Abstract
Background/aim
Competitive alpine skiing is known to be associated with a high risk of traumatic knee injuries. However, little is known about the exact prevalence of knee overuse injuries and their associations with structural changes, particularly in youth skiers. Accordingly, the aim of the present study was to describe the overuse-related knee complaints and MRI abnormalities in a cohort of youth skiers around the growth spurt.
Methods
108 youth competitive alpine skiers aged 13–15 years were examined using an MRI of both knees, an interview on existing knee complaints and a physical examination. As a common baseline for these assessments, skiers were prospectively monitored by the use of the Oslo Sports Trauma Research Centre questionnaire on health problems over a period of 12 months preceding the major investigations.
Results
88.0% of the youth skiers showed at least one MRI abnormality in the knees. The most frequent findings were distal femoral cortical irregularities (63%), focal periphyseal oedema (FOPE) zones (25.0%) and cartilage lesions (18.5%). 47.2% of all skiers suffered from at least one overuse-related knee complaint during the 12 months preceding the MRI examination, mostly at the distal and proximal patellar tendon. However, despite a certain association with corresponding MRI abnormalities, the sensitivity of an MRI-based detection of such complaints was strongly limited.
Conclusion
Youth competitive alpine skiers suffer from a remarkably large number of knee overuse injuries. Accordingly, an effective prevention strategy should include a systematic screening of clinical complaints, ideally already starting around the growth spurt.
Keywords: prevention, skiing, radiology, tendon, young
What are the new findings?
This is the first investigation that assessed the prevalence of knee overuse-related clinical complaints and MRI abnormalities in a cohort of youth competitive alpine skiers, whose knees are particularly exposed to adverse loads. It revealed remarkably high rates of patellar tendon-related complaints, for which despite clear clinical sings, the sensitivity of an MRI-based detection was limited.
How it might impact on clinical practice in the near future?
Based on our findings, it is strongly recommended to systematically screen youth athletes for knee overuse injuries in general and the patellar tendon in particular. Moreover, the current study is expected to stimulate future research focusing on novel innovative assessment tools to detect early (or even subclinical) stages of such injuries.
Introduction
In competitive alpine skiing, the risk to sustain a traumatic knee injury is known to be relatively high.1–3 Accordingly, previous research primarily focused on traumatic injuries, whereas overuse-related injuries have received little attention.4 However, while skiing, the knee joint has to withstand enormous mechanical stress,5 6 plausibly putting athletes at high risks for accumulating structural damages over time. This risk for irreparable joint deteriorations might be particularly high in competitive alpine skiers (typical single leg loadings of up to 1.75 times body weight7) and youth athletes around the growth spurt, whose bodies are still maturing and, therefore, are especially vulnerable to adverse loadings. Moreover, youth athletes are not regularly seen by any medical staff yet, and in less severe cases, affected persons might not immediately ask for professional help.
In sports other than competitive alpine skiing, several abnormal (however mostly asymptomatic) knee MRI findings have been reported.8–12 In adolescent high-level volleyball players, degenerative changes of the knee like osteophytes and subarticular cysts were detected; however, they showed no change in prevalence or severity within a 2-year follow-up.13 In asymptomatic adolescent swimmers, significantly more abnormalities such as fat pad oedema, bone marrow oedema and joint effusion were observed than in age-matched and weight-matched controls.12 Across the literature, the occurrence of patellar tendon-related health problems appears to be remarkably high.14–16 However, to date, no study has assessed the exact prevalence of knee overuse injuries and their specific associations with structural changes in competitive alpine skiers; whereas, a more fundamental understanding of the corresponding onset, patterns and severity would help to define more effective prevention strategies in the near future.
Accordingly, the aim of the present study was to describe the knee overuse-related clinical complaints and MRI abnormalities in a cohort of youth competitive alpine skiers around the growth spurt.
Materials and methods
Participants and study design
In this cross-sectional study, 108 Swiss youth competitive alpine skiers aged 13–15 years were evaluated. In Switzerland, the skiers of the highest level advance to a national squad at the age of 16–17 years. During the preceding years, they are organised in certified regional performance centres (RLZ/CRP). Thus, the examinations took place during their years at the RLZ/CRP. Study participation was voluntary, and none of the participants reported systemic pathologies such as inflammatory arthritis or diabetes mellitus that would have been reasons.
MRI examination
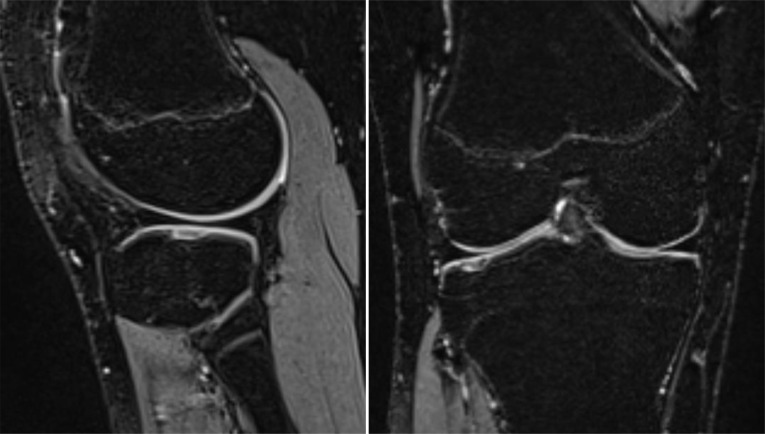
All youth skiers underwent an MRI scan of both knees. Examinations were performed using a 3T MR scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) and a dedicated knee coil. The standardised protocol was an isotropic fat-suppressed T2-weighted three-dimensional sequence (SPACE) with the following parameters: in-plane resolution 0.63×0.63 mm, slice thickness 0.63 mm, field of view (FOV) 160×160, Matrix 256×256, echo time (TE) 108 ms, repetition time (TR) 1000 ms, receiver bandwidth 415 Hz/Px, parallel imaging acceleration factor 4, duration 4:42 min. An example image is presented in figure 1.
