchoscopy 7, 9. Consequently, the advice of the WHO is for droplet precautions to be observed for all suspected patients, with the addition of airborne precautions around AGPs 7.
Mechanisms of airborne viral particle formation
There are three mechanisms that describe the formation of respiratory airborne particles. All necessitate surface tension disruption of the respiratory tract lining fluid 10, 11.
Open‐close cycling of glottic structures (> 1 μm diameter)
Shearing forces due to high velocity gas flow (2–5 μm diameter)
Open‐close cycling of terminal bronchiole airways (< 1 μm diameter)
Based on composition analysis, exhaled particles have been demonstrated to come from lower rather than upper respiratory tract origins 12. Viral growth in‐medium has been demonstrated from particles < 5 μm produced from infected humans 13, 14, 15, 16, 17. Infected human subjects produce a greater number of particles when coughing compared with healthy controls; furthermore, particles from infected patients contain viable virions 13, 14, 16, 18, 19. If inhaled, particles in the range < 5–20 μm have the ability to reach the respiratory portion of the airways 19, 20, 21, 22, 23.
Gas flow velocities vary with type of exhalation. Tidal volume breathing may generate airflow velocities up to 1 m.s−1; talking 5 m.s−1; coughing 2–50 m.s−1; and sneezing > 100 m.s−1 10, 24. The explosive shear forces generated from coughing and sneezing lead to expulsion of large numbers of varyingly sized particles and the highest number of particles, but significant numbers and a range of sizes are produced during talking and even tidal volume breathing 10, 21, 25, 26, 27, 28. Exhaling to closing capacity has been strongly correlated with significant aerosol production 11, 29.
Particle exhalation and deposition
Exhalation creates a jet with a cone‐shaped geometry. Sneezes and coughs can form a turbulent multiphase gas cloud protecting the droplets from evaporation. This may extend the lifespan of a droplet allowing it to travel further 30. This cloud can travel up to 8 m, carrying a polydispersed range of droplets. Eventually the cloud loses momentum and the remaining droplets evaporate forming droplet nuclei that remain suspended for hours with the ability to cause longer‐range infectious transmission 30, 31.
Mechanisms of particle deposition within the atmosphere and airways partly depend on particle diameter. Diameter is a constantly changing variable due to the effect of humidity. As a particle leaves the respiratory tract, the relative humidity decreases and a rapid decrease in particle diameter of 25–50% occurs. This process is reversed on inhalation of a particle 20, 32.
The distance particles may travel is dependent on numerous variables, making it impossible to precisely define a safe distance to avoid transmission 26, 30. The number of particles reduces with an increasing distance from the source. Larger particles generally take a ballistic trajectory, travelling shorter distances, and smaller particles remain suspended indefinitely. Larger particles are subject to inertial impaction and gravitational settlement, governed by Stokes’ Law, and smaller particles to diffusion described by Fick's law 10. Depending on the droplet's density, aerodynamic diameter and momentum, droplets may move faster, slower or at the same speed as the airstream with which they are exhaled 10, 26. When encountering a barrier, the stream will typically be deflected or bifurcate 24.
The site of particle deposition in the airway may depend on: (1) particle aerodynamic diameter, shape, velocity, charge, composition, density, temperature and humidity; and (2) subject‐specific variables, disease and airway geometry 10, 20, 32. Increased temperature and humidity have both been shown to increase the rate of respiratory viral decay. This is likely a factor in seasonal and regional differences in respiratory infections 33. Even heat from the patient and healthcare worker will alter airflows due to thermal air‐currents or plumes 34. Determinants of airborne viral concentration are displayed in Fig. 1.
Figure 1.
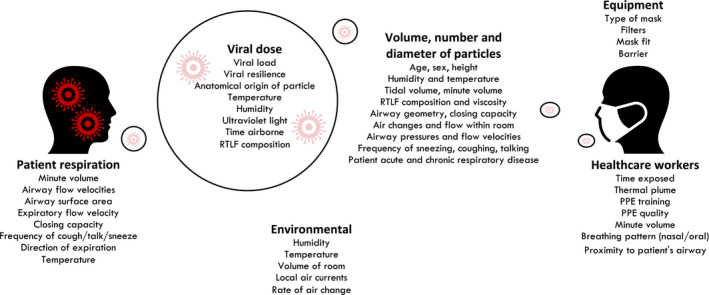
Key determinants of healthcare worker aerosol transmission in spontaneously breathing patient. RTLF, respiratory tract lining fluid; HCW, healthcare worker; PPE, personal protective equipment.
