Dear Editor,
Recently, Chen Tao (Doctor) and colleagues published a retrospective study, and delineated the clinical characteristics of patients with coronavirus disease 2019 (COVID-19) who died1. They found that chronic hypertension and other cardiovascular comorbidities were more frequent among deceased patients than recovered patients1. And there was no difference in the prevalence of the autoimmune disease between the two group patients1. We appreciate this discovery, however, the conclusion of their study drew from a retrospective study, and the number of patients is only 113. Higher levels of evidence are needed to evaluate the association between severe or death COVID-19 and autoimmune disease. Therefore, we conducted the present systematic review and meta-analysis.
Studies published up to 8 May 2020 were searched through PubMed, Embase.com, Web of Science and Cochrane Library. The published language was not restricted. Keywords included “COVID-19”, “coronavirus disease-19”, “new coronavirus”, “2019-nCoV”, “novel corona virus”, “novel coronavirus”, “nCoV-2019”, “2019 novel coronavirus”, “coronavirus disease 2019”, “SARS-CoV-2”, “severe acute respiratory syndrome coronavirus 2”, “autoimmune disease”, “clinical characteristic”, “clinical feature”, “risk factor”, and “comorbidities”. In addition, we searched the reference lists of eligible studies and relevant reviews to find potentially eligible studies (See search strategy of PubMed in Appendix Table 1 ).
Table 1.
Characteristics of included studies.
| Study | Country | Language | Age.yeara | Sex |
Severe |
Non-severe |
Death |
Survival |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Events | Total | Events | Total | Events | Total | Events | Total | ||||
| Wei YY3 | China | English | 42.3±15.3 | 95 | 72 | 0 | 30 | 2 | 137 | ||||
| Wang L(1)4 | China | Chinese | 63.0(51.0-70.0) | 88 | 114 | 1 | 33 | 3 | 169 | ||||
| Du RH5 | China | English | 70.7±10.9 | 74 | 35 | 1 | 51 | 0 | 58 | ||||
| Wang L(2)6 | China | English | 69.0 (65.0-76.0) | 168 | 171 | 1 | 65 | 4 | 274 | ||||
| Chen T1 | China | English | 62.0 (44.0-70.0) | 171 | 103 | 1 | 113 | 1 | 161 | ||||
| Argenziano MG7 | USA | English | 63.0(50.0-75.0) | 596 | 404 | 9 | 231 | 26 | 769 | ||||
Age data presented as median (IQR) or mean ± SD.
Study inclusion criteria: (1) patient was diagnosed as COVID-19 by the laboratory test; (2) provided data of autoimmune disease with severe or non-severe patients or between death and survivors. Study exclusion criteria: (1) studies did not provide the prevalence of autoimmune disease; (2) studies without comparisons (severe versus non-severe patients, death versus survival); (3) studies sample size is less than 10 patients; (4) abstracts, news, comments, editorials and review articles. According to the published studies2, the severity of disease was defined mainly on the basis of the symptoms present at diagnosis (e.g. patients with pulse oxygen saturation (SpO2) less than 90%, or need of intensive care unit (ICU) care, or with acute respiratory distress syndrome).
Study selection and data extraction were independently conducted by two reviewers. Disagreements were resolved by consensus or by a third investigator. We extracted the following data: first author, year of publication, country of the corresponding author, publication language, recruitment time frame, age and sex of patients, sample size, number of participants in severe (or death) and non-severe (or survival) disease groups, and outcomes of interest. The primary outcome was the association between autoimmune disease and risk of severe disease in patients with COVID-19. The secondary outcome was the association between autoimmune disease and risk of mortality in COVID-19 patients.
Review Manager 5.3 (Nordic Cochrane Centre, Copenhagen, Denmark) was used to estimate pooled odds risk (OR) and its 95% confidence interval (CI) for dichotomous outcomes using the Mantel-Haenszel statistical method with the random-effects model. We used the I2 statistic to assess the heterogeneity, value of <25%, 26-50%, and >50% considered as low, moderate, and high degrees of heterogeneity, respectively. Subgroup analysis was conducted for the secondary outcome between different countries. In addition, we also conducted sensitivity analysis by excluding studies published in Chinese to assess the stability of the results.
A total of 2472 records were obtained through systematic electronic searches and other ways. After screening titles, abstracts, and full texts, 6 studies1, 3, 4, 5, 6, 7 were included for analysis (See flowchart in Appendix Fig. 1 ). All studies were published in 2020, incorporated a total of 2091 patients (1192 males, 57.01%). The sample size of patients per study ranged from 109 to 1000. Only one study from USA7, five studies from China1 , 3, 4, 5, 6. One study published in Chinese 4, and five studies published in English1 , 3 , 5, 6, 7. See detail in Table 1. The range of quality scores was 5 to 8, with a median of 7 (7.17±1.17) (Appendix Table 2).