Figure 1.
Sagittal (left) and coronar (right) fat-suppressed T2-weighted image of a cartilage lesion in the lateral tibial plateau.
Assessment of anthropometrics and biological maturation
In addition to the MRI examinations, the anthropometrics and biological maturation of all participating skiers were assessed. Body mass index (BMI) was defined as body weight in kilogram divided by squared body height in centimetre. Δheight was defined as the absolute growth in centimetre within the last 12 months. Athletes’ age at peak height velocity and their maturity offset were determined using the sex-specific formulae of Mirwald and colleagues17 that based on the anthropometric input parameters body height, sitting height and subischial leg length.
Assessment of clinical complaints
Over a period of 12 months preceding the MRI examinations, and as a common baseline for all other clinical assessments, athletes were prospectively monitored by a questionnaire on health problems that was completed in 14-day intervals (Oslo Sports Trauma Research Centre (OSTRC) questionnaire).18 19 This questionnaire was particularly recommended to detect overuse injuries and to quantify their severity.18 All health problems were classified as illness, traumatic or overuse injury.20 If athletes selected the option ‘registered for the first time’ in the questionnaire, a health problem was defined as being a ‘new’ incident. Illnesses and all injuries that were not related to the knee were not further considered for the current analysis. Immediately prior the MRI examinations, athletes underwent a systematic physical examination of their knees combined with an additional retrospective interview. The interview was intended to verify all OSTRC entries during the preceding 12 months and to complete the information on existing knee-related health problems (ie, to get additional relevant information on the knee problems previously reported in the questionnaire such as specific diagnosis or therapy) and, in rare cases, to possibly detect additional problems that might have been missed by the questionnaire. The physical examination was intended to exactly classify specific conditions like distal patellar tendon complaints (Osgood-Schlatter’s disease) and to detect other joint pathologies like ligamentous injuries. The assessments included inspection, palpation, evaluation of range of motion and stability in the sagittal and frontal plane. All examinations and interviews were performed by the same experienced physician specialised in orthopaedics and sports medicine. Finally, athletes were classified as ‘symptomatic’ when they suffered from at least one verified knee overuse-related health problem episode within the last 12 months prior to the MRI examination.
MRI interpretation
All MR images were systematically assessed by the same experienced radiologist specialised in musculoskeletal imaging. They were evaluated for the following findings: meniscus abnormalities, cartilage lesions, abnormalities of the ligaments and tendons, bone marrow oedema, trochlear dysplasia, distal femoral cortical irregularities, focal periphyseal oedema (FOPE) zones, joint effusion, Baker’s cyst and Hoffa’s fat pad oedema. The changes were classified as abnormal if they met the criteria listed in table 1.
Table 1.
Definition of the MRI findings assessed
| MRI finding | Definition |
| Meniscal degeneration | Significant hyperintense signal change within the meniscus without contact to the surface. |
| Meniscal tear | Significant linear hyperintense signal change within the meniscus with contact to the surface. |
| Cartilage lesion | Focal substance loss of the cartilage ICRS first to ICRS fourth degree. |
| ACL and PCL abnormalities | Tears, partial tears and significant signal alterations of the ACL or the PCL as well as the presence of a graft after ligament reconstruction. |
| Abnormalities of the patellar tendon or the quadriceps tendon (overall and subclassified with respect to location) | Morphological changes of the insertion or the tendon itself (hyperintense signal change, tendon thickening, oedema and ossicles). |
| Trochlear dysplasia | Flattened trochlear groove (Dejour type A–D). |
| Bone marrow oedema of the femoral condyles | Significant hyperintense signal change within the bone of the medial or lateral femoral condyle close to the articular surface. |
| Distal femoral cortical irregularities | Circumscript area of signal hyperintensity with a dark rim at the periphery at the insertion sites of the medial or lateral head of the gastrocnemius or the adductor magnus at the distal femur. |
| FOPE zones | Focal bone marrow oedema (significant hyperintense signal change) adjacent to areas of physeal fusion. |
| Joint effusion | Presence of increased intra-articular fluid. |
| Baker’s cyst | Popliteal fluid collection between medial head of the M. gastrocnemius and M. semimembranosus. |
| Hoffa’s fat pad oedema | Significant hyperintense signal change in the Hoffa’s fat pad. |
ACL, anterior cruciate ligament; FOPE, focal periphyseal oedema; ICRS, International Cartilage Repair Society; PCL, posterior cruciate ligament.