During inhalation negative pressure creates airflow in a spherical breathing zone around the mouth and nose. A 500‐ml breath will generally draw gas from a radius approximately 10 cm from the healthcare worker's mouth. The nasopharynx filters some particles including aerosols, but mouth breathing involves less filtration. Approximate hourly healthy adult alveolar ventilation is over 200 l of air, which will be in contact with an alveolar surface area of 750 m2 23. This is a large volume of gas which may carry a viral inoculum.
The airborne particle size continuum
The WHO 5‐μm size threshold used to differentiate droplet from airborne transmission is an over‐simplification of the multifactorial mechanisms governing aerosol dispersal and deposition 7. It is not clear if 5 μm refers to the diameter obtained experimentally (which varies with measurement method and environmental conditions), or at which stage in the dynamic airborne journey. There is heterogeneity between individual subjects and between experimental methodologies with regard to particle size and number measured during expiration. Due to irregular particle geometric shape, ‘aerodynamic diameter’ is the preferred term which assigns a diameter as if the particle were a perfect sphere. The median aerodynamic diameter and the geometric standard deviation are more predictive of particle deposition than ‘simple’ diameter 20.
It is demonstrable that larger particles tend not to reach the respiratory airways but the exact particle size that determines this cannot be defined 20, 22, 25, 30, 32, 35. There may be outliers from the median distribution that will deposit more deeply in the airway than the average. These particles may carry a disproportionately large viral inoculum due to their volume. Measuring the aerodynamic diameter of particles and determining exactly where in the lung they deposit is challenging. Rather than defining an exact 5‐μm diameter cut‐off to define droplet or aerosol spread, lung particle deposition should be considered a continuum under which variables define the risk of lung deposition.
SARS‐CoV‐2 airborne transmission
In human influenza models, aerosol inoculation is associated with increased disease severity and lower (rather than upper) respiratory tract infection, and may transmit infection even in a one‐hundred‐fold lower inoculum size 14, 18, 22, 25, 36, 37, 38, 39. Air sampling studies in commercial aircraft and health centres during influenza season demonstrated significant numbers of viral genome copies within airborne particles. The airborne viral content was calculated to be in excess of the minimal infectious dose 40. Medical students contracted SARS‐CoV‐1 despite being considerably over a meter away from the hospitalised index patient. Post‐hoc modelling postulated airflows that could have carried aerosols causing viral transmission 41. An epidemiological study of SARS‐CoV‐1 using airflow modelling suggested that residents of a tower block were infected by airborne spread via a rising plume of contaminated air in a ventilator shaft 31. During the same epidemic viral ribonucleic acid (RNA) was sampled from air within a patient's room 42.
Caution is required when directly inferring specifics of transmission from one respiratory virus to another as each has its own infective inoculum and aerosol characteristics. The SARS‐CoV‐2 virus uses the S‐spike protein to bind to the angiotensin‐converting enzyme‐2 (ACE‐2) receptor. Angiotensin‐converting enzyme‐2 has significantly greater expression on the surface of alveolar type‐2 epithelial cells compared with bronchial epithelial cells 43. The alveolar epithelium has less protection due to a thinner respiratory tract lining fluid, providing more direct access to the ACE‐2 receptor possibly facilitating infection 43, 44. Severe acute respiratory syndrome coronavirus‐2 remains stable in artificially generated aerosols (< 5 μm) for up to 3 hours whilst maintaining an infectious titre 45.
Viral SARS‐CoV‐2 RNA have also been isolated on a ceiling extractor fan in a patient's negative pressure room where no AGPs had been reported 46. Pre‐submission articles, yet to be peer‐reviewed, are suggestive of airborne RNA from normal breathing, the significance of which is undetermined (Liu et al., Chia et al. unpublished observations). Viral RNA in aerosol‐sized particles in public, staff and clinical areas have been reported (Liu et al. unpublished observations). Levels were notably elevated in the protective apparel removal (doffing) room and patient toilets. Levels were lower in the intensive care unit, perhaps due to increased ventilation, and the peak size of particles was in the sub‐micron range (0.25–1 μm) (Liu et al. unpublished observations).
