To Editor
Protecting healthcare workers (HCWs) is crucial during Corona Virus Disease 2019 pandemic and requires wearing personal protective equipment (PPE). 1 While most of the studies have focused on the skin reactions caused by gloves, other PPE such as gowns, respirator masks, face shields and goggles are also worn by HCWs for long hours during the current epidemic and skin irritations caused by these equipment may cause discouragement of health workers from using them. 2 In this letter, we have focused on the reaction caused by non‐glove PPE.
The N95 respirator masks are made of polypropylene fabric processed by a non‐woven technology and should fit tightly to the face to be effective. 3 The study by Foo et al. revealed that 35.5% of the staff who used N95 masks regularly experienced acne, facial dermatitis and pigmentation of nasal bridge, cheeks and chin. In this study, acne was one of the most prevalent skin reactions related to the use of N95 respirator masks. 3 The dermatitis that often presented with pruritic skin lesions was mostly irritant type but allergic contact dermatitis (ACD) due to adhesives or other parts of the respirator masks such as rubber straps and metal clips was also reported. 3 Several factors including humidity, warm environment and occlusion due to local pressures could explain the exacerbation of these conditions. 3 In another study by Donovan et al., 4 on the possible N95 mask reactions during the SARS epidemic in Toronto, urticarial facial eruption was reported in three patients, dermatitis in five patients and acute respiratory symptoms without skin lesions in two patients. Pressure effect on the nose has also been reported as one of the 15 delphi measures that discouraged HCWs to use N95 respirator masks. 5
Goggles have been used routinely to protect HCWs against highly infectious diseases related to exposure to contaminated body fluids. 6 Heat and dehydration were major complications of both goggles and face shields application during the Ebola outbreak. 7 Other dermatologic side‐effects such as pressure injury, contact dermatitis, urticaria, xerosis and aggravation of underlying dermatosis might occur due to the impairment of the skin integrity during mechanical trauma of goggles. 8 A study by Lan et al., 2 revealed that 87.9% of HCWs, who were wearing goggles for more than 6 h, developed skin reactions on their nasal bridge. Skin reactions such as acne, ACD and irritant contact dermatitis (ICD) were mentioned following the use of goggles in HCWs. Occlusion and friction were mentioned as the underlying mechanism. 6
Wearing gowns and coveralls may cause heat stress and dehydration. 7 Skin reactions due to the clothing, which are made of natural and synthetic untreated fabrics, are rare. 9 However, additive chemicals and dye fibres might be the main reason of ICD and ACD. 9 Skin dermatoses are mostly developed where the gowns adhere tightly to the skin. 10 Friction, moisture and warmth of those regions might increase the risk of ACD. 10 In the study by Foo et al., 3 four (1.6%) out of 258 cases developed adverse skin reactions related to the repetitive wearing of disposable gowns for average time of 6.2 h during a mean period of 8.8 months in the SARS epidemic in Singapore. Itching and wrist rashes were the most frequent reactions, while pruritus without skin lesions was also observed in one case. 3 In Toronto SARS epidemic, there were reports of developing ACD due to the reaction to formaldehyde textiles and resin in gowns. 10 Avoiding over‐tight gowns and sufficient ingestion of liquids are of paramount importance for HCWs to preserve a balance between self‐protection and the ability to care for patients efficiently, while wearing PPE. Skin reactions to personal protective equipment and management strategies are depicted in Fig. 1.
Figure 1.
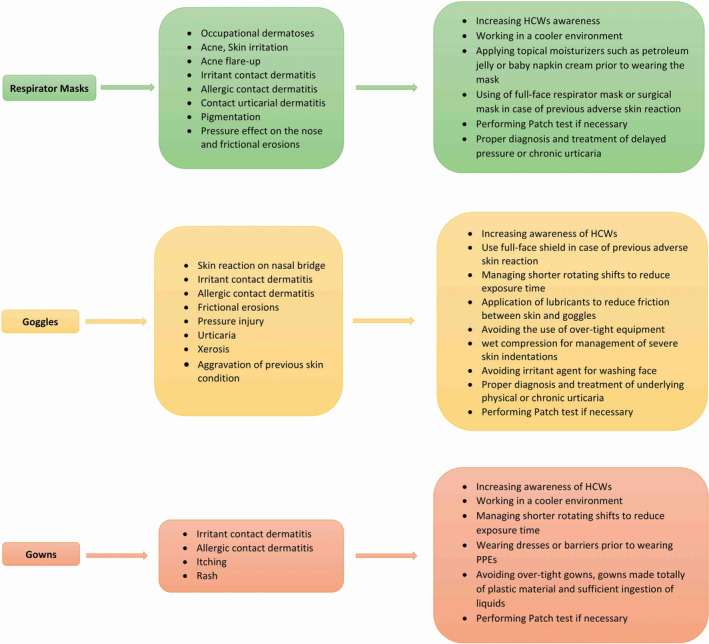
Adverse skin reaction to personal protective equipment and management strategies.
Acknowledgement
The patients in this manuscript have given written informed consent to publication of their case details.
Contributor Information
M. Tabary, Email: mohammadrezatabary@gmail.com.
S. Dadkhahfar, Email: sahar.dadkhahfar@gmail.com.
References
- 1. Zhou P, Huang Z, Xiao Y, Huang X, Fan XG. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect Control Hosp Epidemiol 2020; 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oranges T, Janowska A, Dini V. Reply to: “Skin damage among healthcare workers managing coronavirus disease‐2019”. J Am Acad Dermatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Foo CCI, Goon ATJ, Leow YH, Goh CL. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome–a descriptive study in Singapore. Contact Dermatitis 2006; 55: 291–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Donovan J, Kudla I, Holness LD, Skotnicki‐Grant S, Nethercott JR. Skin reactions following use of N95 facial masks. Dermatitis 2007; 18: 104. [Google Scholar]
- 5. Honarbakhsh M, Jahangiri M, Farhadi P. Effective factors on not using the N95 respirators among health care workers: application of fuzzy delphi and fuzzy analytic hierarchy process (FAHP). J Healthc Risk Manag 2017; 37: 36–46. [DOI] [PubMed] [Google Scholar]
- 6. Bhoyrul B, Lecamwasam K, Wilkinson M et al. A review of non‐glove personal protective equipment‐related occupational dermatoses reported to EPIDERM between 1993 and 2013. Contact Dermatitis 2019; 80: 217–221. [DOI] [PubMed] [Google Scholar]
- 7. Den Boon S, Vallenas C, Ferri M, Norris SL. Incorporating health workers’ perspectives into a WHO guideline on personal protective equipment developed during an Ebola virus disease outbreak. F1000Research. 2018; 7: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yan Y, Chen H, Chen L et al. Consensus of Chinese experts on protection of skin and mucous membrane barrier for healthcare workers fighting against coronavirus disease 2019. Dermatol Ther 2020; e13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fowler JF. Formaldehyde as a textile allergen. Curr Probl Dermatol 2003; 31: 156–165. [DOI] [PubMed] [Google Scholar]
- 10. Donovan J, Skotnicki‐Grant S. Allergic contact dermatitis from formaldehyde textile resins in surgical uniforms and nonwoven textile masks. Dermatitis. 2007; 18: 40–44. [DOI] [PubMed] [Google Scholar]