Patient and public involvement
Participating athletes and their parents were regularly informed and empowered for maintaining a superior adherence to the study tasks, such as the 2 weekly questionnaire on health problems. Individual findings were communicated to the participants by email and were, on request, discussed with their coaches. Overall findings were disseminated to all relevant expert stakeholders within the National Ski Federation Swiss-Ski and within the associated RLZ/CRP youth development structures by means of regular presentations and advanced training activities.
Statistical analysis
Statistical analyses were performed in Microsoft Excel and/or IBM SPSS statistics software V.23. For the purpose of this study, the following analysis steps were conducted: first, as suggested by Razali and Wah,21 the Shapiro-Wilk test, graphical techniques (ie, histograms and quantile-quantile plots) and shape parameters (ie, skewness and kurtosis coefficients) were used to check distribution normality in any metric data. Due to a slight departure from normality (as defined in West et al22), all statistical tests including age, Δheight and BMI were backed-up by bias-corrected accelerated (BCa) bootstrapping with 10 000 samples; otherwise standard parametric tests were used. Second, the participants’ baseline characteristics were expressed as mean±SD and differences in subgroups were tested for significance using unpaired sample t-tests (p<0.05). Third, the prevalence of skiers suffering from specific clinical complaints and MRI findings of the knee was described as the number of skiers with corresponding indications, as well as by their percentage proportion (number of subjects affected/total number of subjects per group or subgroup * 100). Corresponding sex differences, or differences between asymptomatic and symptomatic athletes, were analysed by Pearson χ2 tests (p<0.05). Fourth, if a pursuing analysis was indicated, univariate binary logistic regression models were used to assess the relationships between specific anthropometrics, clinical complaints and MRI abnormalities. Finally, the sensitivity and specificity for an MRI-based detection of patellar tendon-related clinical complaints were calculated.
Results
Baseline characteristics
The baseline characteristics of the participating athletes at the time of the MRI examinations are summarised in table 2.
Table 2.
Baseline characteristics
| Overall (n=108) |
Women (n=42) |
Men (n=66) |
|
| Age (years) | 14.83±0.58 | 14.74±0.66 | 14.88±0.52 |
| Maturity offset (years) | 1.27±1.09 | 2.26±0.59 | 0.64±0.83*** |
| APHV (years) | 13.56±1.05 | 12.48±0.46 | 14.24±0.68*** |
| Body height (cm) | 166.4±7.7 | 163.1±5.9 | 168.5±8.0*** |
| Δheight (cm) | 4.95±3.06 | 2.70±2.54 | 6.39±2.44*** |
| Body weight (kg) | 56.6±9.2 | 55.3±7.5 | 57.4±10.2 |
| BMI (kg/m2) | 20.33±2.34 | 20.78±2.50 | 20.04±2.20 |
All data are expressed as mean±SD. Level of significance based on unpaired sample t-tests and backed-up by bias-corrected accelerated bootstrapping with 10 000 samples: ***p<0.001.
APHV, age at peak height velocity; BMI, body mass index; Δheight, growth in body height during the last year.
MRI findings and sex differences
The major MRI findings observed in the knees of youth female and male competitive alpine skiers are summarised in table 3. As much as 88.0% of the youth skiers showed at least one MRI-detected abnormality in the knee. The most frequent MRI-detected knee abnormalities of athletes around the growth spurt were with 63% distal femoral cortical irregularities. They were generally located close to tendon insertions (95% at the femoral insertion of the medial head of the gastrocnemius muscle, 5% at the femoral insertion of the lateral head of the gastrocnemius muscle). In this connection, there was found a significant association between the predictor variable ‘increase in body height within the last 12 months’ and the dependent variable ‘occurrence of distal femoral cortical irregularities (univariate binary logistic regression analysis backed-up by BCa bootstrapping with 10 000 samples: χ2=13.533, p<0.001, R2Nagelkerke=0.161, n=108 and B=0.257 with the 95% CI 0.122 to 0.433), SEB=0.079, eB=1.293, p<0.001). Other frequent MRI findings were FOPE zones (25.0%) and cartilage lesions (18.5%) and bone marrow oedemas of the femoral condyles (13.9%). In view of the high proportion of athletes with clinical complaints at the distal or proximal patellar tendon (overall: 30.6%), there were relatively few MRI abnormalities on the distal insertion of the patellar tendon (11.1%) and even no MRI findings related to the proximal insertion and midportion of the patellar tendon. Comparing the different sexes, women showed a significantly higher prevalence of meniscal tears and a trend towards more cartilage lesions than males. However, within the 108 youth skiers assessed, there was only one case in which the MRI findings required an immediate stop of participating in ski training and competitions.
Table 3.