It may prove difficult to unequivocally establish whether SARS‐CoV‐2 is infectious when airborne due to technical difficulties associated with air sampling of viable viral particles, and human‐to‐human transmission study being unethical. Current arguments against this and supportive of airborne transmission are displayed in Fig. 2.
Figure 2.

Evidence for and against airborne transmission of Severe acute respiratory syndrome coronavirus‐2. ARDS, acute respiratory distress syndrome; ACE, angiotensin‐converting enzyme; AGP, aerosol‐generating procedure.
Aerosol‐generating procedures
A number of studies have shown an association between AGPs and healthcare worker infection during the SARS‐CoV‐1 epidemic. These are retrospective cohort studies and case series with multiple confounding factors, including: recall bias from retrospective questionnaires; variation in PPE; hand washing and training; incomplete follow‐up; and small study sizes 1, 2, 4, 5, 6. Crucially, aerosol levels were never measured in any of the studies. The authors of a systematic review of AGPs identified 10 studies suitable for inclusion, all of which were deemed ‘very low‐quality evidence’ as per grading of recommendations, assessment, development and evaluations (GRADE) criteria 9. Grading of recommendations, assessment, development and evaluations suggest caution when interpreting these results as ‘any estimate of effect is very uncertain’.
An association is observed between healthcare worker infections and proximity to critically unwell patients who required emergency care 1, 2, 4, 5, 6. Tracheal intubation was associated with a relative risk (95%CI) of healthcare worker infection of 4.2 (1.5–11.4), manipulation of an oxygen mask carried a relative risk of 9 (11.2–64) and urinary catheter insertion with a relative risk of 5 (2.4–10.2) 4, 9. This may imply that physical proximity and time in the presence of a critical patient is high risk rather than the procedure per se.
Few studies have measured expired pathogen load in relation to AGPs 35, 47. Particles containing viral RNA were found in the air around patients with influenza H1N1 in the intensive care unit, even during tidal volume breathing. The WHO‐defined AGPs were not associated with a significant rise in airborne viral content, with the exception of bronchoscopy and in‐line airway suctioning 9, 48. Airborne viral content decreased with increasing duration of illness and with increasing relative humidity 47.
Shear stress and respiratory physiology
Surface tension occurs when two immiscible fluids share an interface. Across this surface of separation there is a discontinuity in density and the surface behaves like a stretched membrane under tension. Aerosol particle formation is dependent on shear forces across the airway walls overcoming respiratory tract lining fluid surface tension. The ratio of inertial to viscous forces described by the Reynolds number determines the likelihood of transition from laminar turbulent flow. Fluid velocity is increased by pressure difference and radius, and decreased by viscosity. As the velocity of gas flow rises, laminar shear forces will increase before a transition to turbulent flow with significant further increase in shear forces. Therefore, a higher differential between atmospheric and alveolar pressure causes a rise in respiratory tract lining fluid shear stress and increases aerosol particle formation 49.
Acute respiratory distress syndrome (ARDS) leads to alveolar inflammatory damage, compromise of lung mechanics and reduced respiratory function. Respiratory tract lining fluid composition is altered due to leucocyte infiltration and pulmonary oedema. Increased atelectasis, closing capacity and decreased compliance lead to a rise in pressure gradients to enable alveolar ventilation. During exercise, airway pressures may persistently swing from −30 cmH2O to + 30cmH2O, with peaks in excess of 100 cmH2O recorded 50. It is likely that similarly high‐pressure changes occur in spontaneously ventilating ARDS patients contributing to patient self‐inflicted lung injury 50, 51. Furthermore, distal airway collapse will lead to increased open‐close terminal airway cycling, which also causes greater aerosol formation 11, 29.
Medical therapies and airborne transmission
Based on our interpretation of the current aerobiological and limited clinical evidence, we risk stratify key WHO AGPs with the addition of the ‘natural’ aerosol generators of coughing and dyspnoeic breathing in Table 1.
Table 1.
