The World Health Organization considers noncommunicable diseases, such as obesity, to be a major risk factor for becoming seriously ill with 2019 novel coronavirus (COVID‐19) (1). A study by the UK Intensive Care National Audit and Research Centre indicates that two‐thirds of people who have developed serious or fatal COVID‐19–related complications had overweight or obesity (2). The report includes data from all COVID‐19 admissions in intensive care units in the UK until midnight, March 19, 2020. The study shows that almost 72% of those in critical care units had either overweight or obesity, suggesting the impact of obesity in seriously ill COVID‐19 patients.
At the outset of the COVID‐19 outbreak, the Italian National Institute of Health (Instituto Superiore di Sanità) launched a surveillance system to collect information on all people with COVID‐19 throughout the country. Data on all COVID‐19 cases were obtained from all 19 Italian regions and the 2 autonomous provinces of Trento and Bozen (3). The report from Italy indicates that 99% of deaths occurred in patients with preexisting noncommunicable diseases, such as obesity, hypertension, type 2 diabetes mellitus, heart disease, kidney damage, and cancer (3). As of April 2, 2020, 145 of the 12,250 (1.2%) COVID‐19–positive patients under the age of 50 have died. In particular, 35 of these were less than 40 years, 94 men and 26 women (age range between 26 and 39 years). For 14 patients under the age of 40 years, no clinical information is available; the remaining 18 had serious preexisting pathologies, such as severe obesity and its comorbidities (cardiovascular, renal, diabetes mellitus, and psychiatric pathologies), and 3 had no major pathologies (3).
The frequent co‐occurrence of both obesity and diabetes can clearly confound or at least make more difficult the identification of the independent role of obesity. The anamnestic collection of the history of diabetes and other active obesity comorbidities at the time of admission is what is important to separate the risk of obesity from its comorbid complications for the development of serious COVID‐19 infection.
Obesity seems to be a risk factor for poor adverse outcomes of COVID‐19, as summarized in Figure 1. The propensity of people with obesity to develop more serious complications if exposed to a virus could be attributed to multiple factors, such as the chronic inflammatory status and the delayed and ineffective immune response. Nevertheless, so far, the adipose tissue has been not been taken into full consideration as a major player of the COVID‐19 infection
Figure 1.
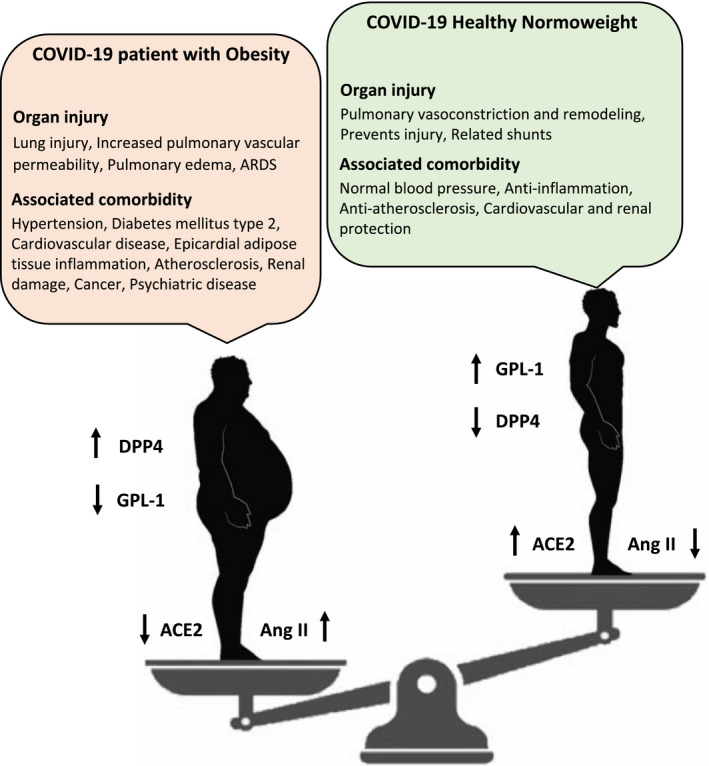
Cartoon depicts imbalance between individuals with obesity and normal weight in developing COVID‐19 complications. [Color figure can be viewed at wileyonlinelibrary.com]
Severe acute respiratory syndrome coronavirus (SARS‐CoV) binds with the angiotensin converting enzyme 2 (ACE2) receptor for intracellular invasion, and the mechanism for acute lung injury during infection has been postulated to be mediated through the activation of the renin‐angiotensin system (RAS) (4). RAS blockade has been proposed as a potential treatment for COVID‐19 (5). Remarkably, ACE2 is expressed in the human adipose tissue. The overall ACE/angiotensin II/type 1 angiotensin 2 receptor RAS axis activation plays an important role in the pathophysiology of obesity and visceral adiposity‐related cardiac risk (6). The interaction between the ACE2‐RAS system, adipose tissue, and COVID‐19 could, at least partially, explain the higher morbidity and mortality risk for COVID‐19 patients with obesity. However, the role of ACE2‐RAS in COVID‐19 remains to be elucidated.