MRI findings in the knees of youth female and male competitive alpine skiers
| MRI finding | Overall (n=108) |
Women (n=42) |
Men (n=66) |
χ2 | P value |
| ≥1 MRI finding | 95 (88.0) | 35 (83.3) | 60 (90.9) | 0.167 | 0.682 |
| Meniscal degeneration | 11 (10.2) | 5 (11.9) | 6 (9.1) | 0.200 | 0.655 |
| Meniscal tear | 6 (5.6) | 5 (11.9) | 1 (1.5)* | 4.987 | 0.026 |
| Cartilage lesion | 20 (18.5) | 12 (28.6) | 8 (12.1)(t) | 3.751 | 0.053 |
| ACL and PCL abnormalities | 7 (6.5) | 4 (9.5) | 3 (4.5) | 0.981 | 0.322 |
| Abnormalities of the distal insertion of the patellar tendon | 12 (11.1) | 3 (7.1) | 9 (13.6) | 0.974 | 0.324 |
| Trochlear dysplasia | 7 (6.5) | 4 (9.5) | 3 (4.5) | 0.981 | 0.322 |
| Bone marrow oedema of the femoral condyles | 15 (13.9) | 3 (7.1) | 12 (18.2) | 2.252 | 0.133 |
| Distal femoral cortical irregularities | 68 (63.0) | 24 (57.1) | 44 (66.7) | 0.370 | 0.543 |
| FOPE zones | 27 (25.0) | 7 (16.7) | 20 (30.3) | 1.909 | 0.167 |
| Joint effusion | 11 (10.2) | 3 (7.1) | 8 (12.1) | 0.625 | 0.429 |
| Baker’s cyst | 15 (13.9) | 3 (7.1) | 12 (18.2) | 2.252 | 0.133 |
| Hoffa’s fat pad oedema | 8 (7.4) | 2 (4.8) | 6 (9.1) | 0.650 | 0.420 |
Prevalence data are expressed as the number of skiers with specific MRI findings, as well as their percentage proportion (number of subjects affected/total number of subjects per group or subgroup * 100; (%)) in brackets. Level of significance for sex differences based on Pearson’s χ2 tests: (t)p<0.10; *p<0.05.
FOPE, focal periphyseal oedema.
Clinical complaints and sex differences
The response rate to the OSTRC questionnaire during the 12-month observation period was 97.1%±2.5% on average. As much as 47.2% of all skiers suffered at least one overuse-related knee complaint during the preceding 12 months (table 4). Distal patellar complaints (17.6%) and proximal patellar complaints (18.5%) were most prevalent, whereas 16.7% had to be classified as indistinct overuse complaints. The only sex difference with respect to clinical complaints was found for traumatic knee sprains (overall: 10/108 skiers (9.3%); women: 8/42 skiers (19.0%); men: 2/66 skiers (3.0%), χ2=7.112, p=0.008).
Table 4.
Overuse-related knee complaints of youth female and male competitive alpine skiers
| Overuse-related knee complaints | Overall (n=108) |
Women (n=42) |
Men (n=66) |
χ2 | P value |
| ≥1 clinical complaint | 51 (47.2) | 21 (50.0) | 30 (45.5) | 0.112 | 0.738 |
| Distal patellar tendon complaint | 19 (17.6) | 5 (11.9) | 14 (21.2) | 1.264 | 0.261 |
| Proximal patellar tendon complaint | 20 (18.5) | 9 (21.4) | 11 (16.7) | 0.314 | 0.575 |
| Indistinct overuse complaint | 18 (16.7) | 9 (21.4) | 9 (13.6) | 0.935 | 0.334 |
Prevalence data are expressed as the number of skiers with specific clinical indications, as well as their percentage proportion (number of subjects affected/total number of subjects per group or subgroup * 100; (%)) in brackets. Level of significance for sex differences are based on Pearson’s χ2 tests. There were no significant results at p<0.05.
MRI findings in skiers with and without overuse-related knee complaints
Table 5 summarises the MRI findings in the knees of youth competitive alpine skiers with (symptomatic) and without (asymptomatic) overuse-related knee complaints. Comparing the groups of asymptomatic versus symptomatic skiers in general, there were no significant differences at p<0.05. The only exceptions were abnormalities of the distal insertion of the patellar tendon, which were significantly higher in symptomatic (21.6%) versus asymptomatic (1.8%) skiers (p<0.01).
Table 5.
MRI findings in the knees of youth competitive alpine skiers with (symptomatic) and without (asymptomatic) overuse-related knee complaints
| MRI finding | Overall (n=108) |
Asymptomatic (n=57) |
Symptomatic (n=51) |
χ2 | P value |
| ≥1 MRI finding | 95 (88.0) | 47 (82.5) | 48 (94.1) | 0.416 | 0.519 |
| Meniscal degeneration | 11 (10.2) | 7 (12.3) | 4 (7.8) | 0.520 | 0.471 |
| Meniscal tear | 6 (5.6) | 4 (7.0) | 2 (3.9) | 0.464 | 0.496 |
| Cartilage lesion | 20 (18.5) | 10 (17.5) | 10 (19.6) | 0.062 | 0.803 |
| ACL and PCL abnormalities | 7 (6.5) | 5 (8.8) | 2 (3.9) | 0.978 | 0.323 |
| Abnormalities of the distal insertion of the patellar tendon | 12 (11.1) | 1 (1.8) | 11 (21.6)** | 9.510 | 0.002 |
| Trochlear dysplasia | 7 (6.5) | 5 (8.8) | 2 (3.9) | 0.978 | 0.323 |
| Bone marrow oedema of the femoral condyles | 15 (13.9) | 8 (14.0) | 7 (13.7) | 0.002 | 0.966 |
| Distal femoral cortical irregularities | 68 (63.0) | 31 (54.4) | 37 (72.5) | 1.410 | 0.235 |
| FOPE zones | 27 (25.0) | 13 (22.8) | 14 (27.5) | 0.232 | 0.630 |
| Joint effusion | 11 (10.2) | 5 (8.8) | 6 (11.8) | 0.237 | 0.626 |
| Baker’s cyst | 15 (13.9) | 9 (15.8) | 6 (11.8) | 0.314 | 0.575 |
| Hoffa’s fat pad oedema | 8 (7.4) | 2 (3.5) | 6 (11.8) | 2.476 | 0.116 |
Prevalence data are expressed as the number of skiers with specific MRI findings, as well as their percentage proportion (number of subjects affected/total number of subjects per group or subgroup * 100; (%)) in brackets. Level of significance for sex differences are based on Pearson’s χ2 tests: **p<0.01.