Procedures graded by risk of aerosol generation
| Aerosol generator | Applied physiology | Clinical evidence | Estimated risk of aerosol generation |
|---|---|---|---|
| Bronchoscopy | High airway pressures and distal airway collapse | Increased viral aerosols in H1N1 35, 47 | Extreme |
| Percutaneous tracheostomy with bronchoscopy | High airway pressures and distal airway collapse with tracheostomy patent for unfiltered aerosols | Limited | Extreme |
| Bag‐valve mask ventilation | Aerosol generation with high pressures and airway collapse | Associated with HCW transmission of SARS‐CoV‐1 2, 4 | Technique‐dependent |
| CPR | Airway collapse, shear forces from CPR, high airway pressures for ventilation | Strongly associated 6 | Extreme |
| Suctioning |
Shear forces from significant negative pressure and flows. Causes coughing |
Increased viral aerosols in H1N1 47 | High |
| Frequent cough | Natural aerosol generator | Associated with HCW transmission of SARS‐CoV‐1 1, 2, 4 | High |
| Dyspnoeic spontaneous respiration | Likely natural aerosol generator | Association with HCW transmission of SARS‐CoV‐1 1, 2, 4 | High |
| Extubation | High risk due to coughing and distal airway collapse | Not studied | High |
| Laryngoscopy | Unlikely to cause aerosols per se | None showing rise in viral aerosols. Associated with HCW transmission of SARS‐CoV‐1 2, 4 | Dependent on peri‐intubation period |
| Oxygen facemask | De‐humidified cold gas could promote viral viability. | Adjustment of mask strongly associated with risk of transmission of SARS‐CoV‐1 2, 3, 4 Increased dispersal 24. | High – moderate |
| High‐flow nasal cannula |
Possibly reduce viral aerosols through decreased airway collapse and airway pressures. Unsealed circuit |
Associated in limited quality studies. Used as part of Chinese COVID‐19 protocol. Increased dispersal 53, 55, 56 | High – moderate |
| Non‐invasive ventilation |
Possibly reduce viral aerosols through decreased airway collapse and pressures. Sealed mask and circuit beneficial. High positive pressure may lead to leak |
Association in limited quality studies. Used safely in small study 3. Increased dispersal24. | High – Moderate |
| Nebulisers | Alter the composition of RTLF and viscosity. Subject‐dependent effect (24). Could reduce shear forces. | Associated in low quality studies. Increased dispersal 24. | High – Moderate |
HCW, Healthcare worker; SARS, severe acute respiratory syndrome; CPR, cardiopulmonary resuscitation; RTLF, respiratory tract lining fluid.
Formula A provides a simplified equation for the determinants of healthcare worker airborne risk. These can be mitigated by applying the methods listed in Table 2.
Table 2.
Precautions to prevent airborne transmission
| Environmental | Healthcare worker | Patient | Procedure |
|---|---|---|---|
| Increase room ventilation rates | Wear suitable PPE at times of transmission risk | Wear a surgical mask | Minimise shear stress on airways |
| If no formal ventilation system open windows and doors | Use a visor | Avoid coughing, sneezing, talking | Avoid airway open‐close cycling |
| Increase temperature, humidity and UV light | Use the most efficient airborne mask protection available | Avoid high minute volumes, expiratory flows and volumes | Avoid bronchoscopy and CPR |
| Avoid small crowded rooms | Keep out of direct exhalation plume | Avoid atelectasis | Use fitted sealed masks or hoods with viral filters |
| Minimise time in close contact with patient | Minimise suctioning | ||
| Breathe nasally and reduce minute volume | Prevent coughing |
PPE, personal protective equipment; UV, ultraviolet; CPR, cardiopulmonary resuscitation.
where: b = breathing zone particle viable virion aerosol concentration v = minute volume of healthcare worker t = time exposed e = mask efficiency.
Positive pressure ventilation
International airway management societies have developed guidelines to minimise the risk of healthcare worker COVID‐19 transmission during tracheal intubation and extubation 52. We defer to these, but offer some additional precautions based on the aerobiological literature summarised in Table 1.
Coronavirus disease 2019 patients with respiratory distress could produce high levels of aerosols secondary to cough; high airway pressures; minute volumes; altered secretions; and basal collapse. The same meticulous droplet and airborne precautions must be applied in these periods of close healthcare worker‐patient contact as during the AGPs.
