Coronavirus disease 2019 (COVID‐19) is particularly deleterious to older adults,1 and there has been a massive increase in reports of elder abuse during the pandemic. Reports of elder abuse range from financial scams to incidents of family violence, with public warnings issued accordingly from the Federal Trade Commission2 and the American Bar Association.3 The Centers for Disease Control and Prevention defines elder abuse as an intentional act or failure to act by a caregiver or another person in a relationship involving an expectation of trust that causes or creates a risk of harm to an older adult.4 Abuse of older adults can be physical, emotional, financial, neglect, or any combination of these. To better understand the complex dynamics that lead to elder abuse, our group developed a theoretical model called the Abuse Intervention/Prevention Model (AIM5). This model focuses on three core and intersecting considerations: (1) the vulnerable older adult, (2) the trusted other, and (3) the context in which the abuse occurs. We consider each of these in relation to the COVID‐19 pandemic and end with suggested ways to mitigate the risks.
THE VULNERABLE OLDER ADULT
A model of elder abuse must begin with an understanding of the vulnerability profile of the older adult. Vulnerabilities can encompass physical, emotional, cognitive, and financial considerations, and those who are experiencing frailty in any of these facets of life are at greater risk. We know aging adults are a particularly vulnerable group to the deleterious effects of COVID‐19. This knowledge likely exacerbates already high rates of depressive and anxiety symptoms, resulting in an even greater multidimensional state of vulnerability. The many necessary social distancing programs currently in place additionally create a growing dependency on others for the completion of daily living activities, and this dependency can be viewed as another vulnerability. The documented negative health effects of social isolation and loneliness in old age6 will undoubtedly intensify during this pandemic, and social isolation has been established as one of the strongest predictors of elder abuse.
THE TRUSTED OTHER
The “trusted other” is a term that broadly refers to others surrounding the vulnerable older adult, and can refer to family members, caregivers, neighbors, friends, and financial advisors. The degree to which these others are involved in the life of an older adult can vary; however, there is a general expectation that these others will act in accordance of mutual well‐being and trust. The trusted other becomes a consideration for elder abuse when trust is broken, similar to situations of domestic violence or child abuse. With numerous “shelter‐in‐place” orders in effect to promote social distancing during the COVID‐19 era, and increased dependency of older adults on others, the potential for elder abuse is all the more heightened, particularly since perpetrators of abuse are often close relations,7 and as more strangers opportunistically strive to take advantage of the fearful situation to exploit older adults for financial gain.2 Older adults with dementing illness are known to be of higher risk for abuse and neglect. With the shuttering of adult daycare programs, senior centers, and outpatient programs occurring concomitantly with adult children working from home, the possibility of unbuffered time together may contribute to circumstances leading to greater incidents of abuse.
THE CONTEXT
In the AIM model,6 contextual factors, such as cultural norms, inform elder abuse dynamics. Another contextual factor that colors virtually every discussion of older adults in the COVID‐19 pandemic is ageism. The World Health Organization defines ageism as “the stereotyping, prejudice, and discrimination against people on the basis of their age,”8 and a recent systematic review found ageism to be associated with numerous negative health consequences worldwide.9 Ageism is pervasive, harmful, and arguably the primary vice underlying elder abuse. From the beginning, coronavirus has inspired ageist thoughts and comments given its predilection toward harming older adults. As the consequences of necessary social distancing increase, ageist views will continue to rise to the surface, potentially leading to tragic and unjust utilitarian conversations about “the needs of the many versus the needs of the few.”
MITIGATION
Although the risks of elder abuse in the COVID‐19 pandemic will increase, steps can be taken to mitigate them (Figure 1). The vulnerabilities of older adults and the dependencies they create can be proactively addressed with organized, systematic, and creative efforts. Older adults within families and local communities can be contacted on a regular basis by those who are designated as advocates. Multiple communication methods can be leveraged for this purpose, similar to the development of telehealth approaches that the medical community is mobilizing. Creativity in the development of resources to address specific vulnerabilities should be encouraged. The ingenuity of developing specific hours for older adult shopping by some commercial stores is a brilliant example of this. Ways to address the potential threat of a trusted other range from increasing penalties for elder abuse at the societal level to the creation of an individualized safety plan that incorporates the wishes and preferences for autonomy and self‐reliance of the older adult. Caregivers of older adults with dementia or other medical conditions are under particular strain given their responsibilities and should be offered additional means of support and guidance. To combat rampant and increasing ageism, the perspective of older adults can be elevated by increasing representation on panels with significant decision‐making power in public and private sectors during the pandemic. Those who have a substantial social media footprint can be of particular help combating ageist sentiments. Creative community‐based resources that address any of these three intersecting domains of elder abuse must be rapidly developed and implemented. Resources such as the National Center on Elder Abuse10 and local Adult Protective Service entities are actively adapting their services to help protect older adults. Religious and nonprofit organizations can play a key role in the development of programs to further buttress against the rising wave of elder abuse and neglect.
