To the Editor,
The coronavirus disease 2019 (COVID‐19) pandemic started as an outbreak in Wuhan and spread from there to the rest of the world. The lungs are the site primarily affected by COVID‐19 and the severe form of the disease is characterized by severe pneumonia, acute respiratory distress syndrome (ARDS), and hypercoagulation. 1
Until now, the exact transmission route of COVID‐19 remains unclear. The respiratory tract probably is not the only transmission route for this viral infection; some authors hypothesized that COVID‐19 droplets, or infected hands, can also contaminate the conjunctiva, that could represent the initial site of a spread infection. 2 The conjunctivitis, also called “Pink eye,” is a frequent disease and its etiology could be bacterial or viral. This has been previously described as associated to coronavirus infection in humans and animals. 3
Recent studies showed that conjunctivitis could be a manifestation of COVID‐19. 4 Because the eye could be considered as a direct potential portal of entry for the virus, 5 it is of interest to analyze the association between conjunctivitis and the severity of COVID‐19; scarce and conflicting data have been reported. In particular, only three studies in Chinese population described this topic, 6 with different results. Xia et al 7 did not find an increased incidence of conjunctivitis in severe COVID‐19; they performed a prospective study in 30 COVID‐19 patients to assess the presence of the virus in the tears. 7 Conversely, Guan et al, 6 who retrospectively analyzed clinical characteristics of 1099 COVID‐19 patients, and Wu et al, 8 who retrospectively investigated the ocular characteristics of 38 COVID‐19 patients, reported an increased incidence of conjunctivitis in patients with severe disease.
Thus, to better explore this issue, this meta‐analysis aims to evaluate the incidence of conjunctivitis in patients affected by severe and nonsevere COVID‐19.
Methods are reported in Supporting Information Material.
We included studies in patients with COVID‐19 that assessed the severe (as severe pneumonia, mortality, ARDS, use of mechanical ventilation or intensive care unit recovery) and nonsevere forms of the disease and reported the incidence of conjunctivitis.
Three studies, 6 , 7 , 8 including 1167 patients, assessed the clinical course of patients with COVID‐19 and presence or absence of conjunctivitis. Clinical characteristics of the studies are reported in Supporting Information Material. The age of the patients enrolled ranged from a median of 47 to 68 years old and the male sex was prevalent in all the studies.
The presence of COVID‐19 at conjunctival polymerase chain reaction (PCR) was analyzed only by Xia and Wu; only in 4% (3/68) of the cases, PCR revealed the positivity of COVID‐19 (Supporting Information Material).
The overall rate of conjunctivitis was 1.1%; it was 3% and 0.7% in severe and nonsevere COVID‐19 patients, respectively. The meta‐analysis showed that patients with severe COVID‐19 infection had, at admission to the hospital, increased incidence of conjunctivitis (odds ratio: 3.4; 95% confidence interval:1.1‐10.2; P = .030) (Figure 1). No heterogeneity between trials was observed (I 2 = 0); the publication bias was not statistically significant (Egger's test; P = .336).
Figure 1.
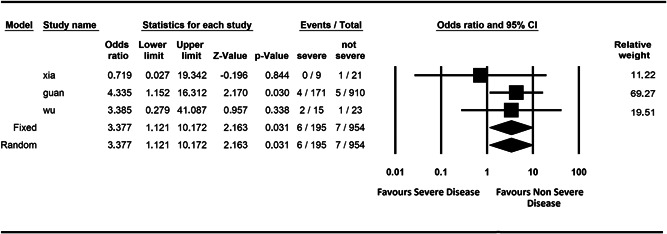
Meta‐analysis of conjunctivitis in patients with severe vs nonsevere coronavirus disease 2019
This meta‐analysis provides evidence that conjunctivitis could be associated with a more severe form of COVID‐19.
Previous studies reported about eye infection and conjunctivitis in animals and humans infected by coronavirus. 3 However, the role of conjunctiva in COVID‐19 still remains unclear. 9 , 10
The results of this study could have important clinical implications. First, medical doctors have to recognize conjunctivitis as a possible sign of COVID‐19 associated to a severe form of disease. Second, considering that eye could be a COVID‐19 route, we want to underscore the necessity to use protective equipment for healthcare personnel and for all the people that enter in contact with a suspected or diagnosed COVID patient. To confirm the importance of eye protection, a previous study in patients infected by SARS‐COV‐1 showed that unprotected eye contact was associated with transmission of the disease to healthcare workers. 11
This study has the following limitations. First, even if this meta‐analysis included 1167 COVID‐19 patients, more studies with a major number of patients are needed to have solid results. Second, conjunctival swab to test the local involvement of COVID‐19 was not reported in all the studies; however, a previous study showed that conjunctival swab test results positive for COVID‐19 only in about 5% of the patients. 8 Third, the population included in this meta‐analysis is composed only of Chinese patients who might have different clinical features from those of the patients of other countries. Future studies in other populations will be necessary to confirm the results of this meta‐analysis.
In conclusion, the results of this meta‐analysis show that conjunctivitis may represent a sign of COVID‐19 infection associated to a more severe form of disease and suggest the use of protective equipment for all people potentially exposed to infected subjects.
Supporting information
Supporting information
REFERENCES
- 1. Violi FPD, Cangemi R, Pignatelli P, Loffredo L. Hypercoagulation and anti‐thrombotic treatment in COVID‐19: a new challenge. Thromb Haemost. 2020. 10.1055/s-0040-1710317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li JO, Lam DSC, Chen Y, Ting DSW. Novel Coronavirus disease 2019 (COVID‐19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104(3):297‐298. [DOI] [PubMed] [Google Scholar]
- 3. Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID‐19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28(3):391‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Qing H, Li Z, Yang Z, et al. The possibility of COVID‐19 transmission from eye to nose. Acta Ophthalmol. 2020;98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Belser JA, Rota PA, Tumpey TM. Ocular tropism of respiratory viruses. MMBR. 2013;77(1):144‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guan W‐j, Ni Z‐y, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. 10.1056/nejmoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol. 2020;92:589‐594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID‐19) in Hubei province, China. JAMA Ophthalmol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guo D, Xia J, Shen Y, Tong J. SARS‐CoV‐2 may be related to conjunctivitis but not necessarily spread through the conjunctiva SARS‐CoV‐2 and conjunctiva. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liu Z, Sun CB. Conjunctiva is not a preferred gateway of entry for SARS‐CoV‐2 to infect respiratory tract. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Raboud J, Shigayeva A, McGeer A, et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010;5(5):e10717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