In a patient receiving non‐invasive ventilation (NIV), airborne particle formation will be dependent on airway pressure differentials, gas flow velocities and open‐close cycling of distal airways. The quantity of fugitive particles escaping into the atmosphere will depend on circuit, mask or hood leak, viral filters and minute volumes 34, 53. During the 2003 epidemic, 20 SARS‐CoV‐1 infected patients were treated with NIV by over 100 health care workers. Using appropriate PPE, training and patient selection, zero transmission to healthcare workers was reported 3.
Spontaneously breathing patients exhale in a conical jet plume that is assumed to be at least 2 m in length, while healthcare workers inhalation will be drawn from 10 cm around the face. Whenever possible, healthcare workers should stand over 2 m away and out of the direct exhalation plume. During a rapid sequence intubation, neuromuscular blockade should be protective as coughing will be prevented and high airway gas flow and expiratory output will terminate. When expiratory flow is ended, as shown by absent respiratory effort and flat end‐tidal carbon dioxide trace, aerosol particles should start settling in the airways. The forces generated in gentle laryngoscopy are unlikely to cause aerosol formation. Suction typically generates a negative pressure of 100–200 cm H2O and is associated with a measured rise in H1N1 aerosol particles 47.
The scalpel incision, insertion of a gum‐elastic bougie and tracheal tube as part of an emergency surgical front‐of‐neck airway is unlikely to specifically generate aerosols per se. However, the newly formed cricothyroidotomy will immediately allow the escape of un‐viral‐filtered gases which will likely be high in aerosols due to recent high airway pressures and atelectasis. Extreme caution must be taken to minimise unfiltered gas leak through the new cricothyroidotomy and tracheal tube. In a ‘cannot ventilate cannot oxygenate’ scenario, the airway operator must avoid high pressures or volumes 52, 54.
Oxygen facemasks, nebulisers and high‐flow nasal oxygen
Facemasks act as barriers to high velocity particle plumes, leading to redirection and dispersal of aerosols. The distance the exhaled plume will travel is reduced to as low as 0.1–0.4 m with the application of a facemask 24. If the mask has an exhalation port gas will move directly out of this. Increased gas flow in the proximity of a patient should not increase the number of aerosols produced. It will disperse the expired tidal volume and plausibly increase the range of particles. Humidity is known to increase viral decay, so dry compressed gas potentially could increase viral viability.
Nebulisers increase the distance that an exhaled smoke jet plume will travel to 0.8 m 24. Moistening the upper airways could increase the larger droplets produced. It is plausible medical‐aerosol particles could collide with patient respiratory‐airborne particles in the mask, becoming larger droplets and therefore travelling a shorter distance. If a bronchospastic patient generates marked intrathoracic pressures, this will theoretically increase the production of aerosols. Human laboratory studies have shown significant unexplained heterogeneity in the respiratory particle output of individuals. When given saline 3% nebulisers, high particle output producers considerably reduced aerosol output, whereas those who produced small numbers of particles at baseline exhibited a rise. The overall effect was a marked drop in aerosols as the high particle producers contribute more to the total output 19. The benefit of using a nebuliser vs. the limited evidence against should be considered.
High‐flow nasal oxygen will disperse a concentrated jet of aerosols, potentially spreading them over a further distance, in a more dilute concentration. It provides humidification which can reduce viable virus load and if inspiratory pressures and minute volume are reduced, this is aerosol‐protective. However, unlike a continuous positive airway pressure (CPAP) mask or hood, there is no sealed exhalation path through a viral filter. At higher flows, for example 60 l.min−1, it is plausible this could generate local turbulence driven droplets within the oropharynx which will be flow rate dependent. It is important to note that this generates flows significantly less than a cough 53, 55. High‐flow nasal oxygen was used by physicians in China as a standard part of escalating respiratory support in the current pandemic to good effect 56, 57.
Cardiopulmonary resuscitation
Distal airway collapse, chest compressions, suctioning, unsecured bag‐mask ventilation and multiple people in close proximity to the airway will all create a high risk of healthcare worker transmission of SARS‐CoV‐2. This was demonstrated from the previous SARS‐CoV‐1 experience where multiple healthcare worker transmissions were recorded from one cardiopulmonary resuscitation (CPR) event 6. Efforts must be made to recognise deterioration and either escalate care or withhold CPR, if appropriate. In the event of a cardiac arrest secondary to respiratory failure in a COVID‐19 patient, it must be considered whether the risk to staff is acceptable when balanced with the likelihood of the patient surviving to a good functional outcome.