FOPE, focal periphyseal oedema.
Sensitivity and specificity of MRI-based assessments of the patellar tendon
Indeed, an additional univariate logistic regression analysis revealed a direct association of the predictor variable ‘abnormalities of the distal insertion of the patellar tendon’ and the clinical indication ‘distal patellar tendon complaint’ (eg, Osgood-Schlatter disease) as the dependent variable (χ2=29.924, p<0.001, R2Nagelkerke=0.400, n=108 and B=3.878, SEB=0.850, eB=48.333, p<0.001). However, the sensitivity of an MRI-based detection of a ‘distal patellar tendon complaint’ (ie, a clinically diagnosed Osgood-Schlatter disease) by the MRI finding ‘abnormalities of the distal insertion of the patellar tendon’ was 0.526, while the specificity revealed to be 0.978 (n=108; positive: 19; negative: 89 → true positive: 10; false negative: 9; true negative: 87; false positive: 2). For athletes with the clinical indication ‘proximal patellar complaint’, even no MRI-detected abnormalities were observed.
Discussion
The major findings of the study were: (1) in 88.0% of the analysed youth competitive alpine skiers at least one knee-related MRI abnormality was found; (2) the most frequent MRI findings were distal femoral cortical irregularities, FOPE zones and cartilage lesions and bone marrow oedemas of the femoral condyles; (3) highly prevalent clinical complaints were distal and proximal patellar tendon-related problems; (4) the only MRI findings differing between a group of youth skiers with and without overuse-related knee complaints were abnormalities of the distal insertion of the patellar tendon; and (5) despite a certain association between clinical complaints and MRI abnormalities related to the distal insertion of the patellar tendon, as well as a superior determination specificity, an MRI-based detection of such complaints was strongly limited with respect to sensitivity.
High prevalence of MRI abnormalities and overuse-related knee complaints in youth competitive alpine skiers
As revealed in this study, youth competitive alpine skiers suffer from a remarkably large number of knee MRI abnormalities (88.0%); most frequently, these are distal femoral cortical irregularities, FOPE zones, cartilage lesions and bone marrow oedemas of the femoral condyle (table 3). The prevalence of cartilage lesions is as high as 18.5%. Compared with literature, this is a relatively high proportion. A study evaluating 44 knees of 44 adult asymptomatic volunteers aged 20–68 years found cartilage lesions in 11%.23 Another study looking at 100 asymptomatic knees of 100 subjects with symptoms on the contralateral side (aged 18–73 years) found cartilage lesions in 25%.24 In 40 knees of 20 professional basketball players, 47.5% had cartilage lesions.10 During the 2016 Summer Olympics, 64 cartilage lesions were seen in the MRIs of 113 athletes of different sports.25 However, these studies did not target on youth athletes. In 18 adolescent volleyball players, for instance, no cartilage lesions were detected.13
The distal femoral cortical irregularities appear to be of no clinical relevance and, therefore, are considered as incidental findings. It is assumed that they are the result of tensile stress at the tendinous attachment sites of skeletal muscles in areas with excessive growth-dependent metaphyseal cortical remodelling.26 27 This presumption is further supported by our finding of a significant association between the increase in body height within the last 12 months and the occurrence of distal femoral cortical irregularities. In literature, they are generally considered benign and self-limiting.27 28 The same applies to FOPE zones. They are discussed as a potential reason for knee pain,29 30 but the actual clinical importance remains unclear.
Bone marrow oedemas of the femoral condyle were certainly common (13.9%) but not associated with clinical symptoms. This finding in youth competitive alpine skiers is in line with other studies focusing on that abnormality in different populations.9 11 12 31–33 However, the clinical value of this MRI finding remains unclear.12 34 35 Some authors claim that bone marrow oedemas represent an unspecific stress reaction and not a relevant pathology.9 33 36
The number of youth skiers reporting at least one overuse-related knee complaint during the preceding 12 months was with 47.2% also relatively high (table 4). A previous study evaluating 45 skiers of a slightly higher mean age of 17, even found a higher prevalence magnitude of 73%.37 This suggests that the rate is still increasing at that age. Thus, effective prevention measures should ideally be established before the age at which our examinations were conducted.