Figure 1.
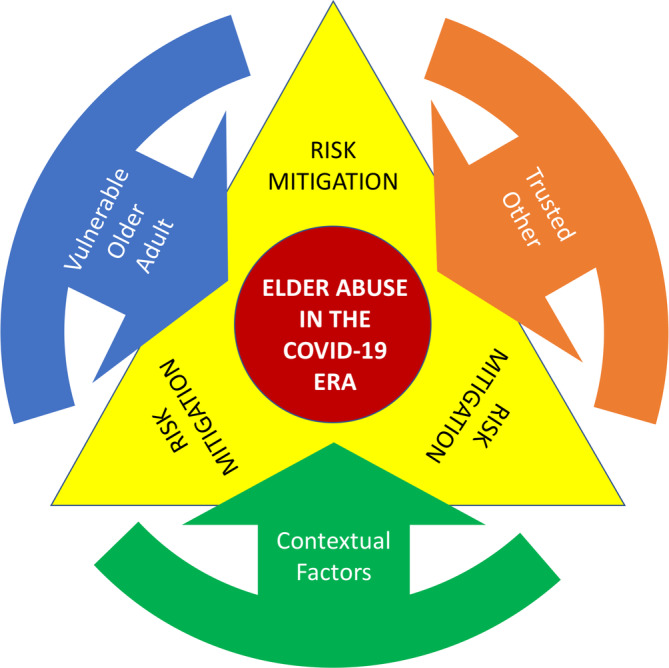
Abuse Invention/Prevention Model (AIM). AIM describes three core intersecting considerations in elder abuse: (1) the vulnerable older adult, (2) the trusted other, and (3) the context in which the abuse occurs. Tailored approaches that consider each of these can be developed to mitigate risks for elder abuse in the coronavirus disease 2019 (COVID‐19) era.
ACKNOWLEDGMENTS
Financial Disclosure
This work was supported by the National Institute on Aging at the National Institutes of Health grants (R01AG055430 to S.D.H., R01AG060096 to L.M.) and the Administration for Community Living grant (90ABRC0001‐02‐00 to L.M.), as well as the Department of Family Medicine of the University of Southern California.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author Contributions
S.D.H. and L.M.: conception and design, drafting the article, and final approval.
Sponsor's Role
None.
REFERENCES
- 1. Dong E, Du H, Gardner L. An interactive web‐based dashboard to track COVID‐19 in real time. Lancet Infect Dis. 2020. 10.1016/S1473-3099(20)30120-1. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. https://www.consumer.ftc.gov/blog/2020/02/coronavirus-scammers-follow-headlines. Accessed April 15, 2020.
- 3. https://www.americanbar.org/groups/law_aging/resources/coronavirus-update/coronavirus-and-elder-abuse/. Accessed April 15, 2020.
- 4. Hall JE, Karch DL, Crosby AE. Elder Abuse Surveillance: Uniform Definitions and Recommended Core Data Elements for Use in Elder Abuse Surveillance, Version 1.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 5. Mosqueda L, Burnight K, Gironda MW, Moore AA, Robinson J, Olsen B. The abuse intervention model: a pragmatic approach to intervention for elder mistreatment. J Am Geriatr Soc. 2016;64:1879‐1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ong AD, Uchino BN, Wethington E. Loneliness and health in older adults: a mini‐review and synthesis. Gerontology. 2016;62:443‐449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weissberger GH, Goodman MC, Mosqueda L, et al. Elder abuse characteristics based on calls to the National Center on Elder Abuse resource line. J Appl Gerontol. 2019. 10.1177/0733464819865685. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. https://www.who.int/ageing/ageism/en/. Accessed April 15, 2020.
- 9. Chang E‐S, Kannoth S, Levy S, Wang S‐Y, Lee JE, Levy BR. Global reach of ageism on older persons’ health: a systematic review. PLoS One. 2020;15(1):e0220857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. https://ncea.acl.gov/. Accessed April 15, 2020.