Conclusions
Due to the numerous complex dynamic variables, ‘droplet‐airborne’ spread should not be viewed as a dichotomy based on exact particle size and specific safe distances, but as a continuum over which probability of lung inoculation alters. Coughing, talking and tidal volume breathing produce respiratory tract lining fluid‐derived particles which could be inhaled into a respiratory portion of the lung 10, 11. The mechanisms of SARS‐CoV‐2 transmission are currently undetermined leaving a potential role for airborne infection 7. We speculate the respiratory pathophysiology of COVID‐19 could increase exhaled infectious particles. These particles could gain direct access to alveolar surface ACE‐2 receptors and transmit lung infection under suitable biological, physical and environmental conditions 58.
There is limited evidence to suggest AGPs cause an increase in airborne healthcare worker transmission, as this has not been studied. The few studies to sample pathogenic airborne particles in relation to procedures show no increase with the majority of AGPs 35, 47. Several of the AGPs have been shown to be periods of high risk to healthcare workers but the exact timing and cause of transmission is unknown 9. We observe an association between time in close proximity to SARS‐CoV‐1 patients requiring emergent respiratory therapy and increased staff transmission 1, 2, 4, 5, 6. Therefore, we would not limit meticulous airborne precaution to the procedural periods alone but increase this protection to all times of risk. Unfortunately, the specifics of what defines a high‐risk patient or activity remain undetermined. We have identified potential key determinants of airborne transmission (Fig. 1), which we combine with the limited known clinical evidence to risk stratify natural and medical aerosol generators (Table 1).
We speculate that in patients with a high viral load, respiratory symptoms and procedures that increase airway shear forces, open‐close airway cycling and un‐viral‐filtered expired minute volume would increase risk. Conversely, certain AGPs employing enhanced techniques and equipment could minimise aerosol production compared with a coughing patient with a high work of breathing. However, the existence of poorly understood asymptomatic ‘super‐spreaders’ highlights our knowledge‐gaps and a need for sustained vigilance during a pandemic.
The environmental, healthcare worker, patient and procedural measures for mitigating airborne risk (Table 2) will deter ‘direct‐droplet’ transmission reflecting the continuum across which these modes sit. Some of these measures can be applied without the addition of further PPE or cost. Given a global shortage in airborne protective equipment, regional centres must rationalise its use by appraising the current evidence and applying this to the risk of local transmission.
In the aftermath of the current pandemic, the exact mode of transmission may still remain controversial as was the case with SARS‐CoV‐1 and influenza. Urgent further research is required to investigate SARS‐CoV‐2 transmission, risk factors and strategies to assure the safety of healthcare workers. In the interim, healthcare workers may choose to take a precautionary approach until robust evidence is available.
Acknowledgements
We would like to thank Dr A. Chan (Consultant Anaesthetist and Intensivist, Prince of Wales Hospital, Hong Kong) and Dr E. Tovey (Honorary Affiliate Senior Research Fellow, Woolcock Institute, University of Sydney) for assistance with the manuscript. No external funding or competing interests declared.
References
- 1. Park BJ, Peck AJ, Kuehnert MJ, et al. Lack of SARS transmission among healthcare workers, United States. Emerging Infectious Diseases 2004; 10: 217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fowler RA, Guest CB, Lapinsky SE, et al. Transmission of severe acute respiratory syndrome during intubation and mechanical ventilation. American Journal of Respiratory and Critical Care Medicine 2004; 169: 1198–202. [DOI] [PubMed] [Google Scholar]
- 3. Cheung TMT, Yam LYC, So LKY, et al. Effectiveness of noninvasive positive pressure ventilation in the treatment of acute respiratory failure in severe acute respiratory syndrome. Chest 2004; 126: 845–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Loeb M, McGeer A, Henry B, et al. SARS among critical care nurses, Toronto. Emerging Infectious Diseases 2004; 10: 251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lau JTF, Fung KS, Wong TW, et al. SARS transmission among hospital workers in Hong Kong. Emerging Infectious Diseases 2004; 10: 280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Christian MD, Loutfy M, McDonald LC, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerging Infectious Diseases 2004; 10: 287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organisation . Modes of transmission of virus causing COVID‐19: implications for IPC precaution recommendations. 2020. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed 08/04/2020).