Sex differences with respect to MRI abnormalities and overuse-related knee complaints
The significantly higher prevalence of meniscus tears in women with respect to a similar prevalence of meniscus degenerations for both sexes (table 3) is most likely an incidental finding. It might be explained by the significantly higher rate of knee sprains (8/42 (19.0%) women, 2/66 (3.0%) men, χ2 7.112, p=0.008) during the observation period. The same applies to the trend towards a higher prevalence of cartilage injuries in women. In the literature, no other studies detecting female sex as a risk factor for meniscal injuries in adolescents are available. It has been shown that meniscal tears often heal spontaneously in that age group.38
The clinically most relevant complaints relate to the distal and proximal patellar tendon
Patellar tendinopathy is relatively common in adolescent athletes. In the literature, prevalence magnitudes of 5.8% (n=760, average age 13 years) and 7% (n=134, age 14–18 years) were reported for different sports.39 40 In elite volleyball players aged 15–19 years, the rate of jumper’s knee was as high as 11%.41 An ultrasound study of 119 young soccer players (mean age 15.97 years) showed high rates of structural abnormalities within the tendon,42 and other studies demonstrated a high correlation between a clinical tendinopathy and structural intratendinous alterations in ultrasound.43 44 In the current study with a cohort of youth skiers, even a higher proportion of the athletes had clinical complaints at the distal or proximal patellar tendon (overall: 31.5%; distal: 17.6%; proximal: 18.5%). While in most cases the clinical diagnosis ‘Osgood-Schlatter disease’ (ie, distal patellar tendon complaints) was accompanied by radiological findings in the MRI, for the clinical diagnosis ‘proximal patellar tendinopathy/jumper’s knee’ (ie, proximal patellar tendon complaints), no radiological equivalent (including radiological signs of Sinding-Larsen-Johansson disease) was found. Sinding-Larsen-Johansson disease describes the combination of the clinical condition with a fragmentation or calcification at the inferior pole of the patella.14 45 However, regardless of whether radiological signs are present or not, it is worth pointing out that due to the high prevalence of the patellar tendon-related problems, these problems should be of primary prevention focus in youth skiers.
The sensitivity of an MRI-based early recognition of patellar tendon-related problems: so far not so good
As shown in this study, despite clear clinical signs, the sensitivity of MRI to detect indications of patellar tendon-related complaints was strongly limited. Accordingly, an effective patellar tendon screening approach in youth competitive alpine skiers should rather include a systematic assessment of clinical complaints than an MRI.
Methodological considerations
There are a couple of limitations one should be aware of when interpreting the study findings. First, the collection of data on clinical complaints may suffer from a recall and/or reporting bias. In an attempt to reduce the recall bias, data on knee overuse injuries were collected prospectively in 2-week intervals. To verify the correctness and completeness of the prospectively self-reported questionnaire data and to counteract the risk of a reporting bias, retrospective interviews with a team physician were conducted. Moreover, for being able to provide a complete picture of the occurring knee overuse injuries (eg, including specific clinical diagnoses), additionally physical examinations were conducted. Second, the cross-sectional nature of the major examinations of the clinical complaints and MRI abnormalities does not allow conclusively answering questions on causal relationships and on the process of development of overuse injuries over time. Thus, for clarifying the clinical relevance of certain (so far) asymptomatic MRI findings, further longitudinal studies are required. Nevertheless, at least in some cases, associations between specific clinical complaints and MRI abnormalities were already evident, implying valuable new insights for the prevention of knee overuse injuries in youth competitive alpine skiers.
Conclusion
Youth competitive alpine skiers present a remarkably large number of knee MRI abnormalities. The only clinically relevant MRI abnormalities were those at the distal insertion of the patellar tendon, which were directly associated with clinical signs of Osgood-Schlatter disease. However, despite clear complaints related to the distal patellar tendon, the sensitivity of MRI to detect such clinical conditions was strongly limited. Accordingly, an effective prevention strategy should primarily include a systematic screening of clinical complaints, ideally starting in youth athletes around the growth spurt.
Acknowledgments
We would like to thank all participants, parents and coaches involved. A special thank goes to Serge Allemand, the U16 Coordinator of Swiss-Ski, and the Swiss Centre for Musculoskeletal Imaging, SCMI, Balgrist Campus AG, Zürich, where the study was conducted.