Human dipeptidyl peptidase 4 (DPP4) was also identified as a functional receptor for the spike protein of the Middle East respiratory syndrome (MERS)‐CoV (7). MERS‐CoV binds to the receptor‐binding domain and interacts with T cells and nuclear factors involved in the pathogenesis of inflammatory disorders. DPP4, a transmembrane protein, has been identified in human adipose tissue and is associated with obesity‐related type 2 diabetes. DPP4 inhibition increases glucagon like peptide‐1 secretion, leading to an improved insulin sensitivity and glucose metabolism within the adipocyte. DPP4 inhibition could also play a role in the immune response to COVID‐19 by reducing inflammation (8). Inhibition of the DPP4 enzymatic activity suppresses T‐cell proliferation and the secretion of proinflammatory cytokines, such as interleukin (IL)‐6 and ‐10 (9).
Besides the expression of these enzymes and their possible role, there are multiple mechanisms by which the adipose tissue may contribute to the development and progression of COVID‐19 (10). Complex interactions occur between the immune system and adipose tissue. The overexpression of inflammatory adipokines from visceral fat depots can affect the immune response, impair the chemotaxis, and alter the macrophage differentiation. The imbalance between anti‐ and proinflammatory adipokine secretion from thoracic visceral fat depots, such as the epicardial and mediastinal, can also play a role in the cytokine storm described in patients with severe SARS‐COv2. Interestingly, adiponectin was reported to predict mortality in critically ill patients upon admission to the intensive care unit. The innate inflammatory response of the visceral fat depots can cause an upregulation and higher release of inflammatory cytokines such as IL‐6. Excessive proinflammatory cytokine release was thought to be the link between visceral obesity and influenza‐related severe respiratory complications. As elderly individuals are at higher risk of COVID‐19 complications and poorer outcome, it is worth noting that aging can cause visceral fat accumulation and adipose tissue inflammation and fibrosis. Similar changes have also been described in patients with HIV.
Hence, the role of the adipose tissue during infectious diseases, such as COVID‐19, could be important. If obesity represents a predictor for poor prognosis or higher rate of complications in SARS‐Cov2 patients, it is still a modifiable risk factor. Therapeutic actions targeting the adipose tissue may be considered to reduce the burden of COVID‐19.
References
- 1. Ryan DH, Ravussin E, Heymsfield S. COVID 19 and the patient with obesity ‐ the editors speak out. Obesity (Silver Spring) 2020;28:847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. ICNARC . Report on 196 patients critically ill with COVID‐19. https://www.icnarc.org/About/Latest‐News. Published March 22, 2020. Accessed March 22, 2020.
- 3. EpiCentro ‐ Istituto Superiore di Sanità . Characteristics of COVID‐19 patients dying in Italy. Report based on available data on April 2nd, 2020. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report‐COVID‐2019_2_april_2020.pdf. Accessed April 2, 2020.
- 4. Li W, Moore MJ, Vasilieva N, et al. Angiotensin‐converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 2003;426:450‐454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gurwitz D. Angiotensin receptor blockers as tentative SARS‐CoV‐2 therapeutics [published online March 4, 2020]. Drug Dev Res. doi: 10.1002/ddr.21656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin‐angiotensin‐aldosterone system inhibitors in patients with COVID‐19. N Engl J Med 2020;382:1653‐1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Raj VS, Mou H, Smits SL, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus‐EMC. Nature 2013;495:251‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Iacobellis G. COVID‐19 and Diabetes: can DPP4 inhibition play a role? Diabetes Res Clin Pract 2020;26:108125. doi: 10.1016/j.diabres.2020.108125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reinhold D, Brocke S. DPP4‐directed therapeutic strategies for MERS‐CoV. Lancet Infect Dis 2014;14:100‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes (Lond) 2013;37:333‐340. [DOI] [PubMed] [Google Scholar]