- 8. Gu J, Han B, Wang J. COVID‐19: gastrointestinal manifestations and potential fecal‐oral transmission. Gastroenterology 2020. Epub 3 March. 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tran K, Cimon K, Severn M, Pessoa‐Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012; 7: e35797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. American Journal of Infection Control 2016; 44: S102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Almstrand A‐C, Bake B, Ljungström E, et al. Effect of airway opening on production of exhaled particles. Journal of Applied Physiology 2010; 108: 584–8. [DOI] [PubMed] [Google Scholar]
- 12. Bredberg A, Gobom J, Almstrand A‐C, et al. Exhaled endogenous particles contain lung proteins. Clinical Chemistry 2012; 58: 431–40. [DOI] [PubMed] [Google Scholar]
- 13. Lindsley WG, Pearce TA, Hudnall JB, et al. Quantity and size distribution of cough‐generated aerosol particles produced by influenza patients during and after illness. Journal of Occupational and Environmental Hygiene 2012; 9: 443–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lindsley WG, Noti JD, Blachere FM, et al. Viable influenza A virus in airborne particles from human coughs. Journal of Occupational and Environmental Hygiene 2015; 12: 107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blachere FM, Lindsley WG, Pearce TA, et al. Measurement of airborne influenza virus in a hospital emergency department. Clinical Infectious Diseases 2009; 48: 438–40. [DOI] [PubMed] [Google Scholar]
- 16. Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathogens 2013; 9: e1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kormuth KA, Lin K, Prussin AJ, et al. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity. Journal of Infectious Diseases 2018; 218: 739–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Seto WH. Airborne transmission and precautions: facts and myths. Journal of Hospital Infection 2015; 89: 225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Edwards DA, Man JC, Brand P, et al. Inhaling to mitigate exhaled bioaerosols. Proceedings of the National Academy of Sciences of the United States of America 2004; 101: 17383–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miguel AF. Penetration of inhaled aerosols in the bronchial tree. Medical Engineering and Physics 2017; 44: 25–31. [DOI] [PubMed] [Google Scholar]
- 21. Johnson GR, Morawska L, Ristovski ZD, et al. Modality of human expired aerosol size distributions. Journal of Aerosol Science 2011; 42: 839–51. [Google Scholar]
- 22. Gralton J, Tovey E, McLaws M‐L, Rawlinson WD. The role of particle size in aerosolised pathogen transmission: a review. Journal of Infection 2011; 62: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles, 2nd edn. New York: Wiley, 1999. [Google Scholar]
- 24. Xie X, Li Y, Chwang ATY, Ho PL, Seto WH. How far droplets can move in indoor environments–revisiting the Wells evaporation‐falling curve. Indoor Air 2007; 17: 211–25. [DOI] [PubMed] [Google Scholar]
- 25. Tellier R. Review of aerosol transmission of influenza A virus. Emerging Infectious Diseases 2006; 12: 1657–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Loudon RG, Roberts RM. Relation between the airborne diameters of respiratory droplets and the diameter of the stains left after recovery. Nature 1967; 213: 95–6. [Google Scholar]
- 27. Duguid JP. The size and the duration of air‐carriage of respiratory droplets and droplet‐nuclei. Journal of Hygiene 1946; 44: 471–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. Journal of Aerosol Medicine 1997; 10: 105–16. [DOI] [PubMed] [Google Scholar]
- 29. Bake B, Larsson P, Ljungkvist G, Ljungström E, Olin A‐C. Exhaled particles and small airways. Respiratory Research 2019; 20: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID‐19. Journal of the American Medical Association 2020; 323: 1837–38. [DOI] [PubMed] [Google Scholar]
- 31. Yu ITS, Li Y, Wong TW, et al. Evidence of airborne transmission of the severe acute respiratory syndrome virus. New England Journal of Medicine 2004; 350: 1731–9. [DOI] [PubMed] [Google Scholar]
- 32. Wells WF. Air‐borne infection. Journal of the American Medical Association 1936; 107: 1698. [Google Scholar]
- 33. Lowen AC, Steel J. Roles of humidity and temperature in shaping influenza seasonality. Journal of Virology 2014; 88: 7692–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hui DSC, Chan MTV, Chow B. Aerosol dispersion during various respiratory therapies: a risk assessment model of nosocomial infection to health care workers. Hong Kong Medical Journal 2014; 20(Suppl. 4): 9–13. [PubMed] [Google Scholar]