Footnotes
Contributors: JS and RS conceptualised and designed the study. JS recruited the participants and organised the data collection. SF, LP and JS collected the data. SF, LP, CS and JS evaluated the data and performed the statistical analysis. All authors substantially contributed to the interpretation of data. SF and JS drafted the current manuscript; all authors revised it critically, approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Funding: This study was generously supported by the Balgrist Foundation, Swiss-Ski, the ‘Stiftung Passion Schneesport’ and the ‘Stiftung zur Förderung des alpinen Skisportes in der Schweiz’.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Ethics approval: The underlying study protocol was approved by the local ethics committee (KEK-ZH-NR: 2017-01395).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Flørenes TW, Bere T, Nordsletten L, et al. Injuries among male and female world cup alpine skiers. Br J Sports Med 2009;43:973–8. 10.1136/bjsm.2009.068759 [DOI] [PubMed] [Google Scholar]
- 2.Bere T, Flørenes TW, Nordsletten L, et al. Sex differences in the risk of injury in world cup alpine skiers: a 6-year cohort study. Br J Sports Med 2014;48:36–40. 10.1136/bjsports-2013-092206 [DOI] [PubMed] [Google Scholar]
- 3.Haaland B, Steenstrup SE, Bere T, et al. Injury rate and injury patterns in FIS world cup alpine skiing (2006-2015): have the new Ski regulations made an impact? Br J Sports Med 2016;50:32–6. 10.1136/bjsports-2015-095467 [DOI] [PubMed] [Google Scholar]
- 4.Supej M, Senner V, Petrone N, et al. Reducing the risks for traumatic and overuse injury among competitive alpine skiers. Br J Sports Med 2017;51:1–2. 10.1136/bjsports-2016-096502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klous M, Müller E, Schwameder H. Three-Dimensional knee joint loading in alpine skiing: a comparison between a carved and a skidded turn. J Appl Biomech 2012;28:655–64. 10.1123/jab.28.6.655 [DOI] [PubMed] [Google Scholar]
- 6.Zorko M, Nemec B, Babič J, et al. The waist width of Skis influences the kinematics of the knee joint in alpine skiing. J Sports Sci Med 2015;14:606–19. [PMC free article] [PubMed] [Google Scholar]
- 7.Kröll J, Spörri J, Gilgien M, et al. Effect of Ski geometry on aggressive Ski behaviour and visual aesthetics: equipment designed to reduce risk of severe traumatic knee injuries in alpine giant slalom Ski racing. Br J Sports Med 2016;50:20–5. 10.1136/bjsports-2015-095433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunner MC, Flower SP, Evancho AM, et al. MRI of the athletic knee. findings in asymptomatic professional basketball and collegiate football players. Invest Radiol 1989;24:72–5. 10.1097/00004424-198901000-00015 [DOI] [PubMed] [Google Scholar]
- 9.Chang X-D, Yang P, Mu X-Y, et al. Evaluation of knees in asymptomatic amateur ice hockey players using 3.0-T magnetic resonance imaging: a case-control study. Chin Med J 2018;131:1038–44. 10.4103/0366-6999.230723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan LD, Schurhoff MR, Selesnick H, et al. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy 2005;21:557–61. 10.1016/j.arthro.2005.01.009 [DOI] [PubMed] [Google Scholar]
- 11.Pappas GP, Vogelsong MA, Staroswiecki E, et al. Magnetic resonance imaging of asymptomatic knees in collegiate Basketball players: the effect of one season of play. Clin J Sport Med 2016;26:483–9. 10.1097/JSM.0000000000000283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soder RB, Mizerkowski MD, Petkowicz R, et al. MRI of the knee in asymptomatic adolescent swimmers: a controlled study. Br J Sports Med 2012;46:268–72. 10.1136/bjsm.2010.083345 [DOI] [PubMed] [Google Scholar]
- 13.Boeth H, MacMahon A, Eckstein F, et al. MRI findings of knee abnormalities in adolescent and adult volleyball players. J Exp Orthop 2017;4:6. 10.1186/s40634-017-0080-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medlar RC, Lyne ED. Sinding-Larsen-Johansson disease. its etiology and natural history. J Bone Joint Surg Am 1978;60:1113–6. 10.2106/00004623-197860080-00021 [DOI] [PubMed] [Google Scholar]
- 15.Atanda A, Shah SA, O'Brien K. Osteochondrosis: common causes of pain in growing bones. Am Fam Physician 2011;83:285–91. [PubMed] [Google Scholar]
- 16.Peace KAL, Lee JC, Healy J. Imaging the infrapatellar tendon in the elite athlete. Clin Radiol 2006;61:570–8. 10.1016/j.crad.2006.02.005 [DOI] [PubMed] [Google Scholar]
- 17.Mirwald RL, Baxter-Jones ADG, Bailey DA, et al. An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc 2002;34:689–94. 10.1097/00005768-200204000-00020 [DOI] [PubMed] [Google Scholar]
- 18.Clarsen B, Myklebust G, Bahr R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: the Oslo sports trauma research centre (OSTRC) overuse injury questionnaire. Br J Sports Med 2013;47:495–502. 10.1136/bjsports-2012-091524 [DOI] [PubMed] [Google Scholar]
- 19.Hirschmüller A, Steffen K, Fassbender K, et al. German translation and content validation of the OSTRC questionnaire on overuse injuries and health problems. Br J Sports Med 2017;51:260–3. 10.1136/bjsports-2016-096669 [DOI] [PubMed] [Google Scholar]
- 20.Clarsen B, Rønsen O, Myklebust G, et al. The Oslo sports trauma research center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med 2014;48:754–60. 10.1136/bjsports-2012-092087 [DOI] [PubMed] [Google Scholar]
- 21.Razali NM, Wah YB. Power comparisons of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. J Stat Model Anal 2011;2:21–33. [Google Scholar]