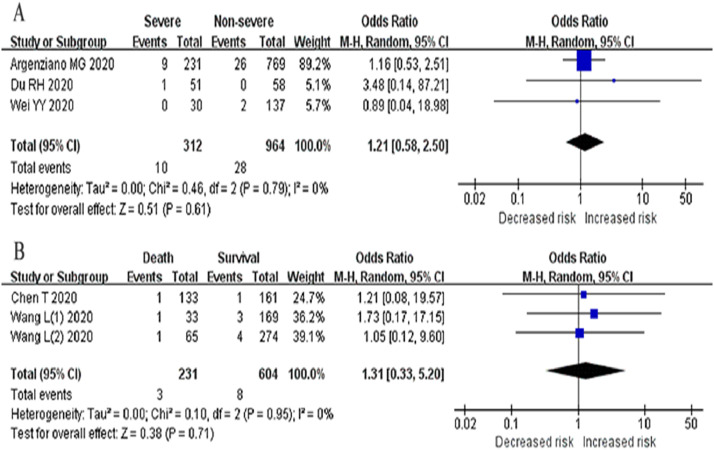
Fig. 1.
Association between autoimmune disease and COVID-19 disease (A: Severe versus Non-severe patients; B: Death versus Survival).
The meta analysis showed that autoimmune disease was associated with a 1.21-fold increased risk of severe COVID-19 disease (3 studies3 , 5 , 7, 1276 patients; OR=1.21, 95%CI: 0.58 to 2.50, P=0.79; I2=0%) (Fig. 1A). We found that autoimmune disease was associated with a 1.31-fold increased risk of mortality in patients with COVID-19 (3 studies1 , 4 , 6, 835 patients; OR=1.31, 95%CI: 0.33 to 5.20, P=0.95; I2=0%) (Fig. 1B). Although these two analysis results are not statistically significant (P>0.05). The subgroup analysis based on countries indicated no significant association between autoimmune disease and risk of mortality in patients with COVID-19 from China (2 studies1 , 6, 651 patients; OR=1.11, 95%CI: 0.20 to 6.27, P=0.94; I2=0%).
COVID-19 is an acute inflammatory infectious disease. It is now generally accepted that the occurrence of autoimmune diseases is related to autoinflammatory8. Over the course of the COVID-19 pandemic, Zachary SW and colleagues proposed three key reasons that COVID-19 may affect patients with autoimmune diseases9. Understanding how COVID-19 is associated with rheumatic diseases is imperative for rheumatology health professionals and people living with rheumatic diseases. Our study showed that autoimmune disease was slightly associated with increased risk of severity and mortality of COVID-19 through meta-analysis, but the statistical difference was not significant. In terms of treatment and prognosis, COVID-19 patients combined with autoimmune diseases may not need special attention. Nevertheless, we cannot let our guard down. Because our study was limited by small sample size, and five included studies are from China, the results should be interpreted with caution. In addition, researchers should also pay more attention to the impact of the types of autoimmune diseases and drugs on treatment and prognosis.
In conclusion, we should not relax our focus on the COVID-19 patients with autoimmune diseases. More high-quality studies from different regions are needed to better understand the association between COVID-19 disease and autoimmune diseases.
Declaration of Competing interest
The authors declare that they have no competing interests.
Acknowledgments
Funding
This work was supported by the Emergency Research Project of Key Laboratory of Evidence-based Medicine and Knowledge Translation of Gansu Province (Grant No. GSEBMKT-2020YJ01).
Role of the Funding Source
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Key message: Autoimmune disease was slightly associated with increased risk of severity and mortality of COVID-19 disease.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2020.05.065.
Appendix. Supplementary materials
References
- 1.Chen T., Wu D., Chen H. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study [published correction appears in BMJ. 2020 Mar 31;368:m1295]. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. Published 2020 Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mao R., Qiu Y., He J.S. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis [published online ahead of print, 2020 May 12] Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wei Y.Y., Wang R.R., Zhang D.W. Risk factors for severe COVID-19: Evidence from 167 hospitalized patients in Anhui, China [published online ahead of print, 2020 Apr 17] J Infect. 2020 doi: 10.1016/j.jinf.2020.04.010. S0163-4453(20)30219-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang L., He W.B., Yu X.M., Liu H.F., Zhou W.J., Jiang H., Zhonghua Yan Ke Za Zhi, 2020; 56(0):E009. doi: 10.3760/cma.j.cn112148-20200313-00202. [DOI] [PubMed]
- 5.Du R.H., Liu L.M., Yin W. Hospitalization and Critical Care of 109 Decedents with COVID-19 Pneumonia in Wuhan, China [published online ahead of print, 2020 Apr 7] Ann Am Thorac Soc. 2020 doi: 10.1513/AnnalsATS.202003-225OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L., He W., Yu X. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639‐645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Argenziano M.G., Bruce S.L., Slater C.L. Characterization and Clinical Course of 1000 Patients with COVID-19 in New York: retrospective case series. medRxiv. 2020 doi: 10.1101/2020.04.20.20072116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frizinsky S., Haj-Yahia S., Machnes M.D. The innate immune perspective of autoimmune and autoinflammatory conditions. Rheumatology (Oxford) 2019;58(Suppl 6):vi1‐vi8. doi: 10.1093/rheumatology/kez387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace Z.S., Bhana S., Hausmann J.S. The Rheumatology Community responds to the COVID-19 pandemic: the establishment of the COVID-19 global rheumatology alliance [published online ahead of print, 2020 May 6] Rheumatology (Oxford). 2020 doi: 10.1093/rheumatology/keaa191. keaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.