- 35. O'Neil CA, Li J, Leavey A, et al. Characterization of aerosols generated during patient care activities. Clinical Infectious Diseases 2017; 65: 1342–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proceedings of the Society for Experimental Biology and Medicine 1966; 122: 800–4. [DOI] [PubMed] [Google Scholar]
- 37. Snyder MH, Stephenson EH, Young H, et al. Infectivity and antigenicity of live avian‐human influenza A reassortant virus: comparison of intranasal and aerosol routes in squirrel monkeys. Journal of Infectious Diseases 1986; 154: 709–11. [DOI] [PubMed] [Google Scholar]
- 38. Loosli CG, Lemon HM, Robertson OH, Appel E. Experimental air‐borne influenza infection. I. Influence of humidity on survival of virus in air. Experimental Biology and Medicine 1943; 53: 205–6. [Google Scholar]
- 39. Cowling BJ, Ip DKM, Fang VJ, et al. Aerosol transmission is an important mode of influenza A virus spread. Nature Communications 2013; 4: 1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yang W, Elankumaran S, Marr LC. Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day‐care centre and on aeroplanes. Journal of the Royal Society, Interface 2011; 8: 1176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wong T, Lee C, Tam W, et al. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerging Infectious Diseases 2004; 10: 269–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Booth TF, Kournikakis B, Bastien N, et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. Journal of Infectious Diseases 2005; 191: 1472–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. Journal of Pathology 2004; 203: 631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin‐converting enzyme 2 (ACE2) as a SARS‐CoV‐2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Medicine 2020. Epub 3 March. 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS‐CoV‐2 as Compared with SARS‐CoV‐1. New England Journal of Medicine 2020; 382: 1564–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) From a Symptomatic Patient. Journal of the American Medical Association 2020; 323: 1610–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Thompson K‐A, Pappachan JV, Bennett AM, et al. Influenza aerosols in UK hospitals during the H1N1 (2009) pandemic – the risk of aerosol generation during medical procedures. PLoS ONE 2013; 8: e56278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Li J, Leavey A, Yang W, et al. Defining aerosol generating procedures and pathogen transmission risks in healthcare settings. Open Forum Infectious Diseases 2017; 4: S34–5. [Google Scholar]
- 49. Nucci G, Suki B, Lutchen K. Modeling airflow‐related shear stress during heterogeneous constriction and mechanical ventilation. Journal of Applied Physiology 2003; 95: 348–56. [DOI] [PubMed] [Google Scholar]
- 50. Olafsson S, Hyatt RE. Ventilatory mechanics and expiratory flow limitation during exercise in normal subjects. Journal of Clinical Investigation 1969; 48: 564–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yoshida T, Grieco DL, Brochard L, Fujino Y. Patient self‐inflicted lung injury and positive end‐expiratory pressure for safe spontaneous breathing. Current Opinion in Critical Care 2020; 26: 59–65. [DOI] [PubMed] [Google Scholar]
- 52. Cook TM, El‐Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID‐19. Anaesthesia 2020; 75: 785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during high‐flow nasal cannula therapy versus CPAP via different masks. European Respiratory Journal 2019; 53: 1802339. [DOI] [PubMed] [Google Scholar]
- 54. Cook TM, El‐Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID‐19. Anaesthesia 2020. 75: 785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lyons C, Callaghan M. The use of high‐flow nasal oxygen in COVID‐19. Anaesthesia 2020; 75: 843–847. [DOI] [PubMed] [Google Scholar]
- 56. Zhejiang University School of Medicine . Handbook of COVID‐19 Prevention and Treatment. 2020. https://iau-aiu.net/Zhejiang-University-Handbook-of-COVID-19-Prevention-and-Treatment (accessed 28/03/2020).
- 57. Wang K, Zhao W, Li J, Shu W, Duan J. The experience of high‐flow nasal cannula in hospitalized patients with 2019 novel coronavirus‐infected pneumonia in two hospitals of Chongqing, China. Annals of Intensive Care 2020; 10: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019‐nCoV on the epithelial cells of oral mucosa. International Journal of Oral Science 2020; 12: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]