- 22.West SG, Finch JF, Curran PJ. Structural equation models with nonnormal variables: problems and remedies : Structural equation modeling: concepts, issues, and applications. Thousand Oaks, CA, US: Sage Publications, Inc, 1995: 56–75. [Google Scholar]
- 23.Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage 2005;13:181–6. 10.1016/j.joca.2004.11.001 [DOI] [PubMed] [Google Scholar]
- 24.Zanetti M, Pfirrmann CWA, Schmid MR, et al. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol 2003;181:635–41. 10.2214/ajr.181.3.1810635 [DOI] [PubMed] [Google Scholar]
- 25.Kompel AJ, Murakami AM, Engebretsen L, et al. Mri-Detected sports-related knee injuries and abnormalities at the Rio de Janeiro 2016 summer Olympic Games. AJR Am J Roentgenol 2018;211:880–6. 10.2214/AJR.17.19334 [DOI] [PubMed] [Google Scholar]
- 26.Goldin A, Muzykewicz DA, Dwek J, et al. The aetiology of the non-ossifying fibroma of the distal femur and its relationship to the surrounding soft tissues. J Child Orthop 2017;11:373–9. 10.1302/1863-2548.11.170068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vieira RLR, Bencardino JT, Rosenberg ZS, et al. Mri features of cortical desmoid in acute knee trauma. AJR Am J Roentgenol 2011;196:424–8. 10.2214/AJR.10.4815 [DOI] [PubMed] [Google Scholar]
- 28.Tscholl PM, Biedert RM, Gal I. Cortical desmoids in adolescent top-level athletes. Acta Radiol Open 2015;4:205846011558087. 10.1177/2058460115580878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leschied JR, Udager KG. Imaging of the pediatric knee. Semin Musculoskelet Radiol 2017;21:137–46. 10.1055/s-0037-1599205 [DOI] [PubMed] [Google Scholar]
- 30.Zbojniewicz AM, Laor T, Edema FP. Focal Periphyseal edema (FOPE) zone on MRI of the adolescent knee: a potentially painful manifestation of physiologic physeal fusion? AJR Am J Roentgenol 2011;197:998–1004. 10.2214/AJR.10.6243 [DOI] [PubMed] [Google Scholar]
- 31.Kornaat PR, Van de Velde SK. Bone marrow edema lesions in the professional runner. Am J Sports Med 2014;42:1242–6. 10.1177/0363546514521990 [DOI] [PubMed] [Google Scholar]
- 32.Major NM, Helms CA. MR imaging of the knee: findings in asymptomatic collegiate basketball players. AJR Am J Roentgenol 2002;179:641–4. 10.2214/ajr.179.3.1790641 [DOI] [PubMed] [Google Scholar]
- 33.Soder RB, Simões JD, Soder JB, et al. MRI of the knee joint in asymptomatic adolescent soccer players: a controlled study. AJR Am J Roentgenol 2011;196:W61–5. 10.2214/AJR.10.4928 [DOI] [PubMed] [Google Scholar]
- 34.Culvenor AG, Øiestad BE, Hart HF, et al. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med 2019;53:1268–78. 10.1136/bjsports-2018-099257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kornaat PR, de Jonge MC, Maas M. Bone marrow edema-like signal in the athlete. Eur J Radiol 2008;67:49–53. 10.1016/j.ejrad.2008.01.057 [DOI] [PubMed] [Google Scholar]
- 36.Krajnc Z, Rupreht M, Drobnič M. Quantitative evaluation of growth plates around the knees of adolescent soccer players by diffusion-weighted magnetic resonance imaging. Biomed Res Int 2015;2015:1–6. 10.1155/2015/482017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bergstrøm KA, Brandseth K, Fretheim S, et al. Activity-Related knee injuries and pain in athletic adolescents. Knee Surg Sports Traumatol Arthrosc 2001;9:146–50. 10.1007/s001670100206 [DOI] [PubMed] [Google Scholar]
- 38.Ekås GR, Laane MM, Larmo A, et al. Knee pathology in young adults after pediatric anterior cruciate ligament injury: a prospective case series of 47 patients with a mean 9.5-Year follow-up. Am J Sports Med 2019;47:1557–66. 10.1177/0363546519837935 [DOI] [PubMed] [Google Scholar]
- 39.Cassel M, Baur H, Hirschmüller A, et al. Prevalence of Achilles and Patellar tendinopathy and their association to intratendinous changes in adolescent athletes. Scand J Med Sci Sports 2015;25:e310–8. 10.1111/sms.12318 [DOI] [PubMed] [Google Scholar]
- 40.Cook JL, Khan KM, Kiss ZS, et al. Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 Patellar tendons in players aged 14-18 years. Scand J Med Sci Sports 2000;10:216–20. 10.1034/j.1600-0838.2000.010004216.x [DOI] [PubMed] [Google Scholar]
- 41.Gisslèn K, Gyulai C, Söderman K, et al. High prevalence of jumper's knee and sonographic changes in Swedish elite junior volleyball players compared to matched controls. Br J Sports Med 2005;39:298–301. 10.1136/bjsm.2004.014290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bode G, Hammer T, Karvouniaris N, et al. Patellar tendinopathy in young elite soccer- clinical and sonographical analysis of a German elite soccer Academy. BMC Musculoskelet Disord 2017;18:344. 10.1186/s12891-017-1690-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cassel M, Risch L, Intziegianni K, et al. Incidence of Achilles and Patellar tendinopathy in adolescent elite athletes. Int J Sports Med 2018;39:726–32. 10.1055/a-0633-9098 [DOI] [PubMed] [Google Scholar]
- 44.Gisslén K, Alfredson H. Neovascularisation and pain in jumper's knee: a prospective clinical and sonographic study in elite junior volleyball players. Br J Sports Med 2005;39:423–8. 10.1136/bjsm.2004.013342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iwamoto J, Takeda T, Sato Y, et al. Radiographic abnormalities of the inferior pole of the patella in juvenile athletes. Keio J Med 2009;58:50–3. 10.2302/kjm.58.50 [DOI] [PubMed] [Google Scholar]